Antimicrobial allergies and cross-reactivity US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antimicrobial allergies and cross-reactivity. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antimicrobial allergies and cross-reactivity US Medical PG Question 1: A 10-year-old boy presents with a painful rash for 1 day. He says that the reddish, purple rash started on his forearm but has now spread to his abdomen. He says there is a burning pain in the area where the rash is located. He also says he has had a stuffy nose for several days. Past medical history is significant for asthma and epilepsy, medically managed. Current medications are a daily chewable multivitamin, albuterol, budesonide, and lamotrigine. On physical examination, there is a red-purple maculopapular rash present on upper extremities and torso. There are some blisters present over the rash, as shown in the image, which is also present in the oral mucosa. Which of the following is the most likely cause of this patient’s symptoms?
- A. Multivitamin
- B. Budesonide
- C. Albuterol
- D. Lamotrigine (Correct Answer)
- E. Infection
Antimicrobial allergies and cross-reactivity Explanation: ***Lamotrigine***
- The patient's symptoms, including a **painful, rapidly spreading maculopapular rash** with **blisters** involving the skin and **oral mucosa**, are highly suggestive of **Stevens-Johnson Syndrome (SJS)** or **toxic epidermal necrolysis (TEN)**.
- **Lamotrigine** is a known medication commonly associated with SJS/TEN, especially when initiated or titrated rapidly.
*Multivitamin*
- **Multivitamins** are generally safe and are not known to cause severe dermatological reactions like SJS/TEN.
- While allergic reactions to specific components in multivitamins are possible, they are typically mild and do not present with widespread blistering rashes.
*Budesonide*
- **Budesonide** is an inhaled corticosteroid primarily used for asthma and is not associated with SJS/TEN.
- Corticosteroids are more commonly used *to treat* inflammatory skin conditions rather than cause them.
*Albuterol*
- **Albuterol** is a bronchodilator for asthma and is not a recognized cause of SJS/TEN.
- Adverse effects of albuterol are typically cardiac (e.g., tachycardia) or neurological (e.g., tremor).
*Infection*
- While some **infections** (e.g., *Mycoplasma pneumoniae*, herpes simplex virus) can trigger SJS, the abrupt onset of symptoms in a patient on a high-risk medication makes the drug the more likely primary cause.
- The "stuffy nose" could be an upper respiratory infection, which can sometimes precede SJS, but the distinctive rash and medication history strongly point to lamotrigine as the precipitating factor.
Antimicrobial allergies and cross-reactivity US Medical PG Question 2: An 8-year-old girl is brought to the emergency department because of a 2-day history of low-grade fever, itchy rash, and generalized joint pain. The rash initially started in the antecubital and popliteal fossae and then spread to her trunk and distal extremities. One week ago, she was diagnosed with acute sinusitis and was started on amoxicillin. She has no history of adverse drug reactions and immunizations are up-to-date. Her temperature is 37.5°C (99.5°F), pulse is 90/min, and blood pressure is 110/70 mm Hg. Physical examination shows periorbital edema and multiple erythematous, annular plaques of variable sizes over her entire body. One of the lesions in the right popliteal fossa has an area of central clearing and the patient's mother reports that it has been present for over 24 hours. Urinalysis is normal. Which of the following is the most likely diagnosis?
- A. Stevens-Johnson syndrome
- B. Pemphigus vulgaris
- C. Drug reaction with eosinophilia and systemic symptoms
- D. Serum sickness-like reaction (Correct Answer)
- E. IgA vasculitis
Antimicrobial allergies and cross-reactivity Explanation: ***Serum sickness-like reaction***
- The patient's symptoms, including **low-grade fever, itchy rash (urticarial or morbilliform), generalized joint pain (arthralgia)**, and **periorbital edema**, developing about a week after starting **amoxicillin**, are classic for a serum sickness-like reaction. This reaction is often triggered by **beta-lactam antibiotics** in children.
- The presence of **annular plaques with central clearing** (targetoid lesions) and the 24-hour duration of lesions further supports this diagnosis, as these are common cutaneous manifestations.
