Combination antimicrobial therapy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Combination antimicrobial therapy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Combination antimicrobial therapy US Medical PG Question 1: A 72-year-old woman presents to the clinic complaining of diarrhea for the past week. She mentions intense fatigue and intermittent, cramping abdominal pain. She has not noticed any blood in her stool. She recalls an episode of pneumonia last month for which she was hospitalized and treated with antibiotics. She has traveled recently to Florida to visit her family and friends. Her past medical history is significant for hypertension, peptic ulcer disease, and hypercholesterolemia for which she takes losartan, esomeprazole, and atorvastatin. She also has osteoporosis, for which she takes calcium and vitamin D and occasional constipation for which she takes an over the counter laxative as needed. Physical examination shows lower abdominal tenderness but is otherwise insignificant. Blood pressure is 110/70 mm Hg, pulse is 80/min, and respiratory rate is 18/min. Stool testing is performed and reveals the presence of anaerobic, gram-positive bacilli. Which of the following increased this patient’s risk of developing this clinical presentation?
- A. Hypercholesterolemia treated with atorvastatin
- B. Constipation treated with laxatives
- C. Osteoporosis treated with calcium and vitamin D
- D. Peptic ulcer disease treated with esomeprazole
- E. Recent antibiotic use for pneumonia treatment (Correct Answer)
Combination antimicrobial therapy Explanation: ***Recent antibiotic use for pneumonia treatment***
- **Antibiotic exposure** is the single most important risk factor for *Clostridioides difficile* infection (CDI), present in approximately 70% of cases.
- Antibiotics disrupt the normal protective gut microbiota, eliminating competitive bacteria and allowing *C. difficile* spores to germinate, colonize, and produce toxins.
- The patient's recent hospitalization and antibiotic treatment for pneumonia directly precipitated this infection by creating an ecological niche for *C. difficile* overgrowth.
- Common culprit antibiotics include fluoroquinolones, clindamycin, cephalosporins, and penicillins.
*Peptic ulcer disease treated with esomeprazole*
- **Proton pump inhibitors (PPIs)** like esomeprazole are an independent risk factor for CDI, increasing risk approximately 2-3 fold.
- PPIs reduce gastric acid production, which normally serves as a defense mechanism against ingested *C. difficile* spores.
- However, PPIs alone do not typically cause CDI without concurrent disruption of gut flora (usually by antibiotics).
- While this is a contributory risk factor in this patient, it is not the primary cause.
*Hypercholesterolemia treated with atorvastatin*
- **Statins** like atorvastatin have no established association with increased risk of *Clostridioides difficile* infection.
- They work by inhibiting HMG-CoA reductase to lower cholesterol and do not affect gastric pH or gut microbiota composition.
*Constipation treated with laxatives*
- Occasional **over-the-counter laxative use** is not a risk factor for *Clostridioides difficile* infection.
- While laxatives affect gut motility, they do not disrupt the protective gut microbiota or increase susceptibility to CDI.
*Osteoporosis treated with calcium and vitamin D*
- **Calcium and vitamin D supplementation** has no association with increased risk of *Clostridioides difficile* infection.
- These supplements support bone health and calcium metabolism without affecting gut flora or gastric acid production.
Combination antimicrobial therapy US Medical PG Question 2: A 68-year-old man comes to the physician because of headache, fatigue, and nonproductive cough for 1 week. He appears pale. Pulmonary examination shows no abnormalities. Laboratory studies show a hemoglobin concentration of 9.5 g/dL and an elevated serum lactate dehydrogenase concentration. A peripheral blood smear shows normal red blood cells that are clumped together. Results of cold agglutinin titer testing show a 4-fold elevation above normal. An x-ray of the chest shows diffuse, patchy infiltrates bilaterally. Treatment is begun with an antibiotic that is also used to promote gut motility. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of bacterial RNA polymerase
- B. Inhibition of folic acid synthesis
- C. Free radical creation within bacterial cells
- D. Inhibition of transpeptidase cross-linking at the cell wall
- E. Inhibition of peptide translocation at the 50S ribosomal subunit (Correct Answer)
Combination antimicrobial therapy Explanation: ***Inhibition of peptide translocation at the 50S ribosomal subunit***
- This drug described is likely **erythromycin** or another **macrolide antibiotic**, which inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit** and preventing translocation.
