Polymyxins US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Polymyxins. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Polymyxins US Medical PG Question 1: A forty-five-year-old farmer with past medical history of diabetes, hypertension, and possible narrow angles comes into your emergency room confused, diaphoretic, salivating, vomiting and shedding tears. He has pinpoint pupils. You conclude that he is showing effects of acute organophosphate poisoning. While administering the antidote, you should carefully monitor for which of the following side effects?
- A. Barotrauma to middle ear
- B. Bronchospasm
- C. Hyperkalemia
- D. Acute closed-angle glaucoma (Correct Answer)
- E. Tinnitus
Polymyxins Explanation: ***Acute closed-angle glaucoma***
- **Atropine**, a common antidote for organophosphate poisoning, can dilate the pupils and **increase intraocular pressure**, precipitating acute closed-angle glaucoma in susceptible individuals.
- The patient's history of "possible narrow angles" indicates a predisposition to this condition, making careful monitoring essential during atropine administration.
*Barotrauma to middle ear*
- **Barotrauma** is typically associated with changes in **ambient pressure**, such as during air travel or diving.
- There is no direct physiological link between organophosphate poisoning treatment and middle ear barotrauma.
*Bronchospasm*
- **Organophosphate poisoning** *causes* bronchospasm due to excessive cholinergic stimulation, while atropine is used to *reverse* it.
- Therefore, bronchospasm would improve, not worsen, with appropriate antidote administration.
*Hyperkalemia*
- **Hyperkalemia** is not a direct side effect of atropine or a common complication of organophosphate poisoning treatment.
- While electrolyte imbalances can occur in critically ill patients, hyperkalemia is not specifically monitored for in this context.
*Tinnitus*
- **Tinnitus** is a perception of noise or ringing in the ears often associated with **auditory system damage** or certain medications.
- It is not a recognized side effect of atropine or a complication to specifically monitor for in organophosphate poisoning.
Polymyxins US Medical PG Question 2: A 42-year-old woman with a history of multiple sclerosis and recurrent urinary tract infections comes to the emergency department because of flank pain and fever. Her temperature is 38.8°C (101.8°F). Examination shows left-sided costovertebral angle tenderness. She is admitted to the hospital and started on intravenous vancomycin. Three days later, her symptoms have not improved. Urine culture shows growth of Enterococcus faecalis. Which of the following best describes the most likely mechanism of antibiotic resistance in this patient?
- A. Increased efflux across bacterial cell membranes
- B. Production of beta-lactamase
- C. Alteration of penicillin-binding proteins
- D. Alteration of peptidoglycan synthesis (Correct Answer)
- E. Alteration of ribosomal targets
Polymyxins Explanation: ***Alteration of peptidoglycan synthesis***
- **Vancomycin** targets the **D-Ala-D-Ala terminus** on the peptidoglycan precursor, preventing cross-linking during bacterial cell wall synthesis.
- **Vancomycin resistance in Enterococcus faecalis** occurs through acquisition of resistance genes (vanA, vanB) that encode enzymes modifying the peptidoglycan precursor from **D-Ala-D-Ala to D-Ala-D-Lac**.
- This structural change reduces vancomycin's binding affinity by approximately 1000-fold, rendering the antibiotic ineffective.
- The mechanism directly involves **alteration of the peptidoglycan synthesis pathway**, specifically the terminal amino acid residues of the pentapeptide precursor.
*Increased efflux across bacterial cell membranes*
- This mechanism involves **efflux pumps that actively transport antibiotics out of the bacterial cell**, reducing intracellular concentration.
- While efflux pumps contribute to resistance for antibiotics like **tetracyclines, fluoroquinolones, and macrolides**, this is not the primary mechanism of vancomycin resistance in Enterococcus.
*Production of beta-lactamase*
- **Beta-lactamase enzymes** hydrolyze the **beta-lactam ring** of antibiotics like **penicillins and cephalosporins**, rendering them inactive.
- **Vancomycin is a glycopeptide antibiotic, not a beta-lactam**, so its efficacy is not affected by beta-lactamase production.
*Alteration of ribosomal targets*
- This mechanism confers resistance to antibiotics that target **bacterial ribosomes** to inhibit protein synthesis, such as **macrolides, aminoglycosides, and tetracyclines**.
