Polyenes (amphotericin formulations) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Polyenes (amphotericin formulations). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Polyenes (amphotericin formulations) US Medical PG Question 1: You are taking care of a patient with renal failure secondary to anti-fungal therapy. The patient is a 66-year-old male being treated for cryptococcal meningitis. This drug has a variety of known side effects including acute febrile reactions to infusions, anemia, hypokalemia and hypomagnesemia. What is the mechanism of action of this drug?
- A. Inhibition of squalene epoxidase
- B. Binding of the 50S subunit
- C. Pore formation secondary to ergosterol binding (Correct Answer)
- D. Disruption of microtubule formation
- E. Inhibition of 1,3-beta-glucan synthase
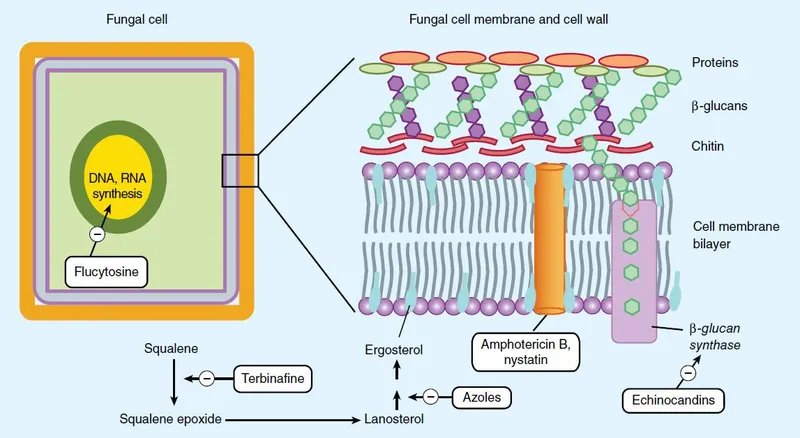
Polyenes (amphotericin formulations) Explanation: ***Pore formation secondary to ergosterol binding***
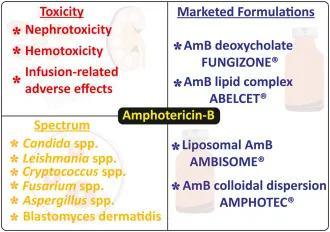
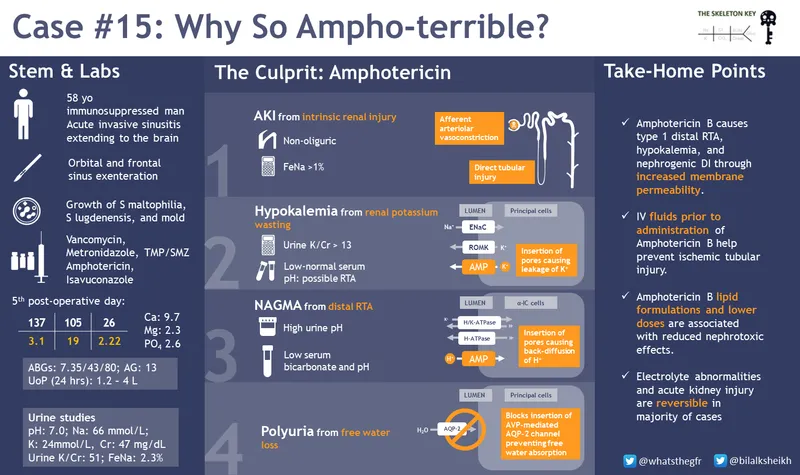
- This describes the mechanism of action of **amphotericin B**, the antifungal agent used for cryptococcal meningitis.
- Amphotericin B binds to **ergosterol** in the fungal cell membrane, leading to the formation of pores, disruption of membrane integrity, and ultimately cell death.
- The side effects described—**nephrotoxicity with renal failure, hypokalemia, and hypomagnesemia**—are classic adverse effects of amphotericin B due to its effect on renal tubular cells and electrolyte wasting.
*Inhibition of squalene epoxidase*
- This is the mechanism of action for **terbinafine**, an antifungal primarily used for dermatophyte infections (e.g., onychomycosis), not systemic infections like cryptococcal meningitis.
- Terbinafine inhibits ergosterol synthesis at an earlier step but does not cause the severe nephrotoxicity and electrolyte disturbances described.
