ACE inhibitors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for ACE inhibitors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
ACE inhibitors US Medical PG Question 1: A 51-year-old woman presents to the emergency department with a 2-day history of bilateral lower extremity swelling. She says that her legs do not hurt, but she noticed she was gaining weight and her legs were becoming larger. Her past medical history is significant for morbid obesity, hypertension, and hypercholesterolemia. She says the swelling started after she was recently started on a new medication to help her blood pressure, but she does not remember the name of the medication. Which of the following is most likely the mechanism of action for the drug that was prescribed to this patient?
- A. Potassium-sparing diuretic
- B. Inhibition of calcium channels (Correct Answer)
- C. Inhibition of enzyme in the lung
- D. Potassium-wasting diuretic
- E. Inhibition of hormone receptor
ACE inhibitors Explanation: ***Inhibition of calcium channels***
- The patient's presentation of **bilateral lower extremity swelling** (peripheral edema) after starting a new blood pressure medication is a classic side effect of **calcium channel blockers (CCBs)**, particularly dihydropyridine CCBs like amlodipine.
- CCBs cause **vasodilation of arterioles**, leading to increased hydrostatic pressure in the capillaries and subsequent fluid extravasation into the interstitial space.
*Potassium-sparing diuretic*
- **Potassium-sparing diuretics** primarily work in the collecting duct to increase sodium excretion and retain potassium, without causing or significantly worsening peripheral edema.
- They are used to treat hypertension and heart failure, but their mechanism does not directly cause dependent edema in the way described.
*Inhibition of enzyme in the lung*
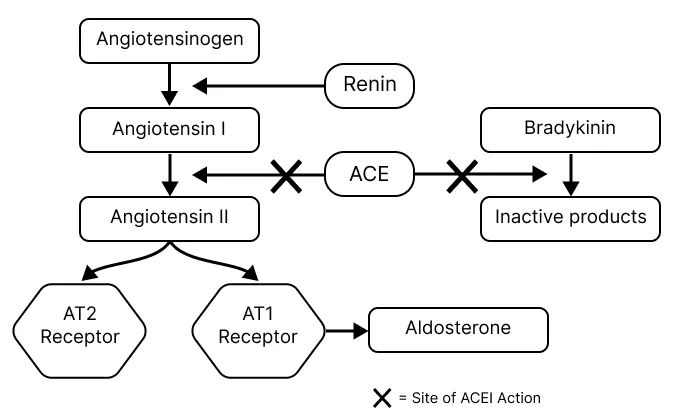
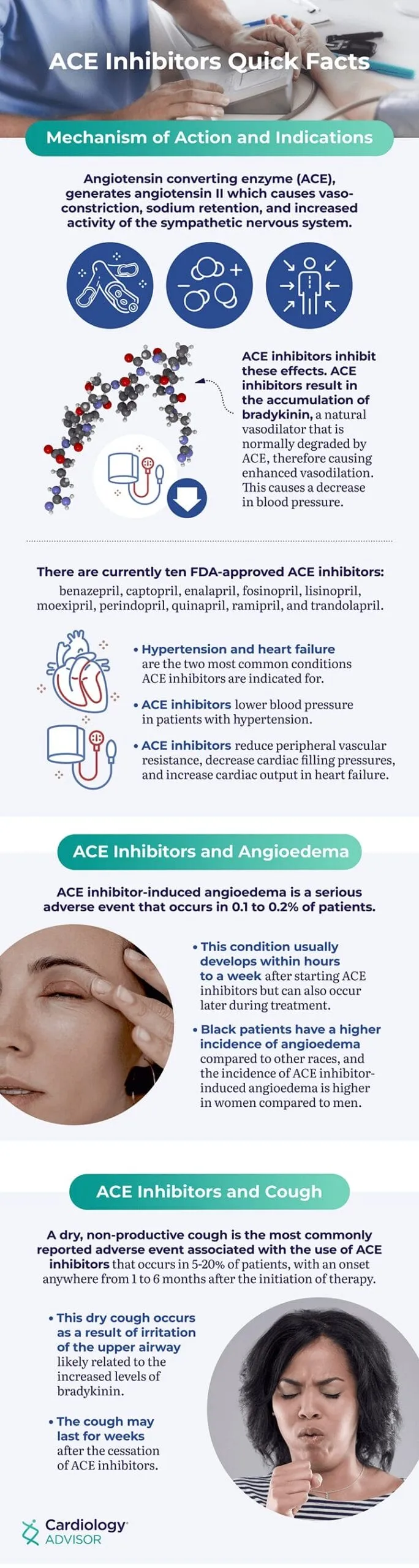
- This description most closely refers to the **angiotensin-converting enzyme (ACE)**, which is inhibited by ACE inhibitors used for hypertension.
