Alpha-2 agonists US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alpha-2 agonists. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alpha-2 agonists US Medical PG Question 1: A 75 year-old gentleman presents to his general practitioner. He is currently being treated for hypertension and is on a multi-drug regimen. His current blood pressure is 180/100. The physician would like to begin treatment with minoxidil or hydralazine. Which of the following side effects is associated with administration of these drugs?
- A. Persistent cough
- B. Cyanosis in extremities
- C. Fetal renal toxicity
- D. Systemic volume loss
- E. Reflex tachycardia (Correct Answer)
Alpha-2 agonists Explanation: ***Reflex tachycardia***
- Both **minoxidil** and **hydralazine** are direct arterial vasodilators, causing a significant drop in **peripheral vascular resistance**.
- This vasodilation triggers a **baroreflex response**, leading to an increase in heart rate and **cardiac contractility** to maintain cardiac output, resulting in reflex tachycardia.
*Persistent cough*
- **Persistent cough** is a common side effect associated with **ACE inhibitors**, such as lisinopril or enalapril, due to the accumulation of **bradykinin**.
- This side effect is not typically seen with **minoxidil** or **hydralazine**, which act directly on vascular smooth muscle to cause vasodilation.
*Cyanosis in extremities*
- **Cyanosis** (bluish discoloration of the skin and mucous membranes) usually indicates **hypoxemia** or poor peripheral perfusion.
- While sometimes associated with severe cardiogenic shock or specific drug toxicities like methemoglobinemia (not related to minoxidil or hydralazine), it is not a direct or typical side effect of these vasodilators.
*Fetal renal toxicity*
- **Fetal renal toxicity**, including **fetal renal dysfunction** and **oligohydramnios**, is a well-known risk associated with **ACE inhibitors** and **ARBs** during pregnancy.
- Neither **minoxidil** nor **hydralazine** are primarily linked to this specific fetal adverse effect, though hydralazine can be used in pregnancy for severe hypertension.
*Systemic volume loss*
- **Systemic volume loss** is usually caused by conditions like **dehydration**, excessive diuresis, or hemorrhage.
- While vasodilators can reduce blood pressure, they do not directly cause **systemic volume depletion**; rather, the reflex response to vasodilation can include fluid retention to counteract the blood pressure drop.
Alpha-2 agonists US Medical PG Question 2: A patient presents with periods of severe headaches and flushing however every time they have come to the physician they have not experienced any symptoms. The only abnormal finding is a blood pressure of 175 mmHg/100 mmHg. It is determined that the optimal treatment for this patient is surgical. Prior to surgery which of the following noncompetitive inhibitors should be administered?
- A. Phentolamine
- B. Isoproterenol
- C. Atropine
- D. Propranolol
- E. Phenoxybenzamine (Correct Answer)
Alpha-2 agonists Explanation: ***Phenoxybenzamine***
- This patient likely has a **pheochromocytoma**, which explains the episodic headaches, flushing, and hypertension. **Phenoxybenzamine** is a **non-competitive, irreversible alpha-adrenergic blocker** that is crucial for preoperative preparation to prevent a **hypertensive crisis** during surgery.
- Its **irreversible binding** provides sustained alpha blockade, essential to control blood pressure and avoid catecholamine-induced surges during tumor manipulation.
*Phentolamine*
- **Phentolamine** is a **competitive alpha-adrenergic blocker** used to manage acute hypertensive episodes, but it has a shorter duration of action.
- It is not preferred for sustained preoperative alpha blockade due to its **reversible nature** and potential for drug washout during surgery, which could lead to catecholamine surges.
*Isoproterenol*
- **Isoproterenol** is a **beta-adrenergic agonist** that increases heart rate and contractility, and causes bronchodilation.
- It would be contraindicated in a patient with pheochromocytoma as it could worsen hypertension and cardiac symptoms by stimulating beta receptors that are already overly sensitive to endogenous catecholamines.
*Atropine*
- **Atropine** is a **muscarinic acetylcholine receptor antagonist** that blocks parasympathetic effects, like bradycardia and salivation.
- It has no role in managing hypertension or the catecholamine excess seen in pheochromocytoma.
*Propranolol*
- **Propranolol** is a **non-selective beta-adrenergic blocker** that can be used to control tachycardia and arrhythmias in pheochromocytoma, but only *after* adequate alpha-blockade has been established.
- Using **propranolol alone** or before alpha-blockade can lead to **unopposed alpha-adrenergic stimulation**, resulting in a severe, life-threatening hypertensive crisis.