- Macrolides are used to treat **atypical pneumonia** caused by *Mycoplasma pneumoniae*, which is indicated by the patient's symptoms (headache, fatigue, nonproductive cough, bilateral patchy infiltrates) and **cold agglutinin disease**.
*Inhibition of bacterial RNA polymerase*
- This is the mechanism of action of **rifampin**, which is primarily used for **tuberculosis** and **meningitis prophylaxis**, not for atypical pneumonia.
- Rifampin's side effects and spectrum of activity do not align with the implied clinical scenario, especially the gut motility promotion.
*Inhibition of folic acid synthesis*
- This is the mechanism for **sulfonamides** and **trimethoprim**, which are bacteriostatic and target different pathogens than those causing cold agglutinin positive pneumonia.
- These drugs are not known for promoting gut motility.
*Free radical creation within bacterial cells*
- This mechanism is characteristic of **metronidazole**, an antibiotic used for anaerobic bacterial and parasitic infections.
- Metronidazole does not fit the clinical context of atypical pneumonia with cold agglutinins, nor is it a macrolide that promotes gut motility.
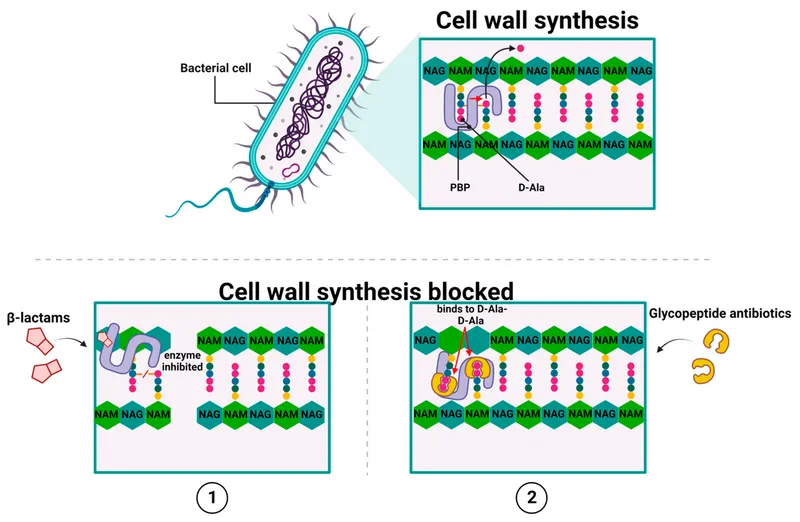
*Inhibition of transpeptidase cross-linking at the cell wall*
- This describes the mechanism of **beta-lactam antibiotics** (e.g., penicillins, cephalosporins), which are ineffective against **atypical pneumonia** because *Mycoplasma* lacks a cell wall.
- Beta-lactams do not typically promote gut motility.
Combination antimicrobial therapy US Medical PG Question 3: A 33-year-old HIV-positive male is seen in clinic for follow-up care. When asked if he has been adhering to his HIV medications, the patient exclaims that he has been depressed, thus causing him to not take his medication for six months. His CD4+ count is now 33 cells/mm3. What medication(s) should he take in addition to his anti-retroviral therapy?
- A. Azithromycin and fluconazole
- B. Azithromycin, dapsone, and fluconazole
- C. Dapsone
- D. Fluconazole
- E. Azithromycin and trimethoprim-sulfamethoxazole (Correct Answer)
Combination antimicrobial therapy Explanation: ***Azithromycin and trimethoprim-sulfamethoxazole***
- With a **CD4+ count of 33 cells/mm3**, this patient is at high risk for **Pneumocystis jirovecii pneumonia (PJP)** and **Toxoplasma gondii encephalitis**, for which **trimethoprim-sulfamethoxazole (TMP-SMX)** is the prophylaxis of choice.