- **Vancomycin acts on cell wall synthesis**, not protein synthesis, so alteration of ribosomal targets is not relevant to vancomycin resistance.
*Alteration of penicillin-binding proteins*
- **Penicillin-binding proteins (PBPs)** are the targets of **beta-lactam antibiotics** (penicillins, cephalosporins, carbapenems).
- Alterations in PBPs cause resistance to beta-lactams, not to vancomycin.
- **Vancomycin does not interact with PBPs**; it binds directly to the D-Ala-D-Ala terminus of peptidoglycan precursors in the cell wall.
Polymyxins US Medical PG Question 3: A 77-year-old woman is brought to the emergency department from her nursing home because she was found down overnight. On presentation she was found to be delirious and was unable to answer questions. Chart review shows that she is allergic to cephalosporins. Her temperature is 102.2°F (39°C), blood pressure is 105/52 mmHg, pulse is 94/min, and respirations are 23/min. Physical exam reveals a productive cough. A metabolic panel is obtained with the following results:
Serum:
Na+: 135 mEq/L
Cl-: 95 mEq/L
K+: 4 mEq/L
HCO3-: 19 mEq/L
BUN: 40 mg/dL
Creatinine: 2.5 mg/dL
Glucose: 150 mg/dL
Based on these findings two different drugs are started empirically. Gram stain on a blood sample is performed showing the presence of gram-positive organisms on all samples. One of the drugs is subsequently stopped. The drug that was most likely stopped has which of the following characteristics?
- A. Resistance conveyed through acetylation
- B. Associated with red man syndrome
- C. Single-ringed ß-lactam structure (Correct Answer)
- D. Causes discolored teeth in children
- E. Accumulates inside bacteria via O2-dependent uptake
Polymyxins Explanation: ***Single-ringed ß-lactam structure***
- The patient presents with **sepsis** due to **pneumonia** likely caused by **gram-positive organisms**. Given a cephalosporin allergy, **aztreonam** (a monobactam) would be an initial empirical antibiotic choice to cover gram-negative bacteria, alongside a drug for gram-positive coverage (like vancomycin).
- Since the **blood cultures** confirmed **gram-positive organisms**, the drug covering gram-negative bacteria (aztreonam) would be stopped. Aztreonam is characterized by its **single-ringed β-lactam structure**.
*Resistance conveyed through acetylation*
- This mechanism of resistance is typical of **aminoglycosides** (e.g., gentamicin) and **chloramphenicol**.
- Aminoglycosides were unlikely to be one of the empirically started drugs, as they are often used in combination with β-lactams, and this patient has a cephalosporin allergy.
*Associated with red man syndrome*
- **Red man syndrome** is a common adverse effect associated with **vancomycin** administration, especially with rapid infusion.
- Vancomycin would likely be continued, as it effectively targets gram-positive organisms, including **MRSA**, and is a suitable alternative given the cephalosporin allergy.
*Causes discolored teeth in children*
- This is a characteristic side effect of **tetracyclines** (e.g., doxycycline), which are contraindicated in young children and pregnant women due to their effects on bone and teeth development.
- Tetracyclines are not typically first-line empiric therapy for severe pneumonia or sepsis, especially in an elderly patient.
*Accumulates inside bacteria via O2-dependent uptake*
- This describes the mechanism of uptake for **aminoglycosides**. Their entry into bacteria is an **energy-dependent process** requiring oxygen.
- As mentioned, aminoglycosides are less likely to be the initial drug stopped in this scenario, as they target gram-negative bacteria.
Polymyxins US Medical PG Question 4: A scientist is studying the mechanisms by which bacteria become resistant to antibiotics. She begins by obtaining a culture of vancomycin-resistant Enterococcus faecalis and conducts replicate plating experiments. In these experiments, colonies are inoculated onto a membrane and smeared on 2 separate plates, 1 containing vancomycin and the other with no antibiotics. She finds that all of the bacterial colonies are vancomycin resistant because they grow on both plates. She then maintains the bacteria in liquid culture without vancomycin while she performs her other studies. Fifteen generations of bacteria later, she conducts replicate plating experiments again and finds that 20% of the colonies are now sensitive to vancomycin. Which of the following mechanisms is the most likely explanation for why these colonies have become vancomycin sensitive?