Alpha-2 agonists US Medical PG Question 3: A patient with a history of hypertension and bipolar disorder is seen in your clinic for new-onset tremor, increased urination, and mild dehydration symptoms. Her bipolar disorder has been well-controlled with her current medication regimen. She recently started a new medication for better management of her hypertension. Which of the following medications did she most likely start?
- A. Amlodipine
- B. Lisinopril
- C. Hydrochlorothiazide (Correct Answer)
- D. Furosemide
- E. Metoprolol
Alpha-2 agonists Explanation: ***Hydrochlorothiazide***
- **Thiazide diuretics** are first-line antihypertensive agents that promote **sodium and water excretion**.
- Volume depletion from thiazides **decreases renal lithium clearance**, increasing serum lithium levels and causing **lithium toxicity**.
- Classic lithium toxicity presents with **tremor, polyuria (nephrogenic diabetes insipidus), polydipsia**, and dehydration.
- This represents a critical **drug-drug interaction** between thiazides and lithium.
*Incorrect: Amlodipine*
- **Calcium channel blocker** (dihydropyridine class) commonly used for hypertension.
- Does **not affect lithium levels** or renal clearance.
- Side effects include peripheral edema and reflex tachycardia, not the symptoms described.
*Incorrect: Lisinopril*
- **ACE inhibitor** used as first-line therapy for hypertension.
- Does **not significantly affect lithium clearance** (though ACE inhibitors can have minor effects, they don't typically cause clinically significant lithium toxicity).
- Common side effects include dry cough and hyperkalemia, not tremor or polyuria.
*Incorrect: Furosemide*
- **Loop diuretic** that can cause dehydration and polyuria.
- Could potentially increase lithium levels through volume depletion, but **thiazides are more commonly implicated** in lithium toxicity.
- Furosemide is typically reserved for **resistant hypertension or heart failure**, not as initial therapy.
*Incorrect: Metoprolol*
- **Beta-blocker** used for hypertension management.
- Does **not affect lithium levels** or cause the described symptoms.
- Side effects include bradycardia, fatigue, and bronchospasm in susceptible patients.
Alpha-2 agonists US Medical PG Question 4: A 60-year-old man presents to the office for a scheduled follow-up visit. He has had hypertension for the past 30 years and his current anti-hypertensive medications include lisinopril (40 mg/day) and hydrochlorothiazide (50 mg/day). He follows most of the lifestyle modifications recommended by his physician, but is concerned about his occasional occipital headaches in the morning. His blood pressure is 160/98 mm Hg. The physician adds another drug to his regimen that acts centrally as an α2-adrenergic agonist. Which of the following second messengers is involved in the mechanism of action of this new drug?
- A. Calcium ions
- B. Inositol triphosphate
- C. Cyclic guanosine monophosphate
- D. Cyclic adenosine monophosphate (Correct Answer)
- E. Diacylglycerol
Alpha-2 agonists Explanation: ***Cyclic adenosine monophosphate***
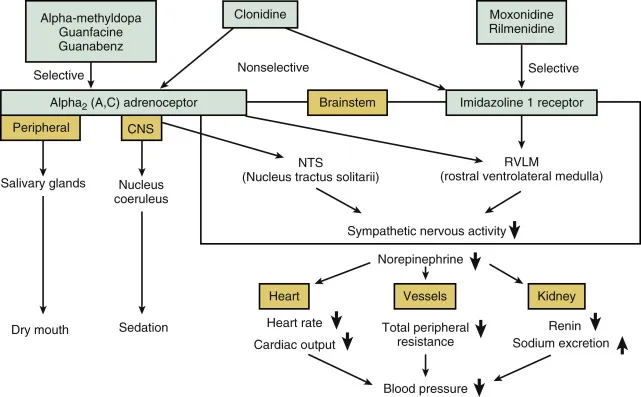
- The physician likely added **clonidine or methyldopa**, both of which are **central α2-adrenergic agonists** used to treat hypertension.
- Activation of **α2-adrenergic receptors** leads to the **inhibition of adenylyl cyclase** and a decrease in **intracellular cyclic AMP (cAMP) levels**, which is the second messenger.
*Calcium ions*
- While calcium ions are crucial second messengers in many cellular processes, they are primarily involved in the mechanism of action of **α1-adrenergic receptors** and **voltage-gated calcium channels**, not directly inhibited by α2-agonists.
