Anthelmintics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Anthelmintics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Anthelmintics US Medical PG Question 1: A 40-year-old woman presents to clinic with multiple complaints. She complains of swelling around her eyes (Image A) and generalized weakness. A complete blood count reveals eosinophilia. She recently returned from a trip to Asia where she reports having eaten street food, including pork. If this patient's disease is explained by a parasite that causes inflammation of skeletal muscle, what would be the appropriate treatment?
- A. Praziquantel
- B. Niridazole
- C. Albendazole or mebendazole (Correct Answer)
- D. Ivermectin
- E. Diethylcarbamazine
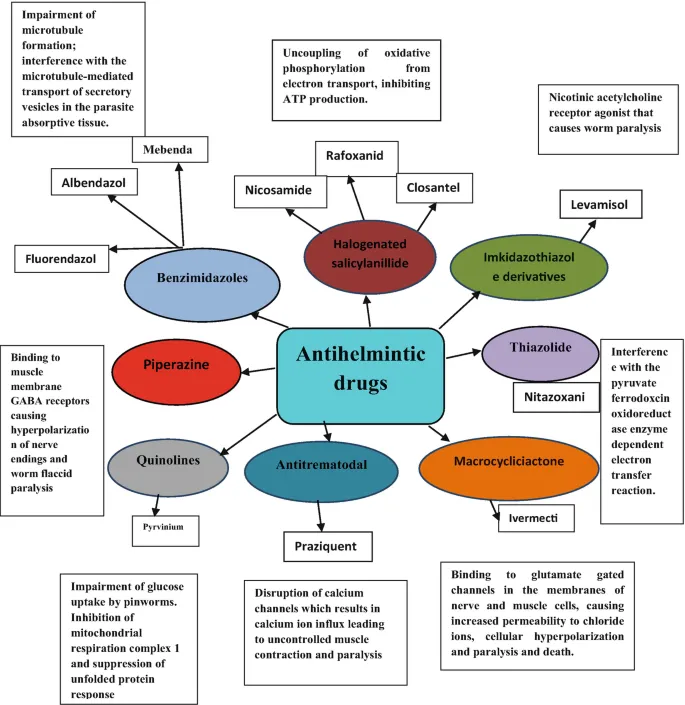
Anthelmintics Explanation: ***Albendazole or mebendazole***
- The clinical presentation (periorbital edema, myalgia/weakness, eosinophilia, recent travel to Asia with consumption of pork) strongly suggests **trichinellosis**, caused by *Trichinella spiralis*.
- **Albendazole** or **mebendazole** (both benzimidazole anthelmintics) are the drugs of choice for treating trichinellosis by killing adult worms in the intestine and larvae in muscle tissue.
- Treatment is most effective when started early in the course of infection.
*Praziquantel*
- This agent is primarily used to treat infections caused by **trematodes** (flukes) and **cestodes** (tapeworms), such as schistosomiasis and taeniasis.
- It is **not effective** against *Trichinella spiralis*.
*Niridazole*
- Niridazole is an **older antischistosomal drug** that is now rarely used due to significant side effects.
- It has **no activity** against *Trichinella spiralis*.
*Ivermectin*
- Ivermectin is effective against various **nematodes**, including *Onchocerca volvulus* (river blindness) and *Strongyloides stercoralis*.
- While it has some activity against *Trichinella*, it is generally considered less effective than benzimidazoles and **not the first-line treatment** for trichinellosis.
*Diethylcarbamazine*
- This medication is primarily used to treat **lymphatic filariasis** (*Wuchereria bancrofti*, *Brugia malayi*) and **loiasis** (*Loa loa*).
- It is **not effective** against *Trichinella spiralis* infection.
Anthelmintics US Medical PG Question 2: A 68-year-old man presents to his physician for symptoms of chronic weight loss, abdominal bloating, and loose stools. He notes that he has also been bothered by a chronic cough. The patient’s laboratory work-up includes a WBC differential, which is remarkable for an eosinophil count of 9%. Stool samples are obtained, with ova and parasite examination revealing roundworm larvae in the stool and no eggs. Which of the following parasitic worms is the cause of this patient’s condition?
