Antimicrobial toxicities US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antimicrobial toxicities. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antimicrobial toxicities US Medical PG Question 1: You are taking care of a patient with renal failure secondary to anti-fungal therapy. The patient is a 66-year-old male being treated for cryptococcal meningitis. This drug has a variety of known side effects including acute febrile reactions to infusions, anemia, hypokalemia and hypomagnesemia. What is the mechanism of action of this drug?
- A. Inhibition of squalene epoxidase
- B. Binding of the 50S subunit
- C. Pore formation secondary to ergosterol binding (Correct Answer)
- D. Disruption of microtubule formation
- E. Inhibition of 1,3-beta-glucan synthase
Antimicrobial toxicities Explanation: ***Pore formation secondary to ergosterol binding***
- This describes the mechanism of action of **amphotericin B**, the antifungal agent used for cryptococcal meningitis.
- Amphotericin B binds to **ergosterol** in the fungal cell membrane, leading to the formation of pores, disruption of membrane integrity, and ultimately cell death.
- The side effects described—**nephrotoxicity with renal failure, hypokalemia, and hypomagnesemia**—are classic adverse effects of amphotericin B due to its effect on renal tubular cells and electrolyte wasting.
*Inhibition of squalene epoxidase*
- This is the mechanism of action for **terbinafine**, an antifungal primarily used for dermatophyte infections (e.g., onychomycosis), not systemic infections like cryptococcal meningitis.
- Terbinafine inhibits ergosterol synthesis at an earlier step but does not cause the severe nephrotoxicity and electrolyte disturbances described.
*Binding of the 50S subunit*
- This mechanism of action is characteristic of **macrolide antibiotics** like azithromycin or clarithromycin, which are antibacterial agents, not antifungals.
- These drugs inhibit bacterial protein synthesis and are ineffective against fungal infections.
*Disruption of microtubule formation*
- This is the mechanism of action for **griseofulvin**, an antifungal drug used for dermatophyte infections of the skin, hair, and nails.
- Griseofulvin interferes with fungal cell division and is not used for life-threatening systemic infections like cryptococcal meningitis.
*Inhibition of 1,3-beta-glucan synthase*
- This mechanism is associated with **echinocandins** (e.g., caspofungin, micafungin), which inhibit fungal cell wall synthesis.
- While echinocandins are used for some systemic fungal infections (particularly Candida and Aspergillus), they do not typically cause the severe renal failure and electrolyte disturbances characteristic of amphotericin B.
Antimicrobial toxicities US Medical PG Question 2: You are seeing a patient in clinic who recently started treatment for active tuberculosis. The patient is currently being treated with rifampin, isoniazid, pyrazinamide, and ethambutol. The patient is not used to taking medicines and is very concerned about side effects. Specifically regarding the carbohydrate polymerization inhibiting medication, which of the following is a known side effect?
