Topical antifungal agents US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Topical antifungal agents. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Topical antifungal agents US Medical PG Question 1: A 10-year-old girl presents to the clinic, with her mother, complaining of a circular, itchy rash on her scalp for the past 3 weeks. Her mother is also worried about her hair loss. The girl has a past medical history significant for asthma. She needs to use her albuterol inhaler once per week on average. Her blood pressure is 112/70 mm Hg; the heart rate is 104/min; the respiratory rate is 20/min, and the temperature is 37.0°C (98.6°F). On exam, the patient is alert and interactive. Her lungs are clear on bilateral auscultation. On palpation, a tender posterior cervical node is present on the right side. Examination of the head is shown in the image. Which of the following is the best treatment option for the patient?
- A. Subcutaneous triamcinolone
- B. Topical betamethasone
- C. Ketoconazole shampoo
- D. Oral terbinafine (Correct Answer)
- E. Oral doxycycline
Topical antifungal agents Explanation: ***Oral terbinafine***
- The patient's clinical presentation with an **itchy, circular rash** and **hair loss** on the scalp, along with a **tender posterior cervical node**, is highly suggestive of **tinea capitis**.
- **Oral antifungals** like terbinafine are the **first-line treatment** for tinea capitis because topical agents cannot effectively penetrate the hair shaft where the fungus resides.
*Subcutaneous triamcinolone*
- Triamcinolone is a **corticosteroid** and is used to treat inflammatory conditions, not fungal infections.
- While it might reduce swelling or itching temporarily, it would **not eradicate the underlying fungal infection** and could potentially worsen it.
*Topical betamethasone*
- Betamethasone is a **topical corticosteroid** which might reduce inflammation and itchiness.
- However, topical antifungals and steroids are **ineffective for tinea capitis** as they do not reach the fungal elements within the hair follicles.
*Ketoconazole shampoo*
- While ketoconazole is an antifungal, **shampoo formulations** are generally **not sufficient** to treat tinea capitis on their own.
- They can be used as an **adjunct** to oral therapy to reduce shedding of fungal spores and prevent spread but cannot cure the infection effectively.
*Oral doxycycline*
- Doxycycline is an **antibiotic** primarily used to treat bacterial infections, and some inflammatory skin conditions such as acne or rosacea.
- It has **no antifungal properties** and would be completely ineffective against tinea capitis.
Topical antifungal agents US Medical PG Question 2: A 46-year-old man with HIV infection comes to the physician because of a 1-week history of severe retrosternal pain while swallowing. He has not been compliant with his antiretroviral drug regimen. His CD4+ T-lymphocyte count is 98/mm3 (N ≥ 500). Endoscopy shows white plaques in the esophagus. The most appropriate immediate treatment is a drug that inhibits which of the following enzymes?
- A. DNA polymerase
- B. Hydrogen-potassium ATPase
- C. Cytochrome p450 enzymes (Correct Answer)
- D. Phospholipase A2
- E. Squalene epoxidase
Topical antifungal agents Explanation: ***Cytochrome P450 enzymes***
- The patient's symptoms (retrosternal pain on swallowing, white plaques on endoscopy) and severely low **CD4+ count (98/mm³)** are highly suggestive of **esophageal candidiasis**, a common opportunistic infection in AIDS.
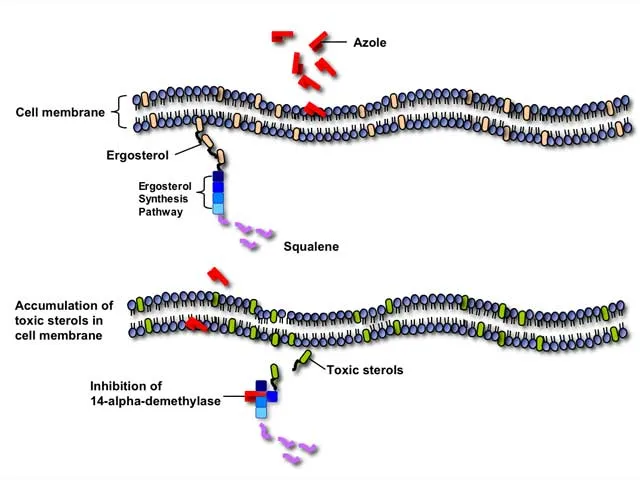
- **Fluconazole**, an azole antifungal, is the **first-line treatment** for esophageal candidiasis and works by inhibiting **14α-demethylase (lanosterol demethylase)**, a fungal **cytochrome P450 enzyme**.
