Antimalarial medications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antimalarial medications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antimalarial medications US Medical PG Question 1: An investigator is studying growth patterns of various fungal pathogens. Incubation of an isolated fungus at 25°C shows branching hyphae with rosettes of conidia under light microscopy. After incubation at 37°C, microscopic examination of the same organism instead shows smooth, white colonies with rounded, elongated cells. Infection with the investigated pathogen is most likely to cause which of the following conditions?
- A. Pityriasis versicolor
- B. Candidiasis
- C. Cryptococcosis
- D. Sporotrichosis (Correct Answer)
- E. Coccidioidomycosis
Antimalarial medications Explanation: ***Sporotrichosis***
- The description of a fungal pathogen exhibiting **thermal dimorphism** (different forms at 25°C and 37°C) is characteristic of **Sporothrix schenckii**.
- At 25°C, it typically grows as **mold with branching hyphae and conidia in rosettes**, and at 37°C, it grows as **yeast-like cells (cigar-shaped bodies in tissue)**, which can appear rounded and elongated.
*Pityriasis versicolor*
- Caused by **Malassezia globosa**, which is a **lipophilic yeast** and does not exhibit thermal dimorphism described here.
- Characterized by **hypo- or hyperpigmented skin patches**, not deep tissue infection with dimorphic growth.
*Candidiasis*
- Caused by **Candida species**, which are **opportunistic yeasts** that can form pseudohyphae and true hyphae but do not display the specific dimorphism with rosettes of conidia at 25°C.
- Infections range from superficial mucocutaneous to systemic, but the fungal morphology described does not fit.
*Cryptococcosis*
- Caused by **Cryptococcus neoformans** or **Cryptococcus gattii**, which are **encapsulated yeasts** and do not exhibit dimorphism (mold at 25°C, yeast at 37°C).
- Primarily causes **meningoencephalitis** or pulmonary disease, and is identified by its capsule and yeast form.
*Coccidioidomycosis*
- Caused by **Coccidioides immitis** or **Coccidioides posadasii**, which are **thermally dimorphic fungi**, but their morphology differs from the description.
- At 25°C, they grow as molds with **arthroconidia**, and at 37°C, they form **spherules containing endospores** in tissue, not smooth, white colonies with rounded, elongated cells.
Antimalarial medications US Medical PG Question 2: A 32-year-old woman, gravida 2, para 1, at 20 weeks' gestation comes to the physician for a prenatal visit. She feels well. Her first pregnancy was uncomplicated and the child was delivered vaginally. Medications include folic acid and an iron supplement. Her temperature is 37°C (98.6°F), pulse is 98/min, respirations are 18/min, and blood pressure is 108/76 mm Hg. Abdominal examination shows a uterus that is consistent with a 20-week gestation. The second-trimester scan shows no abnormalities. The patient intends to travel next month to Mozambique to visit her grandmother. Which of the following drugs is most suitable for pre-exposure prophylaxis against malaria?
- A. Mefloquine (Correct Answer)
- B. Primaquine
- C. Chloroquine
- D. Doxycycline
- E. Proguanil
Antimalarial medications Explanation: ***Mefloquine***
- **Mefloquine** is the **most appropriate antimalarial prophylaxis** for pregnant women traveling to **chloroquine-resistant areas** such as Mozambique, particularly after the first trimester.
- Mozambique has **widespread chloroquine-resistant *P. falciparum* malaria**, making mefloquine the preferred choice according to CDC and WHO guidelines.
- While mefloquine is avoided in the first trimester due to limited safety data, it is considered **safe in the second and third trimesters** of pregnancy.
- Though neuropsychiatric side effects can occur, the benefits outweigh risks when traveling to high-risk malaria areas during pregnancy.