*Binding of the 50S subunit*
- This mechanism of action is characteristic of **macrolide antibiotics** like azithromycin or clarithromycin, which are antibacterial agents, not antifungals.
- These drugs inhibit bacterial protein synthesis and are ineffective against fungal infections.
*Disruption of microtubule formation*
- This is the mechanism of action for **griseofulvin**, an antifungal drug used for dermatophyte infections of the skin, hair, and nails.
- Griseofulvin interferes with fungal cell division and is not used for life-threatening systemic infections like cryptococcal meningitis.
*Inhibition of 1,3-beta-glucan synthase*
- This mechanism is associated with **echinocandins** (e.g., caspofungin, micafungin), which inhibit fungal cell wall synthesis.
- While echinocandins are used for some systemic fungal infections (particularly Candida and Aspergillus), they do not typically cause the severe renal failure and electrolyte disturbances characteristic of amphotericin B.
Polyenes (amphotericin formulations) US Medical PG Question 2: A 57-year-old florist presents to his family physician with nodular lesions on his right hand and forearm. He explains that he got pricked by a rose thorn on his right "pointer finger" where the first lesions appeared, and the other lesions then began to appear in an ascending manner. The physician prescribed a medication and warned him of gynecomastia as a side effect if taken for long periods of time. Which of the following is the mechanism of action of the medication?
- A. Inhibits squalene epoxidase
- B. Binds to ergosterol, forming destructive pores in cell membrane
- C. Disrupts microtubule function
- D. Inhibits ergosterol synthesis (Correct Answer)
- E. Inhibits formation of beta glucan
Polyenes (amphotericin formulations) Explanation: ***Inhibits ergosterol synthesis***
- The clinical presentation of **nodular lesions** on the hand and forearm in an **ascending manner** after a rose thorn prick is characteristic of **sporotrichosis**, caused by *Sporothrix schenckii*.
- **Itraconazole** is the treatment of choice for sporotrichosis, and it works by **inhibiting ergosterol synthesis** via the inhibition of **lanosterol 14-alpha-demethylase**. Gynecomastia is a known side effect of long-term itraconazole use.
*Inhibits squalene epoxidase*
- This is the mechanism of action of **terbinafine**, another antifungal agent.
- While terbinafine is used for some fungal infections, it is **not the first-line treatment for sporotrichosis** and is not typically associated with gynecomastia as a common side effect.
*Binds to ergosterol, forming destructive pores in cell membrane*
- This describes the mechanism of action of **amphotericin B** and **nystatin**.
- Amphotericin B is used for severe systemic fungal infections, but sporotrichosis typically responds well to oral itraconazole, and amphotericin B is reserved for severe or disseminated cases.
*Disrupts microtubule function*
- This is the mechanism of action of **griseofulvin**, an antifungal agent primarily used for dermatophyte infections of the skin, hair, and nails.
- It is **not effective against *Sporothrix schenckii*** and is not associated with the clinical scenario described.
*Inhibits formation of beta glucan*
- This is the mechanism of action of **echinocandins** (e.g., caspofungin, micafungin, anidulafungin).
- Echinocandins are effective against *Candida* and *Aspergillus* species but have **limited activity against dimorphic fungi** like *Sporothrix schenckii*.
Polyenes (amphotericin formulations) US Medical PG Question 3: A 26-year-old female with AIDS (CD4 count: 47) presents to the emergency department in severe pain. She states that over the past week she has been fatigued and has had a progressively worse headache and fever. These symptoms have failed to remit leading her to seek care in the ED. A lumbar puncture is performed which demonstrates an opening pressure of 285 mm H2O, increased lymphocytes, elevated protein, and decreased glucose. The emergency physician subsequently initiates treatment with IV amphotericin B and PO flucytosine. What additional treatment in the acute setting may be warranted in this patient?
- A. Serial lumbar punctures (Correct Answer)
- B. Fluconazole
- C. Mannitol
- D. Chloramphenicol
- E. Acetazolamide
Polyenes (amphotericin formulations) Explanation: **Serial lumbar punctures**
- The elevated opening pressure (285 mm H2O) indicates **increased intracranial pressure (ICP)**, which is common in cryptococcal meningitis and can be life-threatening.
- Serial lumbar punctures can help to **reduce ICP** and relieve symptoms, improving outcomes in patients with cryptococcal meningitis.
