Terbinafine US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Terbinafine. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Terbinafine US Medical PG Question 1: You are seeing a patient in clinic who recently started treatment for active tuberculosis. The patient is currently being treated with rifampin, isoniazid, pyrazinamide, and ethambutol. The patient is not used to taking medicines and is very concerned about side effects. Specifically regarding the carbohydrate polymerization inhibiting medication, which of the following is a known side effect?
- A. Vision loss (Correct Answer)
- B. Paresthesias of the hands and feet
- C. Cutaneous flushing
- D. Arthralgias
- E. Elevated liver enzymes
Terbinafine Explanation: ***Vision loss***
- The "carbohydrate polymerization inhibiting medication" refers to **ethambutol**, which inhibits **arabinosyl transferase** (involved in mycobacterial cell wall arabinogalactan synthesis)
- **Ethambutol** causes **optic neuritis**, leading to **decreased visual acuity**, **red-green color blindness**, and potentially **irreversible vision loss**
- **Regular ophthalmologic monitoring** is essential during ethambutol therapy
*Paresthesias of the hands and feet*
- This describes **peripheral neuropathy** caused by **isoniazid**
- Isoniazid interferes with **pyridoxine (vitamin B6) metabolism**, leading to neurotoxicity
- Risk factors include malnutrition, diabetes, alcoholism, and pregnancy
- Prevented by **pyridoxine supplementation**
*Cutaneous flushing*
- Not a characteristic side effect of first-line anti-tuberculosis medications
- More commonly associated with niacin or certain allergic/vasodilatory reactions
*Arthralgias*
- Classic side effect of **pyrazinamide**, often affecting small joints
- Caused by **pyrazinamide-induced hyperuricemia** (inhibits renal uric acid excretion)
- May require dose adjustment or discontinuation if severe
*Elevated liver enzymes*
- **Hepatotoxicity** can occur with **rifampin**, **isoniazid**, and **pyrazinamide**
- Requires regular monitoring of liver function tests during TB treatment
- Most common serious adverse effect of combination TB therapy
Terbinafine US Medical PG Question 2: A scientist is studying the excretion of a novel toxin X by the kidney in order to understand the dynamics of this new substance. He discovers that this new toxin X has a clearance that is half that of inulin in a particular patient. This patient's filtration fraction is 20% and his para-aminohippuric acid (PAH) dynamics are as follows:
Urine volume: 100 mL/min
Urine PAH concentration: 30 mg/mL
Plasma PAH concentration: 5 mg/mL
Given these findings, what is the clearance of the novel toxin X?
- A. 1,500 mL/min
- B. 600 mL/min
- C. 300 mL/min
- D. 60 mL/min (Correct Answer)
- E. 120 mL/min
Terbinafine Explanation: ***60 ml/min***
- First, calculate the **renal plasma flow (RPF)** using PAH clearance: RPF = (Urine PAH conc. × Urine vol.) / Plasma PAH conc. = (30 mg/mL × 100 mL/min) / 5 mg/mL = 600 mL/min.
- Next, calculate the **glomerular filtration rate (GFR)**, which is the clearance of inulin. GFR = RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min. Toxin X clearance is half of inulin clearance, so 120 mL/min / 2 = **60 mL/min**.
*1,500 ml/min*
- This value is likely obtained if an incorrect formula or conversion was made, possibly by misinterpreting the units or the relationship between GFR, RPF, and filtration fraction.
- It significantly overestimates the clearance for a substance that is cleared at half the rate of inulin.
*600 ml/min*
- This value represents the **renal plasma flow (RPF)**, calculated using the PAH clearance data.
- It does not account for the filtration fraction or the fact that toxin X clearance is half of inulin clearance (GFR).
*300 ml/min*
- This value would be obtained if the renal plasma flow (RPF) was incorrectly halved, or if an intermediate calculation was misinterpreted as the final answer.
- It does not align with the given filtration fraction and the relationship between toxin X and inulin clearance.
*120 ml/min*
- This value represents the **glomerular filtration rate (GFR)**, which is equal to the clearance of inulin (RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min).
- The question states that the clearance of toxin X is **half** that of inulin, so this is an intermediate step, not the final answer.
