Alpha-blockers US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alpha-blockers. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alpha-blockers US Medical PG Question 1: A 68-year-old man with hypertension comes to the physician because of fatigue and difficulty initiating urination. He wakes up several times a night to urinate. He does not take any medications. His blood pressure is 166/82 mm Hg. Digital rectal examination shows a firm, non-tender, and uniformly enlarged prostate. Which of the following is the most appropriate pharmacotherapy?
- A. Finasteride
- B. α-Methyldopa
- C. Phenoxybenzamine
- D. Terazosin (Correct Answer)
- E. Tamsulosin
Alpha-blockers Explanation: ***Terazosin***
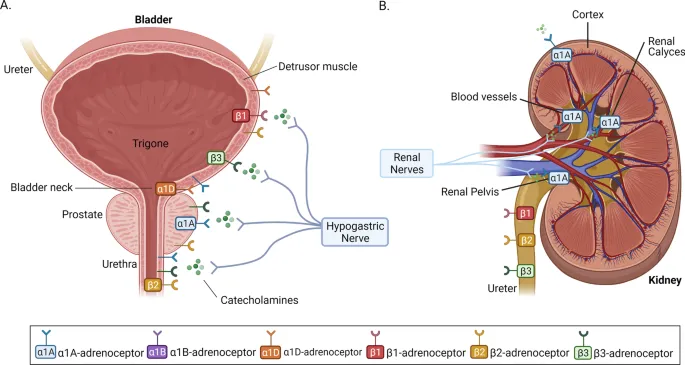
- **Terazosin** is an alpha-1 blocker that relaxes the smooth muscles in the prostate and bladder neck, improving urine flow and relieving symptoms of **benign prostatic hyperplasia (BPH)**.
- It also has the added benefit of lowering blood pressure, making it suitable for this patient with both **BPH** and **hypertension**.
*Finasteride*
- **Finasteride** is a 5-alpha reductase inhibitor that reduces prostate volume by inhibiting the conversion of testosterone to **dihydrotestosterone (DHT)**.
- While effective for **BPH**, it takes longer to show benefits (6-12 months) and does not address the patient's **hypertension**.
*α-Methyldopa*
- **α-Methyldopa** is a centrally acting alpha-2 adrenergic agonist used to treat **hypertension**, particularly in pregnancy.
- It does not have a direct effect on prostate smooth muscle and would not alleviate the patient's urinary symptoms.
*Phenoxybenzamine*
- **Phenoxybenzamine** is a non-selective, irreversible alpha-adrenergic blocker primarily used for **pheochromocytoma** to control blood pressure.
- Its non-selective nature and side effect profile make it less suitable for chronic management of **BPH** and **hypertension** compared to selective alpha-1 blockers.
*Tamsulosin*
- **Tamsulosin** is a selective alpha-1A adrenergic blocker that specifically targets the prostate, rapidly improving **BPH** symptoms with less effect on blood pressure.
- While it effectively treats **BPH**, unlike terazosin, it does not offer the additional advantage of lowering the patient's elevated blood pressure.
Alpha-blockers US Medical PG Question 2: A 34-year-old female presents to the emergency room with headache and palpitations. She is sweating profusely and appears tremulous on exam. Vital signs are as follows: HR 120, BP 190/110, RR 18, O2 99% on room air, and Temp 37C. Urinary metanephrines and catechols are positive. Which of the following medical regimens is contraindicated as a first-line therapy in this patient?
- A. Labetalol
- B. Propranolol (Correct Answer)
- C. Nitroprusside
- D. Lisinopril
- E. Phenoxybenzamine
Alpha-blockers Explanation: ***Propranolol***
- This patient's presentation with headache, palpitations, sweating, hypertension, and tachycardia, along with elevated urinary metanephrines and catechols, is highly suggestive of a **pheochromocytoma**.