- A. Vision loss (Correct Answer)
- B. Paresthesias of the hands and feet
- C. Cutaneous flushing
- D. Arthralgias
- E. Elevated liver enzymes
Antimicrobial toxicities Explanation: ***Vision loss***
- The "carbohydrate polymerization inhibiting medication" refers to **ethambutol**, which inhibits **arabinosyl transferase** (involved in mycobacterial cell wall arabinogalactan synthesis)
- **Ethambutol** causes **optic neuritis**, leading to **decreased visual acuity**, **red-green color blindness**, and potentially **irreversible vision loss**
- **Regular ophthalmologic monitoring** is essential during ethambutol therapy
*Paresthesias of the hands and feet*
- This describes **peripheral neuropathy** caused by **isoniazid**
- Isoniazid interferes with **pyridoxine (vitamin B6) metabolism**, leading to neurotoxicity
- Risk factors include malnutrition, diabetes, alcoholism, and pregnancy
- Prevented by **pyridoxine supplementation**
*Cutaneous flushing*
- Not a characteristic side effect of first-line anti-tuberculosis medications
- More commonly associated with niacin or certain allergic/vasodilatory reactions
*Arthralgias*
- Classic side effect of **pyrazinamide**, often affecting small joints
- Caused by **pyrazinamide-induced hyperuricemia** (inhibits renal uric acid excretion)
- May require dose adjustment or discontinuation if severe
*Elevated liver enzymes*
- **Hepatotoxicity** can occur with **rifampin**, **isoniazid**, and **pyrazinamide**
- Requires regular monitoring of liver function tests during TB treatment
- Most common serious adverse effect of combination TB therapy
Antimicrobial toxicities US Medical PG Question 3: An 8-year-old girl is brought to the emergency department because of a 2-day history of low-grade fever, itchy rash, and generalized joint pain. The rash initially started in the antecubital and popliteal fossae and then spread to her trunk and distal extremities. One week ago, she was diagnosed with acute sinusitis and was started on amoxicillin. She has no history of adverse drug reactions and immunizations are up-to-date. Her temperature is 37.5°C (99.5°F), pulse is 90/min, and blood pressure is 110/70 mm Hg. Physical examination shows periorbital edema and multiple erythematous, annular plaques of variable sizes over her entire body. One of the lesions in the right popliteal fossa has an area of central clearing and the patient's mother reports that it has been present for over 24 hours. Urinalysis is normal. Which of the following is the most likely diagnosis?
- A. Stevens-Johnson syndrome
- B. Pemphigus vulgaris
- C. Drug reaction with eosinophilia and systemic symptoms
- D. Serum sickness-like reaction (Correct Answer)
- E. IgA vasculitis
Antimicrobial toxicities Explanation: ***Serum sickness-like reaction***
- The patient's symptoms, including **low-grade fever, itchy rash (urticarial or morbilliform), generalized joint pain (arthralgia)**, and **periorbital edema**, developing about a week after starting **amoxicillin**, are classic for a serum sickness-like reaction. This reaction is often triggered by **beta-lactam antibiotics** in children.
- The presence of **annular plaques with central clearing** (targetoid lesions) and the 24-hour duration of lesions further supports this diagnosis, as these are common cutaneous manifestations.
*Stevens-Johnson syndrome*
- SJS is characterized by **extensive epidermal necrosis and detachment**, often involving **mucous membranes (oral, ocular, genital)**, which are not described in this patient.
- The rash in SJS typically consists of irregular, dusky red or purple macules and plaques with blistering, evolving into significant skin sloughing, unlike the described annular, itchy plaques.
*Pemphigus vulgaris*
- Pemphigus vulgaris is an **autoimmune blistering disease** causing flaccid bullae and erosions on the skin and mucous membranes. It is not associated with acute drug exposure.
- The patient's rash is described as itchy, erythematous, annular plaques, without mention of flaccid blisters or extensive erosions typical of pemphigus vulgaris.
*Drug reaction with eosinophilia and systemic symptoms*
- **DRESS syndrome** typically presents with a more severe and widespread morbilliform rash, often with **facial edema**, along with systemic symptoms such as **lymphadenopathy, hepatitis, nephritis, and eosinophilia**, which are not indicated in this case (normal urinalysis).
- The onset of DRESS syndrome is usually **2-6 weeks** after drug exposure, which is longer than the 1-week interval presented here.
*IgA vasculitis*
- **IgA vasculitis (Henoch-Schönlein purpura)** characteristically presents with **palpable purpura**, particularly on the lower extremities and buttocks, often accompanied by **arthralgia, abdominal pain, and renal involvement (hematuria/proteinuria)**.
- While arthritis and rash are present, the rash is described as erythematous, annular, and itchy, rather than the non-blanching palpable purpura typical of IgA vasculitis, and urinalysis is normal, ruling out renal involvement.