Terbinafine US Medical PG Question 3: A 65-year-old man comes to the physician for a routine health maintenance examination. He feels well. His most recent examination 2 years ago included purified protein derivative (PPD) skin testing and showed no abnormalities. He is a retired physician and recently came back from rural China where he completed a voluntary service at a local healthcare center. A PPD skin test is performed. Three days later, an induration of 12 mm is noted. An x-ray of the chest shows no abnormalities. He is started on a drug that inhibits the synthesis of mycolic acid. This patient is at greatest risk of developing which of the following adverse effects?
- A. Cytochrome P-450 induction
- B. Hyperuricemia
- C. Liver injury (Correct Answer)
- D. Optic neuropathy
- E. Nephrotoxicity
Terbinafine Explanation: ***Liver injury***
- The drug described is **isoniazid**, which inhibits **mycolic acid synthesis** and is first-line treatment for **latent tuberculosis infection**.
- **Isoniazid-induced hepatotoxicity** is the most significant adverse effect, with risk increasing dramatically in patients **>35 years old** (this patient is 65).
- Additional risk factors include alcohol use, pre-existing liver disease, and concurrent hepatotoxic medications.
- Patients should be monitored with baseline and periodic liver function tests.
*Cytochrome P-450 induction*
- **Rifampin**, not isoniazid, is a potent **CYP450 inducer** that decreases levels of many co-administered drugs.
- Isoniazid is actually a **CYP450 inhibitor** (inhibits CYP2C19, CYP3A4), which can increase levels of other drugs like phenytoin and warfarin.
*Hyperuricemia*
- **Pyrazinamide** is the anti-tuberculosis drug that causes **hyperuricemia** by inhibiting renal tubular secretion of uric acid.
- This can precipitate acute gout attacks in susceptible patients.
- Isoniazid does not affect uric acid metabolism.
*Optic neuropathy*
- **Ethambutol** causes dose-dependent **optic neuropathy**, presenting with decreased visual acuity and **red-green color blindness**.
- Patients on ethambutol require baseline and monthly visual assessments.
- Isoniazid is not associated with optic toxicity.
*Nephrotoxicity*
- **Aminoglycosides** (e.g., streptomycin) and some other antibiotics cause **nephrotoxicity** through tubular damage.
- Isoniazid is not significantly nephrotoxic and does not require renal dose adjustment.
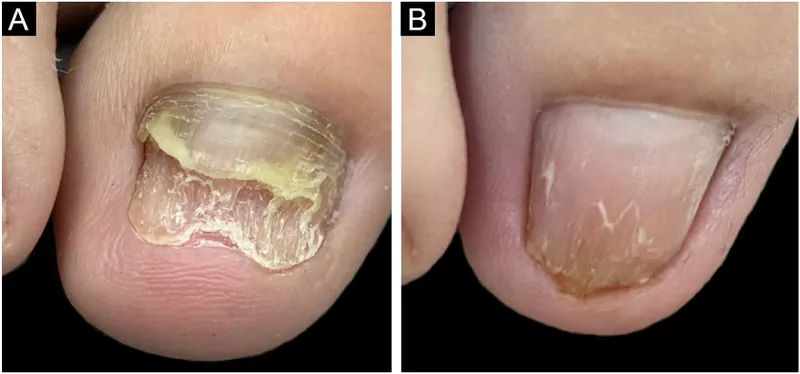
Terbinafine US Medical PG Question 4: A 67-year-old man presents to his family physician’s office for a routine visit and to discuss a growth on his toenail that has been gradually enlarging for a month. He has a history of diabetes mellitus, hyperlipidemia, and hypertension and is on metformin, atorvastatin, and lisinopril. He admits to smoking 2 packs of cigarettes daily for the past 45 years. His blood pressure reading today is 132/88 mm Hg, heart rate is 78/min, respiration rate is 12/min and his temperature is 37.1°C (98.8°F). On exam, the patient appears alert and in no apparent distress. Capillary refill is 3 seconds. Diminished dull and sharp sensations are present bilaterally in the lower extremities distal to the mid-tibial region. An image of the patient’s toenail is provided. A potassium hydroxide (KOH) preparation of a nail clipping sample confirms the presence of hyphae. Which of the following treatment options will be most effective for this condition?
- A. Fluconazole
- B. Betamethasone + vitamin D analog
- C. Griseofulvin
- D. Terbinafine (Correct Answer)
- E. Cephalexin
Terbinafine Explanation: ***Terbinafine***
- **Terbinafine** is a highly effective **antifungal medication** used to treat **onychomycosis**, a fungal infection of the nails, confirmed by the presence of hyphae in the KOH preparation.
