Beta-blockers (cardioselective/non-selective) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Beta-blockers (cardioselective/non-selective). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 1: A 34-year-old female presents to the emergency room with headache and palpitations. She is sweating profusely and appears tremulous on exam. Vital signs are as follows: HR 120, BP 190/110, RR 18, O2 99% on room air, and Temp 37C. Urinary metanephrines and catechols are positive. Which of the following medical regimens is contraindicated as a first-line therapy in this patient?
- A. Labetalol
- B. Propranolol (Correct Answer)
- C. Nitroprusside
- D. Lisinopril
- E. Phenoxybenzamine
Beta-blockers (cardioselective/non-selective) Explanation: ***Propranolol***
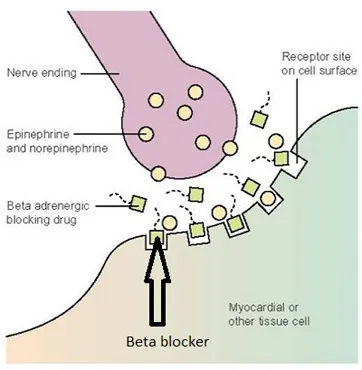
- This patient's presentation with headache, palpitations, sweating, hypertension, and tachycardia, along with elevated urinary metanephrines and catechols, is highly suggestive of a **pheochromocytoma**.
- **Pure beta-blockers** (like propranolol) are **absolutely contraindicated** as first-line therapy because blocking $\beta_2$ receptors without initial $\alpha$-blockade leads to unopposed $\alpha$-adrenergic stimulation, causing severe **vasoconstriction** and a dangerous **hypertensive crisis**.
- This is the **most contraindicated** option among the choices listed.
*Labetalol*
- Labetalol is a **non-selective $\beta$-blocker with some $\alpha_1$-blocking activity** (β:α blockade ratio ~7:1).
- While **not recommended** as first-line monotherapy in pheochromocytoma due to predominant beta-blockade, it has **some alpha-blocking properties** that distinguish it from pure beta-blockers.
- In practice, it's typically avoided as initial therapy, but it carries **less risk** than pure beta-blockers because of its partial alpha-blockade.
- Some sources consider it relatively contraindicated, but propranolol (pure beta-blocker) is more definitively contraindicated.
*Nitroprusside*
- **Nitroprusside** is a potent **vasodilator** that acts on both arterial and venous beds, making it effective for **rapid blood pressure reduction** in hypertensive emergencies.
- It is **not contraindicated** and can be used in a pheochromocytoma crisis for acute blood pressure control, though it should ideally be combined with alpha-blockade.
- It does not directly address catecholamine effects but provides symptomatic BP control.
*Lisinopril*
- **Lisinopril** is an **ACE inhibitor**, which works by preventing the conversion of angiotensin I to angiotensin II, leading to vasodilation and reduced aldosterone secretion.
- It is **not contraindicated** but is **inappropriate** as first-line therapy in pheochromocytoma crisis because it does not directly counteract the massive catecholamine release.
- It would be ineffective for managing the acute hypertensive emergency.
*Phenoxybenzamine*
- **Phenoxybenzamine** is an **irreversible, non-selective $\alpha$-adrenergic blocker** that is the **gold standard first-line therapy** for pheochromocytoma.
- It effectively blocks the vasoconstrictive effects of catecholamines, allowing for adequate blood pressure control before any $\beta$-blockade is considered.
- This is the **correct first-line medication**, not contraindicated.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 2: A 55-year-old woman comes to the physician because of involuntary hand movements that improve with alcohol consumption. Physical examination shows bilateral hand tremors that worsen when the patient is asked to extend her arms out in front of her. The physician prescribes a medication that is associated with an increased risk of bronchospasms. This drug has which of the following immediate effects on the cardiovascular system?
