SGLT2 inhibitors in hypertension US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for SGLT2 inhibitors in hypertension. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
SGLT2 inhibitors in hypertension US Medical PG Question 1: A 56-year-old man with type 2 diabetes mellitus comes to the physician for a follow-up examination. He reports that he has been compliant with his current antidiabetic medication regimen. His hemoglobin A1c concentration is 8.5%. The physician prescribes a drug that reversibly inhibits a membrane-bound enzyme that hydrolyzes carbohydrate bonds. Which of the following drugs was most likely added to this patient's medication regimen?
- A. Canagliflozin
- B. Miglitol (Correct Answer)
- C. Linagliptin
- D. Pramlintide
- E. Rosiglitazone
SGLT2 inhibitors in hypertension Explanation: ***Miglitol***
- Miglitol is an **alpha-glucosidase inhibitor** that reversibly inhibits enzymes like sucrase and maltase in the brush border of the small intestine.
- This action **delays carbohydrate digestion and absorption**, reducing postprandial glucose excursions, which fits the description of inhibiting a "membrane-bound enzyme that hydrolyzes carbohydrate bonds."
*Canagliflozin*
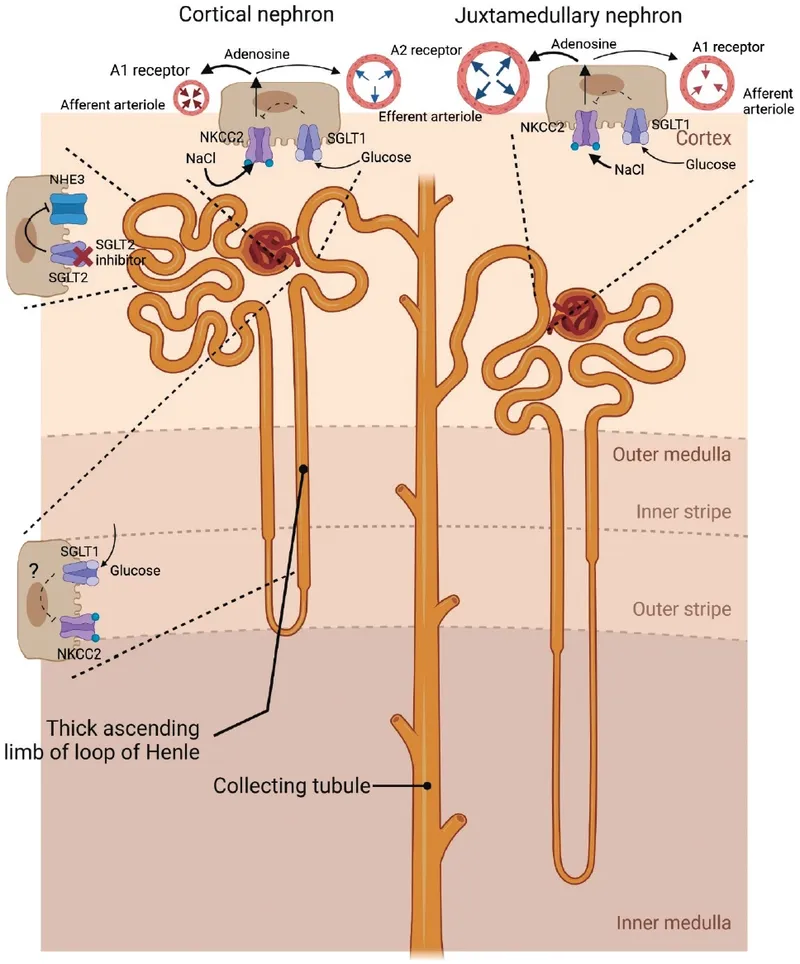
- Canagliflozin is a **sodium-glucose co-transporter 2 (SGLT2) inhibitor** that acts in the kidney to reduce glucose reabsorption, leading to increased glucose excretion in the urine.