- This inhibition prevents the conversion of lanosterol to ergosterol, disrupting **fungal cell membrane synthesis** and leading to fungal cell death.
*Squalene epoxidase*
- **Terbinafine** and **naftifine** (allylamine antifungals) inhibit squalene epoxidase in the ergosterol synthesis pathway.
- These agents are primarily used for **dermatophyte infections** (onychomycosis, tinea) and have **poor activity against Candida species**.
- They are not appropriate for treating esophageal candidiasis.
*DNA polymerase*
- Inhibitors of **DNA polymerase**, such as acyclovir or ganciclovir, are used to treat **herpesvirus infections** (HSV, CMV).
- While herpes esophagitis can occur in immunocompromised patients, it typically presents with **punched-out ulcers**, not white plaques.
*Hydrogen-potassium ATPase*
- **Proton pump inhibitors** (PPIs) target hydrogen-potassium ATPase in gastric parietal cells to reduce **acid secretion**.
- These are used to treat **GERD** or **peptic ulcers**, which do not present with white plaques on endoscopy.
- While PPIs may provide symptomatic relief, they do not treat the underlying fungal infection.
*Phospholipase A2*
- Phospholipase A2 inhibitors are used as **anti-inflammatory agents**, as PLA2 releases arachidonic acid, a precursor to inflammatory mediators.
- These drugs have no role in treating fungal infections like esophageal candidiasis.
Topical antifungal agents US Medical PG Question 3: A 22-year-old woman presents to her primary care physician complaining of a red, itchy rash on her elbows and shoulders for 2 months. She has no history of medical problems, and review of systems is positive only for occasional loose stools. She is appropriately prescribed dapsone, which relieves the rash within hours. What is the diagnosis?
- A. Porphyria cutanea tarda
- B. Candida intertrigo
- C. Leprosy
- D. Dermatitis herpetiformis (Correct Answer)
- E. Systemic lupus erythematosus
Topical antifungal agents Explanation: ***Dermatitis herpetiformis***
- The combination of a **red, itchy rash** on the **elbows and shoulders**, occasional **loose stools**, and a rapid response to **dapsone** is highly characteristic of dermatitis herpetiformis.
- This condition is strongly associated with **celiac disease** (explaining the loose stools) and is characterized by IgA deposits in the dermal papillae, which are targeted by dapsone.
*Porphyria cutanea tarda*
- This condition presents with **photosensitive blistering lesions**, often on sun-exposed areas, and is associated with **liver disease** and iron overload, which are not described here.
- While skin fragility and hypertrichosis can occur, the itching and dapsone response are not typical features.
*Candida intertrigo*
- This is a **fungal infection** typically found in **skin folds** (e.g., groin, axilla, inframammary folds) and presents with a beefy red rash with satellite lesions.
- It would not typically affect the elbows and shoulders in this manner, nor would it respond rapidly to dapsone.
*Leprosy*
- Leprosy presents with **hypopigmented or erythematous skin lesions** with **sensory loss** and nerve involvement.
- The symptoms described (itchy rash, specific location, quick dapsone response for itch) are not consistent with leprosy.
*Systemic lupus erythematosus*
- SLE can present with various skin manifestations, including a **malar rash** or discoid lesions, but a highly itchy rash on the elbows and shoulders rapidly responding to dapsone is not typical.
- SLE is a **multi-system autoimmune disease** with other characteristic symptoms (e.g., arthralgia, fatigue, serositis) and laboratory findings that are not mentioned.
Topical antifungal agents US Medical PG Question 4: A 67-year-old man presents to his family physician’s office for a routine visit and to discuss a growth on his toenail that has been gradually enlarging for a month. He has a history of diabetes mellitus, hyperlipidemia, and hypertension and is on metformin, atorvastatin, and lisinopril. He admits to smoking 2 packs of cigarettes daily for the past 45 years. His blood pressure reading today is 132/88 mm Hg, heart rate is 78/min, respiration rate is 12/min and his temperature is 37.1°C (98.8°F). On exam, the patient appears alert and in no apparent distress. Capillary refill is 3 seconds. Diminished dull and sharp sensations are present bilaterally in the lower extremities distal to the mid-tibial region. An image of the patient’s toenail is provided. A potassium hydroxide (KOH) preparation of a nail clipping sample confirms the presence of hyphae. Which of the following treatment options will be most effective for this condition?