Stroke volume | Heart rate | Peripheral vascular resistance
- A. ↓ ↓ ↓
- B. ↓ ↓ ↑ (Correct Answer)
- C. ↓ ↑ ↑
- D. ↑ ↑ ↑
- E. ↑ ↑ ↓
Beta-blockers (cardioselective/non-selective) Explanation: ***↓ ↓ ↑***
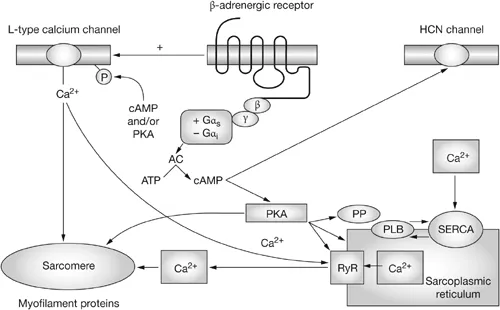
- This patient likely has **essential tremor**, which is characterized by **bilateral hand tremors** that improve with alcohol and worsen with intention (postural tremor). The prescribed medication is a **beta-blocker** (e.g., propranolol), which is associated with an increased risk of bronchospasms due to blocking **beta-2 receptors** in the airways.
- Beta-blockers **decrease heart rate** (negative chronotropic effect) and **stroke volume** (negative inotropic effect) by blocking beta-1 receptors in the heart, reducing cardiac output.
- **Peripheral vascular resistance increases** acutely due to: (1) **unopposed alpha-1 adrenergic tone** in blood vessels (loss of beta-2 mediated vasodilation), and (2) baroreceptor-mediated reflex vasoconstriction in response to decreased cardiac output. This helps maintain blood pressure despite reduced cardiac output.
*↓ ↓ ↓*
- While beta-blockers decrease **heart rate** and **stroke volume**, peripheral vascular resistance does not decrease acutely. A decrease in all three parameters would cause severe hypotension.
- The loss of beta-2 receptor-mediated vasodilation and baroreceptor reflexes lead to increased, not decreased, peripheral vascular resistance.
*↓ ↑ ↑*
- Beta-blockers **decrease heart rate** through beta-1 blockade, not increase it. This is their primary cardiac mechanism of action.
- An increase in heart rate would be expected with sympathomimetic drugs or anticholinergics, not beta-blockers.
*↑ ↑ ↑*
- This combination indicates increased cardiovascular activity, which is the opposite effect of **beta-blockers**.
- Beta-blockers reduce heart rate and stroke volume by blocking beta-1 receptors; they do not increase these parameters.
- This pattern would suggest sympathetic activation or administration of an adrenergic agonist.
*↑ ↑ ↓*
- Beta-blockers **decrease** (not increase) both heart rate and stroke volume through beta-1 receptor blockade.
- While decreased peripheral vascular resistance occurs with vasodilators, beta-blockers acutely **increase** PVR due to unopposed alpha-adrenergic tone.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 3: A 55-year-old man comes to the physician because of episodic retrosternal chest pain and shortness of breath for the past 6 months. His symptoms occur when he takes long walks or climbs stairs but resolve promptly with rest. He has a history of chronic obstructive pulmonary disease, for which he takes ipratropium bromide. His pulse is 81/min and blood pressure is 153/82 mm Hg. Physical examination shows mild expiratory wheezing over both lungs. Additional treatment with a beta blocker is considered. Which of the following agents should be avoided in this patient?
- A. Betaxolol
- B. Esmolol
- C. Bisoprolol
- D. Atenolol
- E. Labetalol (Correct Answer)
Beta-blockers (cardioselective/non-selective) Explanation: ***Labetalol***
- **Labetalol** is a **non-selective beta-blocker** with additional **alpha-1 blocking activity**.
- Its **non-selective beta-blocking** effects can exacerbate **bronchoconstriction** in patients with **COPD**, leading to worsening respiratory symptoms.
*Betaxolol*
- **Betaxolol** is a **beta-1 selective blocker (cardioselective)**, meaning it primarily targets the heart.
- While no beta-blocker is entirely safe in **COPD**, cardioselective agents are generally preferred due to their reduced risk of **bronchospasm**.
*Esmolol*
- **Esmolol** is an **ultra-short-acting**, **beta-1 selective blocker** often used for acute cardiac conditions.