- A. Taenia saginata
- B. Taenia solium
- C. Strongyloides stercoralis (Correct Answer)
- D. Necator americanus
- E. Ascaris lumbricoides
Anthelmintics Explanation: ***Strongyloides stercoralis***
- The presence of **larvae (rhabditiform)** in the stool, **pulmonary symptoms** (chronic cough), **gastrointestinal symptoms** (weight loss, bloating, loose stools), and **eosinophilia** are classic findings for *Strongyloides stercoralis* infection.
- Unlike most other intestinal nematodes, *Strongyloides* can establish an **autoinfection cycle**, meaning larvae can reinfect the host, leading to persistent and potentially severe infections even in immunocompetent individuals, without the need for external re-exposure or eggs in stool.
*Taenia saginata*
- This is a **tapeworm (cestode)** that causes taeniasis and is acquired by consuming undercooked beef.
- Diagnosis is typically made by finding **proglottids** or **eggs** in the stool, not larvae, and pulmonary symptoms are not characteristic.
*Taenia solium*
- This is another **tapeworm (cestode)**, acquired by consuming undercooked pork; it can cause taeniasis (intestinal infection) and cysticercosis (tissue infection).
- Similar to *T. saginata*, diagnosis involves finding **proglottids** or **eggs** in stool for intestinal infection, and it does not typically present with lung involvement or larvae in stool.
*Necator americanus*
- This is a **hookworm** that causes iron-deficiency anemia due to blood loss in the intestines.
- While it can cause some pulmonary symptoms as larvae migrate through the lungs, and gastrointestinal symptoms, the diagnostic hallmark is finding **eggs** in the stool, not larvae.
*Ascaris lumbricoides*
- This is the **giant roundworm**; infections are common and often asymptomatic, but heavy worm burdens can cause intestinal obstruction or malnutrition.
- While **pulmonary symptoms (Loeffler's syndrome)** can occur during larval migration, and eosinophilia is present, the diagnosis is confirmed by finding characteristic **mammillated eggs** in the stool, not larvae.
Anthelmintics US Medical PG Question 3: A 31-year-old man comes to the physician because of several months of recurrent abdominal pain and diarrhea. Six months ago, he traveled to Lake Superior for a fishing trip with his friends, during which they often ate their day's catch for dinner. Physical examination shows pallor. Laboratory studies show macrocytic anemia with eosinophilia. A peripheral blood smear shows megaloblasts and hypersegmented neutrophils. A cestode infection is suspected and a drug is prescribed that kills cestodes by inducing uncontrollable muscle spasm in the parasite. The drug prescribed for this patient most likely acts by which of the following mechanisms of action?
- A. Increased calcium influx into the sarcoplasm (Correct Answer)
- B. Increased potassium efflux from the sarcoplasm
- C. Increased sodium efflux from the sarcoplasm
- D. Phosphorylation of adenosine diphosphate
- E. Blockade of myosin binding sites
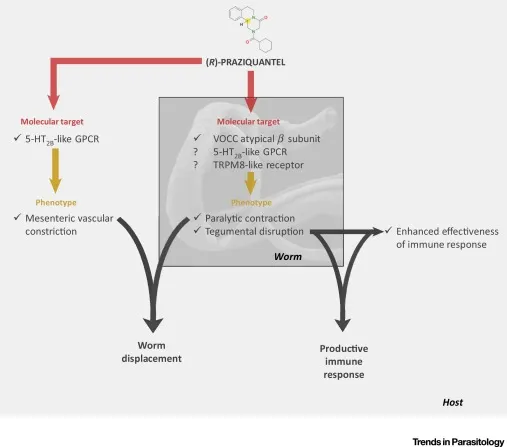
Anthelmintics Explanation: ***Increased calcium influx into the sarcoplasm***
- The clinical picture (macrocytic anemia, eosinophilia, travel history, eating raw fish) points to **Diphyllobothriasis**, caused by the **fish tapeworm** *Diphyllobothrium latum*.
- The drug described, causing **uncontrollable muscle spasm**, is likely **Praziquantel**, which works by increasing **calcium influx** into the worms, leading to paralysis and dislodgement.
*Increased potassium efflux from the sarcoplasm*
- This mechanism is not characteristic of anti-cestode medications that induce muscle spasms.
