Diuretic classes and mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diuretic classes and mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diuretic classes and mechanisms US Medical PG Question 1: In your peripheral tissues and lungs, carbonic anhydrase works to control the equilibrium between carbon dioxide and carbonic acid in order to maintain proper blood pH. Through which mechanism does carbonic anhydrase exert its influence on reaction kinetics?
- A. Changes the delta G of the reaction
- B. Lowers the free energy of products
- C. Raises the activation energy
- D. Lowers the activation energy (Correct Answer)
- E. Lowers the free energy of reactants
Diuretic classes and mechanisms Explanation: ***Lowers the activation energy***
- Enzymes like **carbonic anhydrase** function by providing an alternative reaction pathway with a **lower activation energy**.
- This reduction in activation energy leads to a significant increase in the **reaction rate**, allowing the reaction to proceed more quickly without altering its equilibrium.
*Changes the delta G of the reaction*
- Enzymes do not alter the **overall Gibbs free energy change (ΔG)** of a reaction.
- The **ΔG** is a thermodynamic property determined by the difference in free energy between reactants and products, which is unaffected by catalyst.
*Lowers the free energy of products*
- Enzymes do not change the **free energy** of either the products or the reactants.
- Affecting the free energy of products would alter the overall **ΔG** of the reaction and thus the **equilibrium constant**.
*Raises the activation energy*
- Raising the **activation energy** would slow down the reaction rate, which is the opposite of an enzyme's function.
- Enzymes are catalysts designed to **accelerate reactions** by lowering the energy barrier.
*Lowers the free energy of reactants*
- Enzymes do not change the **free energy** of reactants.
- Altering the free energy of reactants would also change the overall **ΔG** of the reaction and its equilibrium.
Diuretic classes and mechanisms US Medical PG Question 2: A 72-year-old man is brought to the emergency department by his daughter because he was found to have decreased alertness that has gotten progressively worse. Three weeks ago he was diagnosed with an infection and given an antibiotic, though his daughter does not remember what drug was prescribed. His medical history is also significant for benign prostatic hyperplasia and hypertension, for which he was prescribed tamsulosin, a thiazide, and an ACE inhibitor. He has not sustained any trauma recently, and no wounds are apparent. On presentation, he is found to be confused. Labs are obtained with the following results:
Serum:
Na+: 135 mEq/L
BUN: 52 mg/dL
Creatinine: 2.1 mg/dL
Urine:
Osmolality: 548 mOsm/kg
Na+: 13 mEq/L
Creatinine: 32 mg/dL
Which of the following etiologies would be most likely given this patient's presentation?
- A. Forgetting to take tamsulosin
- B. Overdiuresis by thiazides (Correct Answer)
- C. Toxic reaction to antibiotic
- D. Allergic reaction to antibiotic
- E. Hemorrhage
Diuretic classes and mechanisms Explanation: ***Overdiuresis by thiazides***
- The patient exhibits elevated **BUN** and **creatinine** (52 mg/dL and 2.1 mg/dL respectively), suggestive of **prerenal acute kidney injury**. The low **urine sodium** (13 mEq/L) and high **urine osmolality** (548 mOsm/kg) indicate appropriate renal response to hypovolemia, reflecting reduced renal perfusion.
- **Thiazide diuretics** can cause significant volume depletion, leading to prerenal injury, and the patient's decreased alertness is consistent with dehydration and potential electrolyte imbalances from aggressive diuresis.
*Forgetting to take tamsulosin*
- **Tamsulosin** is an alpha-blocker used for benign prostatic hyperplasia; forgetting it would lead to worsening urinary symptoms, not acute kidney injury or decreased alertness.
- While it can cause orthostatic hypotension, skipping a dose would likely improve, not worsen, blood pressure, and would not explain the observed lab values.
*Toxic reaction to antibiotic*
- While some antibiotics can cause **nephrotoxicity** (e.g., aminoglycosides, vancomycin), this would typically manifest with **acute tubular necrosis**, characterized by a high **urine sodium** and low **urine osmolality**, which contradicts the patient's lab findings.
