Antifungal prophylaxis protocols US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antifungal prophylaxis protocols. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antifungal prophylaxis protocols US Medical PG Question 1: A 26-year-old man comes to the physician for a follow-up examination. He was diagnosed with HIV infection 2 weeks ago. His CD4+ T-lymphocyte count is 162/mm3 (N ≥ 500). An interferon-gamma release assay is negative. Prophylactic treatment against which of the following pathogens is most appropriate at this time?
- A. Cytomegalovirus
- B. Toxoplasma gondii
- C. Mycobacterium tuberculosis
- D. Aspergillus fumigatus
- E. Pneumocystis jirovecii (Correct Answer)
Antifungal prophylaxis protocols Explanation: ***Pneumocystis jirovecii***
- This patient's **CD4+ T-lymphocyte count of 162/mm3** is below the threshold of 200/mm3, indicating a significant risk for **Pneumocystis pneumonia (PCP)**, an opportunistic infection in HIV.
- Prophylaxis with **trimethoprim-sulfamethoxazole (TMP-SMX)** is highly effective and recommended for HIV patients with CD4 counts less than 200/mm3.
*Cytomegalovirus*
- **CMV prophylaxis** is generally not recommended for all HIV patients, even with low CD4 counts, unless there is evidence of active disease or extremely low CD4 counts (e.g., <50/mm3) with high viral loads.
- While CMV can cause end-organ disease in advanced HIV, routine primary prophylaxis is not standard for this CD4 level.
*Toxoplasma gondii*
- **Toxoplasma prophylaxis** is indicated for HIV patients with **CD4 counts less than 100/mm3** who are also seropositive for *Toxoplasma gondii*.
- The patient's CD4 count is 162/mm3, and there's no mention of *Toxoplasma* serostatus, making it less appropriate than PCP prophylaxis.
*Mycobacterium tuberculosis*
- The patient's **interferon-gamma release assay (IGRA) is negative**, which suggests no **latent tuberculosis infection (LTBI)**, thus making primary prophylaxis unnecessary at this time.
- While HIV patients are at high risk for TB, prophylaxis is typically given for LTBI or as secondary prophylaxis for those who have completed treatment for active TB.
*Aspergillus fumigatus*
- **Aspergillus infections** are typically seen in patients with severe **neutropenia** or those receiving high-dose corticosteroids, not primarily in HIV patients based solely on CD4 count.
- Routine prophylaxis for Aspergillus is not recommended for HIV patients, even with low CD4 counts, unless there is a specific risk factor.
Antifungal prophylaxis protocols US Medical PG Question 2: A 45-year-old HIV-positive male presents to his primary care physician complaining of decreased libido. He reports that he has been unable to maintain an erection for the past two weeks. He has never encountered this problem before. He was hospitalized four weeks ago for cryptococcal meningitis and has been on long-term antifungal therapy since then. His CD4 count is 400 cells/mm^3 and viral load is 5,000 copies/ml. He was previously non-compliant with HAART but since his recent infection, he has been more consistent with its use. His past medical history is also notable for hypertension, major depressive disorder, and alcohol abuse. He takes lisinopril and sertraline. His temperature is 98.6°F (37°C), blood pressure is 120/85 mmHg, pulse is 80/min, and respirations are 18/min. The physician advises the patient that side effects like decreased libido may manifest due to a drug with which of the following mechanisms of action?