- A. Point mutation
- B. Gain of function mutation
- C. Viral infection
- D. Plasmid loss (Correct Answer)
- E. Loss of function mutation
Polymyxins Explanation: ***Plasmid loss***
- The initial **vancomycin resistance** in *Enterococcus faecalis* is often mediated by genes located on **plasmids**, which are extrachromosomal DNA.
- In the absence of selective pressure (vancomycin), bacteria that lose the plasmid (and thus the resistance genes) have a **growth advantage** over those that retain the energetically costly plasmid, leading to an increase in sensitive colonies over generations.
*Point mutation*
- A **point mutation** typically involves a change in a single nucleotide and could lead to loss of resistance if it occurred in a gene conferring resistance.
- However, since there was no selective pressure for loss of resistance, it is less likely that 20% of the population would acquire such a specific point mutation to revert resistance.
*Gain of function mutation*
- A **gain of function mutation** would imply that the bacteria acquired a *new* advantageous trait, not the *loss* of resistance.
- This type of mutation would not explain why some colonies became sensitive to vancomycin after the drug was removed.
*Viral infection*
- **Viral infection** (bacteriophages) can transfer genes through transduction or cause bacterial lysis, but it's not the primary mechanism for a widespread reversion of resistance in the absence of antibiotic pressure.
- It would not explain the observed increase in vancomycin-sensitive colonies due to evolutionary pressure.
*Loss of function mutation*
- While a **loss of function mutation** in a gene conferring resistance could lead to sensitivity, it's generally less likely to explain a 20% shift without selective pressure than **plasmid loss**.
- Plasmids are often unstable and are easily lost in the absence of selection, whereas a specific gene mutation causing loss of function would need to arise and become prevalent in the population.
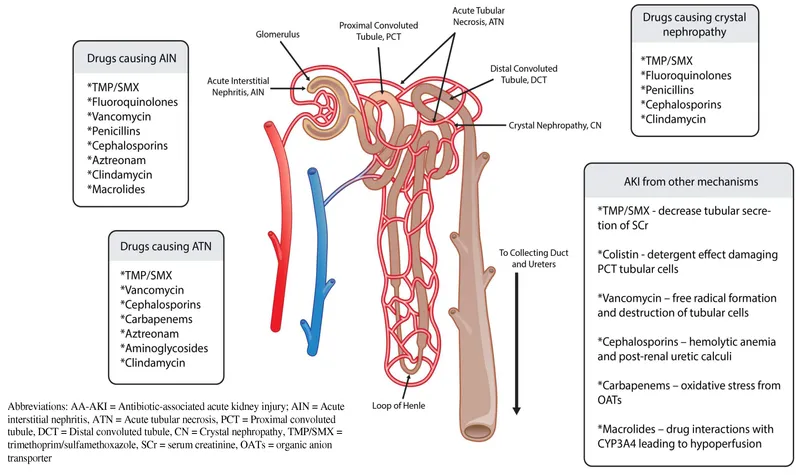
Polymyxins US Medical PG Question 5: A 53-year-old woman presents with a severe headache, nausea, and vomiting for the past 48 hours. Vitals show a blood pressure of 220/134 mm Hg and a pulse of 88/min. Urinalysis shows a 2+ proteinuria and RBC casts. Which of the following renal lesions is most likely to be seen in this patient?
- A. Papillary necrosis
- B. Fibrinoid necrosis (Correct Answer)
- C. Acute tubular necrosis (ATN)
- D. Acute pyelonephritis
- E. Acute interstitial nephritis (AIN)
Polymyxins Explanation: ***Fibrinoid necrosis***
- The patient's presentation with **severe hypertension** (220/134 mm Hg), **proteinuria**, and **RBC casts** is highly suggestive of a **hypertensive crisis with malignant nephrosclerosis**.
- **Fibrinoid necrosis** refers to the accumulation of **fibrin-like material** in the walls of arterioles, a characteristic pathological finding in **malignant hypertension** leading to vascular damage in the kidney.
*Papillary necrosis*
- This condition is typically associated with **analgesic nephropathy**, **diabetes mellitus**, and **urinary tract obstruction** or **sickle cell disease**.
- While it can cause renal dysfunction, it does not directly explain the acute severe hypertension and RBC casts unique to hypertensive emergencies.
