Echinocandins US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Echinocandins. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Echinocandins US Medical PG Question 1: A 45-year-old HIV-positive male presents to his primary care physician complaining of decreased libido. He reports that he has been unable to maintain an erection for the past two weeks. He has never encountered this problem before. He was hospitalized four weeks ago for cryptococcal meningitis and has been on long-term antifungal therapy since then. His CD4 count is 400 cells/mm^3 and viral load is 5,000 copies/ml. He was previously non-compliant with HAART but since his recent infection, he has been more consistent with its use. His past medical history is also notable for hypertension, major depressive disorder, and alcohol abuse. He takes lisinopril and sertraline. His temperature is 98.6°F (37°C), blood pressure is 120/85 mmHg, pulse is 80/min, and respirations are 18/min. The physician advises the patient that side effects like decreased libido may manifest due to a drug with which of the following mechanisms of action?
- A. Inhibition of beta-glucan synthesis
- B. Formation of pores in cell membrane
- C. Inhibition of ergosterol synthesis (Correct Answer)
- D. Disruption of microtubule formation
- E. Inhibition of pyrimidine synthesis
Echinocandins Explanation: ***Inhibition of ergosterol synthesis***
- The patient was recently treated for **cryptococcal meningitis** and is likely on an **azole antifungal**, such as fluconazole or itraconazole, for long-term therapy.
- Azole antifungals inhibit **14-alpha-demethylase**, an enzyme crucial for **ergosterol synthesis**, and are known to cause endocrine side effects like **decreased libido** and **erectile dysfunction** due to their impact on steroid hormone synthesis.
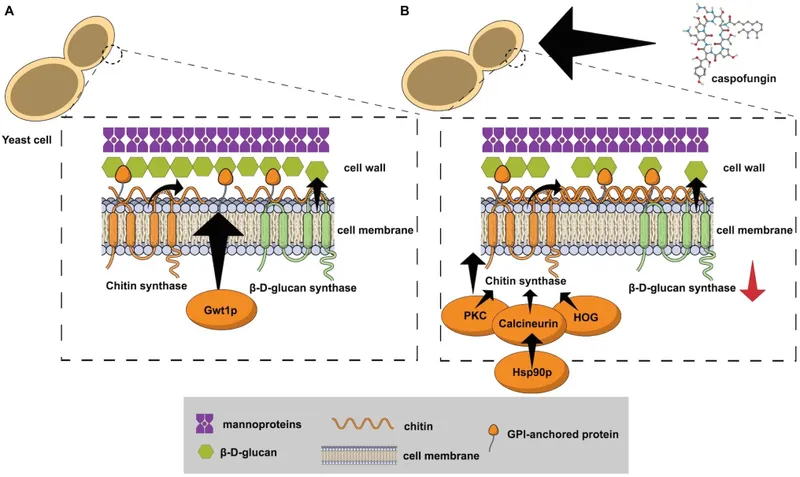
*Inhibition of beta-glucan synthesis*
- This mechanism of action belongs to **echinocandins** (e.g., caspofungin, micafungin), which inhibit the synthesis of **1,3-beta-D-glucan**, a key component of the fungal cell wall.
- Echinocandins are typically used for *Candida* infections and are generally not associated with significant endocrine side effects like decreased libido or erectile dysfunction.
*Formation of pores in cell membrane*
- This is the mechanism of action for **polyene antifungals** like **amphotericin B** and **nystatin**, which bind to ergosterol in the fungal cell membrane, creating pores and leading to cell lysis.
- While effective against *Cryptococcus*, amphotericin B is primarily used for acute, severe infections due to its significant toxicity, including nephrotoxicity, and is not typically used for long-term maintenance in this context with libido as the main symptom.
*Disruption of microtubule formation*
- This mechanism is characteristic of **griseofulvin**, an antifungal primarily used for dermatophyte infections of the skin and nails.
- It interferes with **microtubule function** and inhibits fungal mitosis, but it is not used for systemic fungal infections like cryptococcal meningitis, nor is it commonly associated with decreased libido.
*Inhibition of pyrimidine synthesis*
- This mechanism belongs to **flucytosine**, which is converted to **5-fluorouracil** within fungal cells, inhibiting DNA and RNA synthesis.
- Flucytosine is typically used in combination with amphotericin B for severe cryptococcal infections, but it is not known to cause decreased libido as a common or prominent side effect.