- A. Inhibition of beta-glucan synthesis
- B. Formation of pores in cell membrane
- C. Inhibition of ergosterol synthesis (Correct Answer)
- D. Disruption of microtubule formation
- E. Inhibition of pyrimidine synthesis
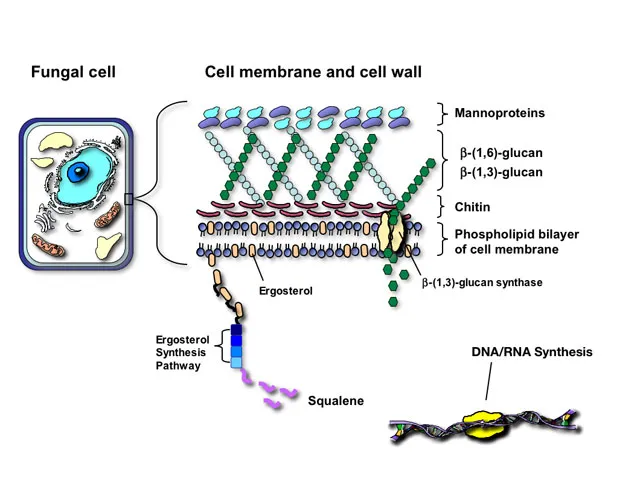
Antifungal prophylaxis protocols Explanation: ***Inhibition of ergosterol synthesis***
- The patient was recently treated for **cryptococcal meningitis** and is likely on an **azole antifungal**, such as fluconazole or itraconazole, for long-term therapy.
- Azole antifungals inhibit **14-alpha-demethylase**, an enzyme crucial for **ergosterol synthesis**, and are known to cause endocrine side effects like **decreased libido** and **erectile dysfunction** due to their impact on steroid hormone synthesis.
*Inhibition of beta-glucan synthesis*
- This mechanism of action belongs to **echinocandins** (e.g., caspofungin, micafungin), which inhibit the synthesis of **1,3-beta-D-glucan**, a key component of the fungal cell wall.
- Echinocandins are typically used for *Candida* infections and are generally not associated with significant endocrine side effects like decreased libido or erectile dysfunction.
*Formation of pores in cell membrane*
- This is the mechanism of action for **polyene antifungals** like **amphotericin B** and **nystatin**, which bind to ergosterol in the fungal cell membrane, creating pores and leading to cell lysis.
- While effective against *Cryptococcus*, amphotericin B is primarily used for acute, severe infections due to its significant toxicity, including nephrotoxicity, and is not typically used for long-term maintenance in this context with libido as the main symptom.
*Disruption of microtubule formation*
- This mechanism is characteristic of **griseofulvin**, an antifungal primarily used for dermatophyte infections of the skin and nails.
- It interferes with **microtubule function** and inhibits fungal mitosis, but it is not used for systemic fungal infections like cryptococcal meningitis, nor is it commonly associated with decreased libido.
*Inhibition of pyrimidine synthesis*
- This mechanism belongs to **flucytosine**, which is converted to **5-fluorouracil** within fungal cells, inhibiting DNA and RNA synthesis.
- Flucytosine is typically used in combination with amphotericin B for severe cryptococcal infections, but it is not known to cause decreased libido as a common or prominent side effect.
Antifungal prophylaxis protocols US Medical PG Question 3: A 69-year-old man with metastatic colon cancer is brought to the emergency department because of shortness of breath, fever, chills, and a productive cough with streaks of blood for the past 5 days. He has a history of emphysema. The patient does not have abdominal pain or headache. He receives chemotherapy with 5-fluorouracil, leucovorin, and oxaliplatin every 6 weeks; his last cycle was 3 weeks ago. His temperature is 38.3°C (101°F), pulse is 112/min, and blood pressure is 100/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 83%. A few scattered inspiratory crackles are heard over the right lung. His mucous membranes are dry. Cardiac examination is normal. Laboratory studies show:
Hemoglobin 9.3 mg/dL
Leukocyte count 700/mm3
Segmented neutrophils 68%
Lymphocytes 25%
Eosinophils 4%
Monocytes 3%
Platelet count 104,000/mm3
Serum
Glucose 75 mg/dL
Urea nitrogen 41 mg/dL
Creatinine 2.1 mg/dL
Galactomannan antigen Positive
Which of the following is the most appropriate initial pharmacotherapy?