Antimicrobial toxicities US Medical PG Question 4: Ten days after being discharged from the hospital, a 42-year-old man comes to the emergency department because of reduced urine output for 3 days. Physical examination is normal. Serum creatinine concentration is 2.9 mg/dL. Urinalysis shows brownish granular casts and 2+ proteinuria. Renal biopsy shows patchy necrosis of the proximal convoluted tubule with sloughing of tubular cells into the lumen and preservation of tubular basement membranes. Administration of which of the following drugs during this patient's hospitalization is most likely the cause of the observed decrease in renal function?
- A. Aspirin
- B. Acyclovir
- C. Omeprazole
- D. Captopril
- E. Gentamicin (Correct Answer)
Antimicrobial toxicities Explanation: ***Gentamicin***
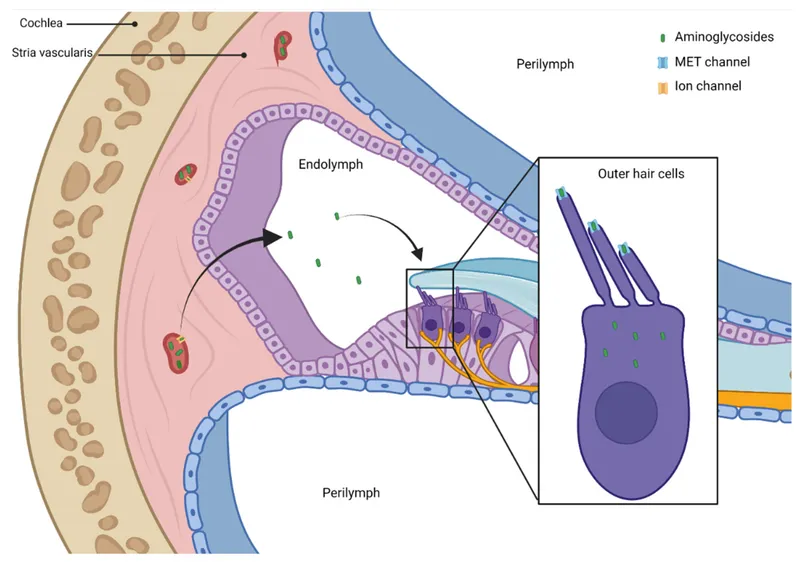
- The patient's presentation with **acute kidney injury** (reduced urine output, elevated creatinine) and characteristic urinalysis findings (**brownish granular casts**, proteinuria) points to **acute tubular necrosis (ATN)**.
- **Gentamicin** is an **aminoglycoside antibiotic** well-known for causing ATN, particularly with prolonged use or in susceptible patients. The biopsy findings of **patchy necrosis of the proximal convoluted tubule** and **sloughing of tubular cells** with preserved basement membranes are classic for ATN.
*Aspirin*
- **Aspirin**, especially at high doses or in sensitive individuals, can cause **analgesic nephropathy** (chronic interstitial nephritis) or, less commonly, acute interstitial nephritis.
- It does not typically cause ATN with the specific biopsy findings described, and its primary renal toxicity is often related to **prostaglandin inhibition**.
*Acyclovir*
- **Acyclovir** can cause acute kidney injury, but it primarily does so through **crystalluria** and **tubular obstruction**, leading to acute interstitial nephritis or acute kidney injury due to crystal deposition.
- The biopsy findings described (patchy tubular necrosis, sloughing cells) are not typical for acyclovir-induced nephrotoxicity.
*Omeprazole*
- **Omeprazole**, a proton pump inhibitor, is most commonly associated with **acute interstitial nephritis (AIN)**, an allergic reaction affecting the renal interstitium.
- AIN would typically present with eosinophiluria, white blood cell casts, and interstitial inflammation on biopsy, rather than primary tubular necrosis.
*Captopril*
- **Captopril**, an ACE inhibitor, can cause acute kidney injury, particularly in patients with **renal artery stenosis** or volume depletion, by altering glomerular hemodynamics.
- It typically does not cause direct tubular necrosis or the specific histological changes seen in ATN; rather, it primarily reduces **glomerular filtration pressure**.
