Treatment guidelines for invasive fungal infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Treatment guidelines for invasive fungal infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Treatment guidelines for invasive fungal infections US Medical PG Question 1: You are taking care of a patient with renal failure secondary to anti-fungal therapy. The patient is a 66-year-old male being treated for cryptococcal meningitis. This drug has a variety of known side effects including acute febrile reactions to infusions, anemia, hypokalemia and hypomagnesemia. What is the mechanism of action of this drug?
- A. Inhibition of squalene epoxidase
- B. Binding of the 50S subunit
- C. Pore formation secondary to ergosterol binding (Correct Answer)
- D. Disruption of microtubule formation
- E. Inhibition of 1,3-beta-glucan synthase
Treatment guidelines for invasive fungal infections Explanation: ***Pore formation secondary to ergosterol binding***
- This describes the mechanism of action of **amphotericin B**, the antifungal agent used for cryptococcal meningitis.
- Amphotericin B binds to **ergosterol** in the fungal cell membrane, leading to the formation of pores, disruption of membrane integrity, and ultimately cell death.
- The side effects described—**nephrotoxicity with renal failure, hypokalemia, and hypomagnesemia**—are classic adverse effects of amphotericin B due to its effect on renal tubular cells and electrolyte wasting.
*Inhibition of squalene epoxidase*
- This is the mechanism of action for **terbinafine**, an antifungal primarily used for dermatophyte infections (e.g., onychomycosis), not systemic infections like cryptococcal meningitis.
- Terbinafine inhibits ergosterol synthesis at an earlier step but does not cause the severe nephrotoxicity and electrolyte disturbances described.
*Binding of the 50S subunit*
- This mechanism of action is characteristic of **macrolide antibiotics** like azithromycin or clarithromycin, which are antibacterial agents, not antifungals.
- These drugs inhibit bacterial protein synthesis and are ineffective against fungal infections.
*Disruption of microtubule formation*
- This is the mechanism of action for **griseofulvin**, an antifungal drug used for dermatophyte infections of the skin, hair, and nails.
- Griseofulvin interferes with fungal cell division and is not used for life-threatening systemic infections like cryptococcal meningitis.
*Inhibition of 1,3-beta-glucan synthase*
- This mechanism is associated with **echinocandins** (e.g., caspofungin, micafungin), which inhibit fungal cell wall synthesis.
- While echinocandins are used for some systemic fungal infections (particularly Candida and Aspergillus), they do not typically cause the severe renal failure and electrolyte disturbances characteristic of amphotericin B.
Treatment guidelines for invasive fungal infections US Medical PG Question 2: A 69-year-old man with metastatic colon cancer is brought to the emergency department because of shortness of breath, fever, chills, and a productive cough with streaks of blood for the past 5 days. He has a history of emphysema. The patient does not have abdominal pain or headache. He receives chemotherapy with 5-fluorouracil, leucovorin, and oxaliplatin every 6 weeks; his last cycle was 3 weeks ago. His temperature is 38.3°C (101°F), pulse is 112/min, and blood pressure is 100/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 83%. A few scattered inspiratory crackles are heard over the right lung. His mucous membranes are dry. Cardiac examination is normal. Laboratory studies show:
Hemoglobin 9.3 mg/dL
Leukocyte count 700/mm3
Segmented neutrophils 68%
Lymphocytes 25%
Eosinophils 4%
Monocytes 3%
Platelet count 104,000/mm3
Serum
Glucose 75 mg/dL
Urea nitrogen 41 mg/dL
Creatinine 2.1 mg/dL
Galactomannan antigen Positive
Which of the following is the most appropriate initial pharmacotherapy?
- A. Ceftriaxone and azithromycin
- B. Rifampin, isoniazid, pyrazinamide, and ethambutol
- C. Ceftazidime and levofloxacin
- D. Piperacillin-tazobactam
- E. Voriconazole (Correct Answer)
Treatment guidelines for invasive fungal infections Explanation: ***Voriconazole***
- The patient has **neutropenic fever** (leukocyte count 700/mm3, recent chemotherapy) with pulmonary symptoms and a positive **galactomannan antigen**, which is highly suggestive of **invasive aspergillosis**.
- **Voriconazole** is the recommended first-line agent for the treatment of **invasive aspergillosis**.