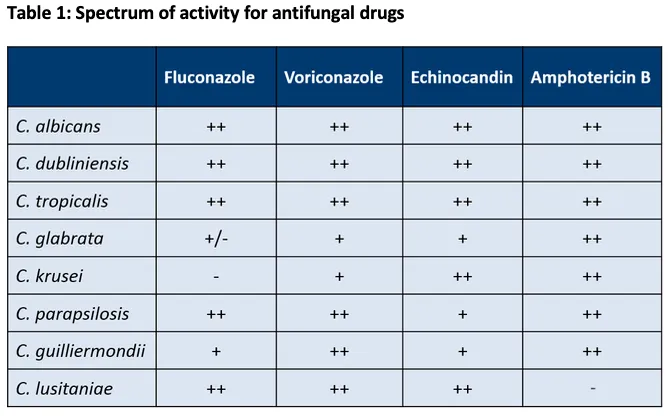
*Fluconazole*
- Fluconazole is used for **maintenance therapy** to prevent relapse after the acute phase of cryptococcal meningitis has been controlled.
- It is generally **not recommended for initial acute treatment** in severe cases due to its fungistatic nature, making it less effective than the combination of amphotericin B and flucytosine.
*Mannitol*
- Mannitol is an **osmotic diuretic** sometimes used to acutely *reduce* ICP in cases of cerebral edema.
- While effective in some situations, it is **not the primary treatment for increased ICP** in cryptococcal meningitis, where repeated LPs are preferred to remove infected CSF and directly reduce pressure.
*Chloramphenicol*
- Chloramphenicol is an **antibiotic** primarily used to treat bacterial infections, not fungal infections.
- It has **no role in the treatment of fungal meningitis** caused by *Cryptococcus neoformans*.
*Acetazolamide*
- Acetazolamide is a **carbonic anhydrase inhibitor** that can reduce CSF production, thereby *reducing* ICP.
- While it can be used in some cases of elevated ICP, routine use in cryptococcal meningitis is **not standard practice**, and serial LPs are generally the preferred method for managing dangerously high ICP in this context due to their immediate efficacy.
Polyenes (amphotericin formulations) US Medical PG Question 4: A 67-year-old man presents to his family physician’s office for a routine visit and to discuss a growth on his toenail that has been gradually enlarging for a month. He has a history of diabetes mellitus, hyperlipidemia, and hypertension and is on metformin, atorvastatin, and lisinopril. He admits to smoking 2 packs of cigarettes daily for the past 45 years. His blood pressure reading today is 132/88 mm Hg, heart rate is 78/min, respiration rate is 12/min and his temperature is 37.1°C (98.8°F). On exam, the patient appears alert and in no apparent distress. Capillary refill is 3 seconds. Diminished dull and sharp sensations are present bilaterally in the lower extremities distal to the mid-tibial region. An image of the patient’s toenail is provided. A potassium hydroxide (KOH) preparation of a nail clipping sample confirms the presence of hyphae. Which of the following treatment options will be most effective for this condition?
- A. Fluconazole
- B. Betamethasone + vitamin D analog
- C. Griseofulvin
- D. Terbinafine (Correct Answer)
- E. Cephalexin
Polyenes (amphotericin formulations) Explanation: ***Terbinafine***
- **Terbinafine** is a highly effective **antifungal medication** used to treat **onychomycosis**, a fungal infection of the nails, confirmed by the presence of hyphae in the KOH preparation.
- It works by inhibiting **squalene epoxidase**, an enzyme essential for fungal cell membrane synthesis, leading to fungicidal action.
*Fluconazole*
- While **fluconazole** is an antifungal medication, it is generally **less effective** than terbinafine for onychomycosis, especially for dermatophyte infections.
- It is often reserved for patients who cannot tolerate terbinafine or have contraindications to it, or for non-dermatophyte molds or yeast infections.
*Griseofulvin*
- **Griseofulvin** is an older antifungal agent that is **less effective** than newer options like terbinafine for onychomycosis and generally requires a much longer treatment course.
- Its use has largely been replaced by more potent and better-tolerated antifungals for nail infections.
*Betamethasone + vitamin D analog*
- This combination is a treatment for **psoriasis**, a chronic inflammatory skin condition that can affect nails, but it is **not effective** against fungal infections.
- The presence of **hyphae** confirmed by KOH preparation rules out psoriasis as the primary diagnosis and indicates a fungal etiology.