- **α2-adrenergic agonism** primarily acts to *reduce* neuronal excitability, which can indirectly affect calcium flux but does not directly involve calcium as the primary second messenger.
*Inositol triphosphate*
- **Inositol triphosphate (IP3)** is a second messenger primarily associated with the activation of **Gq protein-coupled receptors**, leading to the release of intracellular calcium.
- This pathway is characteristic of **α1-adrenergic receptors**, which cause vasoconstriction, and is antagonistic to the α2-agonist mechanism.
*Cyclic guanosine monophosphate*
- **Cyclic GMP (cGMP)** is a key second messenger in processes such as **vasodilation mediated by nitric oxide** and the action of ANP/BNP.
- **α2-adrenergic agonists** do not directly modulate cGMP levels as their primary mechanism of action.
*Diacylglycerol*
- **Diacylglycerol (DAG)** is a second messenger, along with IP3, produced from the hydrolysis of **PIP2** by phospholipase C, following activation of **Gq protein-coupled receptors**.
- This pathway is associated with **α1-adrenergic receptor activation**, not the inhibitory pathway initiated by central α2-adrenergic agonists.
Alpha-2 agonists US Medical PG Question 5: An investigator is studying a local anesthetic that causes increased sympathetic activity. When given intravenously, it causes euphoria and pupillary dilation. Which of the following is the most likely effect of this drug at the synaptic cleft?
- A. Increased release of norepinephrine
- B. Decreased reuptake of norepinephrine (Correct Answer)
- C. Decreased release of acetylcholine
- D. Increased release of serotonin
- E. Decreased breakdown of norepinephrine
Alpha-2 agonists Explanation: ***Decreased reuptake of norepinephrine***
- This drug causes **euphoria** and **pupillary dilation**, which are classic signs of increased **sympathetic nervous system** activity and **CNS stimulation**, consistent with enhanced **noradrenergic transmission**.
- Decreasing the **reuptake of norepinephrine** would increase its concentration in the **synaptic cleft**, leading to more prolonged activation of **alpha and beta adrenergic receptors**.
*Increased release of norepinephrine*
- While increased release would also elevate **norepinephrine** in the **synaptic cleft**, reuptake inhibition is a more common mechanism for drugs producing similar effects like **cocaine** and **amphetamine-like stimulants**.
- Without specific information, **reuptake inhibition** aligns better with the broad activation of **adrenergic receptors** and central effects described.
*Decreased release of acetylcholine*
- This would primarily affect **cholinergic systems**, and while some interactions exist, it does not directly explain the intense **adrenergic activation**, **euphoria**, and **pupillary dilation** observed.
- **Acetylcholine** primarily mediates **parasympathetic responses** and **skeletal muscle contraction**, not the sympathetic effects seen here.
*Increased release of serotonin*
- Increased **serotonin** release is associated with hallucinogenic effects and mood modulation, but it does not directly lead to the pronounced **pupillary dilation** and widespread **alpha/beta adrenergic receptor activation** described.
- The drug explicitly affects **adrenergic receptors**, making an effect on **norepinephrine** more direct.
*Decreased breakdown of norepinephrine*
- This mechanism, typically involving **MAO inhibitors**, would increase **norepinephrine** levels but is described as activating both **alpha and beta adrenergic receptors**, which points more towards a direct increase in synaptic availability rather than metabolic inhibition.
- While it prolongs the action of **norepinephrine**, the primary mechanism described for such a general stimulant often involves **reuptake inhibition** or **enhanced release**.
Alpha-2 agonists US Medical PG Question 6: A 55-year-old woman comes to the physician because of involuntary hand movements that improve with alcohol consumption. Physical examination shows bilateral hand tremors that worsen when the patient is asked to extend her arms out in front of her. The physician prescribes a medication that is associated with an increased risk of bronchospasms. This drug has which of the following immediate effects on the cardiovascular system?
Stroke volume | Heart rate | Peripheral vascular resistance
- A. ↓ ↓ ↓
- B. ↓ ↓ ↑ (Correct Answer)
- C. ↓ ↑ ↑
- D. ↑ ↑ ↑
- E. ↑ ↑ ↓
Alpha-2 agonists Explanation: ***↓ ↓ ↑***
- This patient likely has **essential tremor**, which is characterized by **bilateral hand tremors** that improve with alcohol and worsen with intention (postural tremor). The prescribed medication is a **beta-blocker** (e.g., propranolol), which is associated with an increased risk of bronchospasms due to blocking **beta-2 receptors** in the airways.