- **ACE inhibitors** typically do not cause peripheral edema; their common side effects include cough and angioedema (though less common).
*Potassium-wasting diuretic*
- **Potassium-wasting diuretics** (e.g., loop or thiazide diuretics) increase urine output and are used to *reduce* fluid retention and swelling, not cause it.
- While they can lower blood pressure, they would alleviate, rather than induce, bilateral lower extremity swelling.
*Inhibition of hormone receptor*
- This mechanism could refer to several classes of antihypertensives, such as **beta-blockers** (inhibiting adrenergic receptors) or **angiotensin receptor blockers (ARBs)** (inhibiting angiotensin II receptors).
- Neither beta-blockers nor ARBs are typically associated with prominent bilateral lower extremity swelling as a common side effect.
ACE inhibitors US Medical PG Question 2: A 58-year-old male with a history of congestive heart failure and hypertension comes to you with the chief complaint of new-onset cough as well as increased serum potassium in the setting of a new medication. Which of the following medications is most likely responsible for these findings?
- A. Lisinopril (Correct Answer)
- B. Metoprolol
- C. Furosemide
- D. Amiodarone
- E. Digoxin
ACE inhibitors Explanation: ***Lisinopril***
- **Lisinopril** is an ACE inhibitor, which can cause a **persistent dry cough** due to the accumulation of bradykinin.
- ACE inhibitors can also cause **hyperkalemia** by inhibiting aldosterone secretion, which normally promotes potassium excretion.
*Metoprolol*
- **Metoprolol** is a beta-blocker that primarily decreases heart rate and blood pressure; it is not typically associated with cough or hyperkalemia.
- While it can be used in CHF, its common side effects include bradycardia and fatigue, not the described symptoms.
*Furosemide*
- **Furosemide** is a loop diuretic that promotes potassium excretion, leading to **hypokalemia**, not hyperkalemia.
- It does not typically cause cough; instead, it can help reduce fluid accumulation in the lungs associated with CHF.
*Amiodarone*
- **Amiodarone** is an antiarrhythmic drug known for several significant side effects, including **pulmonary fibrosis** (which can cause cough) and thyroid dysfunction.
- However, it does not typically cause hyperkalemia; instead, it can cause changes in electrolyte levels, but not the specific combination seen here.
*Digoxin*
- **Digoxin** is a cardiac glycoside used to increase cardiac contractility and slow heart rate in heart failure and arrhythmias.
- It does not typically cause cough or hyperkalemia; its toxicity is often associated with nausea, visual disturbances, and arrhythmias.
ACE inhibitors US Medical PG Question 3: A 49-year-old man is diagnosed with hypertension. He has asthma. The creatinine and potassium levels are both slightly elevated. Which of the following anti-hypertensive drugs would be appropriate in his case?
- A. Amlodipine (Correct Answer)
- B. Hydrochlorothiazide (HCT)
- C. Enalapril
- D. Spironolactone
- E. Propranolol
ACE inhibitors Explanation: ***Amlodipine***
- **Amlodipine** is a **calcium channel blocker** that is safe and effective in patients with **asthma** as it does not exacerbate bronchoconstriction.
- It is **renal protective** and does not significantly affect **potassium levels**, making it ideal for this patient with elevated creatinine and potassium.
- This is the **best choice** given all three clinical considerations.
*Hydrochlorothiazide (HCT)*
- While generally safe in asthma, **HCT** is a **thiazide diuretic** that can worsen renal function and **increase creatinine levels**, which is problematic given the patient's already elevated creatinine.
- Although HCT causes **hypokalemia** (low potassium), it is not the preferred agent for managing hyperkalemia, and worsening renal function is a more significant concern here.
- **Amlodipine is safer overall** in this patient.