- The patient was diagnosed with an infection three weeks ago; a toxic reaction usually occurs shortly after administration or with chronic high doses, not with such a delayed presentation without specific signs of organ damage beyond kidney injury.
*Allergic reaction to antibiotic*
- An **allergic reaction** to an antibiotic would likely present with symptoms such as rash, urticaria, angioedema, or anaphylaxis, none of which are described.
- An allergic reaction would not directly cause the patient's specific pattern of **prerenal acute kidney injury** as indicated by the urine and serum labs.
*Hemorrhage*
- A **hemorrhage** could cause **prerenal acute kidney injury** due to hypovolemia, but there is no mention of trauma or signs of bleeding (e.g., melena, hematochezia, ecchymoses), and the patient's daughter did not report any.
- While hemorrhage is a possibility in elderly patients, the history of recent diuretic use provides a more direct and plausible explanation for the observed fluid status and renal parameters.
Diuretic classes and mechanisms US Medical PG Question 3: A 66-year-old man with congestive heart failure presents to the emergency department complaining of worsening shortness of breath. These symptoms have worsened over the last 3 days. He has a blood pressure of 126/85 mm Hg and heart rate of 82/min. Physical examination is notable for bibasilar crackles. A chest X-ray reveals bilateral pulmonary edema. His current medications include metoprolol succinate and captopril. You wish to add an additional medication targeted towards his symptoms. Of the following, which statement is correct regarding loop diuretics?
- A. Loop diuretics can cause metabolic acidosis
- B. Loop diuretics can cause ammonia toxicity
- C. Loop diuretics can cause hyperlipidemia
- D. Loop diuretics decrease sodium, magnesium, and chloride but increase calcium
- E. Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter (Correct Answer)
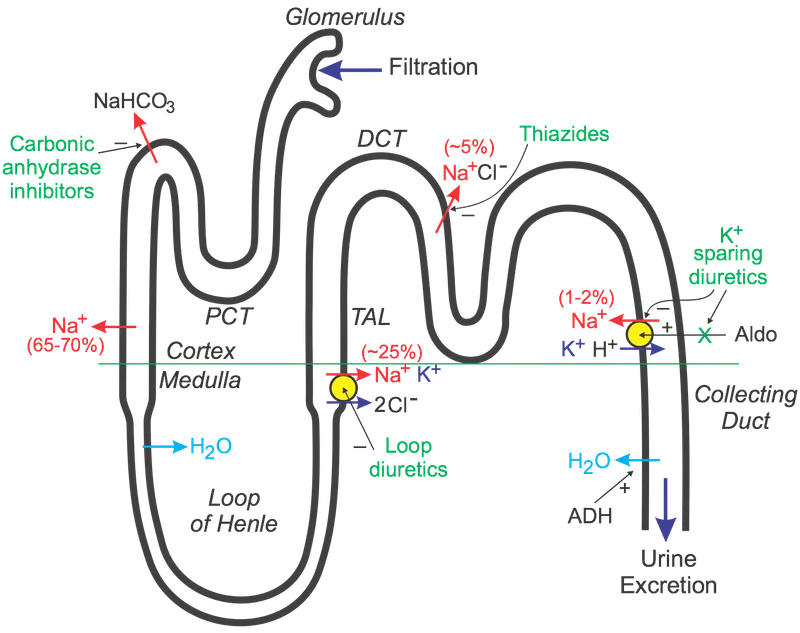
Diuretic classes and mechanisms Explanation: ***Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter***
- Loop diuretics, like furosemide, directly block the **Na+/K+/2Cl- cotransporter** in the **thick ascending limb of the loop of Henle**, preventing the reabsorption of these ions.
- This inhibition leads to increased excretion of water, sodium, potassium, and chloride, which is beneficial in conditions like **pulmonary edema** due to **congestive heart failure**.
*Loop diuretics can cause metabolic acidosis*
- Loop diuretics typically cause **metabolic alkalosis**, not acidosis, because they increase the excretion of hydrogen ions and potassium, leading to a compensatory increase in bicarbonate.