*Primaquine*
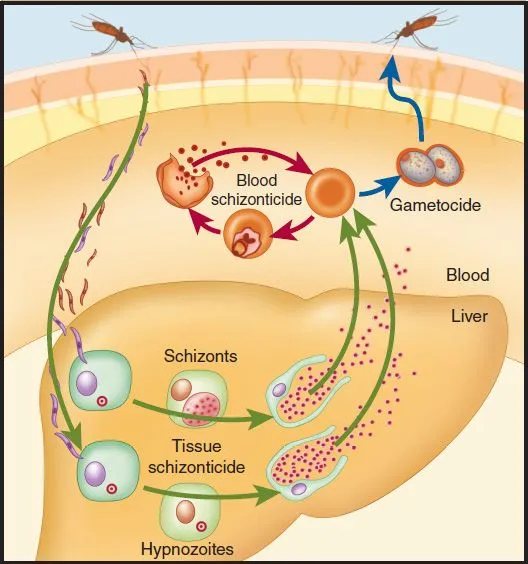
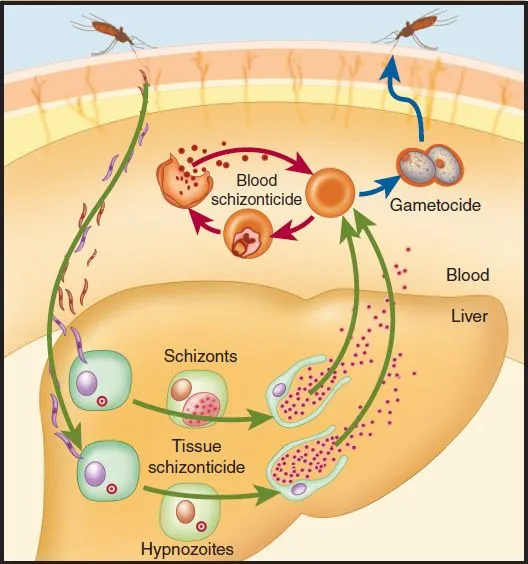
- **Primaquine** is *contraindicated* in pregnancy because it can cause **hemolytic anemia** in the fetus if the fetus has **glucose-6-phosphate dehydrogenase (G6PD) deficiency**.
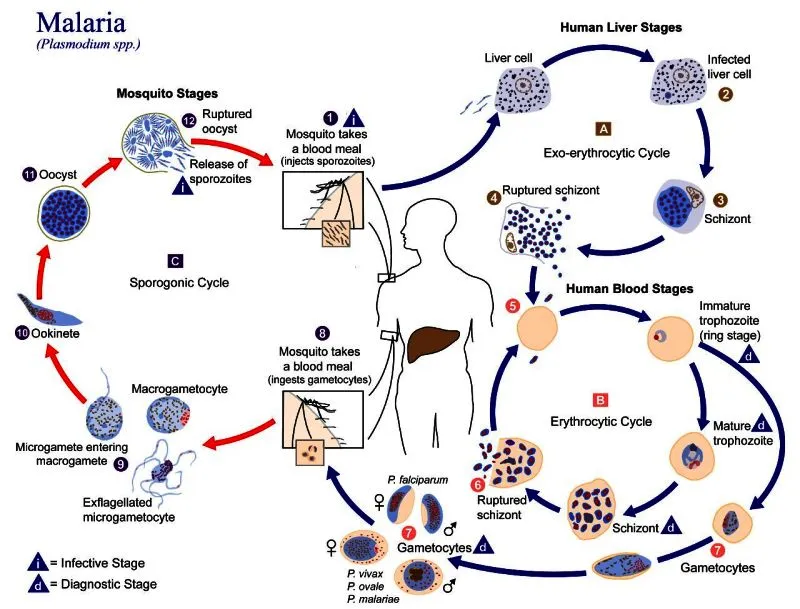
- It is used primarily for the **radical cure** of *P. vivax* and *P. ovale* malaria (to eradicate liver hypnozoites), not as a primary prophylactic agent.
*Chloroquine*
- While **chloroquine** is safe in pregnancy and preferred for **chloroquine-sensitive malaria** areas, it is *not appropriate for Mozambique*.
- Mozambique has **high rates of chloroquine-resistant *P. falciparum* malaria**, making chloroquine ineffective for prophylaxis in this region.
- Chloroquine would only be suitable for travel to areas with confirmed chloroquine-sensitive malaria (e.g., Central America west of Panama Canal, parts of the Middle East).
*Doxycycline*
- **Doxycycline** is *contraindicated* in pregnancy and in children under eight years old due to its potential to cause **permanent dental discoloration**, **enamel hypoplasia**, and inhibition of **bone growth** in the developing fetus.
*Proguanil*
- **Atovaquone-proguanil** (Malarone) has limited safety data in pregnancy and is generally not recommended as a first-line option when other proven alternatives are available.
- While some data suggest it may be safe, **mefloquine** is preferred for chloroquine-resistant areas during pregnancy due to more extensive safety documentation in the second and third trimesters.