Echinocandins US Medical PG Question 2: A 64-year-old female with type 2 diabetes mellitus comes to the physician because of a 1-week history of painful red swelling on her left thigh. Examination shows a 3- x 4-cm, tender, fluctuant mass. Incision and drainage of the abscess are performed. Culture of the abscess fluid grows gram-positive, coagulase-positive cocci that are resistant to oxacillin. Which of the following best describes the mechanism of resistance of the causal organism to oxacillin?
- A. Degradation of the antibiotic
- B. Decreased uptake of the antibiotic
- C. Decreased activation of the antibiotic
- D. Altered target of the antibiotic (Correct Answer)
- E. Acetylation of the antibiotic
Echinocandins Explanation: ***Altered target of the antibiotic***
- The organism described (gram-positive, coagulase-positive cocci, oxacillin-resistant) is **methicillin-resistant *Staphylococcus aureus* (MRSA)**.
- MRSA achieves oxacillin (and other beta-lactam) resistance by acquiring the ***mecA* gene**, which encodes for a **modified penicillin-binding protein (PBP2a)** with reduced affinity for beta-lactam antibiotics.
*Degradation of the antibiotic*
- This mechanism, primarily through the production of **beta-lactamase enzymes**, can degrade beta-lactam antibiotics.
- While *Staphylococcus aureus* can produce beta-lactamases, oxacillin (a **penicillinase-resistant penicillin**) is specifically engineered to be stable against these enzymes.
*Decreased uptake of the antibiotic*
- Reduced permeability of the bacterial cell wall can lead to decreased uptake, a mechanism more commonly associated with **gram-negative bacteria** due to their outer membrane.
- This is not the primary mechanism of resistance for MRSA to oxacillin.
*Decreased activation of the antibiotic*
- Some antibiotics are prodrugs that require activation by bacterial enzymes, and resistance can arise from mutations affecting this activation.
- Oxacillin is active in its administered form and does not require bacterial activation.
*Acetylation of the antibiotic*
- **Enzymatic modification**, such as acetylation, adenylylation, or phosphorylation, is a common mechanism of resistance, particularly against **aminoglycoside antibiotics**.
- This specific mechanism is not responsible for oxacillin resistance in MRSA.
Echinocandins US Medical PG Question 3: A 74-year-old man is admitted to the medical ward after he developed a fungal infection. He has aplastic anemia. The most recent absolute neutrophil count was 450/µL. An anti-fungal agent is administered that inhibits the fungal enzyme, (1→3)-β-D-glucan synthase, and thereby disrupts the integrity of the fungal cell wall. He responds well to the treatment. Although amphotericin B is more efficacious for his condition, it was not used because of the side effect profile. What was the most likely infection?
- A. Invasive aspergillosis
- B. Mucormycosis
- C. Histoplasmosis
- D. Paracoccidioidomycosis
- E. Candidemia (Correct Answer)
Echinocandins Explanation: ***Candidemia***
- The patient's **neutropenia** (absolute neutrophil count of 450/µL) due to aplastic anemia is a major risk factor for invasive candidiasis, including candidemia.
- The antifungal agent's mechanism of action, targeting **(1→3)-β-D-glucan synthase**, is characteristic of **echinocandins**, which are first-line agents for candidemia, especially in critically ill or neutropenic patients, and often preferred over amphotericin B due to a better side effect profile.
*Invasive aspergillosis*
- While neutropenia is a significant risk factor for invasive aspergillosis, the primary antifungal drugs for this condition are typically **voriconazole** or **isavuconazole**, although echinocandins may be used as salvage therapy or in combination.
- The description of the drug's mechanism specifically targeting **(1→3)-β-D-glucan synthase** does not make aspergillosis the *most likely* infection, as some Aspergillus species may have less β-D-glucan in their cell walls compared to *Candida*.
*Mucormycosis*
- This aggressive fungal infection is often seen in immunocompromised patients, particularly those with **diabetes** or profound neutropenia, but the primary treatment is usually **amphotericin B**.
- Mucorales fungi typically **lack ergosterol** and their cell walls do not contain **(1→3)-β-D-glucan**, making echinocandins ineffective.
*Histoplasmosis*
- This is a dimorphic fungal infection endemic to certain geographic regions, primarily affecting the lungs and disseminating in immunocompromised individuals.
- The drug of choice for severe or disseminated histoplasmosis is **amphotericin B**, followed by azoles; echinocandins are generally not active against *Histoplasma*.