- A. Ceftriaxone and azithromycin
- B. Rifampin, isoniazid, pyrazinamide, and ethambutol
- C. Ceftazidime and levofloxacin
- D. Piperacillin-tazobactam
- E. Voriconazole (Correct Answer)
Antifungal prophylaxis protocols Explanation: ***Voriconazole***
- The patient has **neutropenic fever** (leukocyte count 700/mm3, recent chemotherapy) with pulmonary symptoms and a positive **galactomannan antigen**, which is highly suggestive of **invasive aspergillosis**.
- **Voriconazole** is the recommended first-line agent for the treatment of **invasive aspergillosis**.
*Ceftriaxone and azithromycin*
- This combination is typically used for **community-acquired pneumonia**, targeting common bacterial pathogens like *Streptococcus pneumoniae* and atypical bacteria.
- It does not cover **fungal infections** like aspergillosis, nor does it provide broad-spectrum gram-negative coverage suitable for neutropenic fever.
*Rifampin, isoniazid, pyrazinamide, and ethambutol*
- This four-drug regimen is the standard treatment for **active tuberculosis**.
- There is no clinical or laboratory evidence (e.g., acid-fast bacilli smear, cultures) to suggest tuberculosis in this patient.
*Ceftazidime and levofloxacin*
- **Ceftazidime** is a third-generation cephalosporin with good gram-negative coverage, including *Pseudomonas*, which might be considered in neutropenic fever. However, it lacks adequate gram-positive coverage.
- **Levofloxacin** is a fluoroquinolone that provides broad-spectrum coverage, but this combination still misses the likely fungal pathogen and is not ideal for initial empiric therapy in severe neutropenic fever.
*Piperacillin-tazobactam*
- **Piperacillin-tazobactam** is a broad-spectrum antibiotic with good coverage against both gram-positive and gram-negative bacteria, including *Pseudomonas aeruginosa*, making it a common choice for **empiric therapy in neutropenic fever**.
- However, it does not cover **fungal infections**, which are strongly indicated by the positive **galactomannan antigen** in this immunocompromised patient.
Antifungal prophylaxis protocols US Medical PG Question 4: A 67-year-old man is seen on the surgical floor after a transplant procedure. The previous day, the patient had a renal transplant from a matched donor. He is currently recovering and doing well. The patient has a past medical history of IV drug use, diabetes mellitus, oral cold sores, hypertension, renal failure, and dyslipidemia. The patient's current medications include lisinopril, atorvastatin, insulin, and aspirin. Prior to the procedure, he was also on dialysis. The patient is started on cyclosporine. The patient successfully recovers over the next few days. Which of the following medications should be started in this patient?
- A. Azithromycin
- B. TMP-SMX (Correct Answer)
- C. Acyclovir
- D. Low dose acyclovir
- E. Penicillin
Antifungal prophylaxis protocols Explanation: ***TMP-SMX***
- **TMP-SMX (trimethoprim-sulfamethoxazole)** is the **most critical** prophylactic medication for all solid organ transplant recipients on immunosuppression.
- It provides essential prophylaxis against **Pneumocystis jirovecii pneumonia (PJP)**, a life-threatening opportunistic infection with high mortality if not prevented.
- PJP prophylaxis is a **universal recommendation** for all transplant patients and is typically continued for 6-12 months post-transplant.
- Additionally offers protection against **Toxoplasma gondii**, **Nocardia**, and common urinary tract infections, making it particularly valuable in renal transplant recipients.
*Azithromycin*
- Azithromycin is a macrolide antibiotic used for specific bacterial infections and sometimes for **Mycobacterium avium complex (MAC)** prophylaxis in severely immunocompromised patients.
- It is not standard prophylaxis in routine post-transplant care and does not protect against PJP, the most critical opportunistic infection in this setting.
*Acyclovir*
- High-dose acyclovir is used to **treat active HSV or VZV infections**, not for routine prophylaxis.
- This patient has no active viral infection requiring treatment doses at this time.
*Low dose acyclovir*
- Low-dose acyclovir (or valacyclovir) is indeed used for **HSV/VZV prophylaxis** in transplant patients, especially those with a history of cold sores.