Antimalarial medications US Medical PG Question 3: An 8-year-old boy is brought to the physician because of a 1-day history of severe left hand pain. He has had similar painful episodes in the past that required hospitalization. Physical examination shows pale conjunctivae. There is tenderness on palpation of the wrist and the small joints of the left hand. Peripheral blood smear shows crescent-shaped erythrocytes. He is started on a pharmacologic agent that is known to cause macrocytosis. This drug causes an arrest in which of the following cell cycle phases?
- A. S phase (Correct Answer)
- B. G0 phase
- C. G2 phase
- D. M phase
- E. G1 phase
Antimalarial medications Explanation: ***S phase***
- This patient presents with **sickle cell disease** given the history of recurrent severe pain episodes, pale conjunctivae (suggesting anemia), and **crescent-shaped erythrocytes** on peripheral blood smear.
- The pharmacologic agent that causes **macrocytosis** and is used in sickle cell disease is **hydroxyurea** through increasing **fetal hemoglobin**; it primarily works by inhibiting **ribonucleotide reductase**, an enzyme essential for **DNA synthesis**, thereby arresting cells in the **S phase**.
*G0 phase*
- The **G0 phase** is a resting phase where cells are not actively dividing or preparing to divide.
- Hydroxyurea targets rapidly dividing cells by interfering with DNA replication, so it does not primarily arrest cells in the inactive G0 phase.
*G2 phase*
- The **G2 phase** is the growth phase where the cell checks its DNA and prepares for mitosis.
- While hydroxyurea can indirectly affect the G2/M checkpoint, its direct mechanism of action is primarily in the S phase by preventing proper DNA synthesis.
*M phase*
- The **M phase** is the stage of cell division, including mitosis and cytokinesis.
- Drugs that block the M phase typically interfere with **microtubule formation** (e.g., vinca alkaloids, taxanes), which is not the primary mechanism of hydroxyurea.
*G1 phase*
- The **G1 phase** is the initial growth phase where the cell grows and synthesizes proteins.
- While cells must pass through G1 before entering S phase, hydroxyurea's direct DNA synthesis inhibition occurs during the S phase rather than preventing entry into S from G1.
Antimalarial medications US Medical PG Question 4: A 31-year-old woman presents to your office with one week of recurrent fevers. The highest temperature she recorded was 101°F (38.3°C). She recently returned from a trip to Nigeria to visit family and recalls a painful bite on her right forearm at that time. Her medical history is significant for two malarial infections as a child. She is not taking any medications. On physical examination, her temperature is 102.2°F (39°C), blood pressure is 122/80 mmHg, pulse is 80/min, respirations are 18/min, and pulse oximetry is 99% on room air. She has bilateral cervical lymphadenopathy and a visible, enlarged, mobile posterior cervical node. Cardiopulmonary and abdominal examinations are unremarkable. She has an erythematous induration on her right forearm. The most likely cause of this patient's symptoms can be treated with which of the following medications?
- A. Sulfadiazine and pyrimethamine
- B. Atovaquone and azithromycin
- C. Primaquine
- D. Chloroquine
- E. Fexinidazole (Correct Answer)
Antimalarial medications Explanation: ***Fexinidazole***
- This patient's symptoms (recurrent fevers, cervical lymphadenopathy, erythematous induration after a trip to Nigeria with a painful bite) are highly suggestive of **African trypanosomiasis (sleeping sickness)**.
- **Fexinidazole** is an oral nitroimidazole derivative approved for treating both first and second-stage human African trypanosomiasis (HAT) caused by *Trypanosoma brucei gambiense*.
*Sulfadiazine and pyrimethamine*
- This combination is primarily used to treat **toxoplasmosis**, an infection caused by the parasite *Toxoplasma gondii*.
- While it can cause fever and lymphadenopathy, the travel history to Nigeria and a "painful bite" are not typical for toxoplasmosis transmission.
*Atovaquone and azithromycin*
- This combination is utilized for treating **Babesiosis**, a tick-borne parasitic infection.
- While Babesiosis can cause fever and fatigue, the characteristic erythematous induration and prominent lymphadenopathy point away from this diagnosis.
*Primaquine*
- **Primaquine** is an antimalarial drug specifically used for the **radical cure of *Plasmodium vivax*** and ***Plasmodium ovale*** malaria, targeting the hypnozoite liver stages.
- Although the patient has a history of malaria and a travel history to an endemic area, the current presentation with distinct lymphadenopathy and skin lesion points away from a straightforward malarial relapse or new infection primarily requiring primaquine as the sole treatment.