*Paracoccidioidomycosis*
- This is a chronic systemic mycosis found in Latin America, primarily affecting the lungs, skin, and lymph nodes.
- Treatment for severe forms typically involves **amphotericin B**, followed by sulfonamides or azoles for maintenance; echinocandins are not effective against *Paracoccidioides*.
Echinocandins US Medical PG Question 4: A 26-year-old man comes to the emergency department because of a 1-week history of worsening fatigue, nausea, and vomiting. Six weeks ago, he was diagnosed with latent tuberculosis and appropriate low-dose pharmacotherapy was initiated. Physical examination shows right upper quadrant tenderness and scleral icterus. Laboratory studies show elevated aminotransferases. Impaired function of which of the following pharmacokinetic processes is the most likely explanation for this patient's symptoms?
- A. Acetylation (Correct Answer)
- B. Glucuronidation
- C. Hydrolysis
- D. Sulfation
- E. Reduction
Echinocandins Explanation: ***Acetylation***
- This patient is exhibiting symptoms of **hepatotoxicity** (fatigue, nausea, vomiting, RUQ tenderness, scleral icterus, elevated aminotransferases) after starting low-dose pharmacotherapy for latent tuberculosis. The most common drug used for latent TB is **isoniazid**, which is primarily metabolized by **N-acetylation**.
- Impaired acetylation, particularly in **slow acetylators**, can lead to higher plasma concentrations of isoniazid and its toxic metabolites, increasing the risk of **drug-induced liver injury**.
*Glucuronidation*
- **Glucuronidation** is a Phase II metabolic pathway that conjugates drugs with **glucuronic acid** to increase water solubility and facilitate excretion.
- While important for the metabolism of many drugs and endogenous substances (e.g., bilirubin), it is not the primary mechanism of metabolism or the main pathway implicated in the hepatotoxicity of **isoniazid**.
*Hydrolysis*
- **Hydrolysis** is a chemical reaction in which water is used to break down a compound, often involving ester or amide bonds.
- This process is not the primary metabolic pathway for **isoniazid**, nor is impaired hydrolysis a common cause of its hepatotoxicity.
*Sulfation*
- **Sulfation** is a Phase II metabolic reaction that conjugates drugs with a **sulfate group**, typically for detoxification and excretion.
- While various drugs undergo sulfation, it is not the dominant metabolic pathway for **isoniazid**, and impaired sulfation is not typically associated with isoniazid-induced hepatotoxicity.
*Reduction*
- **Reduction** reactions involve the gain of electrons or hydrogen atoms, or the loss of oxygen, and are part of drug metabolism for certain compounds.
- However, reduction is not the primary clearance mechanism for **isoniazid**, and abnormal reduction is not commonly implicated in its hepatotoxic effects.
Echinocandins US Medical PG Question 5: A 32-year-old woman presents with three-days of vaginal burning, itching, and pain with intercourse. She is in a monogamous relationship with her husband and has an intrauterine device for contraception. Her past medical history is unremarkable, except for recently being treated with antibiotics for sinusitis. Pelvic exam is remarkable for vulvar excoriations, vaginal wall edema, and thick, white discharge in the vault. Wet mount with KOH staining reveals budding filaments with pseudohyphae and hyphae. Which of the following is the most appropriate treatment?
- A. Voriconazole
- B. Posaconazole
- C. Metronidazole
- D. Itraconazole
- E. Fluconazole (Correct Answer)
Echinocandins Explanation: ***Fluconazole***
- The patient's symptoms (vaginal burning, itching, pain with intercourse, thick, white discharge) and **wet mount findings (budding filaments with pseudohyphae and hyphae)** are classic for **vulvovaginal candidiasis (VVC)**, often precipitated by recent antibiotic use.
- **Fluconazole** is a highly effective and commonly prescribed oral antifungal for uncomplicated VVC due to its convenience and excellent therapeutic profile.
*Voriconazole*
- **Voriconazole** is a broad-spectrum triazole antifungal primarily used for invasive fungal infections, such as **invasive aspergillosis** and candidemia, and is not a first-line treatment for uncomplicated VVC.
- Its use is typically reserved for more severe or refractory systemic fungal infections, and it has a more significant side effect profile than fluconazole.
*Posaconazole*
- **Posaconazole** is another extended-spectrum triazole antifungal primarily used for the prophylaxis and treatment of **invasive fungal infections** in immunocompromised patients, particularly those unresponsive to other antifungals.