*Ceftriaxone and azithromycin*
- This combination is typically used for **community-acquired pneumonia**, targeting common bacterial pathogens like *Streptococcus pneumoniae* and atypical bacteria.
- It does not cover **fungal infections** like aspergillosis, nor does it provide broad-spectrum gram-negative coverage suitable for neutropenic fever.
*Rifampin, isoniazid, pyrazinamide, and ethambutol*
- This four-drug regimen is the standard treatment for **active tuberculosis**.
- There is no clinical or laboratory evidence (e.g., acid-fast bacilli smear, cultures) to suggest tuberculosis in this patient.
*Ceftazidime and levofloxacin*
- **Ceftazidime** is a third-generation cephalosporin with good gram-negative coverage, including *Pseudomonas*, which might be considered in neutropenic fever. However, it lacks adequate gram-positive coverage.
- **Levofloxacin** is a fluoroquinolone that provides broad-spectrum coverage, but this combination still misses the likely fungal pathogen and is not ideal for initial empiric therapy in severe neutropenic fever.
*Piperacillin-tazobactam*
- **Piperacillin-tazobactam** is a broad-spectrum antibiotic with good coverage against both gram-positive and gram-negative bacteria, including *Pseudomonas aeruginosa*, making it a common choice for **empiric therapy in neutropenic fever**.
- However, it does not cover **fungal infections**, which are strongly indicated by the positive **galactomannan antigen** in this immunocompromised patient.
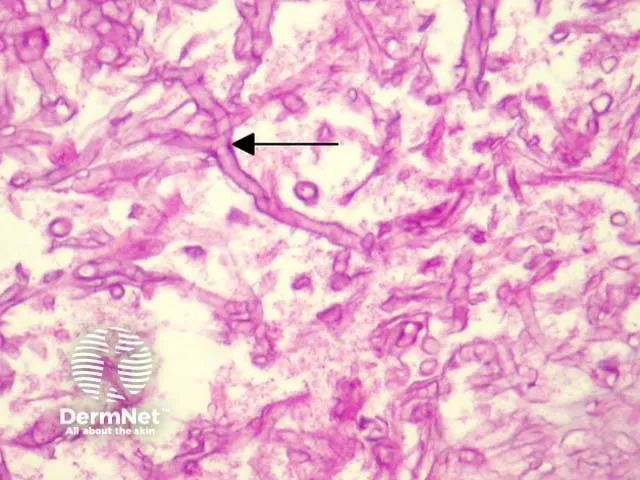
Treatment guidelines for invasive fungal infections US Medical PG Question 3: A 65-year-old woman who lives in New York City presents with headache, fever, and neck stiffness. She received a diagnosis of HIV infection 3 years ago and has been inconsistent with her antiretroviral medications. Recent interferon-gamma release assay testing for latent tuberculosis was negative. A computed tomography of her head is normal. A lumbar puncture shows a white blood cell count of 45/mm3 with a mononuclear predominance, the glucose level of 30 mg/dL, and a protein level of 60 mg/dL. A preparation of her cerebrospinal fluid is shown. Which of the following organisms is the most likely cause of her symptoms?
- A. Blastomyces dermatitidis
- B. Cryptococcus neoformans (Correct Answer)
- C. Aspergillus fumigatus
- D. Coccidioides immitis
- E. Mycobacterium tuberculosis
Treatment guidelines for invasive fungal infections Explanation: ***Cryptococcus neoformans***
- The patient's presentation with **headache, fever, and neck stiffness** in the setting of **HIV infection with poor medication adherence** (indicating immunosuppression) is highly suggestive of **cryptococcal meningitis**.
- **CSF findings** of **mononuclear pleocytosis**, **low glucose**, and **elevated protein** are classic for fungal meningitis. The provided image, if showing encapsulated yeast cells, would further confirm *Cryptococcus neoformans*.
*Blastomyces dermatitidis*
- This fungus is common in the **southeastern, south-central, and midwestern United States**, not typically associated with New York City as a primary endemic region.
- While it can cause meningitis in immunocompromised patients, it often presents with **pulmonary involvement** or characteristic **skin lesions** as well, which are not mentioned.
*Aspergillus fumigatus*
- *Aspergillus* infections are typically seen in individuals with **severe neutropenia** or those on **high-dose steroids**, rather than primarily in HIV patients with inconsistent ART.