*Chloroquine*
- **Chloroquine** is an antimalarial drug, but its use is limited primarily to areas where **chloroquine-sensitive *Plasmodium falciparum*** strains are prevalent.
- While the patient traveled to Nigeria, a region where malaria is endemic, the specific constellation of symptoms, including the bite and lymphadenopathy, is less characteristic of typical malaria than of trypanosomiasis.
Antimalarial medications US Medical PG Question 5: A 52-year-old man presents for a routine checkup. Past medical history is remarkable for stage 1 systemic hypertension and hepatitis A infection diagnosed 10 years ago. He takes aspirin, rosuvastatin, enalapril daily, and a magnesium supplement every once in a while. He is planning to visit Ecuador for a week-long vacation and is concerned about malaria prophylaxis before his travel. The physician advised taking 1 primaquine pill every day while he is there and for 7 consecutive days after leaving Ecuador. On the third day of his trip, the patient develops an acute onset headache, dizziness, shortness of breath, and fingertips and toes turning blue. His blood pressure is 135/80 mm Hg, heart rate is 94/min, respiratory rate is 22/min, temperature is 36.9℃ (98.4℉), and blood oxygen saturation is 97% in room air. While drawing blood for his laboratory workup, the nurse notes that his blood has a chocolate brown color. Which of the following statements best describes the etiology of this patient’s most likely condition?
- A. The patient’s condition is due to consumption of water polluted with nitrates.
- B. The patient had pre-existing liver damage caused by viral hepatitis.
- C. This condition resulted from primaquine overdose.
- D. It is a type B adverse drug reaction. (Correct Answer)
- E. The condition developed because of his concomitant use of primaquine and magnesium supplement.
Antimalarial medications Explanation: ***It is a type B adverse drug reaction.***
- The patient's symptoms (headache, dizziness, shortness of breath, cyanosis, chocolate brown blood) are consistent with **methemoglobinemia**, which is a known idiosyncratic reaction to **primaquine**. Type B adverse drug reactions are **unpredictable** and not dose-dependent, representing an individual's unique response to a drug.
- This reaction likely stems from an underlying **glucose-6-phosphate dehydrogenase (G6PD) deficiency**, making him susceptible to oxidative stress induced by primaquine, leading to methemoglobin formation. The occurrence of symptoms early in the course of medication (3rd day) also supports an idiosyncratic reaction rather than a typical dose-related effect.
*The patient’s condition is due to consumption of water polluted with nitrates.*
- While **nitrate poisoning** can cause methemoglobinemia, the patient’s symptoms appeared shortly after starting primaquine for malaria prophylaxis, making drug-induced methemoglobinemia a more direct and probable cause in this clinical context.
- Exposure to nitrate-polluted water is unlikely to cause a sudden onset of such severe symptoms within 3 days of arrival, especially considering he is taking a known oxidizing agent (primaquine).
*The patient had pre-existing liver damage caused by viral hepatitis.*
- Although **liver dysfunction** can alter drug metabolism, hepatitis A is an acute infection that does not typically cause chronic liver damage leading to altered drug metabolism for primaquine in the long term, especially 10 years after diagnosis.
- The primary risk factor for primaquine-induced methemoglobinemia is G6PD deficiency, not liver damage, which affects red blood cell susceptibility to oxidative stress.
*This condition resulted from primaquine overdose.*
- The prescribed dose of primaquine (one pill daily) is standard for malaria prophylaxis, and there is no indication the patient took more than prescribed. This reaction is likely due to an **idiosyncratic response** rather than an excessive dose.
- Methemoglobinemia from primaquine is often seen in individuals with **G6PD deficiency** even at therapeutic doses, making it an unpredictable Type B adverse reaction rather than a direct dose-dependent toxicity.
*The condition developed because of his concomitant use of primaquine and magnesium supplement.*
- There is no known direct significant **drug interaction** between primaquine and magnesium supplements that would lead to methemoglobinemia.
- The underlying cause of methemoglobinemia with primaquine is typically due to its **oxidative properties** in susceptible individuals (e.g., G6PD deficiency), not an interaction with magnesium.