*Enalapril*
- **Enalapril** is an **ACE inhibitor** that can cause **hyperkalemia**, further worsening the patient's already elevated potassium levels.
- It can also transiently increase **creatinine**, particularly in patients with underlying renal impairment, making it an unfavorable option in this scenario.
*Spironolactone*
- **Spironolactone** is a **potassium-sparing diuretic** that frequently causes **hyperkalemia**, which would be dangerous given the patient's elevated potassium levels.
- It is **contraindicated** in patients with significant hyperkalemia or renal impairment.
*Propranolol*
- **Propranolol** is a **non-selective beta-blocker** that is **contraindicated** in patients with **asthma** as it can cause **bronchospasm** and severe respiratory compromise.
- Beta-blockers should be avoided in asthmatic patients.
ACE inhibitors US Medical PG Question 4: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
ACE inhibitors Explanation: ***Aldosterone***
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
ACE inhibitors US Medical PG Question 5: A 62-year-old man comes to the physician for a follow-up examination. One month ago, therapy with lisinopril was initiated for treatment of hypertension. His blood pressure is 136/86 mm Hg. Urinalysis shows a creatinine clearance of 92 mL/min. The patient's serum creatinine concentration is most likely closest to which of the following values?
- A. 1.7 mg/dL
- B. 1.1 mg/dL (Correct Answer)
- C. 2.0 mg/dL
- D. 1.4 mg/dL
- E. 2.3 mg/dL
ACE inhibitors Explanation: ***1.1 mg/dL***
- For a 62-year-old man with a **creatinine clearance of 92 mL/min**, the serum creatinine can be estimated using the **Cockcroft-Gault relationship**.
- With CrCl of 92 mL/min (near-normal for age), the baseline serum creatinine would be approximately **0.9-1.0 mg/dL** for a typical male patient.
- **Lisinopril (ACE inhibitor)** commonly causes a **mild increase in serum creatinine (10-20%)** due to reduced efferent arteriolar tone, which is acceptable if <30% increase and creatinine clearance remains adequate.
- Therefore, **1.1 mg/dL** represents the expected value: baseline creatinine consistent with CrCl of 92 mL/min plus the typical mild ACE inhibitor-induced elevation.
*1.4 mg/dL*
- A serum creatinine of **1.4 mg/dL** would be inconsistent with a creatinine clearance of **92 mL/min** in this patient.
- Using the Cockcroft-Gault formula for a 62-year-old male, a creatinine of 1.4 mg/dL would correspond to a **CrCl of approximately 65-70 mL/min**, not 92 mL/min.
- This would represent a more significant decrease in GFR than is present in this patient.
*1.7 mg/dL*
- A serum creatinine of **1.7 mg/dL** is far too high for a creatinine clearance of **92 mL/min**.
- This level would correspond to a **CrCl of approximately 50-55 mL/min** in a 62-year-old male, indicating **moderate renal impairment**.
- Such an elevation with ACE inhibitors would warrant investigation for **bilateral renal artery stenosis** or other significant renal pathology.
*2.0 mg/dL*
- A serum creatinine of **2.0 mg/dL** would indicate **significant renal dysfunction** with an estimated CrCl of approximately **40-45 mL/min**, not the 92 mL/min observed.
- This degree of elevation is incompatible with the measured creatinine clearance.
- Would suggest **acute kidney injury** or **severe bilateral renal artery stenosis** and require immediate ACE inhibitor discontinuation.
*2.3 mg/dL*
- A serum creatinine of **2.3 mg/dL** indicates **severe renal impairment** with an estimated CrCl well below 40 mL/min.
- This is completely incompatible with the measured **creatinine clearance of 92 mL/min**.
- Would represent **acute kidney injury** requiring urgent evaluation and medication adjustment.