- While it can cause CNS infections, they often manifest as **brain abscesses** or **vasculitis** and are not characterized by the classic meningitis picture with mononuclear pleocytosis.
*Coccidioides immitis*
- This fungus is endemic to the **southwestern United States** and parts of Central and South America, making it geographically unlikely for a patient living in New York City without a travel history.
- While it can cause meningitis in immunocompromised individuals, the geographical context is a significant differentiating factor.
*Mycobacterium tuberculosis*
- Although **tuberculous meningitis** also presents with mononuclear pleocytosis, low glucose, and elevated protein in the CSF, the **negative interferon-gamma release assay (IGRA)** for latent tuberculosis makes this diagnosis less likely.
- Additionally, CT scans may show **basilar meningeal enhancement** or hydrocephalus in tuberculous meningitis, which is not indicated by a normal CT.
Treatment guidelines for invasive fungal infections US Medical PG Question 4: A 29-year-old woman, gravida 2, para 1, at 10 weeks' gestation comes to the physician for a prenatal visit. Over the past two weeks, she has felt nauseous in the morning and has had vulvar pruritus and dysuria that started 5 days ago. Her first child was delivered by lower segment transverse cesarean section because of macrosomia from gestational diabetes. Her gestational diabetes resolved after the child was born. She appears well. Ultrasound confirms fetal heart tones and an intrauterine pregnancy. Speculum exam shows a whitish chunky discharge. Her vaginal pH is 4.2. A wet mount is performed and microscopic examination is shown. Which of the following is the most appropriate treatment?
- A. Topical nystatin
- B. Oral fluconazole
- C. Intravaginal clotrimazole (Correct Answer)
- D. Oral metronidazole
- E. Intravaginal treatment with lactobacillus
Treatment guidelines for invasive fungal infections Explanation: ***Intravaginal clotrimazole***
- The patient's symptoms of **vulvar pruritus**, **dysuria**, **whitish chunky discharge**, a **vaginal pH of 4.2**, and microscopy consistent with **yeast buds and hyphae** are highly suggestive of **vulvovaginal candidiasis (VVC)**.
- **Intravaginal azole antifungals** like clotrimazole are the **first-line treatment for VVC in pregnancy** due to their local action and minimal systemic absorption, making them safe for the fetus.
*Topical nystatin*
- While **nystatin** is an antifungal used for candidiasis, its **efficacy for vulvovaginal candidiasis is lower** compared to azoles.
- **Topical nystatin** is generally **not the preferred first-line treatment** for VVC, especially when more effective alternatives like azoles are available.
*Oral fluconazole*
- **Oral fluconazole** is generally **avoided in the first trimester of pregnancy** due to potential risks of **teratogenicity**, including an increased risk of miscarriage and congenital malformations at higher doses, though lower single doses are considered by some to be low risk.
- Given the patient is at **10 weeks' gestation**, topical treatment is preferred over oral options to minimize systemic exposure.
*Oral metronidazole*
- **Metronidazole** is an **antibiotic and antiprotozoal** medication primarily used to treat **bacterial vaginosis** or **trichomoniasis**, conditions that do not match the patient's presentation.
- The patient's **vaginal pH of 4.2** and **chunky discharge** differentiate VVC from bacterial vaginosis (which typically has a pH >4.5 and thin, malodorous discharge) or trichomoniasis (often frothy discharge and high pH).
*Intravaginal treatment with lactobacillus*
- **Lactobacillus** is used to help restore the normal vaginal flora, often as an **adjunctive treatment** or for prophylaxis, particularly in cases of **recurrent bacterial vaginosis** or after antibiotic therapy.
- It is **not a primary treatment for active fungal infections** like vulvovaginal candidiasis, as it does not directly eradicate the yeast.
Treatment guidelines for invasive fungal infections US Medical PG Question 5: A 62-year-old man is brought to the emergency department from a senior-care facility after he was found with a decreased level of consciousness and fever. His personal history is relevant for colorectal cancer that was managed with surgical excision of the tumor. Upon admission, he is found to have a blood pressure of 130/80 mm Hg, a pulse of 102/min, a respiratory rate of 20/min, and a body temperature 38.8°C (101.8°F). There is no rash on physical examination; he is found to have neck rigidity, confusion, and photophobia. There are no focal neurological deficits. A head CT is normal without mass or hydrocephalus. A lumbar puncture was performed and cerebrospinal fluid (CSF) is sent to analysis while ceftriaxone and vancomycin are started. Which of the following additional antimicrobials should be added in the management of this patient?