- Its **cardioselective nature** and rapid metabolism make it relatively safer in patients with **COPD** compared to non-selective agents.
*Bisoprolol*
- **Bisoprolol** is a **highly beta-1 selective blocker** commonly used for chronic cardiac conditions.
- Its high **cardioselectivity** minimizes its impact on **bronchial beta-2 receptors**, making it a safer option for patients with **COPD**.
*Atenolol*
- **Atenolol** is a **beta-1 selective blocker** used for conditions like hypertension and angina.
- Like other cardioselective beta-blockers, it has a lower risk of causing **bronchoconstriction** in patients with **COPD** compared to non-selective agents.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 4: A 65-year-old male with a history of CHF presents to the emergency room with shortness of breath, lower leg edema, and fatigue. He is diagnosed with acute decompensated congestive heart failure, was admitted to the CCU, and treated with a medication that targets beta-1 adrenergic receptors preferentially over beta-2 adrenergic receptors. The prescribing physician explained that this medication would only be used temporarily as its efficacy decreases within 2-3 days due to receptor downregulation. Which of the following was prescribed?
- A. Epinephrine
- B. Norepinephrine
- C. Milrinone
- D. Isoproterenol
- E. Dobutamine (Correct Answer)
Beta-blockers (cardioselective/non-selective) Explanation: ***Dobutamine***
- **Dobutamine** is a beta-1 adrenergic agonist preferentially acting on beta-1 receptors in the heart, increasing contractility and heart rate during acute decompensated heart failure.
- Its efficacy reduces over time due to **receptor downregulation**, making it effective for only short-term use, typically less than 72 hours.
*Epinephrine*
- **Epinephrine** is a non-selective adrenergic agonist acting on both alpha and beta receptors, causing vasoconstriction and bronchodilation in addition to cardiac stimulation.
- It is typically used in emergency situations like **cardiac arrest** and **anaphylaxis**, not primarily for acute CHF exacerbation in this manner.
*Norepinephrine*
- **Norepinephrine** primarily acts on alpha-1 adrenergic receptors, causing significant vasoconstriction, and has some beta-1 agonistic effects.
- It is mainly used as a **vasopressor** in septic shock or severe hypotension to increase systemic vascular resistance, rather than directly improving cardiac output in decompensated CHF.
*Milrinone*
- **Milrinone** is a phosphodiesterase-3 inhibitor, increasing intracellular cAMP levels and leading to positive inotropy and vasodilation.
- While used in acute heart failure, its mechanism is distinct from adrenergic agonists, and its efficacy is not limited by a rapid receptor downregulation mechanism as described.
*Isoproterenol*
- **Isoproterenol** is a non-selective beta-adrenergic agonist, stimulating both beta-1 and beta-2 receptors, leading to increased heart rate and contractility, as well as bronchodilation and vasodilation.
- Due to its strong chronotropic effects and potential for severe arrhythmias and hypotension, it is rarely used in CHF and is primarily reserved for conditions like **bradycardia** or **torsades de pointes**.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 5: An investigator is studying the effects of different drugs on the contraction of cardiomyocytes. The myocytes are able to achieve maximal contractility with the administration of drug A. The subsequent administration of drug B produces the response depicted in the graph shown. Which of the following drugs is most likely to produce a response similar to that of drug B?
- A. Albuterol
- B. Phenoxybenzamine
- C. Pindolol (Correct Answer)
- D. Isoproterenol
- E. Propranolol
Beta-blockers (cardioselective/non-selective) Explanation: ***Pindolol***
- The graph shows drug B reducing the maximal contractility achieved by drug A, suggesting it is a **partial agonist** or a **competitive antagonist** that can exert some intrinsic activity. Pindolol is a **beta-blocker** with **intrinsic sympathomimetic activity (ISA)**, meaning it can partially stimulate beta-receptors while blocking full agonists.
- This **partial agonism** allows pindolol to reduce the effect of a stronger agonist (like drug A, if it's a full beta-agonist) but still provide some baseline stimulation, thus decreasing the maximal response rather than completely abolishing it.