- It does not inhibit carbohydrate-hydrolyzing enzymes in the gastrointestinal tract.
*Linagliptin*
- Linagliptin is a **dipeptidyl peptidase-4 (DPP-4) inhibitor** that increases the levels of incretin hormones (GLP-1 and GIP), thereby enhancing glucose-dependent insulin secretion and suppressing glucagon secretion.
- This mechanism is distinct from inhibiting carbohydrate hydrolysis.
*Pramlintide*
- Pramlintide is an **amylin analog** that slows gastric emptying, suppresses postprandial glucagon secretion, and promotes satiety.
- It works by mimicking the action of amylin, not by inhibiting enzymes that break down carbohydrates.
*Rosiglitazone*
- Rosiglitazone is a **thiazolidinedione (TZD)** that acts as an agonist for peroxisome proliferator-activated receptor-gamma (PPAR-γ) to improve insulin sensitivity in peripheral tissues.
- Its mechanism of action is related to gene transcription and insulin sensitization rather than direct inhibition of carbohydrate-hydrolyzing enzymes.
SGLT2 inhibitors in hypertension US Medical PG Question 2: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
SGLT2 inhibitors in hypertension Explanation: ***Aldosterone***
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
SGLT2 inhibitors in hypertension US Medical PG Question 3: A 54-year-old woman presents for follow-up care for her type 2 diabetes mellitus. She was diagnosed approximately 2 years ago and was treated with dietary modifications, an exercise regimen, metformin, and glipizide. She reports that her increased thirst and urinary frequency has not improved with her current treatment regimen. Her hemoglobin A1c is 8.5% at this visit. She is started on a medication that will result in weight loss but places her at increased risk of developing urinary tract infections and vulvovaginal candidiasis. Which of the following is the mechanism of action of the prescribed medication?
- A. Peroxisome proliferator-activated receptor activator
- B. Glucagon-like protein-1 receptor agonist
- C. Sodium-glucose co-transporter-2 inhibitor (Correct Answer)
- D. Alpha-glucosidase inhibitor
- E. Dipeptidyl peptidase-4 inhibitor
SGLT2 inhibitors in hypertension Explanation: ***Sodium-glucose co-transporter-2 inhibitor***
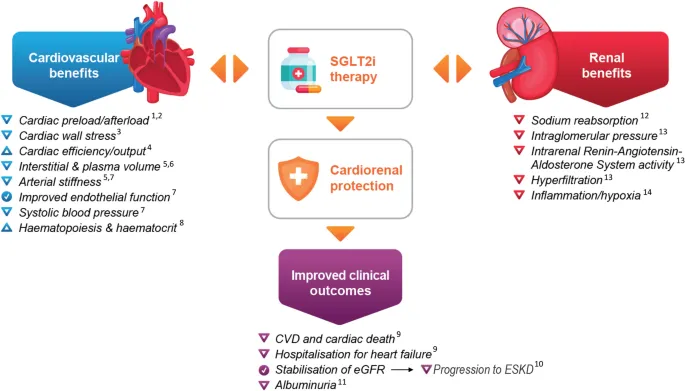
- The patient's **HbA1c of 8.5%** indicates uncontrolled diabetes, and the mention of weight loss and increased risk of **urinary tract infections (UTIs)** and **vulvovaginal candidiasis** strongly points to an SGLT2 inhibitor.
- SGLT2 inhibitors work by **blocking glucose reabsorption in the renal tubules**, leading to increased glucose excretion in urine, which can cause candidiasis and UTIs, and also contributes to weight loss.
*Peroxisome proliferator-activated receptor activator*
- This refers to **thiazolidinediones (TZDs)**, which reduce insulin resistance by increasing glucose uptake in peripheral tissues, but are not associated with increased UTIs or vulvovaginal candidiasis.
- TZDs can cause **weight gain** and fluid retention, which is contrary to the weight loss mentioned in the stem.