Antimalarial medications US Medical PG Question 6: A 32-year-old man is brought to the emergency department with fever, dyspnea, and impaired consciousness. His wife reports that he has also had an episode of dark urine today. Two weeks ago, he returned from a trip to the Republic of Congo. His temperature is 39.4°C (103°F), pulse is 114/min, and blood pressure is 82/51 mm Hg. Physical examination shows scleral icterus. Decreased breath sounds and expiratory crackles are heard on auscultation of the lungs bilaterally. His hemoglobin concentration is 6.3 g/dL. A blood smear shows red blood cells with normal morphology and ring-shaped inclusions. Further laboratory testing shows normal rates of NADPH production. Which of the following is the most appropriate pharmacotherapy for this patient?
- A. Proguanil
- B. Dapsone
- C. Chloroquine
- D. Artesunate (Correct Answer)
- E. Atovaquone
Antimalarial medications Explanation: ***Artesunate***
- This patient presents with **severe malaria**, indicated by fever, impaired consciousness, hypotension, dyspnea, dark urine (hemoglobinuria), scleral icterus (hemolysis), and anemia, following travel to an endemic area (Republic of Congo). The blood smear finding of **ring-shaped inclusions** with normal red cell morphology is characteristic of **Plasmodium falciparum** infection.
- **Artesunate** is the drug of choice for **severe malaria** due to its rapid parasitic clearance and superior efficacy compared to other antimalarials, especially in regions with high chloroquine resistance, as is typical in the Republic of Congo for *P. falciparum*.
*Proguanil*
- Proguanil is primarily used in **malaria prophylaxis** or in combination with other drugs (e.g., atovaquone-proguanil) for uncomplicated malaria.
- It is not indicated as monotherapy for **severe *P. falciparum* malaria**, nor is it suitable for emergency treatment of life-threatening infections.
*Dapsone*
- Dapsone is an **antibiotic** primarily used in the treatment of **leprosy** and prevention of *Pneumocystis jirovecii* pneumonia or toxoplasmosis in immunocompromised patients.
- It has **no significant role** in the treatment of malaria, especially severe *P. falciparum* infection.
*Chloroquine*
- Chloroquine was historically a first-line treatment for malaria but is largely ineffective against **chloroquine-resistant *P. falciparum***, which is widely prevalent in the Republic of Congo and contributes to severe disease.
- Administering chloroquine in this context would likely lead to **treatment failure** and worsening of the patient's severe condition.
*Atovaquone*
- Atovaquone, usually combined with proguanil (Malarone), is effective for **uncomplicated malaria** and prophylaxis.
- However, it is **not the preferred agent for severe malaria** due to slower action and lack of intravenous formulation for initial critical management.
Antimalarial medications US Medical PG Question 7: A 30-year-old man comes to the emergency department because of the sudden onset of back pain beginning 2 hours ago. Beginning yesterday, he noticed that his eyes started appearing yellowish and his urine was darker than normal. Two months ago, he returned from a trip to Greece, where he lived before immigrating to the US 10 years ago. Three days ago, he was diagnosed with latent tuberculosis and started on isoniazid. He has worked as a plumber the last 5 years. His temperature is 37.4°C (99.3°F), pulse is 80/min, and blood pressure is 110/70 mm Hg. Examination shows back tenderness and scleral icterus. Laboratory studies show:
Hematocrit 29%
Leukocyte count 8000/mm3
Platelet count 280,000/mm3
Serum
Bilirubin
Total 4 mg/dL
Direct 0.7 mg/dL
Haptoglobin 15 mg/dL (N=41–165 mg/dL)
Lactate dehydrogenase 180 U/L
Urine
Blood 3+
Protein 1+
RBC 2–3/hpf
WBC 2–3/hpf
Which of the following is the most likely underlying cause of this patient's anemia?
- A. Absence of reduced glutathione (Correct Answer)
- B. Absence of uridine 5'-monophosphate
- C. Crescent-shaped erythrocytes
- D. Defective ankyrin in the RBC membrane
- E. Inhibition of aminolevulinate dehydratase
Antimalarial medications Explanation: ***Absence of reduced glutathione***
- This patient's presentation with anemia, jaundice, dark urine, and particularly the low **haptoglobin** and elevated **LDH**, points to **hemolysis**. The recent initiation of **isoniazid** (an oxidative stressor) and his Greek ancestry strongly suggest **G6PD deficiency**, where a lack of reduced glutathione leads to oxidative damage and hemolysis.
- **Glucose-6-phosphate dehydrogenase (G6PD) deficiency** is an X-linked recessive disorder common in populations of Mediterranean and African descent. It impairs the **hexose monophosphate shunt**, reducing the cell's ability to produce **NADPH**, which is crucial for reducing **oxidative stress** via **reduced glutathione**.