*Albuterol*
- Albuterol is a **selective beta-2 adrenergic agonist** primarily used as a bronchodilator.
- It would increase contractility if beta-2 receptors were present and acted upon, but it would not reduce the maximal contraction from an existing strong agonist.
*Phenoxybenzamine*
- Phenoxybenzamine is an **irreversible alpha-adrenergic antagonist**.
- It would not directly affect cardiac contractility which is primarily mediated by beta-adrenergic receptors, nor would it produce the depicted effect on contractility.
*Isoproterenol*
- Isoproterenol is a **non-selective beta-adrenergic agonist**.
- As a full agonist, it would increase contractility and could even be drug A if drug A is a beta-agonist, but it would not reduce the maximal response of an established agonist.
*Propranolol*
- Propranolol is a **non-selective beta-adrenergic antagonist** without intrinsic sympathomimetic activity (ISA).
- It would act as a **full competitive antagonist**, completely blocking the effects of drug A if drug A is a beta-agonist, thus reducing contractility much more significantly than depicted, potentially to baseline or below.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 6: A 61-year-old man with longstanding diabetes and coronary artery disease presents to the ER with chest pain and dyspnea. The echocardiogram reveals moderate-to-severe mitral regurgitation and an ejection fraction of 27%. A chest X-ray shows bibasilar infiltrates. A new drug is added to his medication regimen, and the physician mentions urinary frequency, increased breast tissue development, and erectile dysfunction as possible side effects. What is the mechanism of action of this drug?
- A. Inhibits Na-Cl symporter on the distal convoluted tubule
- B. Inhibits epithelial Na-channels on the cortical collecting duct
- C. Inhibits mineralocorticoid receptor on the cortical collecting duct (Correct Answer)
- D. Inhibits Na-K-2Cl symporter on the ascending loop of Henle
- E. Inhibits beta-adrenergic receptors to decrease SA node automaticity
Beta-blockers (cardioselective/non-selective) Explanation: ***Inhibits mineralocorticoid receptor on the cortical collecting duct***
- The patient's presentation of **heart failure** (chest pain, dyspnea, low ejection fraction, bibasilar infiltrates, mitral regurgitation) along with the side effects of **urinary frequency**, **gynecomastia**, and **erectile dysfunction** are characteristic of **spironolactone** or **eplerenone**.
- These drugs are **aldosterone antagonists** that work by inhibiting the **mineralocorticoid receptor** in the cortical collecting duct, leading to diuresis and beneficial effects in heart failure.
*Inhibits Na-Cl symporter on the distal convoluted tubule*
- This describes the mechanism of action of **thiazide diuretics**, such as hydrochlorothiazide.
- While thiazides cause urinary frequency, they are not typically associated with gynecomastia or erectile dysfunction.
*Inhibits epithelial Na-channels on the cortical collecting duct*
- This mechanism describes **potassium-sparing diuretics** like amiloride and triamterene (not aldosterone antagonists).
- These drugs primarily prevent sodium reabsorption and potassium secretion, but they do not cause gynecomastia or erectile dysfunction as directly as spironolactone.
*Inhibits Na-K-2Cl symporter on the ascending loop of Henle*
- This is the mechanism of action for **loop diuretics**, such as furosemide or bumetanide.
- Loop diuretics are potent diuretics and cause urinary frequency but are not known to cause gynecomastia or erectile dysfunction.
*Inhibits beta-adrenergic receptors to decrease SA node automaticity*
- This mechanism describes **beta-blockers**, such as metoprolol or carvedilol, which are often used in heart failure management.
- While beta-blockers can cause erectile dysfunction, they do not cause urinary frequency or gynecomastia.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 7: A 48-year-old man presents to the emergency department with complaints of substernal chest pain for the past 1 hour. The pain is crushing in nature and radiates to his neck and left arm. He rates the pain as 7/10. He gives a history of similar episodes in the past that resolved with rest. He is a non-smoker and drinks alcohol occasionally. On physical examination, the temperature is 37.0°C (98.6°F), the pulse rate is 130/min and irregular, the blood pressure is 148/92 mm Hg, and the respiratory rate is 18/min. The physician immediately orders an electrocardiogram, the findings of which are consistent with an acute Q-wave myocardial infarction (MI). After appropriate emergency management, he is admitted to the medical floor. He develops atrial fibrillation on the second day of admission. He is given a β-adrenergic blocking agent for the arrhythmia. On discharge, he is advised to continue the medication for at least 2 years. Which of the following β-adrenergic blocking agents was most likely prescribed to this patient?