*Cephalexin*
- **Cephalexin** is an **antibiotic** used to treat bacterial infections and has **no activity** against fungal pathogens.
- It would be ineffective for onychomycosis, which is a fungal infection.
Polyenes (amphotericin formulations) US Medical PG Question 5: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Polyenes (amphotericin formulations) Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Polyenes (amphotericin formulations) US Medical PG Question 6: A 52-year-old man presents for a routine checkup. Past medical history is remarkable for stage 1 systemic hypertension and hepatitis A infection diagnosed 10 years ago. He takes aspirin, rosuvastatin, enalapril daily, and a magnesium supplement every once in a while. He is planning to visit Ecuador for a week-long vacation and is concerned about malaria prophylaxis before his travel. The physician advised taking 1 primaquine pill every day while he is there and for 7 consecutive days after leaving Ecuador. On the third day of his trip, the patient develops an acute onset headache, dizziness, shortness of breath, and fingertips and toes turning blue. His blood pressure is 135/80 mm Hg, heart rate is 94/min, respiratory rate is 22/min, temperature is 36.9℃ (98.4℉), and blood oxygen saturation is 97% in room air. While drawing blood for his laboratory workup, the nurse notes that his blood has a chocolate brown color. Which of the following statements best describes the etiology of this patient’s most likely condition?
- A. The patient’s condition is due to consumption of water polluted with nitrates.
- B. The patient had pre-existing liver damage caused by viral hepatitis.
- C. This condition resulted from primaquine overdose.
- D. It is a type B adverse drug reaction. (Correct Answer)
- E. The condition developed because of his concomitant use of primaquine and magnesium supplement.
Polyenes (amphotericin formulations) Explanation: ***It is a type B adverse drug reaction.***
- The patient's symptoms (headache, dizziness, shortness of breath, cyanosis, chocolate brown blood) are consistent with **methemoglobinemia**, which is a known idiosyncratic reaction to **primaquine**. Type B adverse drug reactions are **unpredictable** and not dose-dependent, representing an individual's unique response to a drug.
- This reaction likely stems from an underlying **glucose-6-phosphate dehydrogenase (G6PD) deficiency**, making him susceptible to oxidative stress induced by primaquine, leading to methemoglobin formation. The occurrence of symptoms early in the course of medication (3rd day) also supports an idiosyncratic reaction rather than a typical dose-related effect.
*The patient’s condition is due to consumption of water polluted with nitrates.*
- While **nitrate poisoning** can cause methemoglobinemia, the patient’s symptoms appeared shortly after starting primaquine for malaria prophylaxis, making drug-induced methemoglobinemia a more direct and probable cause in this clinical context.
- Exposure to nitrate-polluted water is unlikely to cause a sudden onset of such severe symptoms within 3 days of arrival, especially considering he is taking a known oxidizing agent (primaquine).
*The patient had pre-existing liver damage caused by viral hepatitis.*
- Although **liver dysfunction** can alter drug metabolism, hepatitis A is an acute infection that does not typically cause chronic liver damage leading to altered drug metabolism for primaquine in the long term, especially 10 years after diagnosis.
- The primary risk factor for primaquine-induced methemoglobinemia is G6PD deficiency, not liver damage, which affects red blood cell susceptibility to oxidative stress.
*This condition resulted from primaquine overdose.*
- The prescribed dose of primaquine (one pill daily) is standard for malaria prophylaxis, and there is no indication the patient took more than prescribed. This reaction is likely due to an **idiosyncratic response** rather than an excessive dose.
- Methemoglobinemia from primaquine is often seen in individuals with **G6PD deficiency** even at therapeutic doses, making it an unpredictable Type B adverse reaction rather than a direct dose-dependent toxicity.
*The condition developed because of his concomitant use of primaquine and magnesium supplement.*
- There is no known direct significant **drug interaction** between primaquine and magnesium supplements that would lead to methemoglobinemia.
- The underlying cause of methemoglobinemia with primaquine is typically due to its **oxidative properties** in susceptible individuals (e.g., G6PD deficiency), not an interaction with magnesium.
Polyenes (amphotericin formulations) US Medical PG Question 7: An 82-year-old male with a history of congestive heart failure presented with new-onset atrial fibrillation. He was initially started on carvedilol, but he now requires an additional agent for rate control. He is started on a medicine and is warned by his physician of the following potential side effects associated with this therapy: nausea, vomiting, confusion, blurry yellow vision, electrolyte abnormalities, and potentially fatal arrhythmia. Which of the following is most likely to increase this patient's susceptibility to the toxic effects associated with this medication?