*Absence of uridine 5'-monophosphate*
- Absence of **uridine 5'-monophosphate (UMP)** is associated with **hereditary orotic aciduria**, a rare metabolic disorder.
- This condition typically presents with **megaloblastic anemia** (not hemolytic anemia), growth retardation, and orotic acid crystals in the urine, none of which are consistent with this patient's findings.
*Crescent-shaped erythrocytes*
- **Crescent-shaped erythrocytes** (sickle cells) are characteristic of **sickle cell anemia**, a genetic disorder causing chronic hemolytic anemia, vaso-occlusive crises, and pain.
- While it can cause hemolytic anemia, the triggers and specific laboratory findings (e.g., absence of a specific oxidative stressor like isoniazid causing acute hemolysis, the sudden onset in an adult not previously diagnosed) make it less likely than G6PD deficiency in this context.
*Defective ankyrin in the RBC membrane*
- Defective **ankyrin** in the red blood cell membrane is characteristic of **hereditary spherocytosis**, an inherited disorder causing hemolytic anemia.
- This condition typically presents with **spherocytes** on the blood smear, increased **MCHC**, and a positive **osmotic fragility test**, which are not indicated by the provided lab results.
*Inhibition of aminolevulinate dehydratase*
- Inhibition of **aminolevulinate dehydratase** is associated with **lead poisoning**, which impairs **heme synthesis**.
- This would typically cause a **microcytic or normocytic anemia** with **basophilic stippling** and elevated **protoporphyrin levels**, not an acute hemolytic crisis with jaundice, low haptoglobin, and elevated LDH.
Antimalarial medications US Medical PG Question 8: An 8-year-old boy is brought to the emergency department by his parents because of sudden onset of abdominal pain beginning an hour ago. The parents report that their son has also had an episode of dark urine earlier that morning. Three days ago, he was diagnosed with a urinary tract infection and was treated with trimethoprim-sulfamethoxazole. He emigrated from Liberia to the US with his family 3 years ago. There is no personal history of serious illness. His immunizations are up-to-date. Vital signs are within normal limits. Examination shows diffuse abdominal tenderness and scleral icterus. The spleen is palpated 1–2 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10 g/dL
Mean corpuscular volume 90 μm3
Reticulocyte count 3%
Serum
Bilirubin
Total 3 mg/dL
Direct 0.5 mg/dL
Haptoglobin 20 mg/dL (N=41–165 mg/dL)
Lactate dehydrogenase 160 U/L
Urine
Blood 3+
Protein 1+
RBC 2–3/hpf
WBC 2–3/hpf
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Production of hemoglobin S
- B. Deficient glucose-6-phosphate dehydrogenase (Correct Answer)
- C. Lead poisoning
- D. Cold agglutinins
- E. Defective RBC membrane proteins
Antimalarial medications Explanation: ***Deficient glucose-6-phosphate dehydrogenase***
- The patient's presentation with **hemolytic anemia** (low hemoglobin, elevated reticulocytes, low haptoglobin, elevated LDH, elevated indirect bilirubin) following **trimethoprim-sulfamethoxazole** administration, along with dark urine (hemoglobinuria), is highly suggestive of G6PD deficiency.
- G6PD deficiency is common in individuals of African descent (patient emigrated from Liberia) and certain medications like sulfa drugs can trigger **oxidative stress** leading to hemolysis in affected individuals.
*Production of hemoglobin S*
- While **sickle cell anemia** (due to hemoglobin S) can cause hemolytic anemia and abdominal pain (**vaso-occlusive crisis**), the sudden onset linked to a specific medication and the absence of a prior history of serious illness make G6PD deficiency more likely.
- Sickle cell disease typically presents with recurrent painful crises, dactylitis in infancy, and chronic hemolytic anemia, which are not described here.
*Lead poisoning*
- **Lead poisoning** can cause abdominal pain and anemia, but it typically presents with a **microcytic hypochromic anemia** and **basophilic stippling** on peripheral smear.
- It does not directly cause an acute hemolytic crisis triggered by trimethoprim-sulfamethoxazole.
*Cold agglutinins*
- **Cold agglutinin disease** involves hemolytic anemia triggered by cold exposure, and the antibodies react optimally at cold temperatures.