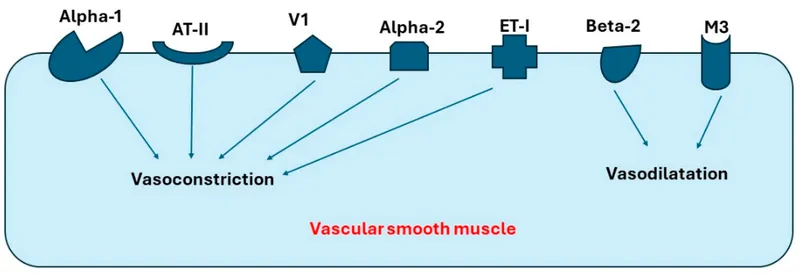
- **Pure beta-blockers** (like propranolol) are **absolutely contraindicated** as first-line therapy because blocking $\beta_2$ receptors without initial $\alpha$-blockade leads to unopposed $\alpha$-adrenergic stimulation, causing severe **vasoconstriction** and a dangerous **hypertensive crisis**.
- This is the **most contraindicated** option among the choices listed.
*Labetalol*
- Labetalol is a **non-selective $\beta$-blocker with some $\alpha_1$-blocking activity** (β:α blockade ratio ~7:1).
- While **not recommended** as first-line monotherapy in pheochromocytoma due to predominant beta-blockade, it has **some alpha-blocking properties** that distinguish it from pure beta-blockers.
- In practice, it's typically avoided as initial therapy, but it carries **less risk** than pure beta-blockers because of its partial alpha-blockade.
- Some sources consider it relatively contraindicated, but propranolol (pure beta-blocker) is more definitively contraindicated.
*Nitroprusside*
- **Nitroprusside** is a potent **vasodilator** that acts on both arterial and venous beds, making it effective for **rapid blood pressure reduction** in hypertensive emergencies.
- It is **not contraindicated** and can be used in a pheochromocytoma crisis for acute blood pressure control, though it should ideally be combined with alpha-blockade.
- It does not directly address catecholamine effects but provides symptomatic BP control.
*Lisinopril*
- **Lisinopril** is an **ACE inhibitor**, which works by preventing the conversion of angiotensin I to angiotensin II, leading to vasodilation and reduced aldosterone secretion.
- It is **not contraindicated** but is **inappropriate** as first-line therapy in pheochromocytoma crisis because it does not directly counteract the massive catecholamine release.
- It would be ineffective for managing the acute hypertensive emergency.
*Phenoxybenzamine*
- **Phenoxybenzamine** is an **irreversible, non-selective $\alpha$-adrenergic blocker** that is the **gold standard first-line therapy** for pheochromocytoma.
- It effectively blocks the vasoconstrictive effects of catecholamines, allowing for adequate blood pressure control before any $\beta$-blockade is considered.
- This is the **correct first-line medication**, not contraindicated.
Alpha-blockers US Medical PG Question 3: An investigator is studying a local anesthetic that causes increased sympathetic activity. When given intravenously, it causes euphoria and pupillary dilation. Which of the following is the most likely effect of this drug at the synaptic cleft?
- A. Increased release of norepinephrine
- B. Decreased reuptake of norepinephrine (Correct Answer)
- C. Decreased release of acetylcholine
- D. Increased release of serotonin
- E. Decreased breakdown of norepinephrine
Alpha-blockers Explanation: ***Decreased reuptake of norepinephrine***
- This drug causes **euphoria** and **pupillary dilation**, which are classic signs of increased **sympathetic nervous system** activity and **CNS stimulation**, consistent with enhanced **noradrenergic transmission**.
- Decreasing the **reuptake of norepinephrine** would increase its concentration in the **synaptic cleft**, leading to more prolonged activation of **alpha and beta adrenergic receptors**.
*Increased release of norepinephrine*
- While increased release would also elevate **norepinephrine** in the **synaptic cleft**, reuptake inhibition is a more common mechanism for drugs producing similar effects like **cocaine** and **amphetamine-like stimulants**.
- Without specific information, **reuptake inhibition** aligns better with the broad activation of **adrenergic receptors** and central effects described.
*Decreased release of acetylcholine*
- This would primarily affect **cholinergic systems**, and while some interactions exist, it does not directly explain the intense **adrenergic activation**, **euphoria**, and **pupillary dilation** observed.