Antimicrobial toxicities US Medical PG Question 5: A 77-year-old woman is brought to the emergency department from her nursing home because she was found down overnight. On presentation she was found to be delirious and was unable to answer questions. Chart review shows that she is allergic to cephalosporins. Her temperature is 102.2°F (39°C), blood pressure is 105/52 mmHg, pulse is 94/min, and respirations are 23/min. Physical exam reveals a productive cough. A metabolic panel is obtained with the following results:
Serum:
Na+: 135 mEq/L
Cl-: 95 mEq/L
K+: 4 mEq/L
HCO3-: 19 mEq/L
BUN: 40 mg/dL
Creatinine: 2.5 mg/dL
Glucose: 150 mg/dL
Based on these findings two different drugs are started empirically. Gram stain on a blood sample is performed showing the presence of gram-positive organisms on all samples. One of the drugs is subsequently stopped. The drug that was most likely stopped has which of the following characteristics?
- A. Resistance conveyed through acetylation
- B. Associated with red man syndrome
- C. Single-ringed ß-lactam structure (Correct Answer)
- D. Causes discolored teeth in children
- E. Accumulates inside bacteria via O2-dependent uptake
Antimicrobial toxicities Explanation: ***Single-ringed ß-lactam structure***
- The patient presents with **sepsis** due to **pneumonia** likely caused by **gram-positive organisms**. Given a cephalosporin allergy, **aztreonam** (a monobactam) would be an initial empirical antibiotic choice to cover gram-negative bacteria, alongside a drug for gram-positive coverage (like vancomycin).
- Since the **blood cultures** confirmed **gram-positive organisms**, the drug covering gram-negative bacteria (aztreonam) would be stopped. Aztreonam is characterized by its **single-ringed β-lactam structure**.
*Resistance conveyed through acetylation*
- This mechanism of resistance is typical of **aminoglycosides** (e.g., gentamicin) and **chloramphenicol**.
- Aminoglycosides were unlikely to be one of the empirically started drugs, as they are often used in combination with β-lactams, and this patient has a cephalosporin allergy.
*Associated with red man syndrome*
- **Red man syndrome** is a common adverse effect associated with **vancomycin** administration, especially with rapid infusion.
- Vancomycin would likely be continued, as it effectively targets gram-positive organisms, including **MRSA**, and is a suitable alternative given the cephalosporin allergy.
*Causes discolored teeth in children*
- This is a characteristic side effect of **tetracyclines** (e.g., doxycycline), which are contraindicated in young children and pregnant women due to their effects on bone and teeth development.
- Tetracyclines are not typically first-line empiric therapy for severe pneumonia or sepsis, especially in an elderly patient.
*Accumulates inside bacteria via O2-dependent uptake*
- This describes the mechanism of uptake for **aminoglycosides**. Their entry into bacteria is an **energy-dependent process** requiring oxygen.
- As mentioned, aminoglycosides are less likely to be the initial drug stopped in this scenario, as they target gram-negative bacteria.
Antimicrobial toxicities US Medical PG Question 6: A 3-year-old boy is brought to the physician because of a 3-day history of a pruritic skin rash on his chest. His mother says that he has no history of dermatological problems. He was born at term and has been healthy except for recurrent episodes of otitis media. His immunizations are up-to-date. He appears pale. His temperature is 37°C (98.6°F), pulse is 110/min, respirations are 26/min, and blood pressure is 102/62 mm Hg. Examination shows vesicles and flaccid bullae with thin brown crusts on the chest. Lateral traction of the surrounding skin leads to sloughing. Examination of the oral mucosa shows no abnormalities. Complete blood count is within the reference range. Which of the following is the most likely diagnosis?