- A. Atenolol (Correct Answer)
- B. Penbutolol
- C. Acebutolol
- D. Pindolol
- E. Celiprolol
Beta-blockers (cardioselective/non-selective) Explanation: ***Atenolol***
- **Atenolol** is a **cardioselective β1-blocker** that is commonly prescribed for atrial fibrillation, especially post-MI, due to its efficacy in reducing heart rate and improving survival.
- It lacks **intrinsic sympathomimetic activity (ISA)**, which is crucial for the post-MI setting to ensure adequate beta-blockade and prevent adverse cardiac events.
*Penbutolol*
- **Penbutolol** is a **non-selective β-blocker** with **intrinsic sympathomimetic activity (ISA)**.
- Beta-blockers with ISA are generally **contraindicated or not preferred** in post-MI patients because their partial agonist activity might negate the protective effects of beta-blockade on myocardial oxygen demand and arrhythmogenesis.
*Acebutolol*
- **Acebutolol** is a **cardioselective β1-blocker** with **intrinsic sympathomimetic activity (ISA)**.
- Like other beta-blockers with ISA, acebutolol is **not typically recommended** for long-term use after myocardial infarction due to concerns about reduced cardioprotective benefits.
*Pindolol*
- **Pindolol** is a **non-selective β-blocker** with **intrinsic sympathomimetic activity (ISA)**.
- Its partial agonist activity can lead to **less reduction in heart rate and myocardial contractility** compared to beta-blockers without ISA, making it an unsuitable choice for post-MI management.
*Celiprolol*
- **Celiprolol** is a **cardioselective β1-blocker** that also has **β2-agonist properties** and **intrinsic sympathomimetic activity (ISA)**.
- Its β2-agonist and ISA effects make it **less desirable post-MI** as it may not provide the full cardioprotective benefits of a pure β-blocker.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 8: A 63-year-old woman presents with dyspnea on exertion. She reports that she used to work in her garden without any symptoms, but recently she started to note dyspnea and fatigue after working for 20–30 minutes. She has type 2 diabetes mellitus diagnosed 2 years ago but she does not take any medications preferring natural remedies. She also has arterial hypertension and takes torsemide 20 mg daily. The weight is 88 kg and the height is 164 cm. The vital signs include: blood pressure is 140/85 mm Hg, heart rate is 90/min, respiratory rate is 14/min, and the temperature is 36.6℃ (97.9℉). Physical examination is remarkable for increased adiposity, pitting pedal edema, and present S3. Echocardiography shows a left ventricular ejection fraction of 51%. The combination of which of the following medications would be a proper addition to the patient’s therapy?
- A. Metoprolol and indapamide
- B. Enalapril and bisoprolol (Correct Answer)
- C. Spironolactone and fosinopril
- D. Indapamide and amlodipine
- E. Valsartan and spironolactone
Beta-blockers (cardioselective/non-selective) Explanation: ***Enalapril and bisoprolol***
- This patient presents with **heart failure with preserved ejection fraction (HFpEF)**, characterized by symptoms of heart failure (dyspnea, fatigue, edema, S3 sound) with an LVEF >50%. She also has **uncontrolled hypertension** (BP 140/85) and a **heart rate of 90/min**.
- **Important:** Unlike HFrEF, **ACE inhibitors and beta-blockers have NOT demonstrated mortality benefit in HFpEF** (CHARM-Preserved, PEP-CHF trials). However, they remain important for **blood pressure control** and **symptom management** in patients with HFpEF and comorbid hypertension.
- **Enalapril** (ACE inhibitor) helps control blood pressure through reduction of preload and afterload. **Bisoprolol** (beta-blocker) provides **heart rate control** (patient's HR is 90/min) and further blood pressure reduction. Both medications address her inadequately controlled hypertension while managing symptoms.