- He is also at very high risk for **Mycobacterium avium complex (MAC) infection**, for which **azithromycin** is the recommended preventative treatment when the CD4 count is below 50 cells/mm3.
*Azithromycin and fluconazole*
- While **azithromycin** is indicated for MAC prophylaxis, **fluconazole** is typically used for **cryptococcal meningitis** or **candidiasis**, which are not the primary, immediate prophylactic concerns at this specific CD4 count unless there's evidence of these infections.
- The most critical opportunistic infections to prevent at a CD4 count of 33 cells/mm3 are PJP, Toxoplasmosis, and MAC.
*Azithromycin, dapsone, and fluconazole*
- **Dapsone** can be used as an alternative for **PJP prophylaxis** if TMP-SMX is contraindicated, but it is not the first-line choice and does not cover toxoplasmosis as effectively as TMP-SMX alone.
- **Fluconazole** again is not a primary prophylactic agent at this CD4 count in the absence of specific indications.
*Dapsone*
- **Dapsone** is an alternative for **PJP prophylaxis** and can also prevent **Toxoplasma gondii encephalitis** when combined with pyrimethamine, but it is not the first-line recommendation.
- It does not provide coverage against **MAC infection**, which is a significant risk at this CD4 count.
*Fluconazole*
- **Fluconazole** is primarily used for **fungal infections** like **candidiasis** or **cryptococcosis**.
- It does not prevent **PJP, Toxoplasmosis, or MAC**, which are the most critical prophylactic concerns for a patient with a CD4 count of 33 cells/mm3.
Combination antimicrobial therapy US Medical PG Question 4: An investigator is studying the chemical structure of antibiotics and its effect on bacterial growth. He has synthesized a simple beta-lactam antibiotic and has added a bulky side chain to the molecule that inhibits the access of bacterial enzymes to the beta-lactam ring. The synthesized drug will most likely be appropriate for the treatment of which of the following conditions?
- A. Folliculitis (Correct Answer)
- B. Nocardiosis
- C. Atypical pneumonia
- D. Erythema migrans
- E. Otitis media
Combination antimicrobial therapy Explanation: ***Folliculitis***
- The bulky side chain provides **steric hindrance** that prevents **staphylococcal beta-lactamases** from accessing and degrading the **beta-lactam ring**.
- This modification creates an **anti-staphylococcal penicillin** (similar to methicillin, nafcillin, or oxacillin), which is effective against **methicillin-sensitive *Staphylococcus aureus* (MSSA)**.
- **Folliculitis** is most commonly caused by *S. aureus*, making this modified beta-lactam an appropriate treatment choice for MSSA-related folliculitis.
- The bulky side chain specifically protects against the **penicillinase** (beta-lactamase) produced by staphylococci.
*Otitis media*
- Otitis media is commonly caused by beta-lactamase-producing organisms like *Haemophilus influenzae* and *Moraxella catarrhalis*.
- However, the beta-lactamases produced by these gram-negative organisms are **not inhibited by bulky side chains** alone.
- Treatment of beta-lactamase-producing *H. influenzae* and *M. catarrhalis* requires **beta-lactamase inhibitors** (such as clavulanic acid combined with amoxicillin), not steric hindrance.
- The mechanism of protection differs: beta-lactamase inhibitors **suicide inhibitors** that bind to the enzyme, whereas bulky side chains provide **physical blocking**.
*Nocardiosis*
- Nocardiosis is caused by *Nocardia* species, which are **aerobic actinomycetes**.
- These bacteria are typically treated with **sulfonamides** (trimethoprim-sulfamethoxazole) for prolonged periods.