- The patient's symptoms are acute and triggered by a medication known to induce oxidative stress, which is not characteristic of cold agglutinin disease.
*Defective RBC membrane proteins*
- **Hereditary spherocytosis** (a defect in RBC membrane proteins like spectrin or ankyrin) causes chronic hemolytic anemia and splenomegaly.
- While it can manifest with jaundice, it typically does not cause an acute, drug-induced hemolytic crisis with hemoglobinuria as seen here.
Antimalarial medications US Medical PG Question 9: An experimental infusable drug, X729, is currently being studied to determine its pharmacokinetics. The drug was found to have a half life of 1.5 hours and is eliminated by first order kinetics. What is the minimum number of hours required to reach a steady state concentration of >90%?
- A. 6 (Correct Answer)
- B. 3
- C. 7.5
- D. 1.5
- E. 4.5
Antimalarial medications Explanation: ***6***
- For a drug eliminated by **first-order kinetics**, approximately **4 to 5 half-lives** are required to reach **steady-state concentration**.
- To reach >90% of steady-state, at least **4 half-lives** are needed, where **93.75%** of the steady state is achieved.
- The time taken would be **4 half-lives × 1.5 hours/half-life = 6 hours**, making this the **minimum time** to exceed 90%.
*3*
- This represents only **2 half-lives** (2 × 1.5 hours = 3 hours), which would achieve roughly **75%** of the steady-state concentration.
- This is insufficient to reach >90% of the steady-state concentration.
*7.5*
- This time point represents **5 half-lives** (5 × 1.5 hours = 7.5 hours), which would achieve approximately **97%** of the steady-state concentration.
- While this does exceed 90%, the question asks for the **minimum** number of hours required, and 90% is already exceeded at 6 hours (4 half-lives).
*1.5*
- This is only **1 half-life**, which would achieve approximately **50%** of the steady-state concentration.
- This is far too early to reach a >90% steady-state concentration.
*4.5*
- This represents **3 half-lives** (3 × 1.5 hours = 4.5 hours), achieving approximately **87.5%** of the steady-state concentration.
- While close to 90%, it does not quite reach "greater than 90%".
Antimalarial medications US Medical PG Question 10: A 72-year-old man with congestive heart failure is brought to the emergency department because of chest pain, shortness of breath, dizziness, and palpitations for 30 minutes. An ECG shows a wide complex tachycardia with a P-wave rate of 105/min, an R-wave rate of 130/min, and no apparent relation between the two. Intravenous pharmacotherapy is initiated with a drug that prolongs the QRS and QT intervals. The patient was most likely treated with which of the following drugs?
- A. Carvedilol
- B. Verapamil
- C. Flecainide
- D. Quinidine (Correct Answer)
- E. Sotalol
Antimalarial medications Explanation: **Quinidine**
- Quinidine is a **Class IA antiarrhythmic** that blocks fast sodium channels, prolonging both the **QRS complex** (due to slowed conduction) and the **QT interval** (due to prolonged repolarization).
- The ECG findings of **wide-complex tachycardia** and **AV dissociation** (P-wave rate different from R-wave rate without apparent relation) are consistent with ventricular tachycardia, which Class IA drugs can treat.
*Carvedilol*
- Carvedilol is a **beta-blocker** (Class II antiarrhythmic) that primarily slows heart rate and AV nodal conduction, generally **shortening the QT interval** or having no effect, and would not widen the QRS complex.
- Beta-blockers are typically contraindicated in **decompensated heart failure** and **wide-complex tachycardia** due to their negative inotropic effects and risk of worsening decompensation.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that mainly slows AV nodal conduction. It would not cause QRS widening and can shorten the QT interval.
- Verapamil is generally contraindicated in **wide-complex tachycardias** of unknown origin as it can precipitate cardiovascular collapse if the arrhythmia is ventricular.
*Flecainide*
- Flecainide is a **Class IC antiarrhythmic** that primarily blocks fast sodium channels, causing significant **QRS widening** but has **minimal effect on the QT interval**, which is contrary to the case description.
- Class IC agents are also generally avoided in patients with **structural heart disease** like congestive heart failure due to increased mortality risk.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic** (beta-blocker with potassium channel blockade) that primarily prolongs the **QT interval** by blocking potassium channels. While it prolongs the QT, it does **not significantly widen the QRS complex**.
- Its beta-blocking effects could exacerbate **decompensated heart failure** in this patient, similar to carvedilol.
More Antimalarial medications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.