*Stevens-Johnson syndrome*
- SJS is characterized by **extensive epidermal necrosis and detachment**, often involving **mucous membranes (oral, ocular, genital)**, which are not described in this patient.
- The rash in SJS typically consists of irregular, dusky red or purple macules and plaques with blistering, evolving into significant skin sloughing, unlike the described annular, itchy plaques.
*Pemphigus vulgaris*
- Pemphigus vulgaris is an **autoimmune blistering disease** causing flaccid bullae and erosions on the skin and mucous membranes. It is not associated with acute drug exposure.
- The patient's rash is described as itchy, erythematous, annular plaques, without mention of flaccid blisters or extensive erosions typical of pemphigus vulgaris.
*Drug reaction with eosinophilia and systemic symptoms*
- **DRESS syndrome** typically presents with a more severe and widespread morbilliform rash, often with **facial edema**, along with systemic symptoms such as **lymphadenopathy, hepatitis, nephritis, and eosinophilia**, which are not indicated in this case (normal urinalysis).
- The onset of DRESS syndrome is usually **2-6 weeks** after drug exposure, which is longer than the 1-week interval presented here.
*IgA vasculitis*
- **IgA vasculitis (Henoch-Schönlein purpura)** characteristically presents with **palpable purpura**, particularly on the lower extremities and buttocks, often accompanied by **arthralgia, abdominal pain, and renal involvement (hematuria/proteinuria)**.
- While arthritis and rash are present, the rash is described as erythematous, annular, and itchy, rather than the non-blanching palpable purpura typical of IgA vasculitis, and urinalysis is normal, ruling out renal involvement.
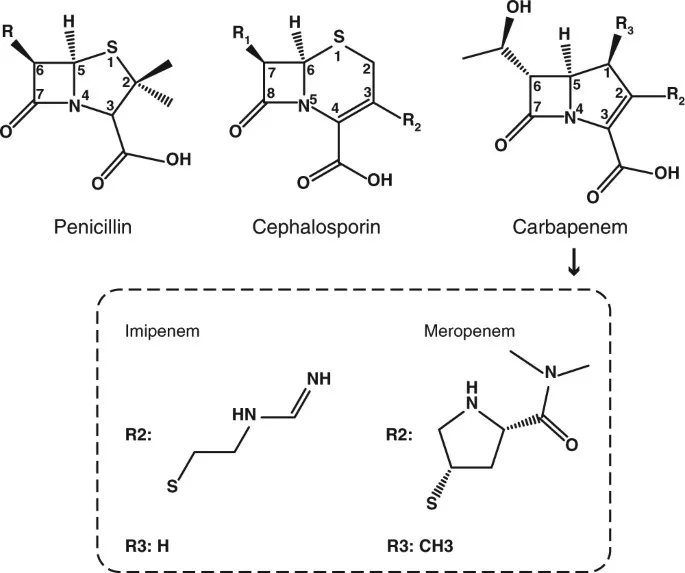
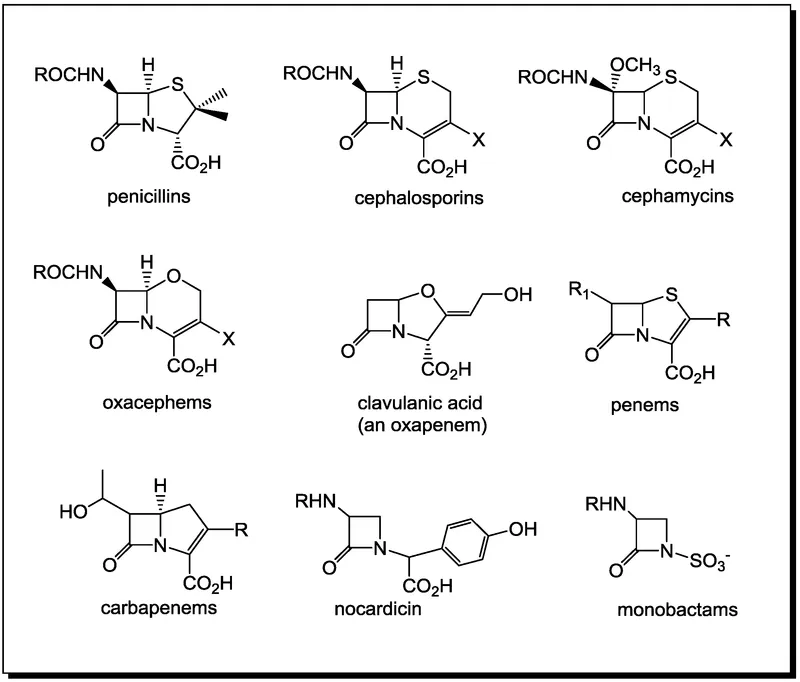
Antimicrobial allergies and cross-reactivity US Medical PG Question 3: An investigator is studying the chemical structure of antibiotics and its effect on bacterial growth. He has synthesized a simple beta-lactam antibiotic and has added a bulky side chain to the molecule that inhibits the access of bacterial enzymes to the beta-lactam ring. The synthesized drug will most likely be appropriate for the treatment of which of the following conditions?
- A. Folliculitis (Correct Answer)
- B. Nocardiosis
- C. Atypical pneumonia
- D. Erythema migrans
- E. Otitis media
Antimicrobial allergies and cross-reactivity Explanation: ***Folliculitis***