- While ion channels are therapeutic targets, **potassium efflux** wouldn't directly lead to spastic paralysis in this context.
*Increased sodium efflux from the sarcoplasm*
- This mechanism is not typically associated with the anti-cestode drug Praziquantel or other drugs causing spastic paralysis in parasites.
- Changes in **sodium concentrations** can affect muscle function, but not in the described manner for cestodes.
*Phosphorylation of adenosine diphosphate*
- This refers to the formation of ATP and is a fundamental process in cellular energy metabolism, not a direct drug mechanism for inducing muscle spasms in parasites.
- Anti-parasitic drugs usually target specific metabolic pathways or ion channels rather than general energy production in this manner.
*Blockade of myosin binding sites*
- This mechanism would typically lead to muscle relaxation or flaccid paralysis (e.g., botulinum toxin in humans), not the spastic, uncontrollable spasms described.
- Drugs that block **myosin binding** prevent muscle contraction, which is the opposite of the described effect.
Anthelmintics US Medical PG Question 4: A 56-year-old woman undergoes open reduction and internal fixation of the distal tibia 1 day after a fall. She has had rheumatoid arthritis for 12 years and diabetes mellitus for 2 years. Her medications over the past year have included metformin, prednisone, calcium supplements, and methotrexate. Prior to surgery, insulin was added to her medications, and the dose of prednisone was increased. She has had appropriate nutrition over the years with regular follow-ups with her healthcare professional. Which of the following is the most appropriate supplement to prevent wound failure in this patient?
- A. Glutamine
- B. Zinc
- C. Vitamin A
- D. Arginine
- E. Vitamin C (Correct Answer)
Anthelmintics Explanation: ***Vitamin C***
- This patient is at high risk for **wound healing complications** due to her comorbidities (diabetes, rheumatoid arthritis) and medications (prednisone, methotrexate). **Vitamin C** (ascorbic acid) is essential for **collagen synthesis** and cross-linking, which is crucial for wound strength and tissue repair.
- While other options play a role in wound healing, Vitamin C is particularly important in patients with **impaired healing** due to chronic inflammation, corticosteroid use, and metabolic disorders, as it counteracts their negative effects on collagen formation.
*Glutamine*
- **Glutamine** is an important fuel for rapidly dividing cells, including immune cells and fibroblasts, and can be beneficial in catabolic states.
- However, its role in directly counteracting the specific challenges of this patient's wound healing (corticosteroid use, diabetes, rheumatoid arthritis) is **less direct** compared to Vitamin C's role in collagen synthesis.
*Zinc*
- **Zinc** is a cofactor for numerous enzymes involved in cell proliferation, immune function, and collagen synthesis.
- While important, zinc deficiency is not explicitly indicated, and its role as a primary intervention to prevent wound failure in a patient with **prednisone-induced healing impairment** is secondary to vitamin C.
*Vitamin A*
- **Vitamin A** can help reverse the negative effects of **corticosteroids** on wound healing by promoting epithelialization and collagen synthesis.
- While relevant due to prednisone use, its overall importance in **collagen formation** and direct wound strength is not as profound or broad as Vitamin C.
*Arginine*
- **Arginine** is a precursor for nitric oxide, which improves blood flow to wounds, and is involved in collagen formation and immune function.
- Although beneficial for wound healing, particularly in critically ill patients, it is **not the most appropriate single supplement** for addressing the specific collagen synthesis impairment seen in this patient's context of corticosteroid use and chronic disease.
Anthelmintics US Medical PG Question 5: A tourist with a travel history to India presents with complaints of abdominal pain and multiple episodes of watery diarrhea. He reports having food at a local restaurant the previous night. Which of the following antidiarrheal agents is used in this condition?
- A. Bismuth subsalicylate
- B. Octreotide
- C. Loperamide
- D. Rifaximin (Correct Answer)
- E. Ciprofloxacin
Anthelmintics Explanation: ***Rifaximin***
- This patient's symptoms, including **abdominal pain**, **watery diarrhea**, and a recent **travel history to India** coupled with eating at a local restaurant, strongly suggest **traveler's diarrhea**, often caused by bacterial pathogens.