*Acute tubular necrosis (ATN)*
- While ATN can cause **acute kidney injury**, it is usually characterized by **muddy brown casts** and is often precipitated by **ischemic** or **nephrotoxic insults**.
- The prominent hypertension and RBC casts point away from primary ATN in this context.
*Acute pyelonephritis*
- Acute pyelonephritis is an **infection of the kidney** characterized by **fever**, **flank pain**, and **pyuria** (white blood cells in urine), usually not severe hypertension and RBC casts.
- The main findings in this patient are related to vascular damage, not infection.
*Acute interstitial nephritis (AIN)*
- AIN is often caused by **drug reactions** or systemic diseases, presenting with **fever**, **rash**, **eosinophilia**, and **white blood cell casts**.
- The clinical picture of severe hypertension and RBC casts is not typical for AIN.
Polymyxins US Medical PG Question 6: A microbiology student was given a swab containing an unknown bacteria taken from the wound of a soldier and asked to identify the causative agent. She determined that the bacteria was a gram-positive, spore-forming bacilli, but had difficulty narrowing it down to the specific bacteria. The next test she performed was the Nagler's test, in which she grew the bacteria on a plate made from egg yolk, which would demonstrate the ability of the bacteria to hydrolyze phospholipids and produce an area of opacity. Half the plate contained a specific antitoxin which prevented hydrolysis of phospholipids while the other half did not contain any antitoxin. The bacteria produced an area of opacity only on half of the plate containing no antitoxin. Which of the following toxins was the antitoxin targeting?
- A. Alpha toxin (Correct Answer)
- B. Exotoxin A
- C. Tetanus toxin
- D. Diphtheria toxin
- E. Botulinum toxin
Polymyxins Explanation: ***Alpha toxin***
- The scenario describes a **Nagler's test**, which is specifically used to detect the presence of **alpha toxin (lecithinase)** produced by *Clostridium perfringens*.
- The antitoxin prevents the hydrolysis of phospholipids and the formation of opacity, confirming that the opacity is due to the alpha toxin.
*Exotoxin A*
- **Exotoxin A** is a toxin produced by *Pseudomonas aeruginosa* and inhibits protein synthesis.
- It is not associated with the **Nagler's test** or phospholipid hydrolysis on egg yolk agar.
*Tetanus toxin*
- **Tetanus toxin** is produced by *Clostridium tetani* and causes spastic paralysis by inhibiting inhibitory neurotransmitter release.
- It is not involved in phospholipid hydrolysis or detected by the **Nagler's test**.
*Diphtheria toxin*
- **Diphtheria toxin** is produced by *Corynebacterium diphtheriae* and inhibits protein synthesis, leading to cellular death.
- This toxin is not detected by the **Nagler's test** and does not cause phospholipid hydrolysis.
*Botulinum toxin*
- **Botulinum toxin** is produced by *Clostridium botulinum* and causes flaccid paralysis by inhibiting acetylcholine release at the neuromuscular junction.
- It is not associated with the **Nagler's test** or the hydrolysis of phospholipids.
Polymyxins US Medical PG Question 7: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Polymyxins Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Polymyxins US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Polymyxins Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Polymyxins US Medical PG Question 9: A 41-year-old homeless man is brought to the emergency department complaining of severe fever, dizziness, and a persistent cough. The patient has a history of long-standing alcohol abuse and has frequently presented to the emergency department with acute alcohol intoxication. The patient states that his cough produces ‘dark brown stuff’ and he provided a sample for evaluation upon request. The patient denies having any other underlying medical conditions and states that he has no other symptoms. He denies taking any medications, although he states that he knows he has a sulfa allergy. On observation, the patient looks frail and severely fatigued. The vital signs include: blood pressure 102/72 mm Hg, pulse 98/min, respiratory rate 15/min, and temperature 37.1°C (98.8°F). Auscultation reveals crackles in the left upper lobe and chest X-ray reveals an infiltrate in the same area. Which of the following is the most appropriate treatment for this patient?