- **Acetylcholine** primarily mediates **parasympathetic responses** and **skeletal muscle contraction**, not the sympathetic effects seen here.
*Increased release of serotonin*
- Increased **serotonin** release is associated with hallucinogenic effects and mood modulation, but it does not directly lead to the pronounced **pupillary dilation** and widespread **alpha/beta adrenergic receptor activation** described.
- The drug explicitly affects **adrenergic receptors**, making an effect on **norepinephrine** more direct.
*Decreased breakdown of norepinephrine*
- This mechanism, typically involving **MAO inhibitors**, would increase **norepinephrine** levels but is described as activating both **alpha and beta adrenergic receptors**, which points more towards a direct increase in synaptic availability rather than metabolic inhibition.
- While it prolongs the action of **norepinephrine**, the primary mechanism described for such a general stimulant often involves **reuptake inhibition** or **enhanced release**.
Alpha-blockers US Medical PG Question 4: A 55-year-old woman comes to the physician because of involuntary hand movements that improve with alcohol consumption. Physical examination shows bilateral hand tremors that worsen when the patient is asked to extend her arms out in front of her. The physician prescribes a medication that is associated with an increased risk of bronchospasms. This drug has which of the following immediate effects on the cardiovascular system?
Stroke volume | Heart rate | Peripheral vascular resistance
- A. ↓ ↓ ↓
- B. ↓ ↓ ↑ (Correct Answer)
- C. ↓ ↑ ↑
- D. ↑ ↑ ↑
- E. ↑ ↑ ↓
Alpha-blockers Explanation: ***↓ ↓ ↑***
- This patient likely has **essential tremor**, which is characterized by **bilateral hand tremors** that improve with alcohol and worsen with intention (postural tremor). The prescribed medication is a **beta-blocker** (e.g., propranolol), which is associated with an increased risk of bronchospasms due to blocking **beta-2 receptors** in the airways.
- Beta-blockers **decrease heart rate** (negative chronotropic effect) and **stroke volume** (negative inotropic effect) by blocking beta-1 receptors in the heart, reducing cardiac output.
- **Peripheral vascular resistance increases** acutely due to: (1) **unopposed alpha-1 adrenergic tone** in blood vessels (loss of beta-2 mediated vasodilation), and (2) baroreceptor-mediated reflex vasoconstriction in response to decreased cardiac output. This helps maintain blood pressure despite reduced cardiac output.
*↓ ↓ ↓*
- While beta-blockers decrease **heart rate** and **stroke volume**, peripheral vascular resistance does not decrease acutely. A decrease in all three parameters would cause severe hypotension.
- The loss of beta-2 receptor-mediated vasodilation and baroreceptor reflexes lead to increased, not decreased, peripheral vascular resistance.
*↓ ↑ ↑*
- Beta-blockers **decrease heart rate** through beta-1 blockade, not increase it. This is their primary cardiac mechanism of action.
- An increase in heart rate would be expected with sympathomimetic drugs or anticholinergics, not beta-blockers.
*↑ ↑ ↑*
- This combination indicates increased cardiovascular activity, which is the opposite effect of **beta-blockers**.
- Beta-blockers reduce heart rate and stroke volume by blocking beta-1 receptors; they do not increase these parameters.
- This pattern would suggest sympathetic activation or administration of an adrenergic agonist.
*↑ ↑ ↓*
- Beta-blockers **decrease** (not increase) both heart rate and stroke volume through beta-1 receptor blockade.
- While decreased peripheral vascular resistance occurs with vasodilators, beta-blockers acutely **increase** PVR due to unopposed alpha-adrenergic tone.
Alpha-blockers US Medical PG Question 5: A 53-year-old man presents to the office for a routine examination. The medical history is significant for diabetes mellitus, for which he is taking metformin. The medical records show blood pressure readings from three separate visits to fall in the 130–160 mm Hg range for systolic and 90–100 mm Hg range for diastolic. Prazosin is prescribed. Which of the following are effects of this drug?