- A. Trimethoprim-sulfamethoxazole (TMP-SMX)
- B. Ampicillin (Correct Answer)
- C. Amphotericin
- D. Meropenem
- E. Clindamycin
Treatment guidelines for invasive fungal infections Explanation: ***Ampicillin***
- This patient is a 62-year-old, indicating an increased risk for **Listeria monocytogenes** meningitis, which is typically susceptible to ampicillin.
- Given his age and presentation with **meningeal signs** and fever, empirical coverage for Listeria with ampicillin is crucial, especially before CSF culture results are known.
*Trimethoprim-sulfamethoxazole (TMP-SMX)*
- While TMP-SMX can cover Listeria, it is generally considered a **second-line agent** for severe infections like meningitis due to slower bactericidal activity and potential for higher rates of treatment failure compared to ampicillin.
- Ampicillin is the **preferred first-line treatment** for Listeria meningitis unless there is a specific contraindication.
*Amphotericin*
- Amphotericin is an **antifungal agent** used for fungal meningitis.
- Although fungemia can occur in immunocompromised individuals or those with indwelling catheters, the initial presentation with bacterial meningitis symptoms and absence of specific risk factors for fungal infection do not support its empirical use.
*Meropenem*
- Meropenem is a **carbapenem** with a broad spectrum of activity, including many gram-negative and gram-positive bacteria, and some anaerobes.
- While it has good CNS penetration and could cover some organisms like penicillin-resistant S. pneumoniae or gram-negative rods, it is not the primary empirical choice specifically for **Listeria monocytogenes**, and there's no indication for its broad-spectrum coverage over standard empirical therapy currently.
*Clindamycin*
- Clindamycin is primarily active against **gram-positive bacteria**, especially anaerobes and some staphylococci and streptococci.
- It has **poor penetration into the CNS** and is therefore not effective for meningitis treatment, especially for common bacterial pathogens or Listeria.
Treatment guidelines for invasive fungal infections US Medical PG Question 6: A potassium hydroxide preparation is conducted on a skin scraping of the hypopigmented area. Microscopy of the preparation shows long hyphae among clusters of yeast cells. Based on these findings, which of the following is the most appropriate pharmacotherapy?
- A. Topical corticosteroid
- B. Oral ketoconazole
- C. Topical selenium sulfide (Correct Answer)
- D. Topical nystatin
- E. Oral fluconazole
Treatment guidelines for invasive fungal infections Explanation: ***Topical selenium sulfide***
- The presence of **long hyphae** and **clusters of yeast cells** on KOH prep is characteristic of **tinea versicolor**, caused by *Malassezia furfur*.
- **Selenium sulfide** is a common and effective topical antifungal agent for tinea versicolor, available in shampoos and lotions.
*Topical corticosteroid*
- **Corticosteroids** have anti-inflammatory properties but do not treat fungal infections.
- Using corticosteroids alone would only mask symptoms and could potentially worsen the fungal infection.
*Oral ketoconazole*
- While **oral ketoconazole** is an antifungal, it is generally reserved for extensive or recalcitrant cases of tinea versicolor due to potential systemic side effects, such as **hepatotoxicity**.
- **Topical treatments** are preferred as first-line therapy for localized infections like this one.
*Topical nystatin*
- **Nystatin** is an antifungal agent primarily effective against *Candida* species.
- It is **not effective** against *Malassezia furfur*, the causative agent of tinea versicolor.
*Oral fluconazole*
- **Oral fluconazole** is an effective systemic antifungal used for various *Candida* and dermatophyte infections.
- Similar to oral ketoconazole, it is typically reserved for **widespread or recalcitrant cases** of tinea versicolor, with topical therapy being the preferred initial approach.