- It is not indicated for the treatment of uncomplicated vulvovaginal candidiasis.
*Metronidazole*
- **Metronidazole** is an antibiotic and antiprotozoal agent used to treat bacterial vaginosis and trichomoniasis, both of which are common causes of vaginitis.
- It is **ineffective against fungal infections**, and the patient's symptoms and wet mount findings rule out bacterial vaginosis and trichomoniasis.
*Itraconazole*
- **Itraconazole** is an antifungal drug effective against superficial and systemic fungal infections, but it is typically used for more severe or recurrent VVC, or in cases of non-albicans Candida species.
- While effective, **fluconazole** is generally preferred as the first-line oral treatment for uncomplicated VVC due to its single-dose efficacy and established safety profile for this indication.
Echinocandins US Medical PG Question 6: A 72-year-old woman with type 2 diabetes mellitus comes to the physician because she is concerned about the appearance of her toenails. Examination shows yellowish discoloration of all toenails on both feet. The edges of the toenails are lifted, and there is subungual debris. Potassium hydroxide preparation of scrapings from the nails shows multiple branching septate hyphae. Treatment with oral terbinafine is begun. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of squalene epoxidase (Correct Answer)
- B. Formation of pores in cell membrane
- C. Inhibition of β-glucan synthesis
- D. Interference with mitosis during metaphase
- E. Prevention of lanosterol to ergosterol conversion
Echinocandins Explanation: ***Inhibition of squalene epoxidase***
- **Terbinafine** is an **allylamine** antifungal that inhibits the enzyme **squalene epoxidase**, an early step in fungal ergosterol synthesis
- This inhibition leads to the accumulation of **squalene**, which is toxic to the fungal cell, and a deficiency of **ergosterol**, disrupting cell membrane integrity and function
- Terbinafine is highly effective for **onychomycosis** (fungal nail infections) caused by dermatophytes
*Formation of pores in cell membrane*
- This mechanism is characteristic of **polyene antifungals** like **amphotericin B** and **nystatin**
- These drugs bind to **ergosterol** in the fungal cell membrane, creating pores that lead to leakage of intracellular contents and cell death
*Inhibition of β-glucan synthesis*
- This is the primary mechanism of action for **echinocandin** antifungals, such as **caspofungin**, **micafungin**, and **anidulafungin**
- These drugs inhibit **(1,3)-β-D-glucan synthase**, which is essential for the synthesis of glucan, a major component of the fungal cell wall
*Interference with mitosis during metaphase*
- This mechanism is characteristic of **griseofulvin**, another antifungal agent used for dermatophyte infections
- **Griseofulvin** interferes with **microtubule function**, disrupting mitotic spindle formation and preventing fungal cell division
*Prevention of lanosterol to ergosterol conversion*
- This mechanism is associated with **azole antifungals** (e.g., fluconazole, itraconazole), which inhibit fungal **cytochrome P450-dependent 14-α-demethylase**
- This enzyme is responsible for the conversion of **lanosterol** to **ergosterol**, leading to ergosterol depletion and accumulation of toxic sterol precursors
Echinocandins US Medical PG Question 7: A potassium hydroxide preparation is conducted on a skin scraping of the hypopigmented area. Microscopy of the preparation shows long hyphae among clusters of yeast cells. Based on these findings, which of the following is the most appropriate pharmacotherapy?
- A. Topical corticosteroid
- B. Oral ketoconazole
- C. Topical selenium sulfide (Correct Answer)
- D. Topical nystatin
- E. Oral fluconazole
Echinocandins Explanation: ***Topical selenium sulfide***
- The presence of **long hyphae** and **clusters of yeast cells** on KOH prep is characteristic of **tinea versicolor**, caused by *Malassezia furfur*.
- **Selenium sulfide** is a common and effective topical antifungal agent for tinea versicolor, available in shampoos and lotions.
*Topical corticosteroid*
- **Corticosteroids** have anti-inflammatory properties but do not treat fungal infections.
- Using corticosteroids alone would only mask symptoms and could potentially worsen the fungal infection.
*Oral ketoconazole*
- While **oral ketoconazole** is an antifungal, it is generally reserved for extensive or recalcitrant cases of tinea versicolor due to potential systemic side effects, such as **hepatotoxicity**.
- **Topical treatments** are preferred as first-line therapy for localized infections like this one.