- A. Vasodilation, decreased heart rate, bronchial constriction
- B. Vasodilation, increased peristalsis, bronchial dilation
- C. Vasoconstriction, bladder sphincter constriction, mydriasis
- D. Vasoconstriction, increase in AV conduction rate, bronchial dilation
- E. Vasodilation, bladder sphincter relaxation (Correct Answer)
Alpha-blockers Explanation: ***Vasodilation, bladder sphincter relaxation***
- **Prazosin** is an **alpha-1 adrenergic receptor antagonist**, which blocks the effects of norepinephrine on vascular smooth muscle, leading to **vasodilation** and decreased blood pressure.
- Blocking alpha-1 receptors in the bladder neck and prostate causes **bladder sphincter relaxation**, which can improve urine flow and is also useful in benign prostatic hyperplasia (BPH).
- These are the two primary clinically relevant effects of alpha-1 blockade with prazosin.
*Vasodilation, decreased heart rate, bronchial constriction*
- While prazosin causes **vasodilation**, it does not typically decrease heart rate directly; alpha-1 blockade can lead to **reflex tachycardia** due to decreased blood pressure.
- Prazosin has no significant effect on bronchial smooth muscle and does not cause **bronchial constriction**; bronchial effects are primarily mediated by beta-2 receptors or muscarinic (M3) receptors.
*Vasodilation, increased peristalsis, bronchial dilation*
- Prazosin does cause **vasodilation** but does not directly cause **increased peristalsis**; gastrointestinal motility is mainly regulated by the autonomic nervous system via muscarinic receptors and the enteric nervous system.
- Prazosin does not cause **bronchial dilation**; this effect is mediated by beta-2 adrenergic receptor stimulation.
*Vasoconstriction, bladder sphincter constriction, mydriasis*
- Prazosin is an alpha-1 antagonist, meaning it *blocks* **vasoconstriction** and instead causes vasodilation.
- Similarly, it causes **bladder sphincter relaxation**, not constriction.
- Prazosin has minimal effects on pupil size; mydriasis would be caused by alpha-1 agonists or muscarinic antagonists, not alpha-1 antagonists.
*Vasoconstriction, increase in AV conduction rate, bronchial dilation*
- Prazosin causes **vasodilation**, not vasoconstriction.
- It does not significantly affect **AV conduction rate** or directly cause **bronchial dilation**.
Alpha-blockers US Medical PG Question 6: A 72-year-old male presents to his primary care physician complaining of increased urinary frequency and a weakened urinary stream. He has a history of gout, obesity, diabetes mellitus, and hyperlipidemia. He currently takes allopurinol, metformin, glyburide, and rosuvastatin. His temperature is 98.6°F (37°C), blood pressure is 130/85 mmHg, pulse is 90/min, and respirations are 18/min. Physical examination reveals an enlarged, non-tender prostate without nodules or masses. An ultrasound reveals a uniformly enlarged prostate that is 40mL in size. His physician starts him on a new medication. After taking the first dose, the patient experiences lightheadedness upon standing and has a syncopal event. Which of the following mechanisms of action is most consistent with the medication in question?
- A. Dihydropyridine calcium channel blocker
- B. Selective muscarinic agonist
- C. Alpha-2-adrenergic receptor agonist
- D. Alpha-1-adrenergic receptor antagonist (Correct Answer)
- E. Non-selective alpha receptor antagonist
Alpha-blockers Explanation: ***Alpha-1-adrenergic receptor antagonist***
- The patient's symptoms of **increased urinary frequency** and **weakened urinary stream** are consistent with **benign prostatic hyperplasia (BPH)**. The physical exam and ultrasound findings of an **enlarged, non-tender prostate** confirm this.
- The medication caused **lightheadedness upon standing** and a **syncopal event** after the first dose, which is indicative of **first-dose orthostatic hypotension**. This adverse effect is characteristic of **alpha-1-adrenergic receptor antagonists**, which relax smooth muscles in the prostate and bladder neck but can also cause vasodilation.
*Dihydropyridine calcium channel blocker*
- These drugs primarily relax **vascular smooth muscle**, leading to vasodilation and can cause **hypotension**, but **orthostatic hypotension** and syncope as a "first-dose effect" are less common compared to alpha-1 blockers.