- A. Bullous pemphigoid
- B. Dermatitis herpetiformis
- C. Bullous impetigo (Correct Answer)
- D. Pemphigus vulgaris
- E. Stevens-Johnson syndrome
Antimicrobial toxicities Explanation: ***Bullous impetigo***
- The presence of **flaccid bullae with thin brown crusts** and the positive **Nikolsky's sign** (sloughing with lateral traction), in the absence of mucosal involvement, are classic signs of bullous impetigo, a **Staphylococcus aureus** infection.
- This condition is common in children and can present with localized lesions, as seen on the chest.
*Bullous pemphigoid*
- Typically presents with **tense bullae** in older adults, often with **urticarial plaques**, unlike the flaccid bullae and crusts seen here.
- **Nikolsky's sign is negative** in bullous pemphigoid, which helps distinguish it from bullous impetigo and pemphigus conditions.
*Dermatitis herpetiformis*
- Characterized by intensely **pruritic papules and vesicles** found symmetrically on extensor surfaces, often associated with **celiac disease**.
- The lesions are usually small and grouped, not flaccid bullae with positive Nikolsky's sign.
*Pemphigus vulgaris*
- Presents with **flaccid bullae** and a positive Nikolsky's sign, but characteristically also involves the **oral mucosa**, which is normal in this patient.
- It usually affects older individuals and can be more widespread than the localized rash described.
*Stevens-Johnson syndrome*
- A severe mucocutaneous reaction typically characterized by **widespread epidermal necrosis**, **target lesions**, and often involves **mucous membranes** (oral, ocular, genital) extensively.
- This patient's localized rash without mucosal involvement, target lesions, or systemic toxicity does not fit the criteria for SJS.
Antimicrobial toxicities US Medical PG Question 7: A 23-year-old woman on prednisone for lupus presents to her primary care physician because she experiences a burning sensation with urination. She has also been urinating more frequently than normal. The patient denies fever, chills, nausea/vomiting, abdominal or back pain, or other changes with urination. Her vital signs and physical exam are unremarkable, and her urine analysis is positive for leukocyte esterase and nitrites. The patient receives a diagnosis and is then prescribed an antimicrobial that acts by inhibiting DNA gyrase. Which adverse effect should the patient be counseled about?
- A. Facial redness/flushing
- B. Tendon rupture (Correct Answer)
- C. Rhabdomyolysis
- D. Hemolytic anemia
- E. Leukopenia
Antimicrobial toxicities Explanation: ***Tendon rupture***
- The patient's symptoms (dysuria, frequent urination, positive leukocyte esterase, and nitrites) are consistent with a **urinary tract infection (UTI)**. The antimicrobial that inhibits **DNA gyrase** is a **fluoroquinolone**, and a well-known adverse effect of fluoroquinolones is **tendon rupture**.
- Risk factors for tendon rupture with fluoroquinolones include older age, corticosteroid use, and renal insufficiency, all of which are pertinent to this patient on **prednisone** for lupus.
*Facial redness/flushing*
- This is an adverse effect more commonly associated with drugs like **niacin** or calcium channel blockers, not fluoroquinolones.
- It is generally not a recognized side effect of antibiotics used to treat UTIs.
*Rhabdomyolysis*
- This serious condition involves the breakdown of muscle tissue and is associated with various drugs (e.g., statins, street drugs) and conditions (e.g., trauma, extreme exertion), but not typically fluoroquinolones.
- While muscle pain can occur with fluoroquinolones, severe rhabdomyolysis is rare.
*Hemolytic anemia*
- Certain antibiotics, like sulfonamides or penicillin, can rarely cause drug-induced hemolytic anemia, particularly in patients with **G6PD deficiency**.
- Fluoroquinolones are not commonly associated with hemolytic anemia.
*Leukopenia*
- While some antibiotics can cause bone marrow suppression leading to leukopenia (e.g., chloramphenicol, trimethoprim-sulfamethoxazole), this is not a common or significant adverse effect of fluoroquinolones.
- The patient's underlying lupus and prednisone use might contribute to immune dysregulation, but leukopenia is not the primary concern with fluoroquinolone use.