- **Note:** Current guidelines emphasize SGLT2 inhibitors as first-line therapy for HFpEF (not offered here), along with diuretics for volume management (patient is already on torsemide) and aggressive treatment of comorbidities like hypertension and diabetes.
*Metoprolol and indapamide*
- Metoprolol is a beta-blocker that could help with rate and blood pressure control. However, **indapamide is a thiazide-like diuretic** that is redundant since the patient is already on **torsemide** (a loop diuretic) for volume management.
- This combination lacks an **ACE inhibitor or ARB** for optimal blood pressure control and neurohormonal modulation, which is important even in HFpEF for managing hypertension and its consequences.
*Spironolactone and fosinopril*
- **Spironolactone** (mineralocorticoid receptor antagonist) showed modest benefit in reducing HF hospitalizations in the TOPCAT trial for HFpEF. **Fosinopril** is an ACE inhibitor appropriate for blood pressure control.
- However, the patient has a **heart rate of 90/min**, indicating need for **rate control** which neither spironolactone nor fosinopril provides. A **beta-blocker would be more appropriate** to address both rate control and blood pressure.
- Additionally, while spironolactone has some evidence in HFpEF, the combination with an ACE inhibitor **without rate control** is suboptimal for this patient's presentation.
*Indapamide and amlodipine*
- **Indapamide** (thiazide-like diuretic) is **redundant** since the patient is already on torsemide. **Amlodipine** (calcium channel blocker) is effective for hypertension but can cause **peripheral edema**, which this patient already has (pitting pedal edema).
- **Calcium channel blockers are not recommended in heart failure** due to lack of mortality benefit and potential to worsen fluid retention. This combination does not address the underlying HFpEF pathophysiology or provide optimal symptom management.
*Valsartan and spironolactone*
- **Valsartan** (ARB) is appropriate for blood pressure control and is an alternative to ACE inhibitors. **Spironolactone** has modest evidence for reducing hospitalizations in HFpEF (TOPCAT trial).
- However, similar to the fosinopril/spironolactone combination, this lacks a **beta-blocker for heart rate control** (patient's HR is 90/min). Rate control is important for optimizing diastolic filling time in HFpEF and controlling blood pressure.
- While this combination has theoretical benefits, **enalapril and bisoprolol** better addresses both blood pressure control and rate control simultaneously.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 9: A 23-year-old active college student has a sudden loss of consciousness 40 minutes after he was playing basketball with his team. Cardiopulmonary resuscitation is administered by bystanders. On arrival of emergency medical professionals, he regains his consciousness. He has no past medical history. He does not smoke or drink alcohol. His family history is positive for a cousin who died suddenly in his youth. On physical examination, a systolic ejection murmur is audible on the left lower sternal border. ECG shows left ventricular hypertrophy and echocardiography shows asymmetric septal hypertrophy. Which of the following decreases the pressure gradient between the aorta and the left ventricle in this patient?
- A. Digoxin
- B. Metoprolol (Correct Answer)
- C. Nitroglycerin
- D. Forceful attempted exhalation against a closed airway
- E. High-dose diuretics
Beta-blockers (cardioselective/non-selective) Explanation: ***Metoprolol***
- This patient presents with symptoms and signs consistent with **hypertrophic cardiomyopathy (HCM)**: sudden syncope during exertion, family history of sudden death, systolic ejection murmur, and asymmetric septal hypertrophy on echocardiography.
- **Beta-blockers** like metoprolol decrease the **heart rate**, allowing for increased **diastolic filling time** and reducing the **contractility** of the left ventricle. This helps to reduce dynamic outflow obstruction and the pressure gradient.
*Digoxin*
- **Digoxin** is a **positive inotrope**, meaning it increases myocardial contractility.
- In HCM, increasing contractility would worsen the **left ventricular outflow tract obstruction** and thereby increase the pressure gradient.
*Nitroglycerin*
- **Nitroglycerin** is a **vasodilator** that primarily reduces preload and, to a lesser extent, afterload.