- A. Trimethoprim-sulfamethoxazole
- B. Vancomycin
- C. Clindamycin (Correct Answer)
- D. Piperacillin-tazobactam
- E. Ciprofloxacin
Polymyxins Explanation: ***Clindamycin***
- The patient, a severely fatigued, homeless man with a history of alcohol abuse, presents with **fever, dizziness, cough producing 'dark brown stuff'**, and crackles/infiltrate in the left upper lobe. This clinical picture is highly suggestive of aspiration pneumonia and/or lung abscess, often caused by **anaerobic bacteria** found in the oral flora.
- **Clindamycin** is the **first-line treatment** for aspiration pneumonia in stable patients, with excellent activity against oral anaerobes, good lung tissue penetration, and proven efficacy in outpatient management.
*Trimethoprim-sulfamethoxazole*
- This antibiotic is **contraindicated** due to the patient's stated **sulfa allergy**.
- While effective against some respiratory pathogens, it does not provide adequate coverage for the likely anaerobic organisms involved in aspiration pneumonia.
*Vancomycin*
- Vancomycin is primarily used for serious **Gram-positive infections**, particularly **MRSA**, and does not provide adequate coverage for **anaerobic bacteria** typically involved in aspiration pneumonia.
- There is no clinical indication for MRSA coverage in this patient's presentation.
*Piperacillin-tazobactam*
- While piperacillin-tazobactam has excellent broad-spectrum activity, including against anaerobes, and would be effective for aspiration pneumonia, it is typically reserved for **hospitalized patients with severe pneumonia** or healthcare-associated infections.
- For a **stable outpatient** with aspiration pneumonia, clindamycin is preferred as it is more targeted, cost-effective, and the standard first-line therapy.
*Ciprofloxacin*
- Ciprofloxacin is a **fluoroquinolone** with good activity against many **Gram-negative bacteria** and some atypical respiratory pathogens.
- However, it has **poor activity against anaerobic bacteria**, which are the primary concern in aspiration pneumonia.
Polymyxins US Medical PG Question 10: A group of scientists discovered a neurotoxin that prevents neurons from releasing neurotransmitters. They performed a series of experiments to determine the protein that the neurotoxin affected. They used a fluorescent molecule that localizes to synaptic vesicles. In the control experiment, they observed the movement of vesicles from the cell body down the axon and finally to the synapse, and they saw movement from the synapse back to the cell body. When the neurotoxin was applied, the vesicles stopped moving down the axon, but movement back to the cell body still occurred. They also applied tetanospasmin and botulinum toxin to see if these toxins exhibited similar behavior but they did not. Which of the following proteins is most likely affected by this neurotoxin?
- A. SNAP-25
- B. Kinesin (Correct Answer)
- C. Dynein
- D. Synaptobrevin
- E. Alpha/Beta tubulin
Polymyxins Explanation: ***Kinesin***
- Kinesin is a **motor protein** responsible for **anterograde transport** (movement away from the cell body) of vesicles along microtubules in axons.
- The neurotoxin stopping vesicles from moving down the axon indicates interference with anterograde transport, which is primarily mediated by kinesin.
*SNAP-25*
- **SNAP-25** is a component of the **SNARE complex** involved in the fusion of synaptic vesicles with the presynaptic membrane, leading to neurotransmitter release.
- Tetanospasmin and botulinum toxin, which affect neurotransmitter release, specifically cleave SNARE proteins like SNAP-25, but the described toxin's effect on vesicle *movement* rather than *fusion* differentiates it.
*Dynein*
- Dynein is a **motor protein** responsible for **retrograde transport** (movement towards the cell body) of vesicles along microtubules.
- The observation that movement back to the cell body (retrograde transport) still occurred after neurotoxin application rules out dynein as the affected protein.
*Synaptobrevin*
- **Synaptobrevin** (also known as VAMP) is another component of the **SNARE complex**, located on the vesicle membrane, crucial for neurotransmitter release.
- Its disruption would primarily impair vesicle fusion and neurotransmitter release, similar to SNAP-25, but would not directly stop the *downstream movement* of vesicles.
*Alpha/Beta tubulin*
- **Alpha/beta tubulin dimers** are the building blocks of **microtubules**, which serve as tracks for both anterograde and retrograde transport.
- While microtubules are essential for vesicle movement, if tubulin itself were directly affected, both anterograde and retrograde transport would likely be impaired, which contradicts the observation that retrograde movement continued.
More Polymyxins US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.