- The increased delivery of sodium to the collecting duct can also stimulate potassium and hydrogen secretion, contributing to alkalosis.
*Loop diuretics can cause ammonia toxicity*
- Loop diuretics do not directly cause **ammonia toxicity**; this is more commonly associated with conditions like **hepatic encephalopathy** or certain other medications.
- Their primary mechanism of action is on renal ion transport, not ammonia metabolism.
*Loop diuretics can cause hyperlipidemia*
- While some diuretics like **thiazide diuretics** can cause mild increases in **lipid levels**, loop diuretics are not typically associated with significant **hyperlipidemia**.
- The most common metabolic side effects of loop diuretics include electrolyte imbalances.
*Loop diuretics decrease sodium, magnesium, and chloride but increase calcium*
- Loop diuretics decrease the reabsorption of **sodium**, **magnesium**, and **chloride**, leading to their increased excretion.
- They also increase **calcium excretion** (cause hypocalcemia), rather than increasing serum calcium levels, by inhibiting its reabsorption in the thick ascending limb of the loop of Henle.
Diuretic classes and mechanisms US Medical PG Question 4: A 33-year-old male presents to his primary care physician with complaints of headaches and muscle weakness. His physical exam is entirely within normal limits except for a blood pressure of 150/95. Subsequent routine blood lab work showed a sodium level of 146 and potassium level of 3.0. What is the best pharmacological therapy for this patient?
- A. Fludrocortisone
- B. Spironolactone (Correct Answer)
- C. Lisinopril
- D. Hydrochlorothiazide
- E. Propranolol
Diuretic classes and mechanisms Explanation: ***Spironolactone***
- This patient's symptoms (hypertension, **hypokalemia**, and **hypernatremia**) are classic for **primary hyperaldosteronism**. **Spironolactone** is an **aldosterone antagonist** that blocks the effects of aldosterone, effectively treating both the hypertension and electrolyte abnormalities.
- Aldosterone antagonists directly target the underlying pathology by countering the excessive mineralocorticoid activity, making it the most appropriate pharmacological therapy for primary hyperaldosteronism.
*Fludrocortisone*
- **Fludrocortisone** is a **mineralocorticoid** used to *replace* aldosterone in conditions like Addison's disease where aldosterone production is deficient.
- Administering fludrocortisone in a patient with excessive aldosterone (primary hyperaldosteronism) would worsen their condition by exacerbating hypertension, hypokalemia, and hypernatremia.
*Lisinopril*
- **Lisinopril** is an **ACE inhibitor** that works by blocking the conversion of angiotensin I to angiotensin II, leading to vasodilation and decreased aldosterone secretion.
- While ACE inhibitors can lower blood pressure, they are not the primary treatment for **primary hyperaldosteronism** because the condition involves autonomous aldosterone production **independent of the renin-angiotensin-aldosterone system (RAAS)**.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that works by increasing the excretion of sodium and water, thereby lowering blood pressure.
- However, thiazide diuretics also increase potassium excretion, which would further worsen the patient's existing **hypokalemia**, making it an inappropriate choice.
*Propranolol*
- **Propranolol** is a **non-selective beta-blocker** that lowers blood pressure by reducing heart rate and cardiac output.
- While useful for hypertension, beta-blockers do not address the underlying electrolyte disturbances characteristic of **primary hyperaldosteronism** and are not a first-line treatment for this specific condition.
Diuretic classes and mechanisms US Medical PG Question 5: A 64-year-old woman is brought to the emergency department because of a 1-week history of progressive shortness of breath, lower extremity edema, and a 4-kg (9-lb) weight gain. She has ischemic cardiomyopathy and rheumatoid arthritis. Her respirations are 27/min. Examination shows pitting edema of the lower extremities and crackles over both lower lung fields. Therapy is initiated with intravenous furosemide. After 2 hours, urine output is minimal. Concomitant treatment with which of the following drugs is most likely to have contributed to treatment failure?