- A. Hyperkalemia
- B. Elevated AST and ALT
- C. Increased GFR with normal creatinine
- D. Hypokalemia (Correct Answer)
- E. Hyponatremia
Polyenes (amphotericin formulations) Explanation: ***Hypokalemia***
- The symptoms described (nausea, vomiting, confusion, blurry yellow vision, potentially fatal arrhythmias) are classic for **digoxin toxicity**.
- **Hypokalemia** increases the binding of digoxin to the **Na+/K+-ATPase pump**, exacerbating its effects and increasing the risk of toxicity.
*Hyperkalemia*
- **Hyperkalemia** actually **inhibits** digoxin binding to the Na+/K+-ATPase pump.
- This can reduce the therapeutic efficacy and the toxic effects of digoxin.
*Elevated AST and ALT*
- Elevated AST and ALT indicate **liver dysfunction**, which can affect the metabolism of certain drugs.
- However, digoxin is primarily eliminated by the **kidneys**, so liver enzyme abnormalities are not a primary risk factor for digoxin toxicity.
*Increased GFR with normal creatinine*
- An increased **Glomerular Filtration Rate (GFR)** would lead to more rapid renal clearance of digoxin.
- This would **decrease** the risk of digoxin accumulation and toxicity, rather than increase it.
*Hyponatremia*
- While electrolyte imbalances can be associated with cardiac conditions, **hyponatremia** itself does not directly increase the susceptibility to digoxin toxicity.
- The most critical electrolyte imbalance for digoxin toxicity is **hypokalemia**.
Polyenes (amphotericin formulations) US Medical PG Question 8: A person presents to the hospital with fever and chills. Fever profile is ordered and is found to be negative for malaria and dengue. Rk39 test is found to be positive. What is the treatment of choice?
- A. Amphotericin B (Correct Answer)
- B. Dapsone
- C. Hydroxychloroquine
- D. Griseofulvin
Polyenes (amphotericin formulations) Explanation: Amphotericin B
- A positive RK39 test suggests visceral leishmaniasis (kala-azar), especially with fever and chills in an endemic area [1].
- Amphotericin B (specifically liposomal Amphotericin B) is a highly effective and often the drug of choice for treating visceral leishmaniasis, particularly in severe cases or regions with antimonial resistance.
Dapsone
- Dapsone is primarily used in the treatment of leprosy and بعض forms of dermatitis (e.g., dermatitis herpetiformis).
- It has no significant role in treating leishmaniasis.
Hydroxychloroquine
- Hydroxychloroquine is an antimalarial drug also used for certain autoimmune diseases like lupus and rheumatoid arthritis [2].
- It is ineffective against leishmaniasis.
Griseofulvin
- Griseofulvin is an antifungal medication used to treat dermatophyte infections (e.g., ringworm of the skin, hair, or nails).
- It has no activity against Leishmania parasites.
Polyenes (amphotericin formulations) US Medical PG Question 9: A 46-year-old man with HIV infection comes to the physician because of a 1-week history of severe retrosternal pain while swallowing. He has not been compliant with his antiretroviral drug regimen. His CD4+ T-lymphocyte count is 98/mm3 (N ≥ 500). Endoscopy shows white plaques in the esophagus. The most appropriate immediate treatment is a drug that inhibits which of the following enzymes?
- A. DNA polymerase
- B. Hydrogen-potassium ATPase
- C. Cytochrome p450 enzymes (Correct Answer)
- D. Phospholipase A2
- E. Squalene epoxidase
Polyenes (amphotericin formulations) Explanation: ***Cytochrome P450 enzymes***
- The patient's symptoms (retrosternal pain on swallowing, white plaques on endoscopy) and severely low **CD4+ count (98/mm³)** are highly suggestive of **esophageal candidiasis**, a common opportunistic infection in AIDS.
- **Fluconazole**, an azole antifungal, is the **first-line treatment** for esophageal candidiasis and works by inhibiting **14α-demethylase (lanosterol demethylase)**, a fungal **cytochrome P450 enzyme**.
- This inhibition prevents the conversion of lanosterol to ergosterol, disrupting **fungal cell membrane synthesis** and leading to fungal cell death.