*Glucagon-like protein-1 receptor agonist*
- GLP-1 receptor agonists like liraglutide and semaglutide encourage **weight loss** and improve glycemic control by increasing insulin secretion and decreasing glucagon secretion, but they are not primarily associated with increased risk of UTIs or candidiasis.
- Their common side effects include **gastrointestinal issues** such as nausea and vomiting.
*Alpha-glucosidase inhibitor*
- These medications (e.g., acarbose) work by **delaying carbohydrate absorption** in the gut, which primarily helps reduce postprandial glucose levels.
- They commonly cause **gastrointestinal side effects** such as flatulence and diarrhea, and are not associated with UTIs, candidiasis, or significant weight loss.
*Dipeptidyl peptidase-4 inhibitor*
- DPP-4 inhibitors (e.g., sitagliptin, saxagliptin) enhance the effects of incretin hormones by **preventing their breakdown**, leading to increased insulin secretion and decreased glucagon.
- They are generally **weight-neutral** and do not cause the specific adverse effects (UTIs, candidiasis) mentioned in the clinical scenario.
SGLT2 inhibitors in hypertension US Medical PG Question 4: Activation of the renin-angiotensin-aldosterone system yields a significant physiological effect on renal blood flow and filtration. Which of the following is most likely to occur in response to increased levels of Angiotensin-II?
- A. Decreased renal plasma flow, decreased filtration fraction
- B. Decreased renal plasma flow, increased glomerular capillary oncotic pressure
- C. Increased renal plasma flow, decreased filtration fraction
- D. Increased renal plasma flow, increased filtration fraction
- E. Decreased renal plasma flow, increased filtration fraction (Correct Answer)
SGLT2 inhibitors in hypertension Explanation: ***Decreased renal plasma flow, increased filtration fraction***
- **Angiotensin II** causes **efferent arteriolar constriction**, which reduces blood flow leaving the glomerulus, thereby **decreasing renal plasma flow**.
- This efferent constriction also increases **glomerular hydrostatic pressure** and reduces plasma flow distal to the glomerulus, leading to a **higher filtration fraction** (GFR/RPF).
*Decreased renal plasma flow, decreased filtration fraction*
- While **renal plasma flow decreases**, a **decreased filtration fraction** would imply that either GFR decreases disproportionately more than RPF or GFR does not increase despite the RPF reduction, which is not the typical response to **angiotensin II** due to its predominant effect on the **efferent arteriole**.
*Decreased renal plasma flow, increased glomerular capillary oncotic pressure*
- **Increased glomerular capillary oncotic pressure** is a consequence of increased filtration fraction, as more fluid is filtered out, leaving behind a more concentrated plasma. This option includes a correct element (decreased RPF) but pairs it with a less direct and defining outcome of acute Angiotensin II action as the primary physiological effect.
*Increased renal plasma flow, decreased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, predominantly of the efferent arteriole, which by definition would **decrease renal plasma flow**, not increase it.
- A **decreased filtration fraction** would be inconsistent with efferent arteriolar constriction which typically raises GFR relative to RPF.
*Increased renal plasma flow, increased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, leading to a **decrease in renal plasma flow**, not an increase.
- While **filtration fraction is increased**, the initial premise of increased renal plasma flow is incorrect.
SGLT2 inhibitors in hypertension US Medical PG Question 5: A 47-year-old woman presents to the physician with complaints of fatigue accompanied by symmetric pain, swelling, and stiffness in her wrists, fingers, knees, and other joints. She describes the stiffness as being particularly severe upon awakening, but gradually improves as she moves throughout her day. Her physician initially suggests that she take NSAIDs. However, after a few months of minimal symptomatic improvement, she is prescribed an immunosuppressive drug that has a mechanism of preventing IL-2 transcription. What is the main toxicity that the patient must be aware of with this particular class of drugs?
- A. Pancytopenia
- B. Osteoporosis
- C. Hepatotoxicity
- D. Nephrotoxicity (Correct Answer)
- E. Hyperglycemia
SGLT2 inhibitors in hypertension Explanation: ***Nephrotoxicity***
- The drug described, which prevents **IL-2 transcription**, is likely a **calcineurin inhibitor** like cyclosporine or tacrolimus, often used in autoimmune diseases.