- It works by inhibiting **squalene epoxidase**, an enzyme essential for fungal cell membrane synthesis, leading to fungicidal action.
*Fluconazole*
- While **fluconazole** is an antifungal medication, it is generally **less effective** than terbinafine for onychomycosis, especially for dermatophyte infections.
- It is often reserved for patients who cannot tolerate terbinafine or have contraindications to it, or for non-dermatophyte molds or yeast infections.
*Griseofulvin*
- **Griseofulvin** is an older antifungal agent that is **less effective** than newer options like terbinafine for onychomycosis and generally requires a much longer treatment course.
- Its use has largely been replaced by more potent and better-tolerated antifungals for nail infections.
*Betamethasone + vitamin D analog*
- This combination is a treatment for **psoriasis**, a chronic inflammatory skin condition that can affect nails, but it is **not effective** against fungal infections.
- The presence of **hyphae** confirmed by KOH preparation rules out psoriasis as the primary diagnosis and indicates a fungal etiology.
*Cephalexin*
- **Cephalexin** is an **antibiotic** used to treat bacterial infections and has **no activity** against fungal pathogens.
- It would be ineffective for onychomycosis, which is a fungal infection.
Terbinafine US Medical PG Question 5: A 72-year-old woman with type 2 diabetes mellitus comes to the physician because she is concerned about the appearance of her toenails. Examination shows yellowish discoloration of all toenails on both feet. The edges of the toenails are lifted, and there is subungual debris. Potassium hydroxide preparation of scrapings from the nails shows multiple branching septate hyphae. Treatment with oral terbinafine is begun. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of squalene epoxidase (Correct Answer)
- B. Formation of pores in cell membrane
- C. Inhibition of β-glucan synthesis
- D. Interference with mitosis during metaphase
- E. Prevention of lanosterol to ergosterol conversion
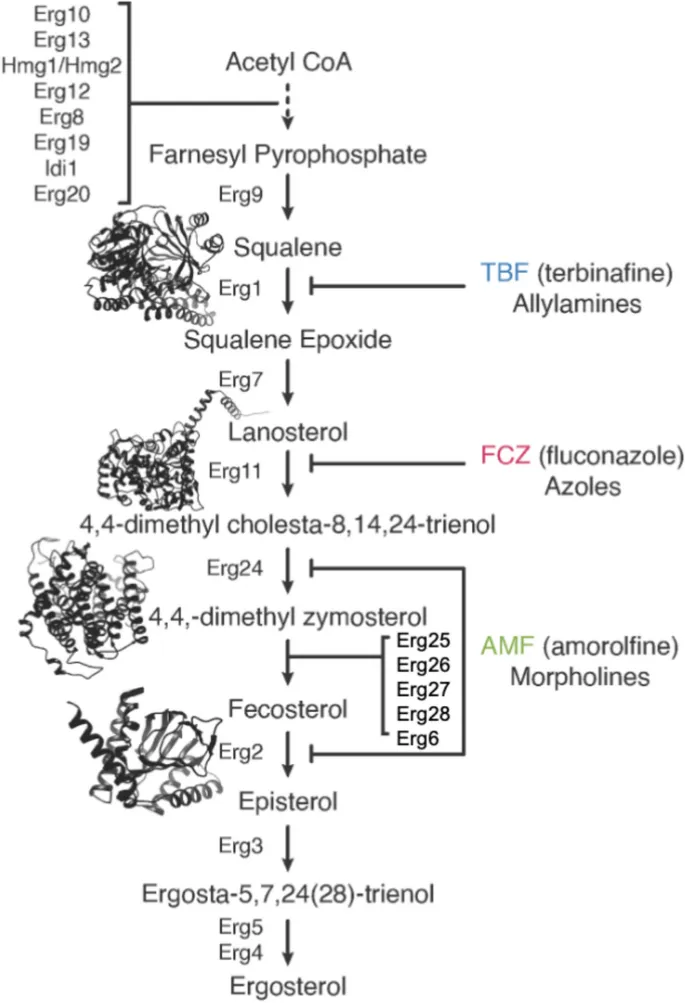
Terbinafine Explanation: ***Inhibition of squalene epoxidase***
- **Terbinafine** is an **allylamine** antifungal that inhibits the enzyme **squalene epoxidase**, an early step in fungal ergosterol synthesis
- This inhibition leads to the accumulation of **squalene**, which is toxic to the fungal cell, and a deficiency of **ergosterol**, disrupting cell membrane integrity and function
- Terbinafine is highly effective for **onychomycosis** (fungal nail infections) caused by dermatophytes
*Formation of pores in cell membrane*
- This mechanism is characteristic of **polyene antifungals** like **amphotericin B** and **nystatin**
- These drugs bind to **ergosterol** in the fungal cell membrane, creating pores that lead to leakage of intracellular contents and cell death
*Inhibition of β-glucan synthesis*
- This is the primary mechanism of action for **echinocandin** antifungals, such as **caspofungin**, **micafungin**, and **anidulafungin**
- These drugs inhibit **(1,3)-β-D-glucan synthase**, which is essential for the synthesis of glucan, a major component of the fungal cell wall
*Interference with mitosis during metaphase*