Treatment guidelines for invasive fungal infections US Medical PG Question 7: A 45-year-old man presents to the emergency department with difficulties swallowing food. He states that he experiences pain when he attempts to swallow his medications or when he drinks water. He reveals that he was diagnosed with HIV infection five years ago. He asserts that he has been taking his antiretroviral regimen, including emtricitabine, rilpivirine, and tenofovir. His temperature is 98°F (37°C), blood pressure is 100/60 mmHg, pulse is 90/min, respirations are 22/min, and oxygen saturation is 99% on room air. His physical exam is notable for a clear oropharynx, no lymphadenopathy, and a normal cardiac and pulmonary exam. No rashes are noted throughout his body. His laboratory results are displayed below:
Hemoglobin: 12 g/dL
Hematocrit: 37 %
Leukocyte count: 8,000/mm^3 with normal differential
Platelet count: 160,000/mm^3
Serum:
Na+: 138 mEq/L
Cl-: 108 mEq/L
K+: 3.5 mEq/L
HCO3-: 26 mEq/L
BUN: 35 mg/dL
Glucose: 108 mg/dL
Creatinine: 1.1 mg/dL
CD4+ count: 90/mm^3
HIV viral load: 59,000 copies/mL
What is the best next step in management?
- A. Fluconazole (Correct Answer)
- B. Nystatin
- C. Oral swab and microscopy
- D. Methylprednisolone
- E. Esophageal endoscopy and biopsy
Treatment guidelines for invasive fungal infections Explanation: ***Fluconazole***
- The patient's **odynophagia**, low **CD4+ count**, and high **HIV viral load** are highly suggestive of **esophageal candidiasis**.
- **Fluconazole** is the initial empiric treatment of choice for suspected esophageal candidiasis in HIV-positive patients, given its high efficacy and good tolerability.
*Nystatin*
- **Nystatin** is typically used for **oral candidiasis (thrush)**, which presents with white plaques in the mouth.
- The patient has a **clear oropharynx** and **odynophagia**, indicating esophageal involvement, for which nystatin is less effective.
*Oral swab and microscopy*
- While an **oral swab** can confirm oral candidiasis, it is not sufficient for diagnosing **esophageal candidiasis**.
- Given the patient's symptoms of odynophagia and high clinical suspicion in an immunocompromised patient, empiric treatment is preferred over initial diagnostic testing for uncomplicated esophageal candidiasis.
*Methylprednisolone*
- **Methylprednisolone** is a corticosteroid used to reduce inflammation and is not indicated for the treatment of **candidal infections**.
- Using corticosteroids in an immunocompromised patient with an active opportunistic infection could worsen his condition.
*Esophageal endoscopy and biopsy*
- **Esophageal endoscopy and biopsy** are typically reserved for patients who **fail empiric antifungal therapy** or present with **atypical symptoms** not consistent with candidiasis.
- Given the clear clinical picture, initial empiric treatment with fluconazole is the standard first step.
Treatment guidelines for invasive fungal infections US Medical PG Question 8: A 57-year-old woman with non-small cell lung cancer comes to the physician 4 weeks after her tumor was resected. She takes no medications. The physician starts her on a treatment regimen that includes vinblastine. This treatment puts the patient at highest risk for which of the following?
- A. Pulmonary embolism
- B. Invasive fungal infection (Correct Answer)
- C. Progressive multifocal leukoencephalopathy
- D. Pulmonary fibrosis
- E. Heart failure
Treatment guidelines for invasive fungal infections Explanation: ***Invasive fungal infection***
- Vinblastine is an **antimitotic chemotherapy agent** that, like other chemotherapeutic agents, can cause **myelosuppression**.
- **Myelosuppression** (particularly **neutropenia**) severely compromises the immune system, making patients highly susceptible to **opportunistic infections**, including invasive fungal infections.
*Pulmonary embolism*
- While cancer itself is a risk factor for **venous thromboembolism**, including pulmonary embolism, vinblastine itself **does not directly increase the risk** more than other chemotherapy agents.
- The highest risk with vinblastine specifically relates to its impact on bone marrow.
*Progressive multifocal leukoencephalopathy*
- This is a rare, severe opportunistic infection of the brain caused by the **JC virus**, primarily seen in patients with **severe immunosuppression**, such as those with HIV/AIDS or on chronic immunosuppressive therapy (e.g., natalizumab).
- While chemotherapy can cause immunosuppression, PML is not the most common or highest specific risk directly associated with vinblastine or its immediate, acute side effects compared to myelosuppression and opportunistic infections.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a known side effect of certain chemotherapeutic agents like **bleomycin** and **busulfan**, but it is **not a primary or common adverse effect of vinblastine**.