- Many transplant centers do initiate this medication alongside TMP-SMX in the post-transplant period.
- However, in a **single-best-answer** context, **TMP-SMX takes priority** as it prevents PJP, which is universally life-threatening and has higher incidence without prophylaxis compared to severe HSV reactivation.
- TMP-SMX is considered the **essential first-line** prophylaxis that all transplant patients must receive.
*Penicillin*
- Penicillin is a narrow-spectrum antibiotic effective against certain gram-positive bacteria.
- It has no role in post-transplant opportunistic infection prophylaxis and does not protect against PJP, HSV, or other transplant-related infections.
Antifungal prophylaxis protocols US Medical PG Question 5: A 74-year-old man is admitted to the medical ward after he developed a fungal infection. He has aplastic anemia. The most recent absolute neutrophil count was 450/µL. An anti-fungal agent is administered that inhibits the fungal enzyme, (1→3)-β-D-glucan synthase, and thereby disrupts the integrity of the fungal cell wall. He responds well to the treatment. Although amphotericin B is more efficacious for his condition, it was not used because of the side effect profile. What was the most likely infection?
- A. Invasive aspergillosis
- B. Mucormycosis
- C. Histoplasmosis
- D. Paracoccidioidomycosis
- E. Candidemia (Correct Answer)
Antifungal prophylaxis protocols Explanation: ***Candidemia***
- The patient's **neutropenia** (absolute neutrophil count of 450/µL) due to aplastic anemia is a major risk factor for invasive candidiasis, including candidemia.
- The antifungal agent's mechanism of action, targeting **(1→3)-β-D-glucan synthase**, is characteristic of **echinocandins**, which are first-line agents for candidemia, especially in critically ill or neutropenic patients, and often preferred over amphotericin B due to a better side effect profile.
*Invasive aspergillosis*
- While neutropenia is a significant risk factor for invasive aspergillosis, the primary antifungal drugs for this condition are typically **voriconazole** or **isavuconazole**, although echinocandins may be used as salvage therapy or in combination.
- The description of the drug's mechanism specifically targeting **(1→3)-β-D-glucan synthase** does not make aspergillosis the *most likely* infection, as some Aspergillus species may have less β-D-glucan in their cell walls compared to *Candida*.
*Mucormycosis*
- This aggressive fungal infection is often seen in immunocompromised patients, particularly those with **diabetes** or profound neutropenia, but the primary treatment is usually **amphotericin B**.
- Mucorales fungi typically **lack ergosterol** and their cell walls do not contain **(1→3)-β-D-glucan**, making echinocandins ineffective.
*Histoplasmosis*
- This is a dimorphic fungal infection endemic to certain geographic regions, primarily affecting the lungs and disseminating in immunocompromised individuals.
- The drug of choice for severe or disseminated histoplasmosis is **amphotericin B**, followed by azoles; echinocandins are generally not active against *Histoplasma*.
*Paracoccidioidomycosis*
- This is a chronic systemic mycosis found in Latin America, primarily affecting the lungs, skin, and lymph nodes.
- Treatment for severe forms typically involves **amphotericin B**, followed by sulfonamides or azoles for maintenance; echinocandins are not effective against *Paracoccidioides*.