- A. Sulfasalazine
- B. Digoxin
- C. Prednisone
- D. Infliximab
- E. Diclofenac (Correct Answer)
Diuretic classes and mechanisms Explanation: ***Diclofenac***
- **NSAIDs** like diclofenac can cause **sodium and water retention** and reduce the effectiveness of loop diuretics like furosemide by inhibiting prostaglandin synthesis in the kidneys.
- This patient's symptoms of **heart failure exacerbation** (shortness of breath, edema, weight gain, crackles) and minimal urine output despite furosemide suggest drug-induced diuretic resistance.
*Sulfasalazine*
- This drug is used for **rheumatoid arthritis** and inflammatory bowel disease, but it does not typically interfere with diuretic action or cause fluid retention.
- Its mechanism involves anti-inflammatory properties, not directly affecting renal hemodynamics or diuretic efficacy.
*Digoxin*
- Digoxin is used to improve **cardiac contractility** and does not directly cause fluid retention or diminish the effects of loop diuretics.
- While it has a narrow therapeutic index, it does not antagonize furosemide's action.
*Prednisone*
- Prednisone is a **corticosteroid** that can cause **fluid retention** due to its mineralocorticoid effects, but it is not known to directly inhibit the action of loop diuretics to this extent.
- Its use in rheumatoid arthritis would primarily suppress inflammation, not directly cause diuretic resistance in acute heart failure.
*Infliximab*
- Infliximab is a **TNF-alpha inhibitor** used in rheumatoid arthritis; it can rarely exacerbate heart failure by its mechanism of action but does not directly interfere with the efficacy of loop diuretics.
- It does not cause fluid retention through renal mechanisms or reduce the renal response to furosemide.
Diuretic classes and mechanisms US Medical PG Question 6: A 23-year-old man presents with a blunt force injury to the head from a baseball bat. He is currently unconscious, although his friends say he was awake and speaking with them en route to the hospital. He has no significant past medical history and takes no current medications. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 165/85 mm Hg, pulse 50/min, and respiratory rate 19/min. On physical examination, there is a blunt force injury to the left temporoparietal region approximately 10.1–12.7 cm (4–5 in) in diameter. There is anisocoria of the left pupil, which is unresponsive to light. The patient is intubated and fluid resuscitation is initiated. A noncontrast computed tomography (CT) scan of the head is acquired and shown in the exhibit (see image). Which of the following is the most appropriate medical treatment for this patient?
- A. Placement of a ventriculoperitoneal (VP) shunt
- B. Acetazolamide
- C. Placing the head of the bed at 0 degrees
- D. Maintain a PaCO2 of 24 mm Hg
- E. Mannitol (Correct Answer)
Diuretic classes and mechanisms Explanation: ***Mannitol***
- The patient presents with classic signs of **epidural hematoma** (lucid interval, ipsilateral pupillary dilation, contralateral hemiparesis), and the CT scan confirms a large, biconvex hemorrhage compressing the brain.
- **Mannitol** is an osmotic diuretic used to rapidly **reduce intracranial pressure (ICP)** by drawing water from the brain into the vasculature, which can be life-saving in cases of acute brain herniation.
*Placement of a ventriculoperitoneal (VP) shunt*
- A VP shunt is used for long-term management of **hydrocephalus** due to impaired CSF absorption or flow, not for acute, traumatic hemorrhage and mass effect.
- Placing a shunt would not address the immediate, life-threatening mass effect from the epidural hematoma.
*Acetazolamide*
- **Acetazolamide** is a carbonic anhydrase inhibitor that reduces CSF production, primarily used for conditions like chronic **idiopathic intracranial hypertension** (pseudotumor cerebri) or hydrocephalus.
- It is not an effective treatment for the rapid reduction of ICP in the setting of acute intracranial hemorrhage and mass effect.
*Placing the head of the bed at 0 degrees*
- Keeping the head of the bed flat (at 0 degrees) is generally discouraged in patients with **elevated ICP** as it can worsen cerebral venous outflow and increase ICP.
- Elevating the head of the bed to **30 degrees** is standard practice to promote venous drainage and reduce ICP.