- Reducing **preload** can worsen the outflow tract obstruction in HCM by decreasing the left ventricular end-diastolic volume, leading to increased septal-mitral contact.
*Forceful attempted exhalation against a closed airway*
- This maneuver, known as the **Valsalva maneuver**, involves increased intra-thoracic pressure, which decreases **venous return to the heart** and subsequently reduces **preload**.
- A reduction in preload would exacerbate the **left ventricular outflow tract obstruction** and thus increase the pressure gradient in HCM.
*High-dose diuretics*
- **Diuretics** decrease the **blood volume** and **preload**.
- Similar to the Valsalva maneuver or nitroglycerin, a reduction in preload can worsen the dynamic outflow tract obstruction characteristic of HCM.
Beta-blockers (cardioselective/non-selective) US Medical PG Question 10: A 72-year-old man presents to the outpatient clinic today. He has New York Heart Association class III heart failure. His current medications include captopril 20 mg, furosemide 40 mg, potassium chloride 10 mg twice daily, rosuvastatin 20 mg, and aspirin 81 mg. He reports that he generally feels well and has not had any recent worsening of his symptoms. His blood pressure is 132/85 mm Hg and heart rate is 84/min. Physical examination is unremarkable except for trace pitting edema of the bilateral lower extremities. What other medication should be added to his heart failure regimen?
- A. Losartan
- B. Metoprolol tartrate
- C. Isosorbide dinitrate/hydralazine
- D. Metoprolol succinate (Correct Answer)
- E. Digoxin
Beta-blockers (cardioselective/non-selective) Explanation: ***Metoprolol succinate***
- Current guidelines recommend adding a **beta-blocker** (specifically metoprolol succinate, carvedilol, or bisoprolol) as part of guideline-directed medical therapy (GDMT) for **NYHA class II-IV heart failure with reduced ejection fraction (HFrEF)**.
- This patient is already on an **ACE inhibitor and diuretic** but is missing a **beta-blocker**, which is a cornerstone of HFrEF therapy.
- Beta-blockers **reduce mortality and morbidity** in HFrEF by counteracting chronic sympathetic activation, improving cardiac remodeling, and reducing heart rate.
- Metoprolol succinate is the **long-acting formulation** preferred for chronic heart failure management.
***Incorrect Option: Losartan***
- The patient is already on an **ACE inhibitor (captopril)**, which acts on the renin-angiotensin-aldosterone system.
- Adding an **ARB (angiotensin receptor blocker)** like losartan to an ACE inhibitor is generally not recommended due to increased risk of hyperkalemia, hypotension, and renal dysfunction without significant additional benefit.
- ARBs are typically used as an alternative when patients cannot tolerate ACE inhibitors (e.g., due to cough or angioedema).
***Incorrect Option: Metoprolol tartrate***
- While metoprolol tartrate is a beta-blocker, it is a **short-acting formulation** typically used for acute conditions like hypertension or angina.
- For **chronic heart failure management**, **long-acting beta-blockers** such as metoprolol succinate are preferred due to sustained therapeutic levels, better adherence, and proven mortality benefit in clinical trials.
***Incorrect Option: Isosorbide dinitrate/hydralazine***
- This combination is primarily indicated for **African American patients with NYHA class III-IV HFrEF** who remain symptomatic despite optimal therapy, or as an alternative in patients who cannot tolerate ACE inhibitors/ARBs.
- While the patient has class III heart failure, he is **not yet on a beta-blocker**, which is a more fundamental component of GDMT and should be added first.
- This combination is typically added as a fourth-line agent.
***Incorrect Option: Digoxin***
- Digoxin is considered for patients with **HFrEF who remain symptomatic** despite optimized therapy with ACE inhibitors/ARBs, beta-blockers, and mineralocorticoid receptor antagonists (MRAs).
- It primarily helps **improve symptoms and reduce hospitalizations** but does not reduce mortality.
- Since this patient is not yet on a beta-blocker, adding the beta-blocker takes priority.
More Beta-blockers (cardioselective/non-selective) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.