Penicillins and beta-lactamase inhibitors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Penicillins and beta-lactamase inhibitors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Penicillins and beta-lactamase inhibitors US Medical PG Question 1: A pharmaceutical company has modified one of its existing antibiotics to have an improved toxicity profile. The new antibiotic blocks protein synthesis by first entering the cell and then binding to active ribosomes. The antibiotic mimics the structure of aminoacyl-tRNA. The drug is covalently bonded to the existing growing peptide chain via peptidyl transferase, thereby impairing the rest of protein synthesis and leading to early polypeptide truncation. Where is the most likely site that this process occurs?
- A. E site
- B. 30S small subunit
- C. A site (Correct Answer)
- D. 40S small subunit
- E. P site
Penicillins and beta-lactamase inhibitors Explanation: ***A site***
- The **A (aminoacyl) site** is where incoming aminoacyl-tRNAs bind during translation, bringing new amino acids to the ribosome. Since the antibiotic mimics **aminoacyl-tRNA** and is covalently bonded to the peptide chain by **peptidyl transferase**, its action must occur at the A site.
- Binding at the A site and subsequent peptide bond formation with the antibiotic would lead to premature polypeptide truncation, as no further amino acids can be added.
*E site*
- The **E (exit) site** is where deacylated tRNAs are released from the ribosome after having delivered their amino acid to the growing peptide chain in the P site.
- The antibiotic's mechanism of action, involving binding and covalent incorporation into the peptide, does not align with the function of the E site.
*30S small subunit*
- The **30S small ribosomal subunit** in prokaryotes is primarily involved in mRNA binding and decoding, ensuring the correct aminoacyl-tRNA binds to the mRNA codon.
- While the antibiotic binds to active ribosomes, its key action described as mimicking aminoacyl-tRNA and being incorporated by peptidyl transferase points to a specific binding site within the ribosome rather than the entire subunit's general function.
*40S small subunit*
- The **40S small ribosomal subunit** is found in **eukaryotic ribosomes**, not prokaryotic ones, and is involved in mRNA binding during initiation.
- The question implies an antibiotic targeting bacterial protein synthesis (given its discussion of modifying an existing antibiotic), making eukaryotic ribosomal subunits an unlikely target.
*P site*
- The **P (peptidyl) site** holds the tRNA carrying the growing polypeptide chain. Peptidyl transferase activity forms a peptide bond between the amino acid in the A site and the peptide in the P site.
- While peptidyl transferase is involved, the antibiotic *mimics* aminoacyl-tRNA, which is delivered to the A site for peptide bond formation, rather than the P site which already holds the growing chain.
Penicillins and beta-lactamase inhibitors US Medical PG Question 2: An 18-year old college freshman presents to his university clinic because he has not been feeling well for the past two weeks. He has had a persistent headache, occasional cough, and chills without rigors. The patient’s vital signs are normal and physical exam is unremarkable. His radiograph shows patchy interstitial lung infiltrates and he is diagnosed with atypical pneumonia. The patient is prescribed azithromycin and takes his medication as instructed. Despite adherence to his drug regimen, he returns to the clinic one week later because his symptoms have not improved. The organism responsible for this infection is likely resistant to azithromycin through which mechanism?
- A. Mutation in topoisomerase II
- B. Methylation of ribosomal binding site
- C. Presence of a beta-lactamase
- D. Decreased binding to RNA polymerase
- E. Insertion of drug efflux pumps (Correct Answer)
Penicillins and beta-lactamase inhibitors Explanation: ***Insertion of drug efflux pumps***
- **Azithromycin** is a macrolide antibiotic that inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit**.
- In **Mycoplasma pneumoniae** (the most common cause of atypical pneumonia in young adults), the **most common** mechanism of macrolide resistance is through **efflux pumps**, particularly the **mef genes**.
- These efflux pumps actively transport macrolides out of the bacterial cell, reducing intracellular drug concentration and conferring resistance.
- This mechanism is responsible for the majority of macrolide-resistant *M. pneumoniae* isolates worldwide.
*Methylation of ribosomal binding site*
- **Methylation** of the ribosomal binding site (specifically the **23S rRNA** via erm genes) does prevent azithromycin from binding effectively.
- While this is a valid macrolide resistance mechanism seen in organisms like *Streptococcus pneumoniae* and *Streptococcus pyogenes*, it is **less common** in *Mycoplasma pneumoniae*.
- Efflux pumps (mef) are the predominant mechanism in *M. pneumoniae* resistant strains.