- This mechanism is characteristic of **griseofulvin**, another antifungal agent used for dermatophyte infections
- **Griseofulvin** interferes with **microtubule function**, disrupting mitotic spindle formation and preventing fungal cell division
*Prevention of lanosterol to ergosterol conversion*
- This mechanism is associated with **azole antifungals** (e.g., fluconazole, itraconazole), which inhibit fungal **cytochrome P450-dependent 14-α-demethylase**
- This enzyme is responsible for the conversion of **lanosterol** to **ergosterol**, leading to ergosterol depletion and accumulation of toxic sterol precursors
Terbinafine US Medical PG Question 6: A potassium hydroxide preparation is conducted on a skin scraping of the hypopigmented area. Microscopy of the preparation shows long hyphae among clusters of yeast cells. Based on these findings, which of the following is the most appropriate pharmacotherapy?
- A. Topical corticosteroid
- B. Oral ketoconazole
- C. Topical selenium sulfide (Correct Answer)
- D. Topical nystatin
- E. Oral fluconazole
Terbinafine Explanation: ***Topical selenium sulfide***
- The presence of **long hyphae** and **clusters of yeast cells** on KOH prep is characteristic of **tinea versicolor**, caused by *Malassezia furfur*.
- **Selenium sulfide** is a common and effective topical antifungal agent for tinea versicolor, available in shampoos and lotions.
*Topical corticosteroid*
- **Corticosteroids** have anti-inflammatory properties but do not treat fungal infections.
- Using corticosteroids alone would only mask symptoms and could potentially worsen the fungal infection.
*Oral ketoconazole*
- While **oral ketoconazole** is an antifungal, it is generally reserved for extensive or recalcitrant cases of tinea versicolor due to potential systemic side effects, such as **hepatotoxicity**.
- **Topical treatments** are preferred as first-line therapy for localized infections like this one.
*Topical nystatin*
- **Nystatin** is an antifungal agent primarily effective against *Candida* species.
- It is **not effective** against *Malassezia furfur*, the causative agent of tinea versicolor.
*Oral fluconazole*
- **Oral fluconazole** is an effective systemic antifungal used for various *Candida* and dermatophyte infections.
- Similar to oral ketoconazole, it is typically reserved for **widespread or recalcitrant cases** of tinea versicolor, with topical therapy being the preferred initial approach.
Terbinafine US Medical PG Question 7: A pharmaceutical company is studying a new drug that inhibits the glucose transporter used by intestinal enterocytes to absorb glucose into the body. The drug was designed such that it would act upon the glucose transporter similarly to how cyanide acts upon cytochrome proteins. During pre-clinical studies, the behavior of this drug on the activity of the glucose transporter is examined. Specifically, enterocyte cells are treated with the drug and then glucose is added to the solution at a concentration that saturates the activity of the transporter. The transport velocity and affinity of the transporters under these conditions are then measured. Compared to the untreated state, which of the following changes would most likely be seen in these transporters after treatment?