- Beta-blockers **decrease heart rate** (negative chronotropic effect) and **stroke volume** (negative inotropic effect) by blocking beta-1 receptors in the heart, reducing cardiac output.
- **Peripheral vascular resistance increases** acutely due to: (1) **unopposed alpha-1 adrenergic tone** in blood vessels (loss of beta-2 mediated vasodilation), and (2) baroreceptor-mediated reflex vasoconstriction in response to decreased cardiac output. This helps maintain blood pressure despite reduced cardiac output.
*↓ ↓ ↓*
- While beta-blockers decrease **heart rate** and **stroke volume**, peripheral vascular resistance does not decrease acutely. A decrease in all three parameters would cause severe hypotension.
- The loss of beta-2 receptor-mediated vasodilation and baroreceptor reflexes lead to increased, not decreased, peripheral vascular resistance.
*↓ ↑ ↑*
- Beta-blockers **decrease heart rate** through beta-1 blockade, not increase it. This is their primary cardiac mechanism of action.
- An increase in heart rate would be expected with sympathomimetic drugs or anticholinergics, not beta-blockers.
*↑ ↑ ↑*
- This combination indicates increased cardiovascular activity, which is the opposite effect of **beta-blockers**.
- Beta-blockers reduce heart rate and stroke volume by blocking beta-1 receptors; they do not increase these parameters.
- This pattern would suggest sympathetic activation or administration of an adrenergic agonist.
*↑ ↑ ↓*
- Beta-blockers **decrease** (not increase) both heart rate and stroke volume through beta-1 receptor blockade.
- While decreased peripheral vascular resistance occurs with vasodilators, beta-blockers acutely **increase** PVR due to unopposed alpha-adrenergic tone.
Alpha-2 agonists US Medical PG Question 7: A 65-year-old male with a history of CHF presents to the emergency room with shortness of breath, lower leg edema, and fatigue. He is diagnosed with acute decompensated congestive heart failure, was admitted to the CCU, and treated with a medication that targets beta-1 adrenergic receptors preferentially over beta-2 adrenergic receptors. The prescribing physician explained that this medication would only be used temporarily as its efficacy decreases within 2-3 days due to receptor downregulation. Which of the following was prescribed?
- A. Epinephrine
- B. Norepinephrine
- C. Milrinone
- D. Isoproterenol
- E. Dobutamine (Correct Answer)
Alpha-2 agonists Explanation: ***Dobutamine***
- **Dobutamine** is a beta-1 adrenergic agonist preferentially acting on beta-1 receptors in the heart, increasing contractility and heart rate during acute decompensated heart failure.
- Its efficacy reduces over time due to **receptor downregulation**, making it effective for only short-term use, typically less than 72 hours.
*Epinephrine*
- **Epinephrine** is a non-selective adrenergic agonist acting on both alpha and beta receptors, causing vasoconstriction and bronchodilation in addition to cardiac stimulation.
- It is typically used in emergency situations like **cardiac arrest** and **anaphylaxis**, not primarily for acute CHF exacerbation in this manner.
*Norepinephrine*
- **Norepinephrine** primarily acts on alpha-1 adrenergic receptors, causing significant vasoconstriction, and has some beta-1 agonistic effects.
- It is mainly used as a **vasopressor** in septic shock or severe hypotension to increase systemic vascular resistance, rather than directly improving cardiac output in decompensated CHF.
*Milrinone*
- **Milrinone** is a phosphodiesterase-3 inhibitor, increasing intracellular cAMP levels and leading to positive inotropy and vasodilation.
- While used in acute heart failure, its mechanism is distinct from adrenergic agonists, and its efficacy is not limited by a rapid receptor downregulation mechanism as described.
*Isoproterenol*
- **Isoproterenol** is a non-selective beta-adrenergic agonist, stimulating both beta-1 and beta-2 receptors, leading to increased heart rate and contractility, as well as bronchodilation and vasodilation.
- Due to its strong chronotropic effects and potential for severe arrhythmias and hypotension, it is rarely used in CHF and is primarily reserved for conditions like **bradycardia** or **torsades de pointes**.
Alpha-2 agonists US Medical PG Question 8: A 37-year-old male presents to general medical clinic reporting sleeping difficulties. He states that he has daytime sleepiness, having fallen asleep several times while driving his car recently. He sometimes experiences very vivid dreams just before awakening. You ask the patient's wife if she has witnessed any episodes where her husband lost all muscle tone and fell to the ground, and she confirms that he has not had this symptom. The patient notes that this condition runs in his family, and he desperately asks for treatment. You begin him on a first-line medication for this illness, which works by which mechanism of action?