- A. Fluconazole
- B. Betamethasone + vitamin D analog
- C. Griseofulvin
- D. Terbinafine (Correct Answer)
- E. Cephalexin
Topical antifungal agents Explanation: ***Terbinafine***
- **Terbinafine** is a highly effective **antifungal medication** used to treat **onychomycosis**, a fungal infection of the nails, confirmed by the presence of hyphae in the KOH preparation.
- It works by inhibiting **squalene epoxidase**, an enzyme essential for fungal cell membrane synthesis, leading to fungicidal action.
*Fluconazole*
- While **fluconazole** is an antifungal medication, it is generally **less effective** than terbinafine for onychomycosis, especially for dermatophyte infections.
- It is often reserved for patients who cannot tolerate terbinafine or have contraindications to it, or for non-dermatophyte molds or yeast infections.
*Griseofulvin*
- **Griseofulvin** is an older antifungal agent that is **less effective** than newer options like terbinafine for onychomycosis and generally requires a much longer treatment course.
- Its use has largely been replaced by more potent and better-tolerated antifungals for nail infections.
*Betamethasone + vitamin D analog*
- This combination is a treatment for **psoriasis**, a chronic inflammatory skin condition that can affect nails, but it is **not effective** against fungal infections.
- The presence of **hyphae** confirmed by KOH preparation rules out psoriasis as the primary diagnosis and indicates a fungal etiology.
*Cephalexin*
- **Cephalexin** is an **antibiotic** used to treat bacterial infections and has **no activity** against fungal pathogens.
- It would be ineffective for onychomycosis, which is a fungal infection.
Topical antifungal agents US Medical PG Question 5: A 72-year-old woman with type 2 diabetes mellitus comes to the physician because she is concerned about the appearance of her toenails. Examination shows yellowish discoloration of all toenails on both feet. The edges of the toenails are lifted, and there is subungual debris. Potassium hydroxide preparation of scrapings from the nails shows multiple branching septate hyphae. Treatment with oral terbinafine is begun. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of squalene epoxidase (Correct Answer)
- B. Formation of pores in cell membrane
- C. Inhibition of β-glucan synthesis
- D. Interference with mitosis during metaphase
- E. Prevention of lanosterol to ergosterol conversion
Topical antifungal agents Explanation: ***Inhibition of squalene epoxidase***
- **Terbinafine** is an **allylamine** antifungal that inhibits the enzyme **squalene epoxidase**, an early step in fungal ergosterol synthesis
- This inhibition leads to the accumulation of **squalene**, which is toxic to the fungal cell, and a deficiency of **ergosterol**, disrupting cell membrane integrity and function
- Terbinafine is highly effective for **onychomycosis** (fungal nail infections) caused by dermatophytes
*Formation of pores in cell membrane*
- This mechanism is characteristic of **polyene antifungals** like **amphotericin B** and **nystatin**
- These drugs bind to **ergosterol** in the fungal cell membrane, creating pores that lead to leakage of intracellular contents and cell death
*Inhibition of β-glucan synthesis*
- This is the primary mechanism of action for **echinocandin** antifungals, such as **caspofungin**, **micafungin**, and **anidulafungin**
- These drugs inhibit **(1,3)-β-D-glucan synthase**, which is essential for the synthesis of glucan, a major component of the fungal cell wall
*Interference with mitosis during metaphase*
- This mechanism is characteristic of **griseofulvin**, another antifungal agent used for dermatophyte infections
- **Griseofulvin** interferes with **microtubule function**, disrupting mitotic spindle formation and preventing fungal cell division
*Prevention of lanosterol to ergosterol conversion*
- This mechanism is associated with **azole antifungals** (e.g., fluconazole, itraconazole), which inhibit fungal **cytochrome P450-dependent 14-α-demethylase**
- This enzyme is responsible for the conversion of **lanosterol** to **ergosterol**, leading to ergosterol depletion and accumulation of toxic sterol precursors
Topical antifungal agents US Medical PG Question 6: A potassium hydroxide preparation is conducted on a skin scraping of the hypopigmented area. Microscopy of the preparation shows long hyphae among clusters of yeast cells. Based on these findings, which of the following is the most appropriate pharmacotherapy?