- **Nephrotoxicity** (kidney damage) is a major dose-limiting toxicity of calcineurin inhibitors, causing both acute and chronic kidney injury.
*Pancytopenia*
- While some immunosuppressants can cause **pancytopenia** (e.g., azathioprine, methotrexate), it is not the classic or primary toxicity associated with calcineurin inhibitors.
- Calcineurin inhibitors primarily affect **renal function** and can cause other side effects like hypertension or neurotoxicity.
*Osteoporosis*
- **Osteoporosis** is a known side effect of long-term glucocorticoid use, but not typically a primary toxicity of calcineurin inhibitors.
- Glucocorticoids reduce bone formation and increase bone resorption, leading to bone density loss.
*Hepatotoxicity*
- **Hepatotoxicity** (liver damage) can occur with various immunosuppressants, such as methotrexate, but it is not the most prominent or defining toxicity for calcineurin inhibitors.
- While cyclosporine can cause some liver enzyme elevation, **nephrotoxicity** is far more common and severe.
*Hyperglycemia*
- **Hyperglycemia** can be a side effect of some immunosuppressants, particularly **glucocorticoids** and **tacrolimus** (another calcineurin inhibitor).
- However, for the class of drugs that prevent IL-2 transcription (calcineurin inhibitors), **nephrotoxicity** remains the most significant and common major toxicity to be aware of.
SGLT2 inhibitors in hypertension US Medical PG Question 6: A randomized controlled trial was initiated to evaluate a novel DPP-4 inhibitor for blood glucose management in diabetic patients. The study used a commonly prescribed sulfonylurea as the standard of care treatment. 2,000 patients were enrolled in the study with 1,000 patients in each arm. One of the primary outcomes was the development of diabetic nephropathy during treatment. This outcome occurred in 68 patients on the DPP-4 inhibitor and 134 patients on the sulfonylurea. What is the relative risk reduction (RRR) for patients using the DPP-4 inhibitor compared with the sulfonylurea?
- A. 23%
- B. 49% (Correct Answer)
- C. 33%
- D. 59%
- E. 43%
SGLT2 inhibitors in hypertension Explanation: ***49%***
- To calculate **relative risk reduction (RRR)**, first determine the **event rate (ER)** for each group.
- ER (DPP-4 inhibitor) = 68/1000 = 0.068. ER (Sulfonylurea) = 134/1000 = 0.134.
- Next, calculate the **absolute risk reduction (ARR)**: ARR = ER (Sulfonylurea) - ER (DPP-4 inhibitor) = 0.134 - 0.068 = 0.066.
- Finally, calculate RRR: RRR = ARR / ER (Sulfonylurea) = 0.066 / 0.134 ≈ 0.4925 or **49%**.
*23%*
- This value is incorrect and does not result from the proper application of the **relative risk reduction (RRR)** formula.
- A common mistake is to reverse the subtrahend and minuend in the numerator or denominator.
*33%*
- This value is incorrect and does not result from the proper application of the **relative risk reduction (RRR)** formula.
- Incorrect calculations in either the numerator or denominator of the **RRR formula** would lead to this incorrect result.
*59%*
- This value is incorrect and is likely the result of an error in calculating either the **absolute risk reduction (ARR)** or dividing it by the wrong **event rate**.
- Always ensure the correct event rates are used for the control group and the intervention group.
*43%*
- This value is incorrect and does not align with the correct calculation of **relative risk reduction (RRR)**.
- Errors in setting up the formula or executing the division could lead to this result.
SGLT2 inhibitors in hypertension US Medical PG Question 7: A 29-year-old female presents to her gynecologist complaining of a painful rash around her genitals. She has multiple sexual partners and uses condoms intermittently. Her last STD screen one year ago was negative. On examination, she has bilateral erosive vesicles on her labia majora and painful inguinal lymphadenopathy. She is started on an oral medication that requires a specific thymidine kinase for activation. Which of the following adverse effects is associated with this drug?