- **Rifaximin** is a non-absorbable antibiotic specifically approved for treating non-invasive traveler's diarrhea, as it targets causative bacteria in the gut lumen with minimal systemic absorption.
- Rifaximin is preferred due to its **excellent safety profile**, minimal systemic effects, and targeted action against enteric pathogens.
*Ciprofloxacin*
- **Ciprofloxacin** is a fluoroquinolone antibiotic that can be effective for traveler's diarrhea and has been used historically for this indication.
- However, rifaximin is now preferred over ciprofloxacin due to increasing **fluoroquinolone resistance** among enteric pathogens, systemic absorption leading to more side effects, and FDA warnings about serious adverse effects associated with fluoroquinolones.
- Ciprofloxacin may be reserved for more severe or invasive diarrhea cases.
*Bismuth subsalicylate*
- While **bismuth subsalicylate** can be used for symptomatic relief in traveler's diarrhea due to its anti-secretory and anti-inflammatory properties, it is not an antimicrobial agent.
- It works by reducing fluid secretion and inflammation but does not directly address the underlying bacterial infection to the same extent as rifaximin.
*Octreotide*
- **Octreotide** is a somatostatin analog primarily used to treat severe, refractory diarrhea associated with conditions like neuroendocrine tumors or chemotherapy, not typical bacterial traveler's diarrhea.
- Its mechanism involves inhibiting gastrointestinal hormone secretion and reducing intestinal motility, which is too potent for this common, self-limiting condition.
*Loperamide*
- **Loperamide** is an opioid-receptor agonist that acts as an anti-motility agent, reducing the frequency of bowel movements.
- It is generally contraindicated as a primary treatment for traveler's diarrhea when an invasive bacterial infection is suspected, as it can prolong the retention of toxins and pathogens in the gut.
Anthelmintics US Medical PG Question 6: A patient from a North-Eastern state was diagnosed to have an infection with P. Falciparum malaria. What is the most appropriate treatment for this patient?
- A. Chloroquine
- B. Mefloquine
- C. Sulfadoxine plus pyrimethamine
- D. Artemether plus lumefantrine (Correct Answer)
- E. Quinine plus doxycycline
Anthelmintics Explanation: ***Artemether plus lumefantrine***
- Artemether-lumefantrine is the recommended first-line treatment for **uncomplicated P. falciparum malaria** in regions with known **chloroquine resistance**, such as North-Eastern India.
- This combination therapy, an **Artemisinin-based Combination Therapy (ACT)**, is highly effective due to its rapid parasiticidal action and synergy.
*Chloroquine*
- Chloroquine resistance in **P. falciparum malaria** is widespread, particularly in many parts of India, including the North East.
- Using chloroquine alone would likely lead to **treatment failure** and worsening of the patient's condition.
*Mefloquine*
- Mefloquine is an alternative treatment option, but it has significant drawbacks including **neuropsychiatric side effects** (e.g., anxiety, depression, hallucinations) and a long half-life.
- It is often reserved for specific situations or as a second-line agent when ACTs are not available or contraindicated.
*Sulfadoxine plus pyrimethamine*
- **Sulfadoxine-pyrimethamine (SP)** is an older antimalarial drug combination that is not recommended as first-line treatment for **uncomplicated P. falciparum malaria** due to widespread **parasite resistance**.
- While it was formerly used for prophylaxis and intermittent presumptive treatment, its efficacy against P. falciparum has significantly declined.
*Quinine plus doxycycline*
- **Quinine plus doxycycline** is an effective alternative for treating **P. falciparum malaria**, particularly in **severe cases** or when ACTs are contraindicated or unavailable.
- However, it is **not the first-line treatment** for uncomplicated malaria due to longer treatment duration (7 days), more frequent dosing, and potential side effects (cinchonism, GI disturbances).
- Requires adherence to a multi-day regimen, making ACTs more practical for uncomplicated cases.
Anthelmintics US Medical PG Question 7: Which of the following chelating agents is indicated in iron overdose?
- A. Desferrioxamine (Correct Answer)
- B. BAL
- C. Calcium Edetate
- D. DTPA
- E. Penicillamine
Anthelmintics Explanation: ***Desferrioxamine***
- **Desferrioxamine** is a **chelate** formed by the bacterium *Streptomyces pilosus* that has a high affinity for **iron**.