- The bulky side chain provides **steric hindrance** that prevents **staphylococcal beta-lactamases** from accessing and degrading the **beta-lactam ring**.
- This modification creates an **anti-staphylococcal penicillin** (similar to methicillin, nafcillin, or oxacillin), which is effective against **methicillin-sensitive *Staphylococcus aureus* (MSSA)**.
- **Folliculitis** is most commonly caused by *S. aureus*, making this modified beta-lactam an appropriate treatment choice for MSSA-related folliculitis.
- The bulky side chain specifically protects against the **penicillinase** (beta-lactamase) produced by staphylococci.
*Otitis media*
- Otitis media is commonly caused by beta-lactamase-producing organisms like *Haemophilus influenzae* and *Moraxella catarrhalis*.
- However, the beta-lactamases produced by these gram-negative organisms are **not inhibited by bulky side chains** alone.
- Treatment of beta-lactamase-producing *H. influenzae* and *M. catarrhalis* requires **beta-lactamase inhibitors** (such as clavulanic acid combined with amoxicillin), not steric hindrance.
- The mechanism of protection differs: beta-lactamase inhibitors **suicide inhibitors** that bind to the enzyme, whereas bulky side chains provide **physical blocking**.
*Nocardiosis*
- Nocardiosis is caused by *Nocardia* species, which are **aerobic actinomycetes**.
- These bacteria are typically treated with **sulfonamides** (trimethoprim-sulfamethoxazole) for prolonged periods.
- Beta-lactam antibiotics are generally not first-line treatment, as *Nocardia* species often show intrinsic resistance or require specific antibiotic combinations.
*Atypical pneumonia*
- Atypical pneumonia is caused by organisms like *Mycoplasma pneumoniae*, *Chlamydophila pneumoniae*, and *Legionella pneumophila*.
- These organisms lack a **peptidoglycan cell wall**, which is the target of all **beta-lactam antibiotics**.
- Beta-lactams (regardless of modifications) are completely ineffective against atypical pneumonia pathogens.
- Treatment requires **macrolides** (azithromycin), **tetracyclines** (doxycycline), or **fluoroquinolones**.
*Erythema migrans*
- Erythema migrans is the characteristic rash of early **Lyme disease**, caused by *Borrelia burgdorferi*.
- While *Borrelia* is sensitive to certain beta-lactam antibiotics (amoxicillin, ceftriaxone), it does **not produce beta-lactamases**.
- The bulky side chain modification is unnecessary for treating *Borreria* infections, as there is no beta-lactamase to protect against.