ACE inhibitors US Medical PG Question 6: A 52-year-old man presents to the emergency department with chest pain radiating to his left jaw and arm. He states that he had experienced similar symptoms when playing basketball. The medical history is significant for diabetes mellitus, hypertension, and GERD, for which he takes metformin, hydrochlorothiazide, and pantoprazole, respectively. The blood pressure is 150/90 mm Hg, the pulse is 100/min, and the respirations are 15/min. The ECG reveals ST elevation in leads V3-V6. He is hospitalized for an acute MI and started on treatment including lisinopril. The next day he complains of dizziness and blurred vision. Repeat vital signs were as follows: blood pressure 90/60 mm Hg, pulse 72/min, and respirations 12/min. The laboratory results were as follows:
Serum chemistry
Sodium 143 mEq/L
Potassium 4.1 mEq/L
Chloride 98 mEq/L
Bicarbonate 22 mEq/L
Blood urea nitrogen 26 mg/dL
Creatinine 2.3 mg/dL
Glucose 120 mg/dL
Which of the following drugs is responsible for this patient's lab abnormalities?
- A. Lisinopril (Correct Answer)
- B. Nitroglycerin
- C. Pantoprazole
- D. Atorvastatin
- E. Digoxin
ACE inhibitors Explanation: ***Lisinopril***
- The patient's **hypotension** (90/60 mmHg), **dizziness**, **blurred vision**, and elevated **creatinine** (2.3 mg/dL) with elevated **BUN** (26 mg/dL) one day after starting lisinopril strongly suggest **acute kidney injury (AKI)** induced by the ACE inhibitor.
- **ACE inhibitors** like lisinopril can cause AKI, especially in patients with pre-existing renal impairment or those with conditions that make them susceptible to reduced renal perfusion, such as **atherosclerotic renovascular disease** (which can be associated with uncontrolled hypertension and diabetes).
*Nitroglycerin*
- **Nitroglycerin** primarily causes **vasodilation**, which can lead to **hypotension** and **headache** or **dizziness**, but it is not directly associated with a rapid increase in **creatinine** or **BUN** to this extent, indicative of AKI.
- While it could contribute to hypotension, it wouldn't explain the acute renal dysfunction observed in this patient.
*Pantoprazole*
- **Pantoprazole**, a **proton pump inhibitor**, is generally well-tolerated but can rarely cause **acute interstitial nephritis**, which might lead to AKI over a longer period.
- However, it would not typically cause such a rapid and significant increase in **BUN** and **creatinine** immediately after an MI and starting other medications, and it's less likely to be the primary cause of acute decompensation compared to an ACE inhibitor in this context.
*Atorvastatin*
- **Atorvastatin** is a **HMG-CoA reductase inhibitor** used for lipid lowering. Its main side effects include **myopathy** and **liver dysfunction**, neither of which are reflected in the presented symptoms or lab findings.
- It does not directly cause **hypotension** or acute **renal dysfunction**.
*Digoxin*
- **Digoxin** is a **cardiac glycoside** used to treat heart failure and arrhythmias. Its toxicity can cause **nausea**, **vomiting**, **arrhythmias**, and **visual disturbances** (e.g., blurred or yellow vision).
- While visual disturbances are present, digoxin is not associated with acute **hypotension** or acute **kidney injury** characterized by elevated **BUN** and **creatinine**.
ACE inhibitors US Medical PG Question 7: A 70-year-old man presents to his primary care physician for a general checkup. He states that he has been doing well and taking his medications as prescribed. He recently started a new diet and supplement to improve his health and has started exercising. The patient has a past medical history of diabetes, a myocardial infarction, and hypertension. He denies any shortness of breath at rest or with exertion. An ECG is performed and is within normal limits. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 6.7 mEq/L
HCO3-: 25 mEq/L
Glucose: 133 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most likely cause of this patient's presentation?
- A. Medication (Correct Answer)
- B. Acute renal failure
- C. Hemolysis
- D. Dietary changes
- E. Rhabdomyolysis
ACE inhibitors Explanation: ***Medication***
- The patient's **hyperkalemia** (K+ 6.7 mEq/L) despite feeling well, suggests a common side effect of medications, particularly those used for his pre-existing conditions like **hypertension** (**ACE inhibitors**, **ARBs**, **spironolactone**) and **diabetes**.
- Medications are a frequent cause of asymptomatic electrolyte abnormalities, and given his complex medical history and the absence of acute symptoms, this is the most likely culprit.
*Acute renal failure*
- While acute renal failure can cause **hyperkalemia**, it typically presents with other symptoms such as **oliguria**, **fluid retention**, or other signs of organ dysfunction, which are not described.