- Beta-lactam antibiotics are generally not first-line treatment, as *Nocardia* species often show intrinsic resistance or require specific antibiotic combinations.
*Atypical pneumonia*
- Atypical pneumonia is caused by organisms like *Mycoplasma pneumoniae*, *Chlamydophila pneumoniae*, and *Legionella pneumophila*.
- These organisms lack a **peptidoglycan cell wall**, which is the target of all **beta-lactam antibiotics**.
- Beta-lactams (regardless of modifications) are completely ineffective against atypical pneumonia pathogens.
- Treatment requires **macrolides** (azithromycin), **tetracyclines** (doxycycline), or **fluoroquinolones**.
*Erythema migrans*
- Erythema migrans is the characteristic rash of early **Lyme disease**, caused by *Borrelia burgdorferi*.
- While *Borrelia* is sensitive to certain beta-lactam antibiotics (amoxicillin, ceftriaxone), it does **not produce beta-lactamases**.
- The bulky side chain modification is unnecessary for treating *Borreria* infections, as there is no beta-lactamase to protect against.
- Standard treatment uses doxycycline, amoxicillin, or ceftriaxone—not anti-staphylococcal penicillins.
Combination antimicrobial therapy US Medical PG Question 5: A 15-year-old boy presents with his father to the urgent care department with a 5-day history of frequent diarrhea, occasionally mixed with streaks of blood. Stool cultures are pending, but preliminary stool samples demonstrate fecal leukocytes and erythrocytes. The patient's vital signs are within normal limits, and he is started on outpatient therapy for presumed Shigella infection. Which of the following was the young man most likely started on?
- A. Oral vancomycin
- B. Oral erythromycin
- C. Oral metronidazole
- D. An oral quinolone
- E. Oral trimethoprim-sulfamethoxazole (TMP-SMX) (Correct Answer)
Combination antimicrobial therapy Explanation: **Oral trimethoprim-sulfamethoxazole (TMP-SMX)**
- **TMP-SMX** is a traditional first-line treatment for **Shigella infection** in settings where susceptibility is expected or confirmed.
- The patient's presentation with **bloody diarrhea**, **fecal leukocytes**, and **erythrocytes** is classic for **Shigella dysentery**.
- While **resistance rates vary by region**, TMP-SMX remains an appropriate choice when local susceptibility patterns support its use.
- It is cost-effective, well-tolerated, and appropriate for outpatient management of uncomplicated cases.
*Oral vancomycin*
- Vancomycin is specifically used for **Clostridioides difficile infection** and does not treat Shigella.
- It has **poor oral absorption** and no activity against Gram-negative enteric pathogens like Shigella.
*Oral erythromycin*
- Erythromycin is primarily effective against **Campylobacter jejuni** and respiratory pathogens.
- It has **limited activity against Shigella** and resistance rates are high, making it an inappropriate choice.
*Oral metronidazole*
- Metronidazole treats **anaerobic bacteria** and protozoal infections (*Giardia*, *Entamoeba histolytica*).
- It has **no significant activity against Shigella**, a facultative anaerobic Gram-negative bacillus.
*An oral quinolone*
- **Fluoroquinolones** (e.g., ciprofloxacin) are highly effective against Shigella and often used as first-line therapy, particularly in areas with high TMP-SMX resistance.
- They are increasingly preferred in current guidelines due to rising resistance to TMP-SMX.
- However, in the context of empiric outpatient treatment where susceptibility is presumed, **TMP-SMX** may still be chosen initially as a narrower-spectrum, cost-effective option, with fluoroquinolones reserved based on culture results or treatment failure.