- Standard treatment uses doxycycline, amoxicillin, or ceftriaxone—not anti-staphylococcal penicillins.
Antimicrobial allergies and cross-reactivity US Medical PG Question 4: A 42-year-old homeless man presents to the emergency department complaining of pain in his right knee and fever. The patient is having difficulty walking and looks visibly uncomfortable. On examination, he is disheveled but his behavior is not erratic. The patient’s right knee is erythematous, edematous, and warm, with evidence of a 3 cm wound that is weeping purulent fluid. The patient has a decreased range of motion secondary to pain and swelling. The wound is cultured and empiric antibiotic therapy is initiated. Four minutes into the patient’s antibiotic therapy, he develops a red, pruritic rash on his face and neck. What is the most likely antibiotic this patient is being treated with?
- A. Gentamicin
- B. Linezolid
- C. Penicillin G
- D. Erythromycin
- E. Vancomycin (Correct Answer)
Antimicrobial allergies and cross-reactivity Explanation: ***Vancomycin***
- The rapid development of a **red, pruritic rash** on the face and neck shortly after starting antibiotic therapy for a systemic infection (likely **septic arthritis** given the symptoms) is highly characteristic of **Red Man Syndrome**.
- **Red Man Syndrome** is a pseudoallergic reaction caused by rapid infusion of **vancomycin**, leading to **histamine release**.
*Gentamicin*
- **Gentamicin** is an aminoglycoside antibiotic used for gram-negative infections, but it is not typically associated with a rapid-onset facial rash.
- Its primary adverse effects include **ototoxicity** and **nephrotoxicity**, which develop with prolonged use rather than acute infusion.
*Linezolid*
- **Linezolid** is an oxazolidinone antibiotic primarily used for resistant gram-positive bacteria like MRSA.
- While it can cause side effects like **myelosuppression** and **serotonin syndrome** (if co-administered with serotonergic drugs), it does not typically cause a rapid, prominent facial rash.
*Penicillin G*
- **Penicillin G** is a beta-lactam antibiotic that can cause allergic reactions, but these are typically **IgE-mediated hypersensitivity reactions** (e.g., anaphylaxis, urticaria, angioedema) and less commonly present as a specific "red man" flush.
- The rash associated with penicillin allergy is usually a more widespread **maculopapular rash** or urticaria, not localized to the face and neck in this specific fashion minutes after administration.
*Erythromycin*
- **Erythromycin** is a macrolide antibiotic whose common side effects include **gastrointestinal upset** (e.g., nausea, vomiting, abdominal pain) and QT prolongation.
- It is not known to cause a rapid-onset, pruritic facial rash like the one described.
Antimicrobial allergies and cross-reactivity US Medical PG Question 5: A 77-year-old woman is brought to the emergency department from her nursing home because she was found down overnight. On presentation she was found to be delirious and was unable to answer questions. Chart review shows that she is allergic to cephalosporins. Her temperature is 102.2°F (39°C), blood pressure is 105/52 mmHg, pulse is 94/min, and respirations are 23/min. Physical exam reveals a productive cough. A metabolic panel is obtained with the following results:
Serum:
Na+: 135 mEq/L
Cl-: 95 mEq/L
K+: 4 mEq/L
HCO3-: 19 mEq/L
BUN: 40 mg/dL
Creatinine: 2.5 mg/dL
Glucose: 150 mg/dL
Based on these findings two different drugs are started empirically. Gram stain on a blood sample is performed showing the presence of gram-positive organisms on all samples. One of the drugs is subsequently stopped. The drug that was most likely stopped has which of the following characteristics?