- It is currently the most commonly used chelating agent for **acute iron overdose** and **chronic iron overload** conditions like hemochromatosis or transfusional hemosiderosis.
*BAL*
- **BAL (dimercaprol)** is a chelating agent primarily used for poisoning with **arsenic**, **mercury**, and **gold**.
- It works by forming stable cyclic compounds with these metals, facilitating their excretion.
*Calcium Edetate*
- **Calcium edetate (Calcium-EDTA)** is primarily used for **lead poisoning**.
- It works by forming a stable, water-soluble complex with lead, which is then excreted by the kidneys.
*DTPA*
- **Diethylenetriamine pentaacetate (DTPA)** is a chelating agent primarily used for poisoning with **plutonium** and other **radioactive metals**.
- It is not indicated for iron overdose.
*Penicillamine*
- **Penicillamine** is a chelating agent primarily used for **copper** overload (Wilson's disease) and can also be used for **lead** and **mercury** poisoning.
- It is not effective for iron chelation in overdose situations.
Anthelmintics US Medical PG Question 8: An 18-year-old boy from Rajasthan weighing 50 kg is diagnosed with mixed P . vivax and P . falciparum malaria. What is the appropriate treatment regimen on day 2?
- A. Artesunate 50 mg (4 tablets) + Primaquine 2.5 mg ( 6 tablets)
- B. Artesunate 50 mg (4 tablets) + Primaquine 7.5 mg (6 tablets)
- C. Artesunate 50 mg (4 tablets) + Sulfadoxine/ pyrimethamine ( 750/37.5 mg ) (2 tablets) + Primaquine 2.5 mg ( 6 tablets) (Correct Answer)
- D. Artesunate 50 mg (4 tablets) + Sulfadoxine/ pyrimethamine ( 750/37.5 mg ) (2 tablets) + Primaquine 7.5 mg ( 6 tablets)
- E. Artesunate 50 mg (4 tablets) only
Anthelmintics Explanation: ***Artesunate 50 mg (4 tablets) + Sulfadoxine/pyrimethamine (750/37.5 mg) (2 tablets) + Primaquine 2.5 mg (6 tablets)***
- For **mixed P. vivax and P. falciparum malaria**, the standard treatment regimen in India includes **Artesunate, Sulfadoxine/Pyrimethamine (SP)**, and **Primaquine**.
- **Artesunate** and **SP** target the erythrocytic stages of P. falciparum, while **Primaquine** is essential for killing P. vivax hypnozoites (to prevent relapse) and P. falciparum gametocytes (to reduce transmission).
- On **Day 2**, the patient continues with Artesunate along with SP (if given as single dose on Day 0, this would not be repeated; if following a specific protocol where Day 2 includes all three drugs, this represents the complete regimen).
- The dosage of Primaquine of **2.5 mg** (0.25 mg/kg for 50 kg individual) daily for 14 days is appropriate for P. vivax radical cure.
*Artesunate 50 mg (4 tablets) + Primaquine 2.5 mg (6 tablets)*
- This regimen is incomplete for **mixed infections** as it lacks **Sulfadoxine/Pyrimethamine (SP)**, which is crucial for effective treatment of P. falciparum infections.
- While Primaquine is included, the absence of SP would likely lead to treatment failure or recrudescence of **P. falciparum**.
*Artesunate 50 mg (4 tablets) + Primaquine 7.5 mg (6 tablets)*
- This regimen also omits **Sulfadoxine/Pyrimethamine (SP)**, which is necessary for the treatment of P. falciparum in mixed infections.
- The **Primaquine dosage of 7.5 mg** is higher than typically used for P. vivax radical cure in this context (usually 0.25 mg/kg), and the absence of SP makes this regimen inadequate for mixed malaria.
*Artesunate 50 mg (4 tablets) + Sulfadoxine/pyrimethamine (750/37.5 mg) (2 tablets) + Primaquine 7.5 mg (6 tablets)*
- While this option includes **Artesunate** and **SP** for P. falciparum, the **Primaquine dose of 7.5 mg** is too high for the standard daily dose required for P. vivax radical cure in a 50 kg individual (which is 2.5 mg/day).