*Topical nystatin*
- **Nystatin** is an antifungal agent primarily effective against *Candida* species.
- It is **not effective** against *Malassezia furfur*, the causative agent of tinea versicolor.
*Oral fluconazole*
- **Oral fluconazole** is an effective systemic antifungal used for various *Candida* and dermatophyte infections.
- Similar to oral ketoconazole, it is typically reserved for **widespread or recalcitrant cases** of tinea versicolor, with topical therapy being the preferred initial approach.
Echinocandins US Medical PG Question 8: A patient is receiving daily administrations of Compound X. Compound X is freely filtered in the glomeruli and undergoes net secretion in the renal tubules. The majority of this tubular secretion occurs in the proximal tubule. Additional information regarding this patient's renal function and the renal processing of Compound X is included below:
Inulin clearance: 120 mL/min
Plasma concentration of Inulin: 1 mg/mL
PAH clearance: 600 mL/min
Plasma concentration of PAH: 0.2 mg/mL
Total Tubular Secretion of Compound X: 60 mg/min
Net Renal Excretion of Compound X: 300 mg/min
Which of the following is the best estimate of the plasma concentration of Compound X in this patient?
- A. 2 mg/mL (Correct Answer)
- B. 3 mg/mL
- C. There is insufficient information available to estimate the plasma concentration of Compound X
- D. 1 mg/mL
- E. 0.5 mg/mL
Echinocandins Explanation: ***2 mg/mL***
* The **net renal excretion of Compound X (300 mg/min)** is the sum of the filtered load and the net tubular secretion.
* Given that Compound X is **freely filtered** and undergoes **net secretion (60 mg/min)**, we can calculate the filtered load and subsequently its plasma concentration.
* **Net excretion = Filtered load + Net tubular secretion**
* **300 mg/min = Filtered load + 60 mg/min**
* **Filtered load = 300 mg/min - 60 mg/min = 240 mg/min**
* Since **Filtered load = Glomerular Filtration Rate (GFR) * Plasma concentration (P_X)**, and GFR is estimated by **inulin clearance (120 mL/min)**:
* **240 mg/min = 120 mL/min * P_X**
* **P_X = 240 mg/min / 120 mL/min = 2 mg/mL**.
*3 mg/mL*
* This value would imply a significantly higher filtered load or a different contribution from tubular secretion.
* Calculations using this plasma concentration would not align with the provided excretion and secretion rates.
*There is insufficient information available to estimate the plasma concentration of Compound X*
* The problem provides all necessary values: **Inulin clearance (GFR)**, **net tubular secretion of Compound X**, and **net renal excretion of Compound X**.
* These parameters are sufficient to determine the filtered load and thus the plasma concentration of Compound X.
*1 mg/mL*
* A plasma concentration of 1 mg/mL would result in a lower filtered load than calculated and would not account for the observed net renal excretion.
* **Filtered load = 120 mL/min * 1 mg/mL = 120 mg/min**. Total excretion would then be 120 mg/min + 60 mg/min = 180 mg/min, which contradicts the given 300 mg/min.
*0.5 mg/mL*
* This plasma concentration would lead to an even lower filtered load, making it impossible to achieve the *net renal excretion of Compound X* given the tubular secretion.
* **Filtered load = 120 mL/min * 0.5 mg/mL = 60 mg/min**. Total excretion would be 60 mg/min + 60 mg/min = 120 mg/min, which is much lower than the given 300 mg/min.
Echinocandins US Medical PG Question 9: A 46-year-old man with HIV infection comes to the physician because of a 1-week history of severe retrosternal pain while swallowing. He has not been compliant with his antiretroviral drug regimen. His CD4+ T-lymphocyte count is 98/mm3 (N ≥ 500). Endoscopy shows white plaques in the esophagus. The most appropriate immediate treatment is a drug that inhibits which of the following enzymes?
- A. DNA polymerase
- B. Hydrogen-potassium ATPase
- C. Cytochrome p450 enzymes (Correct Answer)
- D. Phospholipase A2
- E. Squalene epoxidase
Echinocandins Explanation: ***Cytochrome P450 enzymes***
- The patient's symptoms (retrosternal pain on swallowing, white plaques on endoscopy) and severely low **CD4+ count (98/mm³)** are highly suggestive of **esophageal candidiasis**, a common opportunistic infection in AIDS.