- A. Resistance conveyed through acetylation
- B. Associated with red man syndrome
- C. Single-ringed ß-lactam structure (Correct Answer)
- D. Causes discolored teeth in children
- E. Accumulates inside bacteria via O2-dependent uptake
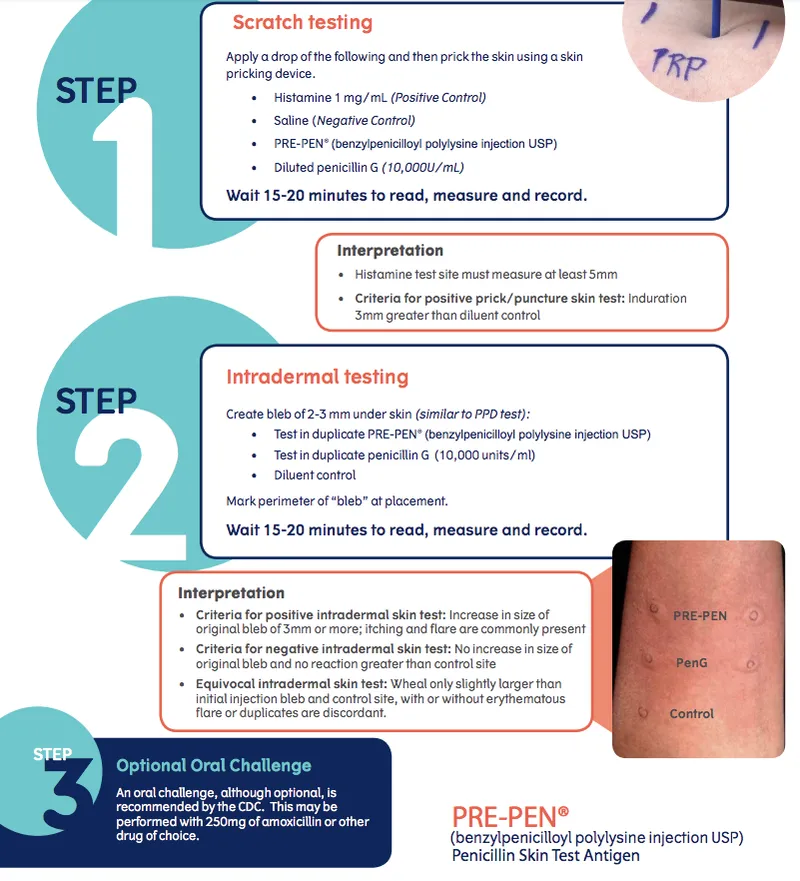
Antimicrobial allergies and cross-reactivity Explanation: ***Single-ringed ß-lactam structure***
- The patient presents with **sepsis** due to **pneumonia** likely caused by **gram-positive organisms**. Given a cephalosporin allergy, **aztreonam** (a monobactam) would be an initial empirical antibiotic choice to cover gram-negative bacteria, alongside a drug for gram-positive coverage (like vancomycin).
- Since the **blood cultures** confirmed **gram-positive organisms**, the drug covering gram-negative bacteria (aztreonam) would be stopped. Aztreonam is characterized by its **single-ringed β-lactam structure**.
*Resistance conveyed through acetylation*
- This mechanism of resistance is typical of **aminoglycosides** (e.g., gentamicin) and **chloramphenicol**.
- Aminoglycosides were unlikely to be one of the empirically started drugs, as they are often used in combination with β-lactams, and this patient has a cephalosporin allergy.
*Associated with red man syndrome*
- **Red man syndrome** is a common adverse effect associated with **vancomycin** administration, especially with rapid infusion.
- Vancomycin would likely be continued, as it effectively targets gram-positive organisms, including **MRSA**, and is a suitable alternative given the cephalosporin allergy.
*Causes discolored teeth in children*
- This is a characteristic side effect of **tetracyclines** (e.g., doxycycline), which are contraindicated in young children and pregnant women due to their effects on bone and teeth development.
- Tetracyclines are not typically first-line empiric therapy for severe pneumonia or sepsis, especially in an elderly patient.
*Accumulates inside bacteria via O2-dependent uptake*
- This describes the mechanism of uptake for **aminoglycosides**. Their entry into bacteria is an **energy-dependent process** requiring oxygen.
- As mentioned, aminoglycosides are less likely to be the initial drug stopped in this scenario, as they target gram-negative bacteria.