*Mutation in topoisomerase II*
- **Topoisomerase II** (DNA gyrase) is the target of **fluoroquinolone antibiotics**, not macrolides.
- Mutations in this enzyme lead to resistance against fluoroquinolones, such as **ciprofloxacin**.
*Presence of a beta-lactamase*
- **Beta-lactamase enzymes** inactivate **beta-lactam antibiotics** (e.g., penicillin, cephalosporins) by hydrolyzing their beta-lactam ring.
- Additionally, *Mycoplasma pneumoniae* **lacks a cell wall**, making it inherently resistant to all beta-lactam antibiotics regardless of beta-lactamase production.
*Decreased binding to RNA polymerase*
- **RNA polymerase** is the target for antibiotics like **rifampin**, which inhibits bacterial transcription.
- Decreased binding to RNA polymerase would lead to rifampin resistance, not azithromycin resistance.
Penicillins and beta-lactamase inhibitors US Medical PG Question 3: A 64-year-old female with type 2 diabetes mellitus comes to the physician because of a 1-week history of painful red swelling on her left thigh. Examination shows a 3- x 4-cm, tender, fluctuant mass. Incision and drainage of the abscess are performed. Culture of the abscess fluid grows gram-positive, coagulase-positive cocci that are resistant to oxacillin. Which of the following best describes the mechanism of resistance of the causal organism to oxacillin?
- A. Degradation of the antibiotic
- B. Decreased uptake of the antibiotic
- C. Decreased activation of the antibiotic
- D. Altered target of the antibiotic (Correct Answer)
- E. Acetylation of the antibiotic
Penicillins and beta-lactamase inhibitors Explanation: ***Altered target of the antibiotic***
- The organism described (gram-positive, coagulase-positive cocci, oxacillin-resistant) is **methicillin-resistant *Staphylococcus aureus* (MRSA)**.
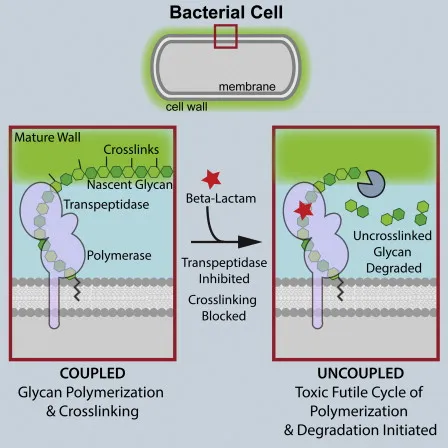
- MRSA achieves oxacillin (and other beta-lactam) resistance by acquiring the ***mecA* gene**, which encodes for a **modified penicillin-binding protein (PBP2a)** with reduced affinity for beta-lactam antibiotics.
*Degradation of the antibiotic*
- This mechanism, primarily through the production of **beta-lactamase enzymes**, can degrade beta-lactam antibiotics.
- While *Staphylococcus aureus* can produce beta-lactamases, oxacillin (a **penicillinase-resistant penicillin**) is specifically engineered to be stable against these enzymes.
*Decreased uptake of the antibiotic*
- Reduced permeability of the bacterial cell wall can lead to decreased uptake, a mechanism more commonly associated with **gram-negative bacteria** due to their outer membrane.
- This is not the primary mechanism of resistance for MRSA to oxacillin.
*Decreased activation of the antibiotic*
- Some antibiotics are prodrugs that require activation by bacterial enzymes, and resistance can arise from mutations affecting this activation.
- Oxacillin is active in its administered form and does not require bacterial activation.
*Acetylation of the antibiotic*
- **Enzymatic modification**, such as acetylation, adenylylation, or phosphorylation, is a common mechanism of resistance, particularly against **aminoglycoside antibiotics**.
- This specific mechanism is not responsible for oxacillin resistance in MRSA.
Penicillins and beta-lactamase inhibitors US Medical PG Question 4: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Penicillins and beta-lactamase inhibitors Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
Penicillins and beta-lactamase inhibitors US Medical PG Question 5: A 51-year-old man is admitted to the hospital because of a 2-day history of fever, nausea, and abdominal pain. His temperature is 39.4°C (102.9°F) and pulse is 106/min. Physical examination shows tenderness in the right upper quadrant. Blood cultures grow nonhemolytic, gram-positive cocci that grow in hypertonic saline. Antibiotic sensitivity testing of the isolated organism shows that gentamicin has a minimum inhibitory concentration (MIC) of 16 μg/mL. The addition of ampicillin, which has an MIC of 2 μg/mL alone, decreases the MIC of gentamicin to 0.85 μg/mL. The decrease in the MIC of gentamicin with the addition of ampicillin is most likely due to which of the following mechanisms?