*Maintain a PaCO2 of 24 mm Hg*
- While **hyperventilation** to lower PaCO2 can cause cerebral vasoconstriction and reduce ICP, maintaining a PaCO2 as low as 24 mm Hg (severe hyperventilation) is typically reserved for **brief periods** in severe, refractory ICP elevation.
- Prolonged severe hyperventilation can lead to **cerebral ischemia** due to excessive vasoconstriction and is generally not the first-line or sustained management strategy.
Diuretic classes and mechanisms US Medical PG Question 7: A 4-day-old boy is monitored in the well baby nursery. He was born to a G1P1 mother at 36 weeks gestation. The child is doing well, and the mother is recovering from vaginal delivery. On physical exam, there is an arousable infant who is crying vigorously and is mildly cyanotic. A red reflex is noted bilaterally on ophthalmologic exam. The infant's fontanelle is soft, and his sucking reflex is present. A positive Babinski sign is noted on physical exam bilaterally. A continuous murmur is auscultated on cardiac exam. Which of the following would most likely have prevented the abnormal finding in this infant?
- A. Prostaglandins
- B. Indomethacin (Correct Answer)
- C. Folic acid
- D. Betamethasone
- E. Oxygen therapy
Diuretic classes and mechanisms Explanation: ***Indomethacin***
- The continuous murmur and mild cyanosis in a premature infant (36 weeks gestation) suggest a **patent ductus arteriosus (PDA)**.
- **Prophylactic indomethacin** given to premature infants shortly after birth can prevent the development of a symptomatic PDA by inhibiting prostaglandin synthesis, which promotes ductal closure.
- Indomethacin, a **prostaglandin inhibitor**, prevents prostaglandin-mediated vasodilation and facilitates closure of the ductus arteriosus in the early postnatal period.
- This is particularly important in premature infants who are at higher risk for persistent PDA due to immature ductal responsiveness.
*Prostaglandins*
- **Prostaglandins** (specifically PGE1) are used to *keep* the ductus arteriosus open, which is desirable in certain cyanotic congenital heart defects that require ductal patency for systemic or pulmonary blood flow (e.g., transposition of great arteries, pulmonary atresia).
- Administering prostaglandins in this case would worsen the **patent ductus arteriosus** by preventing its closure.
*Folic acid*
- **Folic acid** supplementation during pregnancy is crucial for preventing neural tube defects such as spina bifida and anencephaly.
- It has no role in preventing or treating a **patent ductus arteriosus** or other cardiovascular abnormalities in newborns.
*Betamethasone*
- **Betamethasone** is a corticosteroid given to pregnant mothers at risk of preterm delivery (between 24-34 weeks) to accelerate fetal lung maturity and reduce respiratory distress syndrome.
- While it improves neonatal outcomes in premature infants, it does not directly prevent the development of **patent ductus arteriosus**.
*Oxygen therapy*
- **Oxygen therapy** is used to treat hypoxemia and improve tissue oxygenation in cyanotic infants.
- While increased oxygen tension can contribute to ductal constriction, oxygen therapy alone is not a primary or reliable preventative measure for PDA in premature infants.
- Indomethacin remains the definitive pharmacologic intervention for prevention of symptomatic PDA.
Diuretic classes and mechanisms US Medical PG Question 8: A 55-year-old man presents after an episode of severe left ankle pain. The pain has resolved, but he decided to come in for evaluation as he has had pain like this before. He says he has experienced similar episodes of intense pain in the same ankle and his left knee in the past, which he associates with eating copious amounts of fatty food during parties. On one occasion the pain was so excruciating, he went to the emergency room, where an arthrocentesis was performed, revealing needle-shaped negatively birefringent crystals and a high neutrophil count in the synovial fluid. His past medical history is relevant for essential hypertension which is managed with hydrochlorothiazide 20 mg/day. His vital signs are stable, and his body temperature is 36.5°C (97.7°F). Physical examination shows a minimally tender left ankle with full range of motion. Which of the following is the most appropriate long-term treatment in this patient?