Antimicrobial allergies and cross-reactivity US Medical PG Question 6: A 13-year-old boy re-presents to his pediatrician with a new onset rash that began a few days after his initial visit. He initially presented with complaints of sore throat but was found to have a negative strep test. His mother demanded that he be placed on antibiotics, but this was refused by his pediatrician. The boy's father, a neurologist, therefore, started him on penicillin. Shortly after starting the drug, the boy developed a fever and a rash. The patient is admitted and his symptoms worsen. His skin begins to slough off, and the rash covers over 30% of his body. His oropharynx and corneal membranes are also affected. You examine him at the bedside and note a positive Nikolsky's sign. What is the most likely diagnosis?
- A. Erythema Multiforme
- B. Pemphigus Vulgaris
- C. Toxic Epidermal Necrolysis (Correct Answer)
- D. Rocky Mountain Spotted Fever
- E. Stevens-Johnson Syndrome
Antimicrobial allergies and cross-reactivity Explanation: **Toxic Epidermal Necrolysis**
- The rapid onset of a widespread, **sloughing rash** covering **over 30%** of the body surface area, involvement of **mucous membranes** (oropharynx, corneal), **fever**, and a **positive Nikolsky's sign** strongly indicate **Toxic Epidermal Necrolysis (TEN)**.
- TEN is most commonly triggered by **drugs**, and the boy's recent initiation of **penicillin** (an antibiotic) aligns with this etiology.
*Erythema Multiforme*
- Characterized by **target lesions** on the skin, often precipitated by infections (like herpes simplex virus) or drugs.
- While it can involve mucous membranes, it typically does not present with diffuse **epidermal sloughing** covering >30% of the body surface.
*Pemphigus Vulgaris*
- This is a chronic **autoimmune bullous disease** causing intraepidermal blistering, and a positive Nikolsky's sign is characteristic.
- However, it typically presents with more protracted disease course and is not usually triggered acutely by a drug in this manner; also, the widespread, rapid sloughing seen here is more characteristic of TEN.
*Rocky Mountain Spotted Fever*
- Presents with a **maculopapular rash** that typically starts on the extremities and spreads centrally, often involving palms and soles, following a tick bite.
- It does not cause widespread **epidermal necrosis** or a positive Nikolsky's sign.
*Stevens-Johnson Syndrome*
- SJS is indeed a severe mucocutaneous reaction, similar to TEN, often drug-induced, and involves mucous membranes and skin blistering with a positive Nikolsky's sign.
- The critical differentiating factor is the body surface area involvement: SJS affects **less than 10%** of the body surface, whereas TEN involves **over 30%**, as described in the patient.
Antimicrobial allergies and cross-reactivity US Medical PG Question 7: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Antimicrobial allergies and cross-reactivity Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Antimicrobial allergies and cross-reactivity US Medical PG Question 8: A 28-year-old man presents with painless anal ulcer. Dark-field microscopy shows spirochetes. He is allergic to penicillin with history of anaphylaxis. Which of the following is the most appropriate treatment?
- A. Erythromycin 500 mg four times daily for 14 days
- B. Penicillin desensitization followed by benzathine penicillin
- C. Doxycycline 100 mg orally twice daily for 14 days (Correct Answer)
- D. Azithromycin 2 g orally once
- E. Ceftriaxone 250 mg IM
Antimicrobial allergies and cross-reactivity Explanation: **Doxycycline 100 mg orally twice daily for 14 days**
- **Doxycycline** is the recommended alternative for treating **primary syphilis** in patients with a **penicillin allergy**, especially with a history of anaphylaxis.
- The 14-day duration for doxycycline is appropriate for treating early syphilis, including primary syphilis.
*Erythromycin 500 mg four times daily for 14 days*
- While erythromycin is an alternative, its efficacy for syphilis is **lower than doxycycline**, and it requires a longer duration of treatment.
- It is generally considered a less preferred option than doxycycline for penicillin-allergic patients due to adherence issues and potential for gastrointestinal side effects.