- A. Unchanged Km and decreased Vmax (Correct Answer)
- B. Unchanged Km and unchanged Vmax
- C. Increased Km and unchanged Vmax
- D. Increased Km and decreased Vmax
- E. Decreased Km and decreased Vmax
Terbinafine Explanation: ***Unchanged Km and decreased Vmax***
- The drug functions similarly to **cyanide**, which works as a **noncompetitive inhibitor** by binding irreversibly to a site other than the active site
- **Noncompetitive inhibition** results in a **decreased Vmax** (maximum transport velocity) because fewer active transporters are available, but the **Km (substrate affinity) remains unchanged** as the binding affinity of the remaining active transporters is unaffected
- This is the expected pattern when glucose is added at saturating concentrations in the presence of an irreversible noncompetitive inhibitor
*Unchanged Km and unchanged Vmax*
- This would imply no significant effect of the drug on the glucose transporter, which contradicts the drug's design as an inhibitor
- An unaffected Vmax suggests that the maximum transport rate is maintained, and an unchanged Km indicates unaltered affinity—neither of which aligns with the action of a noncompetitive inhibitor
*Increased Km and unchanged Vmax*
- An **increased Km** signifies a **decreased affinity** of the transporter for glucose, which is characteristic of **competitive inhibition**
- An **unchanged Vmax** means the maximum transport rate is still achievable at high substrate concentrations, as competitive inhibitors can be overcome by saturating substrate concentrations
- This pattern does not match the cyanide-like irreversible noncompetitive inhibitor described
*Increased Km and decreased Vmax*
- This pattern suggests **mixed inhibition** or **uncompetitive inhibition**, where both Km and Vmax are affected
- While Vmax is appropriately decreased, the increase in Km indicates reduced affinity, which is not the primary mechanism for a cyanide-like noncompetitive inhibitor that binds irreversibly to a separate site
*Decreased Km and decreased Vmax*
- A **decreased Km** would imply an **increased affinity** of the transporter for glucose, which is not expected from an inhibitor designed to reduce overall transport
- Although Vmax is appropriately decreased, the change in Km does not fit the typical profile of a noncompetitive inhibitor acting in a cyanide-like manner
Terbinafine US Medical PG Question 8: A 46-year-old man with HIV infection comes to the physician because of a 1-week history of severe retrosternal pain while swallowing. He has not been compliant with his antiretroviral drug regimen. His CD4+ T-lymphocyte count is 98/mm3 (N ≥ 500). Endoscopy shows white plaques in the esophagus. The most appropriate immediate treatment is a drug that inhibits which of the following enzymes?
- A. DNA polymerase
- B. Hydrogen-potassium ATPase
- C. Cytochrome p450 enzymes (Correct Answer)
- D. Phospholipase A2
- E. Squalene epoxidase
Terbinafine Explanation: ***Cytochrome P450 enzymes***
- The patient's symptoms (retrosternal pain on swallowing, white plaques on endoscopy) and severely low **CD4+ count (98/mm³)** are highly suggestive of **esophageal candidiasis**, a common opportunistic infection in AIDS.
- **Fluconazole**, an azole antifungal, is the **first-line treatment** for esophageal candidiasis and works by inhibiting **14α-demethylase (lanosterol demethylase)**, a fungal **cytochrome P450 enzyme**.
- This inhibition prevents the conversion of lanosterol to ergosterol, disrupting **fungal cell membrane synthesis** and leading to fungal cell death.
*Squalene epoxidase*
- **Terbinafine** and **naftifine** (allylamine antifungals) inhibit squalene epoxidase in the ergosterol synthesis pathway.
- These agents are primarily used for **dermatophyte infections** (onychomycosis, tinea) and have **poor activity against Candida species**.
- They are not appropriate for treating esophageal candidiasis.
*DNA polymerase*
- Inhibitors of **DNA polymerase**, such as acyclovir or ganciclovir, are used to treat **herpesvirus infections** (HSV, CMV).
- While herpes esophagitis can occur in immunocompromised patients, it typically presents with **punched-out ulcers**, not white plaques.
*Hydrogen-potassium ATPase*
- **Proton pump inhibitors** (PPIs) target hydrogen-potassium ATPase in gastric parietal cells to reduce **acid secretion**.
- These are used to treat **GERD** or **peptic ulcers**, which do not present with white plaques on endoscopy.
- While PPIs may provide symptomatic relief, they do not treat the underlying fungal infection.
*Phospholipase A2*
- Phospholipase A2 inhibitors are used as **anti-inflammatory agents**, as PLA2 releases arachidonic acid, a precursor to inflammatory mediators.
- These drugs have no role in treating fungal infections like esophageal candidiasis.