- A. Dopamine reuptake inhibition (Correct Answer)
- B. Serotonin reuptake inhibition
- C. Mu opioid receptor agonism
- D. GABA receptor agonism
- E. Alpha-2 adrenergic receptor antagonism
Alpha-2 agonists Explanation: ***Dopamine reuptake inhibition***
- The patient's symptoms of **excessive daytime sleepiness**, falling asleep while driving, and vivid dreams (hypnagogic hallucinations) are classic for **narcolepsy type 2** (without cataplexy).
- **First-line treatment** for excessive daytime sleepiness in narcolepsy is **modafinil** or **armodafinil**, which work primarily through **dopamine reuptake inhibition** (along with other mechanisms including effects on orexin neurons).
- Alternative first-line agents include **methylphenidate** and **amphetamines**, which also work via **dopamine and norepinephrine reuptake inhibition**.
- These medications promote wakefulness and are supported by AASM and AAN clinical practice guidelines.
*Serotonin reuptake inhibition*
- **SSRIs** and **SNRIs** are sometimes used in narcolepsy but primarily for **cataplexy** management, not daytime sleepiness.
- This patient has **no cataplexy**, making this mechanism less relevant for his primary complaint.
- Not considered first-line for the excessive daytime sleepiness that is this patient's main concern.
*Alpha-2 adrenergic receptor antagonism*
- This is the mechanism of **mirtazapine**, an atypical antidepressant.
- **Not a first-line treatment** for narcolepsy or excessive daytime sleepiness.
- Mirtazapine is actually somewhat sedating and would worsen daytime sleepiness, not improve it.
*Mu opioid receptor agonism*
- This describes traditional opioid analgesics, which are **not used** in narcolepsy treatment.
- Opioids cause sedation and would worsen daytime sleepiness.
- **Sodium oxybate** (used in narcolepsy) is sometimes confused with opioids, but it works primarily through GABA-B receptors, not mu opioid receptors.
*GABA receptor agonism*
- **Sodium oxybate** (gamma-hydroxybutyrate/GHB) works primarily through **GABA-B receptor agonism** and is FDA-approved for narcolepsy.
- However, it is used primarily for **cataplexy** and to improve **nighttime sleep quality**, not as first-line for daytime sleepiness alone.
- While effective, it is typically considered after trials of modafinil/stimulants due to its scheduling restrictions (Schedule III) and side effect profile.
Alpha-2 agonists US Medical PG Question 9: A 12-year-old boy presents to the pediatrician with complaints of chronic cough for the past two years. The cough is present during the day, especially after returning from school. His school teacher says he does not cough at school. The cough is absent while he is asleep, although it increases during examinations or when he experiences boredom. His mother reports that there was a one-month period where he did not cough, but during that month, he used to shrug his shoulders frequently, especially when he was stressed or fatigued. There is no history of sneezing, nasal discharge, nasal congestion, headache, ear symptoms, or breathing difficulty. Detailed history does not suggest the presence of a mood disorder, obsessive-compulsive symptoms, or attention-deficit/hyperactivity disorder. There is no past history of a known neurological disorder, and there is no history of substance abuse. On physical examination, his vital signs are stable. Examination of his respiratory and cardiovascular systems is normal. However, the pediatrician notes repeated eye blinking; upon asking about eye blinking, the mother reports that he has had this habit since he was almost eight years old. Further inquiry suggests that eye blinking, coughing, and grunting disappear for a few weeks without explanation, only to reappear again. Which of the following drugs is likely to be most effective to control this patient’s symptoms?
- A. Levetiracetam
- B. Atomoxetine
- C. Haloperidol
- D. Fluoxetine
- E. Clonidine (Correct Answer)
Alpha-2 agonists Explanation: **Clonidine**
- This patient's presentation with chronic cough, shoulder shrugs, eye blinking, and grunting, characterized by **waxing and waning symptoms** and **suggestibility (cough absent at school but present post-school, increasing with boredom/examinations)**, is highly suggestive of **Tourette's disorder** or a **chronic tic disorder**.
- **Clonidine**, an alpha-2 adrenergic agonist, is a first-line treatment for tic disorders, especially in children, due to its efficacy in reducing tic severity with a favorable side effect profile.
*Levetiracetam*
- **Levetiracetam** is an antiepileptic drug used to treat various seizure types, including focal and generalized seizures.