*Squalene epoxidase*
- **Terbinafine** and **naftifine** (allylamine antifungals) inhibit squalene epoxidase in the ergosterol synthesis pathway.
- These agents are primarily used for **dermatophyte infections** (onychomycosis, tinea) and have **poor activity against Candida species**.
- They are not appropriate for treating esophageal candidiasis.
*DNA polymerase*
- Inhibitors of **DNA polymerase**, such as acyclovir or ganciclovir, are used to treat **herpesvirus infections** (HSV, CMV).
- While herpes esophagitis can occur in immunocompromised patients, it typically presents with **punched-out ulcers**, not white plaques.
*Hydrogen-potassium ATPase*
- **Proton pump inhibitors** (PPIs) target hydrogen-potassium ATPase in gastric parietal cells to reduce **acid secretion**.
- These are used to treat **GERD** or **peptic ulcers**, which do not present with white plaques on endoscopy.
- While PPIs may provide symptomatic relief, they do not treat the underlying fungal infection.
*Phospholipase A2*
- Phospholipase A2 inhibitors are used as **anti-inflammatory agents**, as PLA2 releases arachidonic acid, a precursor to inflammatory mediators.
- These drugs have no role in treating fungal infections like esophageal candidiasis.
Polyenes (amphotericin formulations) US Medical PG Question 10: A 41-year-old man comes to the physician because of a 3-week history of fatigue, cough, and a 4.5-kg (10-lb) weight loss. He does not smoke or drink alcohol. He appears emaciated. A chest x-ray shows a calcified nodule in the left lower lobe and left hilar lymphadenopathy. The physician initiates therapy for the condition and informs him that he will have to return for monthly ophthalmologic examination for the next 2 months. These examinations are most likely to evaluate the patient for an adverse effect of a drug with which of the following mechanisms of action?
- A. Impaired synthesis of mycolic acids
- B. Impaired protein synthesis due to binding to 50S ribosomes
- C. Impaired production of hemozoin from heme
- D. Impaired synthesis of cell wall polysaccharides (Correct Answer)
- E. Impaired protein synthesis due to binding to 30S ribosomes
Polyenes (amphotericin formulations) Explanation: ***Impaired synthesis of cell wall polysaccharides***
- The patient's clinical presentation (fatigue, cough, weight loss, calcified nodule, hilar lymphadenopathy) is classic for **tuberculosis**.
- The requirement for **monthly ophthalmologic examinations** is pathognomonic for **ethambutol** therapy, as this drug causes **optic neuritis** (decreased visual acuity, red-green color blindness).
- **Ethambutol** inhibits **arabinosyl transferase**, which impairs the synthesis of **arabinogalactan**, a key polysaccharide component of the mycobacterial cell wall.
- Due to the risk of optic neuritis, patients on ethambutol require baseline and monthly ophthalmologic monitoring, especially during the first 2 months of therapy.
*Impaired synthesis of mycolic acids*
- This describes the mechanism of **isoniazid (INH)**, a first-line anti-TB drug that inhibits mycolic acid synthesis.
- The main adverse effects of isoniazid are **peripheral neuropathy** (prevented with pyridoxine/vitamin B6) and **hepatotoxicity**, not optic neuritis.
- Isoniazid does not require routine ophthalmologic monitoring.
*Impaired protein synthesis due to binding to 50S ribosomes*
- This mechanism describes **macrolides** (e.g., clarithromycin, azithromycin) and **chloramphenicol**.
- While macrolides may be used for atypical mycobacterial infections, they are not first-line TB therapy and do not cause optic neuritis requiring monthly eye exams.
*Impaired protein synthesis due to binding to 30S ribosomes*
- This mechanism describes **aminoglycosides** (e.g., streptomycin) and **tetracyclines**.
- While streptomycin is a second-line anti-TB drug, its main adverse effects are **ototoxicity** (hearing loss, vestibular dysfunction) and **nephrotoxicity**, not optic neuritis.
- These drugs do not require ophthalmologic monitoring.
*Impaired production of hemozoin from heme*
- This is the mechanism of **chloroquine** and **hydroxychloroquine**, which are antimalarial drugs.
- While chloroquine can cause retinopathy requiring ophthalmologic monitoring, this patient has **tuberculosis**, not malaria.
- The clinical scenario (calcified lung nodule, hilar lymphadenopathy) and TB treatment context make this mechanism incorrect for this case.
More Polyenes (amphotericin formulations) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.