*Penicillin desensitization followed by benzathine penicillin*
- **Penicillin desensitization** is typically reserved for situations where penicillin is the **only truly effective treatment** and alternatives are not suitable, such as in neurosyphilis or syphilis in pregnancy.
- For primary syphilis in a non-pregnant patient with a clear anaphylactic allergy, an effective alternative like doxycycline is preferred over the risks associated with desensitization.
*Azithromycin 2 g orally once*
- **Azithromycin** resistance in *Treponema pallidum* is increasingly prevalent, making it an unreliable treatment for syphilis.
- A single dose is insufficient for effective treatment and carries a higher risk of treatment failure.
*Ceftriaxone 250 mg IM*
- **Ceftriaxone** is an alternative in some cases of syphilis, but the recommended dose for primary syphilis is typically higher and given for a longer duration (e.g., 1-2 g IM or IV daily for 10-14 days).
- A single 250 mg IM dose is insufficient for the treatment of syphilis and is more commonly used for gonorrhea.
Antimicrobial allergies and cross-reactivity US Medical PG Question 9: A 49-year-old man presents to the clinic for evaluation of puncture wounds on the dorsal aspect of his right second and third metacarpals. He states that he was in a fight 3 nights ago and he struck another individual in the mouth. The patient’s medical history is significant for peripheral vascular disease and hypertension. He takes aspirin, sulfasalazine, and lisinopril. He is allergic to penicillin. He drinks socially on weekends and smokes one and one-half packs of cigarettes daily. Vitals of the patient are as follows: blood pressure is 142/88 mm Hg; heart rate is 88/min; respiratory rate is 14/min; temperature is 38.9°C (102.1°F). On physical examination, the patient appears alert and oriented. His BMI is 33 kg/ m². His eyes are without scleral icterus. His right orbital region reveals ecchymosis along the superior and inferior borders. His heart is regular in rhythm and rate without murmurs. Capillary refill is 4 seconds in fingers and toes. His right dorsal second and third metacarpal region reveals two 3 mm lacerations with edema. Which of the following is the most appropriate management strategy for this patient?
- A. Irrigation and debridement
- B. Clindamycin plus doxycycline with irrigation and debridement (Correct Answer)
- C. Amoxicillin-clavulanate with irrigation and debridement
- D. Doxycycline with irrigation and debridement
- E. Azithromycin with irrigation and debridement
Antimicrobial allergies and cross-reactivity Explanation: **Clindamycin plus doxycycline with irrigation and debridement**
- This patient presents with a **"fight bite"** (puncture wounds from striking someone's mouth), which is a **high-risk injury for infection** due to the polymicrobial oral flora. The presence of **fever (38.9°C)**, **edema**, and increased **capillary refill time (4 seconds)** indicates an active infection.
- The recommended empirical antibiotic regimen for fight bites includes coverage for **aerobes** (e.g., *Staphylococcus aureus*, *Streptococcus spp.*, *Eikenella corrodens*) and **anaerobes**. **Clindamycin** provides excellent anaerobic coverage, and **doxycycline** or a fluoroquinolone can cover *Eikenella corrodens* and other aerobes, making this a suitable combination, especially given the patient's penicillin allergy. **Irrigation and debridement** are crucial for removing contaminants and necrotic tissue.
*Irrigation and debridement*
- While **irrigation and debridement** are essential steps in managing infected wounds, they are insufficient on their own for a high-risk infected "fight bite."
- **Antibiotic therapy** is also necessary to treat the infection and prevent its spread, especially given the signs of systemic involvement (fever).
*Amoxicillin-clavulanate with irrigation and debridement*
- **Amoxicillin-clavulanate** is a commonly recommended first-line antibiotic for fight bites due to its broad spectrum, including coverage of aerobes and anaerobes (including *Eikenella corrodens*).
- However, this patient has a **penicillin allergy**, making amoxicillin-clavulanate an inappropriate choice.