- A. Increase in the intracellular uptake of gentamicin (Correct Answer)
- B. Sequential block of essential micronutrient synthesis
- C. Inhibition of the acetylation of gentamicin
- D. Additive bacteriostatic effect of ampicillin
- E. Stabilization of gentamicin binding at the target site
Penicillins and beta-lactamase inhibitors Explanation: ***Increase in the intracellular uptake of gentamicin***
- This scenario describes **synergism**, where ampicillin (a cell wall synthesis inhibitor) damages the bacterial cell wall, allowing better penetration of gentamicin (an aminoglycoside) into the cell. Aminoglycosides require **active transport** across the bacterial cell membrane, which is enhanced by cell wall disruption.
- The significant reduction in gentamicin's MIC when combined with ampicillin demonstrates that ampicillin facilitates gentamicin's access to its **ribosomal target**, leading to a more potent bactericidal effect.
*Sequential block of essential micronutrient synthesis*
- **Sequential block** typically refers to the synergistic action of drugs like trimethoprim and sulfamethoxazole, which inhibit different steps in the **folic acid synthesis pathway**.
- This mechanism is not directly applicable to the combination of a cell wall inhibitor and an aminoglycoside, which target different cellular processes.
*Inhibition of the acetylation of gentamicin*
- **Acetylation** is a common mechanism of aminoglycoside inactivation by bacterial enzymes (aminoglycoside-modifying enzymes).
- Ampicillin does not primarily work by inhibiting these enzymes; its main action is on **peptidoglycan synthesis** in the bacterial cell wall.
*Additive bacteriostatic effect of ampicillin*
- Ampicillin is a **bactericidal antibiotic** that works by inhibiting cell wall synthesis, not typically bacteriostatic in its primary action, especially against susceptible organisms.
- The dramatic drop in gentamicin's MIC suggests more than just an additive bacteriostatic effect; it indicates a **synergistic interaction** leading to enhanced bactericidal activity.
*Stabilization of gentamicin binding at the target site*
- Gentamicin binds to the bacterial **30S ribosomal subunit**, inhibiting protein synthesis.
- Ampicillin's mechanism of action is on the **bacterial cell wall**, and it does not directly stabilize the binding of gentamicin to the ribosome. Its role is to facilitate gentamicin's entry into the cell.
Penicillins and beta-lactamase inhibitors US Medical PG Question 6: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Penicillins and beta-lactamase inhibitors Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
Penicillins and beta-lactamase inhibitors US Medical PG Question 7: A 14-year-old boy is brought to the emergency department by his parents for joint pain following the acute onset of a diffuse, pruritic rash for the past 24 hours. A week ago, he was diagnosed with pharyngitis after returning home from summer camp and is currently taking antibiotics. There is no family history of serious illness. His temperature is 38.5°C (101.3°F), pulse is 90/min, and blood pressure is 110/70 mm Hg. Physical examination shows periorbital edema, generalized lymphadenopathy, and well-circumscribed, erythematous, confluent skin lesions of variable sizes up to several centimeters in width over his entire body. There is pain on passive movement of wrists and ankle joints bilaterally. Urine dipstick shows 1+ proteinuria. There is no hematuria. Which of the following is the most appropriate next step in management?
- A. Administer diphenhydramine
- B. Perform allergy testing
- C. Administer prednisone
- D. Switch medication to doxycycline
- E. Discontinue antibiotic (Correct Answer)
Penicillins and beta-lactamase inhibitors Explanation: ***Discontinue antibiotic***
- The constellation of **rash, fever, joint pain, lymphadenopathy**, and **mild proteinuria** in a patient recently started on antibiotics strongly suggests **serum sickness-like reaction (SSLR)**. The most crucial initial step is to discontinue the offending agent.
- SSLR is a **Type III hypersensitivity reaction** to certain drugs, particularly beta-lactam antibiotics (like cefaclor or penicillin), which manifest as immune complex deposition.
*Administer diphenhydramine*
- While antihistamines like diphenhydramine might help alleviate some symptoms like **pruritus**, they do not address the underlying **immune complex deposition** causing the systemic reaction.
- Symptomatic treatment alone is insufficient as the primary management for SSLR, which requires removing the causative agent.