- It is **not indicated for tic disorders** and would not be effective in controlling the patient's symptoms.
*Atomoxetine*
- **Atomoxetine** is a selective norepinephrine reuptake inhibitor primarily used to treat **attention-deficit/hyperactivity disorder (ADHD)**.
- While tics can co-occur with ADHD, atomoxetine is **not a primary treatment for tic disorders** and may even exacerbate tics in some individuals.
*Haloperidol*
- **Haloperidol** is a first-generation antipsychotic with strong dopamine receptor-blocking activity, highly effective in severe tic disorders due to its potent antipsychotic effects.
- However, it has a significant side effect profile, including **extrapyramidal symptoms (dystonia, parkinsonism, akathisia, and tardive dyskinesia)**, making it a second or third-line option after alpha-2 agonists or atypical antipsychotics like risperidone, especially given the patient's age and milder symptom presentation.
*Fluoxetine*
- **Fluoxetine** is a selective serotonin reuptake inhibitor (SSRI) primarily used to treat **depression, anxiety disorders, and obsessive-compulsive disorder (OCD)**.
- While OCD can co-occur with tic disorders, fluoxetine directly targets mood and anxiety symptoms, **not the tics themselves**.
Alpha-2 agonists US Medical PG Question 10: A 67-year-old woman presents to her physician for a regular checkup. She is a community-dwelling, retired teacher without any smoking history. She has arterial hypertension and takes hydrochlorothiazide 12.5 mg and valsartan 80 mg daily. She was recently discharged from the hospital after admission for an ulnar fracture she received after a fall from the second step of a ladder in her garden. A year ago, she had a clavicular fracture from tripping over some large rocks in her yard. She does not report lightheadedness or fainting. Her medical history is also significant for an appendectomy 11 years ago. She is in menopause. She mostly consumes vegetables and dairy products. Her height is 163 cm (5 ft 4 in) and weight is 55 kg (123 lb). Her blood pressure is 130/80 mm Hg without orthostatic changes, heart rate is 73/min and regular, respiratory rate is 14/min, and temperature is 36.6°C (97.9°F). Her lungs are clear to auscultation. Cardiac auscultation reveals S2 accentuation over the aorta. The abdomen is mildly distended on palpation; there are no identifiable masses. The neurological examination is unremarkable. Considering the history and presentation, which of the following medications most likely will be prescribed to this patient after additional investigations?
- A. Estrogen plus progestin
- B. Denosumab
- C. Cholecalciferol (Correct Answer)
- D. Atorvastatin
- E. Tocopherol
Alpha-2 agonists Explanation: ***Cholecalciferol***
- The patient presents with multiple risk factors for **osteoporosis** and potential **vitamin D deficiency**, including postmenopausal status, multiple fragility fractures (ulnar and clavicular), and a diet rich in vegetables but potentially low in vitamin D-fortified products or sun exposure.
- **Cholecalciferol (Vitamin D3)** is essential for calcium absorption and bone health, and its supplementation is crucial for preventing and managing osteoporosis, particularly when low levels are suspected.
*Estrogen plus progestin*
- **Hormone replacement therapy (HRT)** with estrogen plus progestin can prevent osteoporosis, but it is typically not a first-line treatment due to increased risks of breast cancer, cardiovascular events, and stroke, especially in a 67-year-old woman.
- Given her age and that she is well past menopause, the risks often outweigh the benefits for bone health alone, and safer alternatives are available for osteoporosis treatment.
*Denosumab*
- **Denosumab** is a potent antiresorptive agent used for osteoporosis, particularly in patients with a high fracture risk or those who cannot tolerate oral bisphosphonates.
- While she has risk factors for osteoporosis, denosumab is usually initiated after a definitive diagnosis of osteoporosis (e.g., via **DEXA scan**) and often after lifestyle modifications and basic supplementation like vitamin D. It's a treatment, not a "most likely prescribed after additional investigation" first step.
*Atorvastatin*
- **Atorvastatin** is a statin used to lower cholesterol and prevent cardiovascular disease.
- While the patient has hypertension, there's no indication in the provided information (e.g., lipid profile, history of cardiovascular events) that she requires atorvastatin at this time.
*Tocopherol*
- **Tocopherol (Vitamin E)** is an antioxidant that plays a role in various bodily functions but is not directly involved in bone metabolism or the prevention/treatment of osteoporosis.
- There is no clinical indication in the patient's history suggesting a need for vitamin E supplementation for her current presentation.
More Alpha-2 agonists US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.