- A. Topical corticosteroid
- B. Oral ketoconazole
- C. Topical selenium sulfide (Correct Answer)
- D. Topical nystatin
- E. Oral fluconazole
Topical antifungal agents Explanation: ***Topical selenium sulfide***
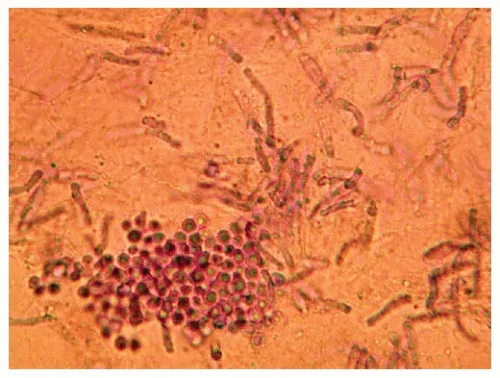
- The presence of **long hyphae** and **clusters of yeast cells** on KOH prep is characteristic of **tinea versicolor**, caused by *Malassezia furfur*.
- **Selenium sulfide** is a common and effective topical antifungal agent for tinea versicolor, available in shampoos and lotions.
*Topical corticosteroid*
- **Corticosteroids** have anti-inflammatory properties but do not treat fungal infections.
- Using corticosteroids alone would only mask symptoms and could potentially worsen the fungal infection.
*Oral ketoconazole*
- While **oral ketoconazole** is an antifungal, it is generally reserved for extensive or recalcitrant cases of tinea versicolor due to potential systemic side effects, such as **hepatotoxicity**.
- **Topical treatments** are preferred as first-line therapy for localized infections like this one.
*Topical nystatin*
- **Nystatin** is an antifungal agent primarily effective against *Candida* species.
- It is **not effective** against *Malassezia furfur*, the causative agent of tinea versicolor.
*Oral fluconazole*
- **Oral fluconazole** is an effective systemic antifungal used for various *Candida* and dermatophyte infections.
- Similar to oral ketoconazole, it is typically reserved for **widespread or recalcitrant cases** of tinea versicolor, with topical therapy being the preferred initial approach.
Topical antifungal agents US Medical PG Question 7: A 45-year-old man presents to the emergency department with difficulties swallowing food. He states that he experiences pain when he attempts to swallow his medications or when he drinks water. He reveals that he was diagnosed with HIV infection five years ago. He asserts that he has been taking his antiretroviral regimen, including emtricitabine, rilpivirine, and tenofovir. His temperature is 98°F (37°C), blood pressure is 100/60 mmHg, pulse is 90/min, respirations are 22/min, and oxygen saturation is 99% on room air. His physical exam is notable for a clear oropharynx, no lymphadenopathy, and a normal cardiac and pulmonary exam. No rashes are noted throughout his body. His laboratory results are displayed below:
Hemoglobin: 12 g/dL
Hematocrit: 37 %
Leukocyte count: 8,000/mm^3 with normal differential
Platelet count: 160,000/mm^3
Serum:
Na+: 138 mEq/L
Cl-: 108 mEq/L
K+: 3.5 mEq/L
HCO3-: 26 mEq/L
BUN: 35 mg/dL
Glucose: 108 mg/dL
Creatinine: 1.1 mg/dL
CD4+ count: 90/mm^3
HIV viral load: 59,000 copies/mL
What is the best next step in management?
- A. Fluconazole (Correct Answer)
- B. Nystatin
- C. Oral swab and microscopy
- D. Methylprednisolone
- E. Esophageal endoscopy and biopsy
Topical antifungal agents Explanation: ***Fluconazole***
- The patient's **odynophagia**, low **CD4+ count**, and high **HIV viral load** are highly suggestive of **esophageal candidiasis**.
- **Fluconazole** is the initial empiric treatment of choice for suspected esophageal candidiasis in HIV-positive patients, given its high efficacy and good tolerability.
*Nystatin*
- **Nystatin** is typically used for **oral candidiasis (thrush)**, which presents with white plaques in the mouth.
- The patient has a **clear oropharynx** and **odynophagia**, indicating esophageal involvement, for which nystatin is less effective.
*Oral swab and microscopy*
- While an **oral swab** can confirm oral candidiasis, it is not sufficient for diagnosing **esophageal candidiasis**.
- Given the patient's symptoms of odynophagia and high clinical suspicion in an immunocompromised patient, empiric treatment is preferred over initial diagnostic testing for uncomplicated esophageal candidiasis.
*Methylprednisolone*
- **Methylprednisolone** is a corticosteroid used to reduce inflammation and is not indicated for the treatment of **candidal infections**.