- An inappropriately high dose of Primaquine for daily use for 14 days increases the risk of side effects, especially in individuals with **G6PD deficiency**, and is not the recommended regimen for mixed malaria in India.
*Artesunate 50 mg (4 tablets) only*
- While Artesunate is a key component of treatment, using it **alone on Day 2** without SP is inadequate for **P. falciparum** and does not address **P. vivax hypnozoites**.
- This incomplete regimen would not provide radical cure for P. vivax and lacks the partner drug (SP) necessary for effective clearance of P. falciparum parasites.
Anthelmintics US Medical PG Question 9: In which phase of clinical trials is drug dosing typically determined?
- A. Phase 1 (Correct Answer)
- B. Phase 2
- C. Phase 3
- D. Phase 4
- E. Phase 0
Anthelmintics Explanation: ***Phase 1***
- This phase involves a small group of **healthy volunteers** to assess the drug's safety, **pharmacokinetics (PK)**, and establish an initial dosing range.
- The primary goal is to determine a **safe dosage level**, establish the **maximum tolerated dose (MTD)**, and identify potential side effects.
- This is where drug dosing is **typically determined**.
*Phase 0*
- This is an exploratory phase involving **microdosing** studies with subtherapeutic doses.
- The goal is to gather preliminary PK/PD data, but **not to determine therapeutic dosing**.
*Phase 2*
- This phase involves a larger group of **patients** with the condition to be treated.
- The main goal is to evaluate the drug's **effectiveness** and further assess safety, but not primarily to determine initial dosing.
*Phase 3*
- This phase involves a large number of patients across multiple sites to confirm the drug's **efficacy** and monitor side effects in a broader population.
- Dosing strategies have generally been established in earlier phases, and this phase primarily validates them.
*Phase 4*
- This phase occurs **after a drug has been approved** and marketed.
- It involves ongoing surveillance to monitor long-term effects, collect additional information on safety, and identify new uses, but not initial dose determination.
Anthelmintics US Medical PG Question 10: Which of the following statements about Ciclesonide is incorrect?
- A. Oral candidiasis is common with its use. (Correct Answer)
- B. It is a prodrug activated by bronchial esterase.
- C. It has comparable efficacy to other inhalational corticosteroids.
- D. It has fewer side effects than other inhalational corticosteroids.
- E. It has low systemic bioavailability due to extensive first-pass metabolism.
Anthelmintics Explanation: ***Oral candidiasis is common with its use.***
* Ciclesonide is a **prodrug** that is activated in the lungs, which minimizes systemic exposure and reduces the risk of local side effects like **oral candidiasis**.
* Therefore, oral candidiasis is **less common** with ciclesonide compared to other inhaled corticosteroids that deliver the active drug directly to the oral cavity.
*It is a prodrug activated by bronchial esterase.*
* Ciclesonide is indeed a **prodrug** that is converted into its active metabolite, **des-ciclesonide**, by **esterases** primarily found in the lungs.
* This specific activation mechanism helps ensure that the drug's therapeutic effects are localized to the airways while minimizing systemic exposure.
*It has comparable efficacy to other inhalational corticosteroids.*
* Studies have shown that ciclesonide provides **comparable efficacy** to other established inhaled corticosteroids in controlling asthma symptoms and improving lung function.
* Its potent anti-inflammatory effects are effective in reducing airway hyperresponsiveness and inflammation.
*It has fewer side effects than other inhalational corticosteroids.*
* Because ciclesonide is a prodrug activated in the lungs and has a **high protein binding capacity**, it has a reduced likelihood of systemic side effects.
* This contributes to a **favorable safety profile**, with a lower incidence of both local and systemic adverse drug reactions compared to some other inhaled corticosteroids.
*It has low systemic bioavailability due to extensive first-pass metabolism.*
* Ciclesonide has **very low systemic bioavailability** (<1%) when administered via inhalation.
* The active metabolite des-ciclesonide that does reach systemic circulation undergoes **extensive first-pass metabolism** in the liver, further reducing systemic exposure.
* This pharmacokinetic property contributes to its excellent safety profile and minimal systemic adverse effects.
More Anthelmintics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.