Antimicrobial toxicities US Medical PG Question 8: A 65-year-old man comes to the physician for a routine health maintenance examination. He feels well. His most recent examination 2 years ago included purified protein derivative (PPD) skin testing and showed no abnormalities. He is a retired physician and recently came back from rural China where he completed a voluntary service at a local healthcare center. A PPD skin test is performed. Three days later, an induration of 12 mm is noted. An x-ray of the chest shows no abnormalities. He is started on a drug that inhibits the synthesis of mycolic acid. This patient is at greatest risk of developing which of the following adverse effects?
- A. Cytochrome P-450 induction
- B. Hyperuricemia
- C. Liver injury (Correct Answer)
- D. Optic neuropathy
- E. Nephrotoxicity
Antimicrobial toxicities Explanation: ***Liver injury***
- The drug described is **isoniazid**, which inhibits **mycolic acid synthesis** and is first-line treatment for **latent tuberculosis infection**.
- **Isoniazid-induced hepatotoxicity** is the most significant adverse effect, with risk increasing dramatically in patients **>35 years old** (this patient is 65).
- Additional risk factors include alcohol use, pre-existing liver disease, and concurrent hepatotoxic medications.
- Patients should be monitored with baseline and periodic liver function tests.
*Cytochrome P-450 induction*
- **Rifampin**, not isoniazid, is a potent **CYP450 inducer** that decreases levels of many co-administered drugs.
- Isoniazid is actually a **CYP450 inhibitor** (inhibits CYP2C19, CYP3A4), which can increase levels of other drugs like phenytoin and warfarin.
*Hyperuricemia*
- **Pyrazinamide** is the anti-tuberculosis drug that causes **hyperuricemia** by inhibiting renal tubular secretion of uric acid.
- This can precipitate acute gout attacks in susceptible patients.
- Isoniazid does not affect uric acid metabolism.
*Optic neuropathy*
- **Ethambutol** causes dose-dependent **optic neuropathy**, presenting with decreased visual acuity and **red-green color blindness**.
- Patients on ethambutol require baseline and monthly visual assessments.
- Isoniazid is not associated with optic toxicity.
*Nephrotoxicity*
- **Aminoglycosides** (e.g., streptomycin) and some other antibiotics cause **nephrotoxicity** through tubular damage.
- Isoniazid is not significantly nephrotoxic and does not require renal dose adjustment.
Antimicrobial toxicities US Medical PG Question 9: A 42-year-old man is brought to the physician 25 minutes after an episode of violent jerky movements of his hands and legs that lasted for 5 minutes. After the episode, he had difficulty conversing. For the past 10 days, he has had a left-sided headache and nausea. Apart from a history of recurrent ear infections treated with antibiotics, he reports no other personal or family history of serious illness. He works as an assistant at a veterinarian clinic. He appears ill and is oriented to place and person only. His temperature is 37.8°C (100°F), pulse is 102/min, and blood pressure 112/78 mm Hg. Examination shows bilateral optic disc swelling. There is no lymphadenopathy. Muscle strength and tone is normal in all extremities. Deep tendon reflexes are 2+ bilaterally. Plantar reflex shows a flexor response bilaterally. Laboratory studies show a CD4 count within the reference range. An MRI of the brain is shown. Intravenous mannitol and levetiracetam are administered. Which of the following is the most appropriate next step in management?
- A. Aspiration and surgical drainage (Correct Answer)
- B. Pyrimethamine and sulfadiazine therapy
- C. Ciprofloxacin and metronidazole therapy
- D. Albendazole therapy
- E. Metronidazole and cefotaxime therapy
Antimicrobial toxicities Explanation: ***Aspiration and surgical drainage***
- The MRI shows a **ring-enhancing lesion** with surrounding edema, consistent with a **brain abscess**, indicated by the patient's symptoms (headache, nausea, seizures, fever, optic disc swelling from increased intracranial pressure) and history of ear infections.