- They are used to treat **hypertension** and **angina**, not directly for BPH symptoms.
*Selective muscarinic agonist*
- **Muscarinic agonists** (e.g., bethanechol) would **increase bladder contraction** and could worsen urinary outflow obstruction in BPH, not improve it.
- Their primary side effects include **diarrhea**, **nausea**, and **bradycardia**, not orthostatic hypotension and syncope.
*Alpha-2-adrenergic receptor agonist*
- **Alpha-2 agonists** (e.g., clonidine) typically **lower blood pressure** by reducing sympathetic outflow from the central nervous system, but they primarily cause **sedation** and **dry mouth**, and are not used for BPH.
- While they can cause hypotension, the specific presentation of first-dose syncope in the context of BPH treatment points away from this class.
*Non-selective alpha receptor antagonist*
- Although non-selective alpha antagonists can also cause **orthostatic hypotension** due to vasodilation, **selective alpha-1 antagonists** are the preferred choice for BPH due to their more targeted action on the prostate and bladder neck, and the question describes a direct therapy for BPH.
- Alpha-2 blockade is less relevant to BPH and can cause additional side effects.
Alpha-blockers US Medical PG Question 7: A 72-year-old man presents to his primary care provider to discuss the frequency with which he wakes up at night to urinate. He avoids drinking liquids at night, but the symptoms have progressively worsened. The medical history is significant for hypertension and hyperlipidemia. He takes lisinopril, atorvastatin, and a multivitamin every day. Today, the vital signs include: blood pressure 120/80 mm Hg, heart rate 90/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical examination, he appears tired. The heart has a regular rate and rhythm and the lungs are clear to auscultation bilaterally. A bedside bladder ultrasound reveals a full bladder. A digital rectal exam reveals an enlarged and symmetric prostate free of nodules, that is consistent with benign prostatic enlargement. He also has a history of symptomatic hypotension with several episodes of syncope in the past. The patient declines a prostate biopsy that would provide a definitive diagnosis and requests less invasive treatment. Which of the following is recommended to treat this patient’s enlarged prostate?
- A. Tadalafil
- B. Finasteride (Correct Answer)
- C. Tamsulosin
- D. Prazosin
- E. Leuprolide
Alpha-blockers Explanation: ***Finasteride***
- This patient's symptoms of **nocturia** and an **enlarged, symmetric prostate** on DRE are classic for **benign prostatic hyperplasia (BPH)**. Finasteride is a **5-alpha reductase inhibitor** that reduces prostate volume by blocking the conversion of testosterone to dihydrotestosterone.
- Given the patient's history of **symptomatic hypotension** and preference for less invasive treatment, finasteride is a suitable choice as it has a lower risk of exacerbating hypotension compared to alpha-blockers.
*Tadalafil*
- While tadalafil is approved for BPH with erectile dysfunction, its primary mechanism involves **vasodilation**, which could worsen the patient's existing **symptomatic hypotension**.
- It does not directly reduce prostate size, which is a key component of long-term BPH management, especially in a patient with a significantly enlarged prostate.
*Tamsulosin*
- Tamsulosin is an **alpha-1 adrenergic blocker** that relaxes smooth muscle in the prostate and bladder neck, improving urine flow. However, it can cause **hypotension** and **syncope**, which would be contraindicated in this patient with a history of symptomatic hypotension.
- While effective for BPH symptoms, the risk of worsening his cardiovascular stability makes it a less favorable option given his medical history.
*Prazosin*
- Prazosin is another **alpha-1 adrenergic blocker** that can be used for BPH. However, it has a significant risk of **first-dose hypotension** and orthostatic hypotension, which would be highly problematic for this patient with a history of symptomatic hypotension and syncope.
- Due to its potent hypotensive effects, prazosin is generally not preferred for BPH, especially in older patients or those with cardiovascular instability.
*Leuprolide*
- Leuprolide is a **GnRH agonist** primarily used in the treatment of **prostate cancer** to reduce testosterone levels. It would effectively reduce prostate size but is an aggressive treatment with significant side effects (e.g., hot flashes, decreased libido, bone density loss) not typically used for benign prostatic hyperplasia.