- A. Photosensitivity
- B. Deafness
- C. Renal failure (Correct Answer)
- D. Gingival hyperplasia
- E. Pulmonary fibrosis
SGLT2 inhibitors in hypertension Explanation: ***Renal failure***
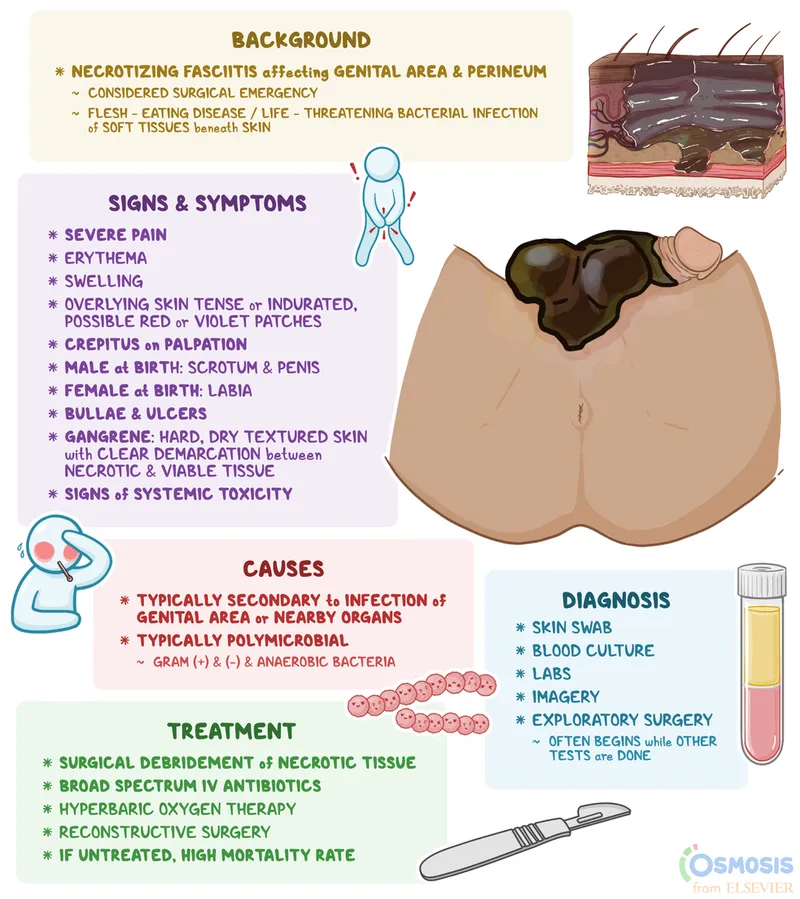
- The patient's symptoms (painful genital rash, erosive vesicles, inguinal lymphadenopathy) are highly suggestive of **herpes simplex virus (HSV) infection**, likely genital herpes.
- The drug described is an antiviral agent like **acyclovir, valacyclovir, or famciclovir**, which require **viral thymidine kinase** for activation and are known to cause **renal impairment** (nephrotoxicity) as an adverse effect, especially with high doses or in dehydrated patients due to crystal nephropathy.
*Photosensitivity*
- **Photosensitivity** is a common side effect of some antibiotics (e.g., tetracyclines, sulfonamides), diuretics (e.g., thiazides), and antifungals, but it is **not a prominent adverse effect of acyclovir or its derivatives**.
- While theoretical, it is not a clinically significant or frequently observed adverse effect associated with the class of antiviral drugs used for HSV.
*Deafness*
- **Ototoxicity**, leading to deafness or hearing loss, is a well-known adverse effect of certain classes of drugs, such as **aminoglycoside antibiotics** (e.g., gentamicin) and **loop diuretics** (e.g., furosemide).