- Using corticosteroids in an immunocompromised patient with an active opportunistic infection could worsen his condition.
*Esophageal endoscopy and biopsy*
- **Esophageal endoscopy and biopsy** are typically reserved for patients who **fail empiric antifungal therapy** or present with **atypical symptoms** not consistent with candidiasis.
- Given the clear clinical picture, initial empiric treatment with fluconazole is the standard first step.
Topical antifungal agents US Medical PG Question 8: A 41-year-old man comes to the physician because of a 3-week history of fatigue, cough, and a 4.5-kg (10-lb) weight loss. He does not smoke or drink alcohol. He appears emaciated. A chest x-ray shows a calcified nodule in the left lower lobe and left hilar lymphadenopathy. The physician initiates therapy for the condition and informs him that he will have to return for monthly ophthalmologic examination for the next 2 months. These examinations are most likely to evaluate the patient for an adverse effect of a drug with which of the following mechanisms of action?
- A. Impaired synthesis of mycolic acids
- B. Impaired protein synthesis due to binding to 50S ribosomes
- C. Impaired production of hemozoin from heme
- D. Impaired synthesis of cell wall polysaccharides (Correct Answer)
- E. Impaired protein synthesis due to binding to 30S ribosomes
Topical antifungal agents Explanation: ***Impaired synthesis of cell wall polysaccharides***
- The patient's clinical presentation (fatigue, cough, weight loss, calcified nodule, hilar lymphadenopathy) is classic for **tuberculosis**.
- The requirement for **monthly ophthalmologic examinations** is pathognomonic for **ethambutol** therapy, as this drug causes **optic neuritis** (decreased visual acuity, red-green color blindness).
- **Ethambutol** inhibits **arabinosyl transferase**, which impairs the synthesis of **arabinogalactan**, a key polysaccharide component of the mycobacterial cell wall.
- Due to the risk of optic neuritis, patients on ethambutol require baseline and monthly ophthalmologic monitoring, especially during the first 2 months of therapy.
*Impaired synthesis of mycolic acids*
- This describes the mechanism of **isoniazid (INH)**, a first-line anti-TB drug that inhibits mycolic acid synthesis.
- The main adverse effects of isoniazid are **peripheral neuropathy** (prevented with pyridoxine/vitamin B6) and **hepatotoxicity**, not optic neuritis.
- Isoniazid does not require routine ophthalmologic monitoring.
*Impaired protein synthesis due to binding to 50S ribosomes*
- This mechanism describes **macrolides** (e.g., clarithromycin, azithromycin) and **chloramphenicol**.
- While macrolides may be used for atypical mycobacterial infections, they are not first-line TB therapy and do not cause optic neuritis requiring monthly eye exams.
*Impaired protein synthesis due to binding to 30S ribosomes*
- This mechanism describes **aminoglycosides** (e.g., streptomycin) and **tetracyclines**.
- While streptomycin is a second-line anti-TB drug, its main adverse effects are **ototoxicity** (hearing loss, vestibular dysfunction) and **nephrotoxicity**, not optic neuritis.
- These drugs do not require ophthalmologic monitoring.
*Impaired production of hemozoin from heme*
- This is the mechanism of **chloroquine** and **hydroxychloroquine**, which are antimalarial drugs.
- While chloroquine can cause retinopathy requiring ophthalmologic monitoring, this patient has **tuberculosis**, not malaria.
- The clinical scenario (calcified lung nodule, hilar lymphadenopathy) and TB treatment context make this mechanism incorrect for this case.
Topical antifungal agents US Medical PG Question 9: A 64-year-old woman presents to the clinic with a history of 3 fractures in the past year with the last one being last month. Her bone-density screening from last year reported a T-score of -3.1 and she was diagnosed with osteoporosis. She was advised to quit smoking and was asked to adapt to a healthy lifestyle to which she complied. She was also given calcium and vitamin D supplements. After a detailed discussion with the patient, the physician decides to start her on weekly alendronate. Which of the following statements best describes this patient’s new therapy?
- A. It should be stopped after 10 years due to the risk of esophageal cancer
- B. It is typically used as a second-line therapy for her condition after raloxifene
- C. It can cause hot flashes, flu-like symptoms, and peripheral edema
- D. It must be taken with the first meal of the day due to the significant risk of GI upset
- E. The patient must stay upright for at least 30 minutes after taking this medication (Correct Answer)
Topical antifungal agents Explanation: ***The patient must stay upright for at least 30 minutes after taking this medication***
- This instruction is crucial for **alendronate** (a bisphosphonate) to prevent **esophageal irritation** and potential esophagitis or ulcers.