Combination antimicrobial therapy US Medical PG Question 6: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Combination antimicrobial therapy Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Combination antimicrobial therapy US Medical PG Question 7: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Combination antimicrobial therapy Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
Combination antimicrobial therapy US Medical PG Question 8: A 62-year-old man is brought to the emergency department from a senior-care facility after he was found with a decreased level of consciousness and fever. His personal history is relevant for colorectal cancer that was managed with surgical excision of the tumor. Upon admission, he is found to have a blood pressure of 130/80 mm Hg, a pulse of 102/min, a respiratory rate of 20/min, and a body temperature 38.8°C (101.8°F). There is no rash on physical examination; he is found to have neck rigidity, confusion, and photophobia. There are no focal neurological deficits. A head CT is normal without mass or hydrocephalus. A lumbar puncture was performed and cerebrospinal fluid (CSF) is sent to analysis while ceftriaxone and vancomycin are started. Which of the following additional antimicrobials should be added in the management of this patient?
- A. Trimethoprim-sulfamethoxazole (TMP-SMX)
- B. Ampicillin (Correct Answer)
- C. Amphotericin
- D. Meropenem
- E. Clindamycin
Combination antimicrobial therapy Explanation: ***Ampicillin***
- This patient is a 62-year-old, indicating an increased risk for **Listeria monocytogenes** meningitis, which is typically susceptible to ampicillin.
- Given his age and presentation with **meningeal signs** and fever, empirical coverage for Listeria with ampicillin is crucial, especially before CSF culture results are known.
*Trimethoprim-sulfamethoxazole (TMP-SMX)*
- While TMP-SMX can cover Listeria, it is generally considered a **second-line agent** for severe infections like meningitis due to slower bactericidal activity and potential for higher rates of treatment failure compared to ampicillin.
- Ampicillin is the **preferred first-line treatment** for Listeria meningitis unless there is a specific contraindication.
*Amphotericin*
- Amphotericin is an **antifungal agent** used for fungal meningitis.
- Although fungemia can occur in immunocompromised individuals or those with indwelling catheters, the initial presentation with bacterial meningitis symptoms and absence of specific risk factors for fungal infection do not support its empirical use.
*Meropenem*
- Meropenem is a **carbapenem** with a broad spectrum of activity, including many gram-negative and gram-positive bacteria, and some anaerobes.
- While it has good CNS penetration and could cover some organisms like penicillin-resistant S. pneumoniae or gram-negative rods, it is not the primary empirical choice specifically for **Listeria monocytogenes**, and there's no indication for its broad-spectrum coverage over standard empirical therapy currently.
*Clindamycin*
- Clindamycin is primarily active against **gram-positive bacteria**, especially anaerobes and some staphylococci and streptococci.
- It has **poor penetration into the CNS** and is therefore not effective for meningitis treatment, especially for common bacterial pathogens or Listeria.
Combination antimicrobial therapy US Medical PG Question 9: A 51-year-old man is admitted to the hospital because of a 2-day history of fever, nausea, and abdominal pain. His temperature is 39.4°C (102.9°F) and pulse is 106/min. Physical examination shows tenderness in the right upper quadrant. Blood cultures grow nonhemolytic, gram-positive cocci that grow in hypertonic saline. Antibiotic sensitivity testing of the isolated organism shows that gentamicin has a minimum inhibitory concentration (MIC) of 16 μg/mL. The addition of ampicillin, which has an MIC of 2 μg/mL alone, decreases the MIC of gentamicin to 0.85 μg/mL. The decrease in the MIC of gentamicin with the addition of ampicillin is most likely due to which of the following mechanisms?
- A. Increase in the intracellular uptake of gentamicin (Correct Answer)
- B. Sequential block of essential micronutrient synthesis
- C. Inhibition of the acetylation of gentamicin
- D. Additive bacteriostatic effect of ampicillin
- E. Stabilization of gentamicin binding at the target site
Combination antimicrobial therapy Explanation: ***Increase in the intracellular uptake of gentamicin***
- This scenario describes **synergism**, where ampicillin (a cell wall synthesis inhibitor) damages the bacterial cell wall, allowing better penetration of gentamicin (an aminoglycoside) into the cell. Aminoglycosides require **active transport** across the bacterial cell membrane, which is enhanced by cell wall disruption.