- The patient is reported to be "doing well" without **shortness of breath** or other acute complaints, making acute renal failure less likely as the primary cause of isolated hyperkalemia.
*Hemolysis*
- **Hemolysis** can release intracellular potassium, leading to **pseudohyperkalemia**, but it would typically be suspected in cases of **blood draw errors** or conditions causing red blood cell breakdown, none of which are indicated.
- The patient's presentation does not include any signs or symptoms suggestive of red cell destruction.
*Dietary changes*
- While an extremely **high-potassium diet** or certain **supplements** could contribute to hyperkalemia, it is less common for dietary changes alone to cause such a significant elevation in a patient with normal organ function.
- Given his medical history, medication-induced hyperkalemia is a more direct and common explanation.
*Rhabdomyolysis*
- **Rhabdomyolysis** involves the breakdown of muscle tissue, releasing potassium and other intracellular contents, but it is usually associated with significant **muscle pain**, **weakness**, and elevated **creatine kinase**.
- The patient denies these symptoms and has no other indicators pointing towards severe muscle injury.
ACE inhibitors US Medical PG Question 8: A 58-year-old man presents for a follow-up appointment. He recently was found to have a history of stage 2 chronic kidney disease secondary to benign prostatic hyperplasia leading to urinary tract obstruction. He has no other medical conditions. His father died at age 86 from a stroke, and his mother lives in an assisted living facility. He smokes a pack of cigarettes a day and occasionally drinks alcohol. His vital signs include: blood pressure 130/75 mm Hg, pulse 75/min, respiratory rate 17/min, and temperature 36.5°C (97.7°F). His physical examination is unremarkable. A 24-hour urine specimen reveals the following findings:
Specific gravity 1,050
pH 5.6
Nitrites (-)
Glucose (-)
Proteins 250 mg/24hrs
Which of the following should be prescribed to this patient to decrease his cardiovascular risk?
- A. Enalapril (Correct Answer)
- B. Ezetimibe
- C. Amlodipine
- D. Carvedilol
- E. Aspirin
ACE inhibitors Explanation: ***Enalapril***
- **Enalapril**, an ACE inhibitor, is indicated for patients with **chronic kidney disease** and **proteinuria** to reduce cardiovascular risk and slow kidney disease progression.
- The patient has stage 2 CKD and **250 mg/24hrs of protein in urine**, which, when coupled with hypertension, makes ACE inhibitors the preferred choice to mitigate cardiovascular risk.
*Ezetimibe*
- **Ezetimibe** is a **cholesterol absorption inhibitor** used to lower LDL-C, but there is no information in the vignette to suggest hyperlipidemia.
- It is an inappropriate choice without evidence of dyslipidemia or a strong indication for lipid-lowering therapy.
*Amlodipine*
- **Amlodipine** is a **calcium channel blocker** used to treat hypertension but does not provide specific renal-protective benefits in patients with proteinuria.
- It would be a consideration for blood pressure control if an ACE inhibitor were contraindicated or insufficient.
*Carvedilol*
- **Carvedilol** is a **beta-blocker** used for hypertension, heart failure, and post-MI, but there is no indication for its use here.
- It is not the first-line agent for cardiovascular risk reduction in patients with chronic kidney disease and proteinuria without other specific cardiac indications.
*Aspirin*
- **Aspirin** is used for primary or secondary prevention of cardiovascular events due to its **antiplatelet effects**. However, in the absence of established cardiovascular disease, its use for primary prevention in CKD patients needs careful consideration of bleeding risk.
- While patients with CKD are at higher cardiovascular risk, an ACE inhibitor addresses both the hypertension and proteinuria, which directly contribute to cardiovascular and kidney disease progression in this patient.
ACE inhibitors US Medical PG Question 9: A 38-year-old man presents to his physician with recurrent episodes of facial swelling and abdominal pain. He reports that these episodes started when he was approximately 16 years of age. His mother also has similar episodes of swelling accompanied by swelling of her extremities. The vital signs include: blood pressure 140/80 mm Hg, heart rate 74/min, respiratory rate 17/min, and temperature 36.6℃ (97.8℉). His physical examination is unremarkable. The laboratory work-up shows the following findings:
Test Result Normal range
C1 esterase inhibitor 22% > 60%
Complement C4 level 9 mg/dL 14–40 mg/dL
Complement C2 level 0.8 mg/dL 1.1–3.0 mg/dL
Complement component 1q 17 mg/dL 12–22 mg/dL
Which of the following anti-hypertensive medications is contraindicated in this patient?