- Due to the size of the lesion and the associated mass effect (seizures, altered mental status, papilledema), **surgical drainage** is crucial to relieve pressure, obtain a pathogen sample for targeted antibiotic therapy, and achieve rapid improvement, especially in cases where empiric antibiotics alone may not be sufficient or the abscess is large.
*Pyrimethamine and sulfadiazine therapy*
- This regimen is the primary treatment for **Toxoplasma gondii encephalitis**, which typically occurs in immunocompromised individuals (e.g., HIV with low CD4 count).
- The patient's **CD4 count is within the reference range**, making toxoplasmosis less likely, and the MRI appearance of a single, large ring-enhancing lesion is not as typical for multifocal toxoplasmosis.
*Ciprofloxacin and metronidazole therapy*
- While metronidazole is often used for anaerobic coverage in brain abscesses, ciprofloxacin is a broad-spectrum antibiotic but not the first-line choice for typical brain abscess pathogens originating from otitis media (e.g., Strep species, anaerobes).
- **Empiric antibiotic therapy** is typically initiated, but given the significant mass effect and neurological compromise, **surgical intervention is generally prioritized alongside antibiotics** for symptomatic abscesses.
*Albendazole therapy*
- **Albendazole** is an **anti-parasitic medication** used to treat infections like neurocysticercosis, which can present with ring-enhancing lesions.
- However, the patient's history (ear infections, no travel to endemic areas for neurocysticercosis) and the imaging characteristics (single, thick-walled cavity) make a bacterial abscess more probable.
*Metronidazole and cefotaxime therapy*
- This is a common **empiric antibiotic regimen for brain abscesses**, covering both anaerobic bacteria (metronidazole) and common streptococcal species (cefotaxime, a third-generation cephalosporin).
- While appropriate as medical therapy, given the patient's **acute neurological symptoms** (seizures, altered mental status from high intracranial pressure) and the size of the abscess on MRI, **surgical aspiration and drainage** are equally, if not more, important as an initial step to reduce mass effect and obtain cultures, rather than relying solely on antibiotics.
Antimicrobial toxicities US Medical PG Question 10: A research group wants to assess the safety and toxicity profile of a new drug. A clinical trial is conducted with 20 volunteers to estimate the maximum tolerated dose and monitor the apparent toxicity of the drug. The study design is best described as which of the following phases of a clinical trial?
- A. Phase 0
- B. Phase III
- C. Phase V
- D. Phase II
- E. Phase I (Correct Answer)
Antimicrobial toxicities Explanation: ***Phase I***
- **Phase I clinical trials** involve a small group of healthy volunteers (typically 20-100) to primarily assess **drug safety**, determine a safe dosage range, and identify side effects.
- The main goal is to establish the **maximum tolerated dose (MTD)** and evaluate the drug's pharmacokinetic and pharmacodynamic profiles.
*Phase 0*
- **Phase 0 trials** are exploratory studies conducted in a very small number of subjects (10-15) to gather preliminary data on a drug's **pharmacodynamics and pharmacokinetics** in humans.
- They involve microdoses, not intended to have therapeutic effects, and thus cannot determine toxicity or MTD.
*Phase III*
- **Phase III trials** are large-scale studies involving hundreds to thousands of patients to confirm the drug's **efficacy**, monitor side effects, compare it to standard treatments, and collect information that will allow the drug to be used safely.
- These trials are conducted after safety and initial efficacy have been established in earlier phases.
*Phase V*
- "Phase V" is not a standard, recognized phase in the traditional clinical trial classification (Phase 0, I, II, III, IV).
- This term might be used in some non-standard research contexts or for post-marketing studies that go beyond Phase IV surveillance, but it is not a formal phase for initial drug development.
*Phase II*
- **Phase II trials** involve several hundred patients with the condition the drug is intended to treat, focusing on **drug efficacy** and further evaluating safety.
- While safety is still monitored, the primary objective shifts to determining if the drug works for its intended purpose and at what dose.
More Antimicrobial toxicities US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.