- The side effect profile of vinblastine primarily involves myelosuppression, neurotoxicity, and gastrointestinal effects.
*Heart failure*
- **Cardiotoxicity leading to heart failure** is a significant concern with certain chemotherapy drugs, particularly **anthracyclines** (e.g., doxorubicin) and some tyrosine kinase inhibitors.
- **Vinblastine is not typically associated with cardiotoxicity or heart failure** as a primary or high-risk adverse effect.
Treatment guidelines for invasive fungal infections US Medical PG Question 9: A 54-year-old man presents with fever, abdominal pain, nausea, and bloody diarrhea. He says that his symptoms started 36 hours ago and have not improved. Past medical history is significant for a left-leg abscess secondary to an injury he sustained from a fall 4 days ago while walking his dog. He has been taking clindamycin for this infection. In addition, he has long-standing gastroesophageal reflux disease, managed with omeprazole. His vital signs include: temperature 38.5°C (101.3°F), respiratory rate 19/min, heart rate 90/min, and blood pressure 110/70 mm Hg. Which of the following is the best course of treatment for this patient’s most likely diagnosis?
- A. Tetracycline
- B. Ciprofloxacin
- C. Trimethoprim-sulfamethoxazole
- D. Erythromycin
- E. Vancomycin (Correct Answer)
Treatment guidelines for invasive fungal infections Explanation: ***Vancomycin***
- The patient's history of recent **clindamycin** use for an abscess, development of **fever, abdominal pain, nausea, and bloody diarrhea**, and use of **omeprazole** (a risk factor), strongly suggests **_Clostridioides difficile_ infection (CDI)**.
- **Oral vancomycin** is a first-line treatment for **severe non-fulminant CDI**, which this patient's symptoms (fever, bloody diarrhea) are consistent with.
*Tetracycline*
- **Tetracycline** is typically used for bacterial infections like **chlamydia, Lyme disease, and rickettsial infections**; it is not effective against _C. difficile_.
- It works by **inhibiting bacterial protein synthesis** but does not target the cell wall of _C. difficile_.
*Ciprofloxacin*
- **Ciprofloxacin**, a fluoroquinolone, is generally **contraindicated in CDI** as it can be a risk factor for developing the infection or exacerbate it due to disruption of gut flora.
- While effective against many gram-negative bacteria, it has **no significant activity against _C. difficile_**.
*Trimethoprim-sulfamethoxazole*
- **Trimethoprim-sulfamethoxazole** is a combination antibiotic used for various bacterial infections, including **UTIs and some respiratory infections**.
- It is **not effective against _C. difficile_** and is not recommended for its treatment.
*Erythromycin*
- **Erythromycin**, a macrolide, is effective against a range of bacterial infections including **atypical pneumonia and skin infections**.
- It has **no role in the treatment of _C. difficile_ infection** and its use could potentially further disrupt the gut microbiome.
Treatment guidelines for invasive fungal infections US Medical PG Question 10: A person presents to the hospital with fever and chills. Fever profile is ordered and is found to be negative for malaria and dengue. Rk39 test is found to be positive. What is the treatment of choice?
- A. Amphotericin B (Correct Answer)
- B. Dapsone
- C. Hydroxychloroquine
- D. Griseofulvin
Treatment guidelines for invasive fungal infections Explanation: Amphotericin B
- A positive RK39 test suggests visceral leishmaniasis (kala-azar), especially with fever and chills in an endemic area [1].
- Amphotericin B (specifically liposomal Amphotericin B) is a highly effective and often the drug of choice for treating visceral leishmaniasis, particularly in severe cases or regions with antimonial resistance.
Dapsone
- Dapsone is primarily used in the treatment of leprosy and بعض forms of dermatitis (e.g., dermatitis herpetiformis).
- It has no significant role in treating leishmaniasis.
Hydroxychloroquine
- Hydroxychloroquine is an antimalarial drug also used for certain autoimmune diseases like lupus and rheumatoid arthritis [2].
- It is ineffective against leishmaniasis.
Griseofulvin
- Griseofulvin is an antifungal medication used to treat dermatophyte infections (e.g., ringworm of the skin, hair, or nails).
- It has no activity against Leishmania parasites.
More Treatment guidelines for invasive fungal infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.