Terbinafine US Medical PG Question 9: A 62-year-old woman presents to her primary care physician for her annual check-up. She has no current complaints and says that she has been healthy over the last year. Her past medical history is significant for obesity and diabetes that is well controlled on metformin. She does not smoke and drinks socially. Selected lab results are shown below:
High-density lipoprotein: 48 mg/dL
Low-density lipoprotein: 192 mg/dL
Triglycerides: 138 mg/dL
Given these results, the patient is placed on the drug that will be the best therapy for these findings. Which of the following is a potential side effect of this treatment?
- A. Gallstones
- B. Pruritus
- C. Gastrointestinal upset
- D. Malabsorption
- E. Hepatotoxicity (Correct Answer)
Terbinafine Explanation: ***Hepatotoxicity***
- This patient has significantly elevated **LDL cholesterol**, necessitating treatment with a **statin drug** (HMG-CoA reductase inhibitor).
- A known, though rare, side effect of statin therapy is **hepatotoxicity**, which requires monitoring of **liver enzymes**.
*Gallstones*
- **Fibrates** are a class of lipid-lowering drugs that can increase the risk of **gallstone formation** by increasing cholesterol secretion into bile.
- While fibrates lower triglycerides, they are not the primary treatment for significantly elevated LDL as seen in this patient.
*Pruritus*
- **Niacin** (vitamin B3) is a lipid-lowering agent known for causing significant **cutaneous flushing and pruritus** due to prostaglandin release.
- Niacin is not the first-line treatment for high LDL, especially given the side effect burden.
*Gastrointestinal upset*
- **Bile acid sequestrants** (e.g., cholestyramine, colestipol) often cause gastrointestinal side effects such as **constipation, bloating, and nausea**.
- These drugs are typically used in combination with statins or as an alternative in statin-intolerant patients, but statins are the initial choice for high LDL.
*Malabsorption*
- **Ezetimibe**, a cholesterol absorption inhibitor, can rarely cause gastrointestinal discomfort, but it is not typically associated with widespread **malabsorption of nutrients**.
- Its primary role is to block cholesterol absorption in the small intestine, leading to a modest reduction in LDL, often as an add-on therapy.
Terbinafine US Medical PG Question 10: A 64-year-old woman with osteoarthritis presents to the emergency room with a 2-day history of nausea and vomiting. Over the past few weeks, the patient has been taking painkillers to control worsening knee pain. Physical examination reveals scleral icterus and tender hepatomegaly. The patient appears confused. Laboratory investigations reveal the following enzyme levels:
Serum alanine aminotransferase (ALT) 845 U/L
Aspartate aminotransferase (AST) 798 U/L
Alkaline phosphatase 152 U/L
Which of the following is the most appropriate antidote for the toxicity seen in this patient?
- A. N-acetylmuramic acid
- B. N-acetyl-p-benzoquinoneimine
- C. N-acetylcysteine (Correct Answer)
- D. N-acetylaspartic acid
- E. N-acetylglucosamine
Terbinafine Explanation: ***N-acetylcysteine***
- The patient's presentation with nausea, vomiting, confusion, scleral icterus, tender hepatomegaly, and significantly elevated **ALT** and **AST** levels (in the hundreds) after taking painkillers strongly suggests **acetaminophen (paracetamol) toxicity** leading to acute liver failure.
- **N-acetylcysteine (NAC)** is the specific antidote for acetaminophen overdose; it works by replenishing hepatic **glutathione** stores, which are crucial for detoxifying the toxic metabolite **N-acetyl-p-benzoquinone imine (NAPQI)**.
*N-acetylmuramic acid*
- This compound is a component of **bacterial cell walls** and is not involved in human metabolism or toxicology.
- It has no role as an antidote for drug-induced liver injury or any known human toxicity.
*N-acetyl-p-benzoquinoneimine*
- This is the highly reactive and **toxic metabolite of acetaminophen (NAPQI)** that causes liver damage when glutathione stores are depleted.
- It is the substance that NAC helps to detoxify, not an antidote itself.
*N-acetylaspartic acid*
- This molecule is concentrated in the **brain** and is involved in neuronal osmoregulation and energy metabolism.
- It is not an antidote for drug toxicity and is primarily associated with neurological conditions like Canavan disease.
*N-acetylglucosamine*
- This is a **monosaccharide derivative** involved in the biosynthesis of glycoproteins and proteoglycans.
- It has no established role as an antidote for acetaminophen toxicity or any other acute poisoning.
More Terbinafine US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.