- Alendronate must be taken with a full glass of plain water on an **empty stomach** at least 30-60 minutes before the first food, beverage, or other medication of the day, and the patient must remain upright.
*It should be stopped after 10 years due to the risk of esophageal cancer*
- The main concern with long-term bisphosphonate use (usually >5 years for oral agents) is the risk of **atypical femoral fractures** and **osteonecrosis of the jaw**, not esophageal cancer.
- While esophageal irritation is a known side effect, the risk of esophageal cancer is **not the primary reason** for treatment discontinuation after 10 years.
*It is typically used as a second-line therapy for her condition after raloxifene*
- **Alendronate** (an oral bisphosphonate) is considered a **first-line therapy** for postmenopausal osteoporosis, especially in patients with a history of fractures and low T-scores.
- **Raloxifene** is a selective estrogen receptor modulator (SERM) typically used when bisphosphonates are contraindicated or not tolerated, or there is a need to also treat breast cancer risk, and it is **less potent** in reducing non-vertebral fractures.
*It can cause hot flashes, flu-like symptoms, and peripheral edema*
- These side effects (hot flashes, flu-like symptoms, peripheral edema) are **not typically associated** with alendronate.
- **Hot flashes** are more common with estrogen-modulating drugs like raloxifene, while **flu-like symptoms** can occur with IV bisphosphonates (like zoledronic acid) or certain anabolic agents.
*It must be taken with the first meal of the day due to the significant risk of GI upset*
- This statement is incorrect; alendronate must be taken on an **empty stomach** (at least 30-60 minutes before the first food or drink) to ensure adequate absorption.
- Taking it with food or other beverages significantly **reduces its absorption**, making it less effective, and the risk of GI upset (specifically esophageal irritation) is why remaining upright and taking with water are stressed.
Topical antifungal agents US Medical PG Question 10: A 12-year-old girl is brought to the physician for a follow-up examination. Two months ago, she was diagnosed with asthma and treatment was begun with an albuterol inhaler as needed. Since then, she has had episodic chest tightness and cough 2–3 times per week. The cough is intermittent and nonproductive; it is worse at night. She has been otherwise healthy and takes no other medications. Her vital signs are within normal limits. Pulmonary examination shows mild expiratory wheezing of all lung fields. Spirometry shows an FEV1:FVC ratio of 81% and an FEV1 of 80% of predicted; FEV1 rises to 93% of predicted after administration of a short-acting bronchodilator. Treatment with low-dose inhaled beclomethasone is begun. The patient is at greatest risk for which of the following adverse effects?
- A. Hypoglycemia
- B. Easy bruisability
- C. Oropharyngeal candidiasis (Correct Answer)
- D. Bradycardia
- E. High-pitched voice
Topical antifungal agents Explanation: ***Oropharyngeal candidiasis***
- **Inhaled corticosteroids** like beclomethasone can suppress the local immune response in the oral cavity and pharynx, leading to opportunistic fungal infections.
- This condition, commonly known as **thrush**, presents as white patches on the tongue and oral mucosa, which can be mitigated by rinsing the mouth after inhaler use.
*Hypoglycemia*
- **Inhaled corticosteroids** typically have minimal systemic absorption at low doses and are not associated with hypoglycemia.
- **Hypoglycemia** is more commonly associated with diabetes treatment or conditions affecting glucose regulation.
*Easy bruisability*
- While **systemic corticosteroids** can cause skin thinning and easy bruising with long-term use, **inhaled corticosteroids** at low doses have very limited systemic effects.
- The risk of easy bruisability is extremely low with the prescribed treatment in this patient.
*Bradycardia*
- **Beta-agonists** (like albuterol) can cause tachycardia, but inhaled corticosteroids themselves do not significantly affect heart rate.
- **Bradycardia** is not a characteristic adverse effect of beclomethasone; it is typically associated with certain cardiac conditions or medications like beta-blockers.
*High-pitched voice*
- **Inhaled corticosteroids** can sometimes lead to hoarseness or dysphonia due to local irritation or candidiasis of the vocal cords, but not specifically to a high-pitched voice.
- A high-pitched voice is not a recognized adverse effect; rather, a change in voice quality such as hoarseness is more typical.
More Topical antifungal agents US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.