- It is not indicated for the management of BPH and would be considered overtreatment for this patient's condition, especially given his desire for less aggressive management.
Alpha-blockers US Medical PG Question 8: A 59-year-old man comes to the physician because of a 3-month history of frequent urination. He has to urinate every 1–2 hours during the day and wakes up at least 2–3 times at night to urinate. He also reports that over the last 2 months, he has difficulty initiating micturition and the urinary stream is weak, with prolonged terminal dribbling. His pulse is 72/min, and blood pressure is 158/105 mm Hg. Rectal exam shows a smooth, symmetrically enlarged prostate without any tenderness or irregularities. Prostate-specific antigen is within the reference range and urinalysis shows no abnormalities. A postvoid ultrasound shows a residual bladder volume of 110 mL. Which of the following is the most appropriate next step in management?
- A. Transurethral resection of the prostate
- B. Terazosin therapy (Correct Answer)
- C. Bladder catheterization
- D. Finasteride therapy
- E. Cystoscopy
Alpha-blockers Explanation: ***Terazosin therapy***
- Terazosin is an **alpha-1 adrenergic antagonist** that blocks receptors in the prostate and bladder neck, causing relaxation of the smooth muscle and improving urinary flow. This is a first-line medical treatment for symptomatic **benign prostatic hyperplasia (BPH)**.
- The patient presents with **obstructive and irritative lower urinary tract symptoms (LUTS)**, a symmetrically enlarged prostate, and a postvoid residual volume that indicates bladder outlet obstruction, all consistent with BPH.
- Alpha-blockers provide **rapid symptom relief** (within days to weeks) and may also help with the patient's **elevated blood pressure** (158/105 mm Hg).
*Transurethral resection of the prostate*
- **Transurethral resection of the prostate (TURP)** is a surgical intervention reserved for patients with severe BPH symptoms refractory to medical therapy or those with complications like recurrent urinary retention or renal dysfunction.
- Given that the patient has not yet tried medical therapy, and his symptoms are not immediately life-threatening, surgery is not the most appropriate first step.
*Bladder catheterization*
- **Bladder catheterization** is indicated for acute urinary retention or in cases of severe bladder obstruction leading to renal impairment.
- While the patient has significant LUTS and a postvoid residual volume, he is not in acute urinary retention, so immediate catheterization is not necessary as a long-term management strategy.
*Finasteride therapy*
- **Finasteride** is a **5-alpha reductase inhibitor** that reduces prostate size by inhibiting the conversion of testosterone to dihydrotestosterone. It is more effective in patients with larger prostate volumes and takes several months to show its full effect.
- Though a valid treatment for BPH, alpha-blockers like terazosin provide faster symptomatic relief by addressing dynamic obstruction and are generally preferred as initial therapy, often in combination with 5-alpha reductase inhibitors for larger prostates.
*Cystoscopy*
- **Cystoscopy** is an invasive procedure used to visualize the bladder and urethra directly. It is typically reserved for cases where there is suspicion of other pathologies like bladder stones, strictures, or bladder cancer, or for preoperative planning.
- The patient's symptoms and examination findings are consistent with BPH, and his PSA is normal, so primary cystoscopy is not indicated as the next step in management.
Alpha-blockers US Medical PG Question 9: A 57-year-old presents to your clinic complaining of baldness. He is overweight, has been diagnosed with BPH, and is currently taking atorvastatin for hyperlipidemia. The patient has tried several over-the-counter products for hair-loss; however, none have been effective. After discussing several options, the patient is prescribed a medication to treat his baldness that has the additional benefit of treating symptoms of BPH as well. Synthesis of which of the following compounds would be expected to decrease in response to this therapy?
- A. Testosterone
- B. FSH
- C. LH
- D. GnRH
- E. DHT (Correct Answer)
Alpha-blockers Explanation: ***DHT***
- The medication described is likely **finasteride**, a **5-alpha-reductase inhibitor**. This enzyme converts **testosterone** to **dihydrotestosterone (DHT)**.