Antifungal prophylaxis protocols US Medical PG Question 6: A 72-year-old woman with type 2 diabetes mellitus comes to the physician because she is concerned about the appearance of her toenails. Examination shows yellowish discoloration of all toenails on both feet. The edges of the toenails are lifted, and there is subungual debris. Potassium hydroxide preparation of scrapings from the nails shows multiple branching septate hyphae. Treatment with oral terbinafine is begun. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of squalene epoxidase (Correct Answer)
- B. Formation of pores in cell membrane
- C. Inhibition of β-glucan synthesis
- D. Interference with mitosis during metaphase
- E. Prevention of lanosterol to ergosterol conversion
Antifungal prophylaxis protocols Explanation: ***Inhibition of squalene epoxidase***
- **Terbinafine** is an **allylamine** antifungal that inhibits the enzyme **squalene epoxidase**, an early step in fungal ergosterol synthesis
- This inhibition leads to the accumulation of **squalene**, which is toxic to the fungal cell, and a deficiency of **ergosterol**, disrupting cell membrane integrity and function
- Terbinafine is highly effective for **onychomycosis** (fungal nail infections) caused by dermatophytes
*Formation of pores in cell membrane*
- This mechanism is characteristic of **polyene antifungals** like **amphotericin B** and **nystatin**
- These drugs bind to **ergosterol** in the fungal cell membrane, creating pores that lead to leakage of intracellular contents and cell death
*Inhibition of β-glucan synthesis*
- This is the primary mechanism of action for **echinocandin** antifungals, such as **caspofungin**, **micafungin**, and **anidulafungin**
- These drugs inhibit **(1,3)-β-D-glucan synthase**, which is essential for the synthesis of glucan, a major component of the fungal cell wall
*Interference with mitosis during metaphase*
- This mechanism is characteristic of **griseofulvin**, another antifungal agent used for dermatophyte infections
- **Griseofulvin** interferes with **microtubule function**, disrupting mitotic spindle formation and preventing fungal cell division
*Prevention of lanosterol to ergosterol conversion*
- This mechanism is associated with **azole antifungals** (e.g., fluconazole, itraconazole), which inhibit fungal **cytochrome P450-dependent 14-α-demethylase**
- This enzyme is responsible for the conversion of **lanosterol** to **ergosterol**, leading to ergosterol depletion and accumulation of toxic sterol precursors
Antifungal prophylaxis protocols US Medical PG Question 7: A 46-year-old man with HIV infection comes to the physician because of a 1-week history of severe retrosternal pain while swallowing. He has not been compliant with his antiretroviral drug regimen. His CD4+ T-lymphocyte count is 98/mm3 (N ≥ 500). Endoscopy shows white plaques in the esophagus. The most appropriate immediate treatment is a drug that inhibits which of the following enzymes?
- A. DNA polymerase
- B. Hydrogen-potassium ATPase
- C. Cytochrome p450 enzymes (Correct Answer)
- D. Phospholipase A2
- E. Squalene epoxidase
Antifungal prophylaxis protocols Explanation: ***Cytochrome P450 enzymes***
- The patient's symptoms (retrosternal pain on swallowing, white plaques on endoscopy) and severely low **CD4+ count (98/mm³)** are highly suggestive of **esophageal candidiasis**, a common opportunistic infection in AIDS.
- **Fluconazole**, an azole antifungal, is the **first-line treatment** for esophageal candidiasis and works by inhibiting **14α-demethylase (lanosterol demethylase)**, a fungal **cytochrome P450 enzyme**.
- This inhibition prevents the conversion of lanosterol to ergosterol, disrupting **fungal cell membrane synthesis** and leading to fungal cell death.
*Squalene epoxidase*
- **Terbinafine** and **naftifine** (allylamine antifungals) inhibit squalene epoxidase in the ergosterol synthesis pathway.
- These agents are primarily used for **dermatophyte infections** (onychomycosis, tinea) and have **poor activity against Candida species**.
- They are not appropriate for treating esophageal candidiasis.
*DNA polymerase*
- Inhibitors of **DNA polymerase**, such as acyclovir or ganciclovir, are used to treat **herpesvirus infections** (HSV, CMV).
- While herpes esophagitis can occur in immunocompromised patients, it typically presents with **punched-out ulcers**, not white plaques.
*Hydrogen-potassium ATPase*
- **Proton pump inhibitors** (PPIs) target hydrogen-potassium ATPase in gastric parietal cells to reduce **acid secretion**.
- These are used to treat **GERD** or **peptic ulcers**, which do not present with white plaques on endoscopy.