- A. Colchicine
- B. Intra-articular steroid injection
- C. Nonsteroidal antiinflammatory drugs (NSAIDs)
- D. Xanthine oxidase inhibitor (Correct Answer)
- E. Uricosuric drug
Diuretic classes and mechanisms Explanation: ***Xanthine oxidase inhibitor***
- The patient's presentation with recurrent episodes of severe joint pain, association with fatty foods, and the finding of **negatively birefringent, needle-shaped crystals** in synovial fluid are classic for **gout**. Xanthine oxidase inhibitors like **allopurinol** or **febuxostat** are the most appropriate **long-term treatment** to reduce uric acid production and prevent future attacks.
- His use of **hydrochlorothiazide**, a thiazide diuretic, further increases the risk of gout by increasing renal uric acid reabsorption, reinforcing the need for urate-lowering therapy.
*Colchicine*
- **Colchicine** is primarily used for the **acute treatment** or **prophylaxis of gout flares** during the initiation of urate-lowering therapy. It does not lower serum uric acid levels.
- While effective in managing acute symptoms, it is not a long-term solution for preventing gout attacks in a patient with recurrent flares and confirmed crystal deposition.
*Intra-articular steroid injection*
- **Intra-articular steroid injections** can effectively treat **acute gout flares**, especially when systemic NSAIDs or colchicine are contraindicated or ineffective.
- However, this is an acute treatment for symptom relief and does not address the underlying **hyperuricemia** or prevent future episodes, making it unsuitable as a long-term strategy for recurrent gout.
*Nonsteroidal antiinflammatory drugs (NSAIDs)*
- **NSAIDs** are effective in treating the **acute inflammation and pain** of a gout flare. The patient's current pain has resolved, so NSAIDs are not indicated at this time.
- Similar to colchicine, NSAIDs treat the symptoms of an acute attack but do not lower uric acid levels or prevent future episodes.
*Uricosuric drug*
- **Uricosuric drugs** (e.g., probenecid) increase the excretion of uric acid via the kidneys. They are indicated for patients who **underexcrete uric acid** and have good renal function.
- These drugs are contraindicated in patients with **renal impairment** or a history of **uric acid kidney stones**. Without knowing the patient's 24-hour uric acid excretion or renal function in detail, and considering his hypertension and potential renal impact of diuretics, a xanthine oxidase inhibitor is generally preferred as first-line long-term therapy.
Diuretic classes and mechanisms US Medical PG Question 9: A 64-year-old man presents to his physician 6 months after experiencing a myocardial infarction. The patient currently denies any symptoms and is only in for a check up. The patient's past medical history is notable for diabetes (type II), obesity, hypertension and cyclothymia. His current medications are hydrochlorothiazide, metoprolol, metformin, insulin, fluoxetine, and fish oil. On physical exam you note a calm elderly man who is moderately obese and in no current distress. The patient's cardiovascular exam is notable for a S4 heart sound. The patients lab work is below.
Serum:
Na+: 140 mEq/L
Cl-: 100 mEq/L
K+: 4.4 mEq/L
HCO3-: 23 mEq/L
BUN: 20 mg/dL
Glucose: 120 mg/dL
Creatinine: 1.6 mg/dL
Ca2+: 10.1 mg/dL
AST: 11 U/L
ALT: 9 U/L
Cholesterol: 190 mg/dL
Triglycerides: 150 mg/dL
High density lipoprotein associated cholesterol: 11 mg/dL
Low density lipoprotein associated cholesterol: 149 mg/dL
The physician updates the patient's medication regimen after this visit.
The patient returns 2 weeks later and presents his blood glucose diary to you demonstrating a mean blood glucose of 167 mg/dL. He is also complaining of flushing that occurs occasionally but otherwise is doing well. Which of the following is most likely to alleviate this patient's current symptom?
- A. Irreversible inactivation of cyclooxygenase (Correct Answer)
- B. Inhibition of angiotensin II formation
- C. GLUT-4 insertion in cell membranes
- D. Decreased inhibition of HMG CoA reductase
- E. Discontinue diuretic that inhibits Na/Cl cotransporter
Diuretic classes and mechanisms Explanation: ***Irreversible inactivation of cyclooxygenase***
- The patient is likely experiencing **flushing** due to **niacin** (nicotinic acid) therapy, which is often used to lower **LDL-C** and **triglycerides** and raise **HDL-C**. Niacin-induced flushing is mediated by **prostaglandins**, specifically **PGD2**, which can be alleviated by irreversible inactivation of COX with **aspirin**.