- The significant reduction in gentamicin's MIC when combined with ampicillin demonstrates that ampicillin facilitates gentamicin's access to its **ribosomal target**, leading to a more potent bactericidal effect.
*Sequential block of essential micronutrient synthesis*
- **Sequential block** typically refers to the synergistic action of drugs like trimethoprim and sulfamethoxazole, which inhibit different steps in the **folic acid synthesis pathway**.
- This mechanism is not directly applicable to the combination of a cell wall inhibitor and an aminoglycoside, which target different cellular processes.
*Inhibition of the acetylation of gentamicin*
- **Acetylation** is a common mechanism of aminoglycoside inactivation by bacterial enzymes (aminoglycoside-modifying enzymes).
- Ampicillin does not primarily work by inhibiting these enzymes; its main action is on **peptidoglycan synthesis** in the bacterial cell wall.
*Additive bacteriostatic effect of ampicillin*
- Ampicillin is a **bactericidal antibiotic** that works by inhibiting cell wall synthesis, not typically bacteriostatic in its primary action, especially against susceptible organisms.
- The dramatic drop in gentamicin's MIC suggests more than just an additive bacteriostatic effect; it indicates a **synergistic interaction** leading to enhanced bactericidal activity.
*Stabilization of gentamicin binding at the target site*
- Gentamicin binds to the bacterial **30S ribosomal subunit**, inhibiting protein synthesis.
- Ampicillin's mechanism of action is on the **bacterial cell wall**, and it does not directly stabilize the binding of gentamicin to the ribosome. Its role is to facilitate gentamicin's entry into the cell.
Combination antimicrobial therapy US Medical PG Question 10: A drug that inhibits mRNA synthesis has the well-documented side effect of red-orange body fluids. For which of the following is this drug used as monotherapy?
- A. Brucellosis
- B. Tuberculosis
- C. Methicillin-resistant staphylococcus aureus infection
- D. Mycobacterium avium intracellulare infection
- E. Neisseria meningitidis prophylaxis (Correct Answer)
Combination antimicrobial therapy Explanation: ***Neisseria meningitidis prophylaxis***
- The drug described is **rifampin**, which inhibits bacterial **DNA-dependent RNA polymerase**, thereby blocking **mRNA synthesis** and causes characteristic **red-orange discoloration of body fluids** (tears, urine, sweat).
- Rifampin is used as **monotherapy** for **prophylaxis** against **Neisseria meningitidis** infection in close contacts of infected patients.
- This is the **only indication** where rifampin monotherapy is appropriate, as prophylaxis requires short-term use where resistance development is not a concern.
*Tuberculosis*
- Rifampin is a **first-line agent** for tuberculosis treatment and a cornerstone of all TB regimens.
- However, it is **never used as monotherapy** for TB due to rapid development of resistance.
- Standard TB treatment requires **multidrug therapy** with rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) for initial phase.
*Methicillin-resistant Staphylococcus aureus infection*
- Rifampin is sometimes used in **combination** with other antibiotics (e.g., vancomycin, daptomycin) to treat **MRSA infections**, especially those involving **prosthetic devices** or **biofilms**.
- It is **not used as monotherapy** for active MRSA infections due to extremely high rates of spontaneous resistance.
*Mycobacterium avium intracellulare infection*
- **Mycobacterium avium complex (MAC)** infections require a multidrug regimen, typically including **macrolides (azithromycin or clarithromycin)**, **ethambutol**, and sometimes **rifabutin** (a rifamycin derivative preferred over rifampin).
- **Monotherapy is never appropriate** for MAC infections due to resistance concerns and treatment failure.
*Brucellosis*
- **Brucellosis** treatment requires **combination therapy**, typically **doxycycline plus rifampin** for 6 weeks or longer.
- **Rifampin monotherapy** is inadequate for eradicating Brucella infection and leads to treatment failure and resistance development.
More Combination antimicrobial therapy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.