- While PPIs may provide symptomatic relief, they do not treat the underlying fungal infection.
*Phospholipase A2*
- Phospholipase A2 inhibitors are used as **anti-inflammatory agents**, as PLA2 releases arachidonic acid, a precursor to inflammatory mediators.
- These drugs have no role in treating fungal infections like esophageal candidiasis.
Antifungal prophylaxis protocols US Medical PG Question 8: A 55-year-old woman presents to the physician because of a fever 4 days after discharge from the hospital following induction chemotherapy for acute myeloid leukemia (AML). She has no other complaints and feels well otherwise. Other than the recent diagnosis of AML, she has no history of a serious illness. The temperature is 38.8°C (101.8°F), the blood pressure is 110/65 mm Hg, the pulse is 82/min, and the respirations are 14/min. Examination of the catheter site, skin, head and neck, heart, lungs, abdomen, and perirectal area shows no abnormalities. The results of the laboratory studies show:
Hemoglobin 9 g/dL
Leukocyte count 800/mm3
Percent segmented neutrophils 40%
Platelet count 85,000/mm3
Which of the following is the most appropriate pharmacotherapy at this time?
- A. Valacyclovir
- B. Vancomycin
- C. Imipenem (Correct Answer)
- D. Caspofungin
- E. Ciprofloxacin
Antifungal prophylaxis protocols Explanation: ***Imipenem***
- This patient presents with **febrile neutropenia** (fever >38.3°C and absolute neutrophil count <500/mm³ or expected to fall below 500/mm³). This is a **medical emergency** requiring prompt empiric **broad-spectrum antibiotic** therapy covering **Gram-positive** and **Gram-negative** organisms.
- **Imipenem** is a carbapenem antibiotic with broad-spectrum activity, making it an appropriate choice for empiric treatment of febrile neutropenia, especially in high-risk patients like those undergoing induction chemotherapy for AML.
*Valacyclovir*
- **Valacyclovir** is an antiviral medication used primarily for **herpes simplex** and **varicella-zoster virus** infections.
- While immunocompromised patients are susceptible to viral infections, there is no clinical evidence at this time to suggest a viral etiology, and **febrile neutropenia** takes precedence for immediate broad-spectrum antibacterial coverage.
*Vancomycin*
- **Vancomycin** is an antibiotic that specifically targets **Gram-positive bacteria**, particularly **methicillin-resistant Staphylococcus aureus (MRSA)**.
- Empiric vancomycin is not typically recommended as initial sole therapy for febrile neutropenia unless there is strong suspicion of a Gram-positive infection (e.g., catheter-related infection, mucositis, skin and soft tissue infection, or known colonization with MRSA), which is not present here.
*Caspofungin*
- **Caspofungin** is an **antifungal** medication used to treat invasive fungal infections, including candidiasis and aspergillosis.
- Initial management of febrile neutropenia focuses on bacterial infections; empiric antifungal therapy is usually initiated if fever persists despite broad-spectrum antibiotics for several days.
*Ciprofloxacin*
- **Ciprofloxacin** is a fluoroquinolone antibiotic with good activity against many **Gram-negative bacteria** but limited activity against **Gram-positive organisms** and anaerobes.
- While it can be used for prophylaxis or as part of a combination regimen, it is not considered sufficient as a single agent for empiric treatment of **high-risk febrile neutropenia** due to its limited spectrum and increasing resistance patterns.
Antifungal prophylaxis protocols US Medical PG Question 9: A previously healthy 16-year-old boy comes to the physician because of a pruritic rash on the chest that has become progressively larger over the past 10 days. It is not painful. He is sexually active with two female partners and uses condoms inconsistently. He works part-time as a lifeguard. He has no family history of serious illness. He does not smoke. He drinks 5–6 beers on weekends. His temperature is 36.7°C (98°F), pulse is 66/min, and blood pressure is 110/70 mm Hg. A photograph of the rash is shown below. Which of the following is the most appropriate next step in management?