- Decreased DHT levels are beneficial for treating both **androgenetic alopecia (baldness)** and **benign prostatic hyperplasia (BPH)** due to its potent androgenic effects on hair follicles and prostate growth.
*Testosterone*
- While finasteride inhibits the conversion of testosterone to DHT, it does not directly decrease testosterone synthesis. In fact, **testosterone levels may slightly increase** as its conversion to DHT is blocked.
- Testosterone itself is not the primary androgen responsible for male pattern baldness or BPH; it's its more potent metabolite, DHT.
*FSH*
- **Follicle-stimulating hormone (FSH)** is a gonadotropin released from the anterior pituitary that stimulates sperm production and ovarian follicle development.
- The medication prescribed does not directly affect FSH synthesis or release; its action is peripheral, affecting androgen metabolism.
*LH*
- **Luteinizing hormone (LH)** is another gonadotropin that stimulates testosterone production in Leydig cells.
- The drug's mechanism of action is local inhibition of an enzyme, not a central regulation of pituitary hormones like LH.
*GnRH*
- **Gonadotropin-releasing hormone (GnRH)** is released from the hypothalamus and stimulates the anterior pituitary to release FSH and LH.
- This therapy specifically targets the conversion of an androgen and does not impact the hypothalamic-pituitary-gonadal axis at the level of GnRH.
Alpha-blockers US Medical PG Question 10: A 67-year-old man presents to the emergency department with trouble urinating. The patient states that in general he has had difficulty urinating but recently, it has taken significant effort for him to initiate a urinary stream. He finds himself unable to completely void and states he has suprapubic tenderness as a result. These symptoms started suddenly 3 days ago. The patient has a history of benign prostatic hyperplasia, constipation, and diabetes mellitus. His current medications include finasteride, sodium docusate, and hydrochlorothiazide. He recently started taking phenylephrine for seasonal allergies. The patient’s last bowel movement was 2 days ago. His temperature is 99.0°F (37.2°C), blood pressure is 167/98 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 100% on room air. Physical exam is notable for suprapubic tenderness, and an ultrasound reveals 750 mL of fluid in the bladder. Which of the following is the most likely etiology of this patient’s symptoms?
- A. Prostatic adenocarcinoma
- B. Medication-induced symptoms (Correct Answer)
- C. Constipation
- D. Urinary tract infection
- E. Worsening benign prostatic hypertrophy
Alpha-blockers Explanation: ***Medication-induced symptoms***
- The patient recently started **phenylephrine**, an **alpha-1 adrenergic agonist**, which can cause **urethral constriction** and worsen urinary outflow obstruction, especially in patients with BPH.
- The **sudden onset** of severe urinary retention, leading to suprapubic tenderness and a distended bladder (750 mL), is highly suggestive of a medication side effect given his existing BPH.
*Prostatic adenocarcinoma*
- While prostatic adenocarcinoma can cause urinary symptoms, these typically develop **gradually** and are less likely to present with such an acute, severe urinary retention episode.
- There are no other features like **weight loss**, **bone pain**, or abnormal **PSA levels** mentioned to suggest malignancy.
*Constipation*
- Although **severe constipation** can sometimes exacerbate urinary symptoms by physical compression on the bladder, the patient's last bowel movement was 2 days ago, which is not severe enough to cause acute urinary retention of this magnitude.
- The primary cause of his urinary symptoms is more likely related to bladder outflow obstruction rather than external compression from constipation.
*Urinary tract infection*
- A UTI typically presents with symptoms like **dysuria**, **frequency**, **urgency**, **fever**, and **chills**, none of which are prominent here.
- While a UTI can cause some urinary difficulty, it's less likely to be the sole cause of such acute and severe urinary retention or a bladder volume of 750 mL without other infection signs.
*Worsening benign prostatic hypertrophy*
- Although the patient has BPH and is on finasteride, a **sudden dramatic worsening** over 3 days, leading to complete inability to void and a large bladder volume, is less typical for a gradual disease progression.
- The acute change points more strongly to an **exacerbating factor**, such as a new medication, rather than a natural progression of BPH.
More Alpha-blockers US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.