*Doxycycline with irrigation and debridement*
- **Doxycycline** covers *Eikenella corrodens* and some other aerobes, but it provides **insufficient coverage for anaerobes**, which are a significant component of oral flora involved in fight bite infections.
- Monotherapy with doxycycline would likely not be effective against the polymicrobial infection present.
*Azithromycin with irrigation and debridement*
- **Azithromycin** has good activity against some aerobes but provides **poor coverage against anaerobes** and *Eikenella corrodens*, making it an unsuitable empirical choice for a fight bite.
- It would not adequately address the polymicrobial nature of the infection.
Antimicrobial allergies and cross-reactivity US Medical PG Question 10: A 12-year-old girl is brought to the physician by her mother because of high fever and left ankle and knee joint swelling. She had a sore throat 3 weeks ago. There is no family history of serious illness. Her immunizations are up-to-date. She had an episode of breathlessness and generalized rash when she received dicloxacillin for a skin infection 2 years ago. She appears ill. Her temperature is 38.8°C (102.3°F), pulse is 87/min, and blood pressure is 98/62 mm Hg. Examination shows left ankle and knee joint swelling and tenderness; range of motion is limited. Breath sounds over both lungs are normal. A grade 3/6 holosytolic murmur is heard best at the apex. Abdominal examination is normal. Which of the following is the most appropriate pharmacotherapy?
- A. Amoxicillin
- B. Ciprofloxacin
- C. Clarithromycin (Correct Answer)
- D. Methotrexate
- E. High-dose glucocorticoids
Antimicrobial allergies and cross-reactivity Explanation: ***Clarithromycin***
- This patient presents with **acute rheumatic fever (ARF)** following pharyngitis, evidenced by polyarthritis (ankle and knee swelling) and carditis (holosystolic murmur at the apex indicating mitral regurgitation).
- The cornerstone of ARF treatment is **eradication of Streptococcus pyogenes** to prevent ongoing immune response and recurrent episodes.
- This patient has a **documented penicillin allergy** (previous reaction to dicloxacillin with breathlessness and rash), making penicillin-based antibiotics contraindicated.
- **Macrolides** (clarithromycin, azithromycin, erythromycin) are the **first-line alternative** for streptococcal eradication in penicillin-allergic patients.
- Anti-inflammatory therapy (aspirin for arthritis/mild carditis, or corticosteroids for severe carditis with heart failure) would also be initiated, but antibiotic therapy is the essential pharmacotherapy.
*Amoxicillin*
- Amoxicillin is a **beta-lactam antibiotic** and would typically be first-line for streptococcal eradication in ARF.
- However, this patient has a **documented penicillin allergy** (reaction to dicloxacillin), making amoxicillin **contraindicated** due to high cross-reactivity between penicillin derivatives.
- Using amoxicillin could precipitate anaphylaxis or severe allergic reaction.
*Ciprofloxacin*
- Ciprofloxacin is a **fluoroquinolone antibiotic** with poor activity against **Streptococcus pyogenes**, the causative organism of ARF.
- Fluoroquinolones are not indicated for streptococcal pharyngitis or ARF treatment.
- Use in children should be avoided when effective alternatives exist due to potential musculoskeletal side effects.
*Methotrexate*
- Methotrexate is a **disease-modifying antirheumatic drug (DMARD)** used for chronic inflammatory conditions like rheumatoid arthritis.
- It has **no role in acute rheumatic fever** management.
- Its slow onset of action and mechanism make it completely inappropriate for ARF.
*High-dose glucocorticoids*
- Glucocorticoids are reserved for **severe carditis with congestive heart failure** in ARF.
- This patient has carditis (murmur) but shows **no signs of heart failure** (normal breath sounds, no respiratory distress, stable vital signs).
- For arthritis and mild-moderate carditis, **aspirin or other NSAIDs** are preferred anti-inflammatory agents.
- Corticosteroids do NOT replace antibiotic therapy, which is the primary treatment to eradicate the streptococcal infection.
More Antimicrobial allergies and cross-reactivity US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.