- A. Topical miconazole (Correct Answer)
- B. Phototherapy
- C. Reassurance
- D. Topical erythromycin
- E. Topical hydrocortisone
Antifungal prophylaxis protocols Explanation: **Topical miconazole**
- The rash described, especially in a lifeguard who is frequently exposed to moisture, suggests **tinea corporis** (ringworm), a **dermatophyte fungal infection**.
- **Topical imidazole antifungals** like miconazole are the first-line treatment for localized tinea infections.
*Phototherapy*
- **Phototherapy** (e.g., UVB or PUVA) is used for chronic widespread dermatoses like **psoriasis** or severe **atopic dermatitis**, not typically for localized fungal infections.
- This rash is likely **infectious** and requires an antifungal agent for resolution.
*Reassurance*
- The rash is described as **progressively larger** and **pruritic**, indicating an active and symptomatic process that requires intervention, not just reassurance.
- Delaying treatment could lead to further spread or secondary bacterial infection.
*Topical erythromycin*
- **Topical erythromycin** is an **antibiotic** used to treat bacterial skin infections, such as **acne vulgaris** or impetigo.
- It would be ineffective against a fungal infection like tinea corporis.
*Topical hydrocortisone*
- **Topical hydrocortisone** is a **corticosteroid** that reduces inflammation and itching.
- While it might temporarily alleviate symptoms, it can actually worsen fungal infections by suppressing the local immune response, leading to **tinea incognito**.
Antifungal prophylaxis protocols US Medical PG Question 10: A 35-year-old African American male is admitted to the hospital following a recent diagnosis of systemic histoplasmosis and subsequently treated with an intravenous anti-fungal agent. During the course of his hospital stay, he complains of headaches. Work-up reveals hypotension, anemia, and elevated BUN and creatinine. His medication is known to cause these side-effects through its binding of cell membrane ergosterol. With which anti-fungal is he most likely being treated?
- A. Griseofulvin
- B. Amphotericin B (Correct Answer)
- C. Flucytosine
- D. Fluconazole
- E. Terbinafine
Antifungal prophylaxis protocols Explanation: ***Amphotericin B***
- **Amphotericin B** is known for its significant side effects, including **nephrotoxicity** (leading to elevated BUN and creatinine, and potentially anemia due to reduced erythropoietin production) and **infusion-related reactions** like headache and hypotension.
- It works by binding to **ergosterol** in fungal cell membranes, forming pores that lead to cell death, but it can also bind to cholesterol in mammalian cell membranes contributing to its toxicity.
*Griseofulvin*
- **Griseofulvin** primarily acts by binding to **keratin** and interfering with fungal **mitosis**; it does not bind to ergosterol.
- Its main side effects include **GI upset**, headache, and photosensitivity, but not prominent nephrotoxicity or hypotension in the manner described.
*Flucytosine*
- **Flucytosine** is an antimetabolite that is converted to **5-fluorouracil** within fungal cells, interfering with RNA and DNA synthesis. It does not bind to ergosterol.
- Its major adverse effects include **bone marrow suppression** (leukopenia, thrombocytopenia) and liver enzyme elevation, not the constellation of symptoms (hypotension, renal failure) described.
*Fluconazole*
- **Fluconazole** is an azole antifungal that inhibits **ergosterol synthesis** by blocking fungal cytochrome P450 enzymes. It does not directly bind to ergosterol.
- While it can cause some GI upset and liver enzyme elevation, it is generally well-tolerated and less associated with acute nephrotoxicity or hypotension compared to Amphotericin B.
*Terbinafine*
- **Terbinafine** inhibits **squalene epoxidase**, an enzyme involved in ergosterol synthesis, rather than binding directly to ergosterol itself.
- Its main side effects include **GI disturbances**, headache, and liver enzyme abnormalities, but typically not the severe nephrotoxicity and hypotension associated with Amphotericin B.
More Antifungal prophylaxis protocols US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.