- Given his history of **myocardial infarction**, poorly controlled diabetes, and dyslipidemia (HDL-C of 11 mg/dL, LDL-C 149 mg/dL), a lipid-modifying agent like niacin would be a reasonable addition to his regimen.
*Inhibition of angiotensin II formation*
- This refers to the mechanism of **ACE inhibitors** or **ARBs**, which are used to manage hypertension and protect the kidneys, especially in patients with diabetes and post-MI.
- While beneficial for this patient's overall cardiovascular health, it does not directly address the symptom of **flushing**.
*GLUT-4 insertion in cell membranes*
- This mechanism is associated with **thiazolidinediones (TZDs)**, a class of antidiabetic drugs that improve **insulin sensitivity**.
- While improved glucose control (mean 167 mg/dL) is needed for this patient, GLUT-4 insertion does not alleviate flushing.
*Decreased inhibition of HMG CoA reductase*
- This response implies stopping or reducing the dose of a **statin**, which inhibits **HMG-CoA reductase** and is crucial for lowering LDL-C.
- The patient's LDL-C of 149 mg/dL is still elevated, and statins are a cornerstone of post-MI therapy; thus, decreasing their inhibition would be detrimental to his cardiovascular risk.
*Discontinue diuretic that inhibits Na/Cl cotransporter*
- The patient is currently on **hydrochlorothiazide**, which inhibits the **Na/Cl cotransporter** in the distal convoluted tubule and helps manage his hypertension.
- Discontinuing this medication would likely worsen his blood pressure and has no direct effect on flushing.
Diuretic classes and mechanisms US Medical PG Question 10: A 67-year-old man presents to his primary care physician for a decline in his hearing that he noticed over the past week. The patient has a past medical history of hypertension and diabetes mellitus and was recently diagnosed with bladder cancer which is currently appropriately being treated. The patient is a hunter and often goes shooting in his spare time. His recent sick contacts include his grandson who is being treated with amoxicillin for ear pain. Physical exam is notable for decreased hearing bilaterally. The Weber test does not localize to either ear, and the Rinne test demonstrates air conduction is louder than bone conduction. Which of the following is the most likely etiology for this patient's hearing loss?
- A. Otitis externa
- B. Presbycusis
- C. Otosclerosis
- D. Medication regimen (Correct Answer)
- E. Otitis media
Diuretic classes and mechanisms Explanation: ***Medication regimen***
- The patient's history of bladder cancer treatment suggests recent exposure to **chemotherapeutic agents**, such as **cisplatin**, which are known to be **ototoxic**.
- A **sudden decline in hearing** over the past week points to an acute cause, such as drug-induced hearing loss.
*Otitis externa*
- This condition typically presents with **ear pain**, **pruritus**, and **discharge**, none of which are mentioned in the patient's presentation.
- The **Weber and Rinne test results** (normal AC > BC, no lateralization) are inconsistent with a conductive hearing loss typically associated with otitis externa.
*Presbycusis*
- **Presbycusis** is an age-related **sensorineural hearing loss** that typically develops **gradually over years**, not suddenly over a week.
- While the patient's age (67) is a risk factor, the acute onset makes this diagnosis less likely.
*Otosclerosis*
- **Otosclerosis** usually causes a **progressive conductive hearing loss**, often starting in young adulthood.
- The **Weber and Rinne test results** (normal AC > BC, no lateralization) are inconsistent with a conductive hearing loss.
*Otitis media*
- **Otitis media** typically presents with **ear pain**, **fullness**, and often **fever** or **discharge**, which are absent in this patient.
- The **Weber and Rinne test results** (normal AC > BC, no lateralization) are inconsistent with the conductive hearing loss that would be expected with otitis media.
More Diuretic classes and mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.