- A. Amlodipine
- B. Fosinopril (Correct Answer)
- C. Atenolol
- D. Indapamide
- E. Valsartan
ACE inhibitors Explanation: ***Fosinopril***
- This patient presents with symptoms and lab findings consistent with **hereditary angioedema (HAE)**, characterized by recurrent episodes of **facial swelling** and **abdominal pain**, low C1 esterase inhibitor, and low C4/C2 levels. **ACE inhibitors** like fosinopril are absolutely **contraindicated in HAE** because they can trigger life-threatening angioedema attacks by increasing bradykinin levels.
- The family history of similar swelling further supports the diagnosis of HAE, making any medication that exacerbates bradykinin a significant risk.
*Amlodipine*
- **Dihydropyridine calcium channel blockers** such as amlodipine are generally considered safe in patients with angioedema and do not interfere with the bradykinin pathway.
- They are a suitable option for hypertension management in these patients.
*Atenolol*
- **Beta-blockers** like atenolol are generally safe for managing hypertension in patients with a history of angioedema, as they do not affect the complement or bradykinin systems.
- There is no evidence to suggest that atenolol would worsen angioedema symptoms.
*Indapamide*
- **Thiazide diuretics** such as indapamide are safe and effective antihypertensive agents in patients with angioedema.
- They work by increasing sodium and water excretion and do not interact with the pathways involved in angioedema.
*Valsartan*
- **Angiotensin receptor blockers (ARBs)** like valsartan are generally considered safer than ACE inhibitors in patients with angioedema, although a small risk of angioedema still exists due to their weak effect on bradykinin.
- However, the primary family of drugs to avoid in HAE is ACE inhibitors due to their direct and significant impact on bradykinin degradation.
ACE inhibitors US Medical PG Question 10: A 63-year-old African American man presents to the emergency department with edema over his face and difficulty breathing. Past medical history is significant for hypertension and dyslipidemia. He recently began lisinopril and atorvastatin several weeks ago. His father died at 80 years from complications of a stroke and his mother lives in a nursing home. His blood pressure is 135/92 mm Hg, the heart rate is 101/min, the respiratory rate is 21/min, the temperature is 37.0°C (98.6°F). Clinical pathology results suggest a normal C1 esterase inhibitor level. Of the following options, which is the most likely diagnosis?
- A. Contact dermatitis
- B. Facial lymphedema
- C. Drug-induced angioedema (Correct Answer)
- D. Scleredema
- E. Erysipelas
ACE inhibitors Explanation: ***Drug-induced angioedema***
- The patient's recent initiation of **lisinopril**, an **ACE inhibitor**, is a strong risk factor for developing **angioedema**, particularly in African American individuals.
- The presentation of **facial edema** and **difficulty breathing** without signs of urticaria or pruritus, and normal C1 esterase inhibitor levels, is consistent with ACE inhibitor-induced bradykinin-mediated angioedema.
*Contact dermatitis*
- This condition typically presents with **pruritus**, **erythema**, and sometimes **vesicles** or **bullae**, which are not described in this patient's symptoms.
- It is usually localized to the area of contact with an allergen or irritant and would be unlikely to cause such acute respiratory distress without other prominent skin manifestations.
*Facial lymphedema*
- **Lymphedema** generally develops **gradually** and is characterized by chronic, non-pitting edema due to impaired lymphatic drainage.
- It would not typically present with acute onset **difficulty breathing** as a primary symptom.
*Scleredema*
- **Scleredema** is a rare connective tissue disorder characterized by diffuse, non-pitting hardening and thickening of the skin, often on the back, neck, and face.
- It is a **chronic condition** and does not typically cause acute onset of facial edema and respiratory distress.
*Erysipelas*
- **Erysipelas** is a superficial skin infection characterized by a well-demarcated, erythematous, warm, and tender plaque, often accompanied by fever and systemic symptoms.
- The patient's presentation of painless facial edema and difficulty breathing without clear signs of infection makes erysipelas less likely.
More ACE inhibitors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.