- It is **not an adverse effect** associated with antiviral medications like acyclovir.
*Gingival hyperplasia*
- **Gingival hyperplasia** (overgrowth of gum tissue) is a recognized side effect of specific medications including **phenytoin** (an anticonvulsant), **cyclosporine** (an immunosuppressant), and **calcium channel blockers** (e.g., nifedipine, amlodipine).
- This adverse effect is **not associated with antiviral drugs** used to treat herpes simplex.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a serious adverse effect linked to various drugs like **amiodarone** (an antiarrhythmic), **bleomycin** (a chemotherapeutic agent), **methotrexate** (an immunosuppressant/chemotherapeutic), and **nitrofurantoin** (an antibiotic).
- **Antiviral medications for HSV** do not typically cause pulmonary fibrosis.
SGLT2 inhibitors in hypertension US Medical PG Question 8: A 58-year-old man presents for a follow-up appointment. He recently was found to have a history of stage 2 chronic kidney disease secondary to benign prostatic hyperplasia leading to urinary tract obstruction. He has no other medical conditions. His father died at age 86 from a stroke, and his mother lives in an assisted living facility. He smokes a pack of cigarettes a day and occasionally drinks alcohol. His vital signs include: blood pressure 130/75 mm Hg, pulse 75/min, respiratory rate 17/min, and temperature 36.5°C (97.7°F). His physical examination is unremarkable. A 24-hour urine specimen reveals the following findings:
Specific gravity 1,050
pH 5.6
Nitrites (-)
Glucose (-)
Proteins 250 mg/24hrs
Which of the following should be prescribed to this patient to decrease his cardiovascular risk?
- A. Enalapril (Correct Answer)
- B. Ezetimibe
- C. Amlodipine
- D. Carvedilol
- E. Aspirin
SGLT2 inhibitors in hypertension Explanation: ***Enalapril***
- **Enalapril**, an ACE inhibitor, is indicated for patients with **chronic kidney disease** and **proteinuria** to reduce cardiovascular risk and slow kidney disease progression.
- The patient has stage 2 CKD and **250 mg/24hrs of protein in urine**, which, when coupled with hypertension, makes ACE inhibitors the preferred choice to mitigate cardiovascular risk.
*Ezetimibe*
- **Ezetimibe** is a **cholesterol absorption inhibitor** used to lower LDL-C, but there is no information in the vignette to suggest hyperlipidemia.
- It is an inappropriate choice without evidence of dyslipidemia or a strong indication for lipid-lowering therapy.
*Amlodipine*
- **Amlodipine** is a **calcium channel blocker** used to treat hypertension but does not provide specific renal-protective benefits in patients with proteinuria.
- It would be a consideration for blood pressure control if an ACE inhibitor were contraindicated or insufficient.
*Carvedilol*
- **Carvedilol** is a **beta-blocker** used for hypertension, heart failure, and post-MI, but there is no indication for its use here.
- It is not the first-line agent for cardiovascular risk reduction in patients with chronic kidney disease and proteinuria without other specific cardiac indications.
*Aspirin*
- **Aspirin** is used for primary or secondary prevention of cardiovascular events due to its **antiplatelet effects**. However, in the absence of established cardiovascular disease, its use for primary prevention in CKD patients needs careful consideration of bleeding risk.
- While patients with CKD are at higher cardiovascular risk, an ACE inhibitor addresses both the hypertension and proteinuria, which directly contribute to cardiovascular and kidney disease progression in this patient.
SGLT2 inhibitors in hypertension US Medical PG Question 9: A 55-year-old man comes to the physician because of a 4-month history of episodic, pressure-like chest pain. The chest pain occurs when he is walking up stairs and improves with rest. He has hypertension and type 2 diabetes mellitus. His father died from a myocardial infarction at the age of 50 years. Current medications include hydrochlorothiazide and metformin. His pulse is 85/min, respirations are 12/min, and blood pressure is 140/90 mm Hg. Cardiac examination shows normal heart sounds without any murmurs, rubs, or gallops. An ECG shows high amplitude of the S wave in lead V3. An exercise stress test is performed but stopped after 4 minutes because the patient experiences chest pain. An ECG obtained during the stress test shows sinus tachycardia and ST-segment depressions in leads V1–V4. Which of the following is the most appropriate long-term pharmacotherapy to reduce the frequency of symptoms in this patient?