- **Fluconazole**, an azole antifungal, is the **first-line treatment** for esophageal candidiasis and works by inhibiting **14α-demethylase (lanosterol demethylase)**, a fungal **cytochrome P450 enzyme**.
- This inhibition prevents the conversion of lanosterol to ergosterol, disrupting **fungal cell membrane synthesis** and leading to fungal cell death.
*Squalene epoxidase*
- **Terbinafine** and **naftifine** (allylamine antifungals) inhibit squalene epoxidase in the ergosterol synthesis pathway.
- These agents are primarily used for **dermatophyte infections** (onychomycosis, tinea) and have **poor activity against Candida species**.
- They are not appropriate for treating esophageal candidiasis.
*DNA polymerase*
- Inhibitors of **DNA polymerase**, such as acyclovir or ganciclovir, are used to treat **herpesvirus infections** (HSV, CMV).
- While herpes esophagitis can occur in immunocompromised patients, it typically presents with **punched-out ulcers**, not white plaques.
*Hydrogen-potassium ATPase*
- **Proton pump inhibitors** (PPIs) target hydrogen-potassium ATPase in gastric parietal cells to reduce **acid secretion**.
- These are used to treat **GERD** or **peptic ulcers**, which do not present with white plaques on endoscopy.
- While PPIs may provide symptomatic relief, they do not treat the underlying fungal infection.
*Phospholipase A2*
- Phospholipase A2 inhibitors are used as **anti-inflammatory agents**, as PLA2 releases arachidonic acid, a precursor to inflammatory mediators.
- These drugs have no role in treating fungal infections like esophageal candidiasis.
Echinocandins US Medical PG Question 10: A 64-year-old woman presents to the clinic with a history of 3 fractures in the past year with the last one being last month. Her bone-density screening from last year reported a T-score of -3.1 and she was diagnosed with osteoporosis. She was advised to quit smoking and was asked to adapt to a healthy lifestyle to which she complied. She was also given calcium and vitamin D supplements. After a detailed discussion with the patient, the physician decides to start her on weekly alendronate. Which of the following statements best describes this patient’s new therapy?
- A. It should be stopped after 10 years due to the risk of esophageal cancer
- B. It is typically used as a second-line therapy for her condition after raloxifene
- C. It can cause hot flashes, flu-like symptoms, and peripheral edema
- D. It must be taken with the first meal of the day due to the significant risk of GI upset
- E. The patient must stay upright for at least 30 minutes after taking this medication (Correct Answer)
Echinocandins Explanation: ***The patient must stay upright for at least 30 minutes after taking this medication***
- This instruction is crucial for **alendronate** (a bisphosphonate) to prevent **esophageal irritation** and potential esophagitis or ulcers.
- Alendronate must be taken with a full glass of plain water on an **empty stomach** at least 30-60 minutes before the first food, beverage, or other medication of the day, and the patient must remain upright.
*It should be stopped after 10 years due to the risk of esophageal cancer*
- The main concern with long-term bisphosphonate use (usually >5 years for oral agents) is the risk of **atypical femoral fractures** and **osteonecrosis of the jaw**, not esophageal cancer.
- While esophageal irritation is a known side effect, the risk of esophageal cancer is **not the primary reason** for treatment discontinuation after 10 years.
*It is typically used as a second-line therapy for her condition after raloxifene*
- **Alendronate** (an oral bisphosphonate) is considered a **first-line therapy** for postmenopausal osteoporosis, especially in patients with a history of fractures and low T-scores.
- **Raloxifene** is a selective estrogen receptor modulator (SERM) typically used when bisphosphonates are contraindicated or not tolerated, or there is a need to also treat breast cancer risk, and it is **less potent** in reducing non-vertebral fractures.
*It can cause hot flashes, flu-like symptoms, and peripheral edema*
- These side effects (hot flashes, flu-like symptoms, peripheral edema) are **not typically associated** with alendronate.
- **Hot flashes** are more common with estrogen-modulating drugs like raloxifene, while **flu-like symptoms** can occur with IV bisphosphonates (like zoledronic acid) or certain anabolic agents.
*It must be taken with the first meal of the day due to the significant risk of GI upset*
- This statement is incorrect; alendronate must be taken on an **empty stomach** (at least 30-60 minutes before the first food or drink) to ensure adequate absorption.
- Taking it with food or other beverages significantly **reduces its absorption**, making it less effective, and the risk of GI upset (specifically esophageal irritation) is why remaining upright and taking with water are stressed.
More Echinocandins US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.