- A. Metoprolol (Correct Answer)
- B. Clopidogrel
- C. Aspirin
- D. Nitroglycerin
- E. Isosorbide mononitrate
SGLT2 inhibitors in hypertension Explanation: ***Metoprolol***
- **Beta-blockers** like metoprolol are first-line agents for **symptom relief** in stable angina by reducing myocardial oxygen demand.
- They decrease **heart rate**, **blood pressure**, and **myocardial contractility**, thereby reducing the frequency and severity of anginal episodes.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent used primarily to prevent **thrombotic events** in patients with established cardiovascular disease or acute coronary syndromes.
- It does not directly reduce the frequency of anginal symptoms, but rather prevents progression to **myocardial infarction** or **stroke**.
*Aspirin*
- **Aspirin** is an antiplatelet medication used for **secondary prevention** of cardiovascular events by inhibiting platelet aggregation.
- While crucial for reducing cardiovascular risk, it does not directly alleviate the **frequency of anginal symptoms** themselves.
*Nitroglycerin*
- **Nitroglycerin** is a short-acting nitrate used to provide **immediate relief** of anginal pain during an acute episode.
- It is not a long-term pharmacotherapy for reducing the *frequency* of symptoms.
*Isosorbide mononitrate*
- **Isosorbide mononitrate** is a long-acting nitrate used to *prevent* angina, but it is typically a **second-line agent** after beta-blockers due to potential for **tolerance** and side effects.
- While it can reduce symptom frequency, beta-blockers are generally preferred as initial long-term therapy for symptom control.
SGLT2 inhibitors in hypertension US Medical PG Question 10: A 55-year-old male is hospitalized for acute heart failure. The patient has a 20-year history of alcoholism and was diagnosed with diabetes mellitus type 2 (DM2) 5 years ago. Physical examination reveals ascites and engorged paraumbilical veins as well as 3+ pitting edema around both ankles. Liver function tests show elevations in gamma glutamyl transferase and aspartate transaminase (AST). Of the following medication, which most likely contributed to this patient's presentation?
- A. Glargine
- B. Pramlintide
- C. Pioglitazone (Correct Answer)
- D. Glipizide
- E. Metformin
SGLT2 inhibitors in hypertension Explanation: ***Pioglitazone***
- **Pioglitazone**, a thiazolidinedione, is known to cause **fluid retention** and can exacerbate or precipitate **congestive heart failure**.
- The patient's presentation with **ascites**, **pitting edema**, and **acute heart failure** is consistent with the adverse effects of this medication, especially in a patient with risk factors like alcoholism.
*Glargine*
- **Glargine** is a **long-acting insulin** analog primarily used to control blood glucose levels in diabetes.
- It does not typically cause **fluid retention** or worsen **heart failure** directly, making it an unlikely contributor to these specific symptoms.
*Pramlintide*
- **Pramlintide** is an **amylin analog** used to improve glycemic control by slowing gastric emptying and suppressing glucagon secretion.
- It is not associated with **fluid retention** or the exacerbation of **heart failure**.
*Glipizide*
- **Glipizide** is a **sulfonylurea** that stimulates insulin release from pancreatic beta cells.
- While it can cause hypoglycemia, it does not typically contribute to **fluid retention** or worsen **heart failure**.
*Metformin*
- **Metformin** is a **biguanide** that reduces hepatic glucose production and increases insulin sensitivity.
- It is generally considered **cardioprotective** and does not cause **fluid retention** or exacerbate **heart failure**.
More SGLT2 inhibitors in hypertension US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.