*Perform allergy testing*
- Allergy testing (e.g., skin prick tests) is generally performed to identify immediate **IgE-mediated hypersensitivity reactions**, not typically for delayed, immune complex-mediated reactions like SSLR.
- The immediate priority is to stop the presumed causative drug, not to perform diagnostic tests that may not even be appropriate for this type of reaction.
*Administer prednisone*
- **Steroids (prednisone)** may be considered for severe cases of SSLR to manage systemic inflammation and immune response.
- However, the initial and most critical step is to identify and **discontinue the offending antibiotic** before initiating corticosteroids, as removing the trigger is paramount to resolving the condition.
*Switch medication to doxycycline*
- Switching to another antibiotic, especially if the current reaction is due to antibiotics, risks **cross-reactivity** or initiating another adverse drug reaction.
- Without a confirmed bacterial infection requiring immediate antibiotic therapy, continuing antibiotic treatment while an SSLR is suspected is inappropriate and potentially harmful.
Penicillins and beta-lactamase inhibitors US Medical PG Question 8: A 26-year-old woman presents to her primary care physician because she has been experiencing occasional fevers and chills for the last 3 weeks. She says that the fevers have been accompanied by abdominal pain and increased vaginal discharge. On presentation her temperature is 101.0°F (38.3°C), blood pressure is 113/75 mmHg, pulse is 105/min, and respirations are 12/min. On physical exam she is found to have tenderness over the lower abdominal quadrants, and speculum exam shows uterine inflammation as well as a retained intrauterine device. The most likely cause of this patient's symptoms should be treated with an antibiotic with which mechanism of action?
- A. Folic acid synthesis inhibitor
- B. Protein synthesis inhibitor (Correct Answer)
- C. RNA synthesis inhibitor
- D. Cell wall synthesis inhibitor
- E. DNA synthesis inhibitor
Penicillins and beta-lactamase inhibitors Explanation: ***Protein synthesis inhibitor***
- This patient's presentation (fever, chills, abdominal pain, increased vaginal discharge, uterine inflammation, and retained IUD) is highly suggestive of **Pelvic Inflammatory Disease (PID)**.
- The question specifically asks about treating **"the most likely cause"** of PID, which is ***Chlamydia trachomatis*** - the most common causative organism, particularly in young women with IUDs.
- **Doxycycline**, a **protein synthesis inhibitor** (tetracycline class - binds 30S ribosomal subunit), is the antibiotic of choice for *Chlamydia trachomatis* and is a **mandatory component** of all CDC-recommended PID treatment regimens.
- Standard outpatient PID treatment includes ceftriaxone (for gonorrhea) **plus** doxycycline (for chlamydia), with optional metronidazole for anaerobic coverage.
*Folic acid synthesis inhibitor*
- This class includes **sulfonamides** and **trimethoprim**, which inhibit bacterial folate synthesis.
- These agents are primarily used for urinary tract infections, *Pneumocystis jirovecii* pneumonia, and toxoplasmosis.
- They are **not first-line agents** for PID and do not adequately cover *Chlamydia trachomatis*, the most common cause.
*RNA synthesis inhibitor*
- **Rifamycins** (such as rifampin and rifabutin) inhibit bacterial DNA-dependent RNA polymerase.
- These antibiotics are primarily used for **tuberculosis**, atypical mycobacterial infections, and prophylaxis for meningococcal or *H. influenzae* exposure.
- They have **no role** in the treatment of PID or chlamydial infections.
*Cell wall synthesis inhibitor*
- **Ceftriaxone**, a third-generation cephalosporin and beta-lactam antibiotic, is indeed a key component of PID treatment regimens.
- However, ceftriaxone primarily targets ***Neisseria gonorrhoeae***, not *Chlamydia trachomatis* (the most common cause).
- *Chlamydia* is an **intracellular organism without peptidoglycan** in its cell wall, making beta-lactams ineffective against it.
- While ceftriaxone is used in PID treatment, it does **not treat the most likely causative organism** specified in the question.
*DNA synthesis inhibitor*
- **Metronidazole** and **quinolones** are DNA synthesis inhibitors that disrupt bacterial DNA replication.
- Metronidazole is often added to PID regimens to provide **anaerobic coverage**, particularly for *Bacteroides* species and other anaerobes associated with bacterial vaginosis.
- However, metronidazole has **no activity against *Chlamydia trachomatis***, the most common cause of PID.
- Quinolones are no longer recommended for PID due to increasing resistance in *N. gonorrhoeae*.
Penicillins and beta-lactamase inhibitors US Medical PG Question 9: A hospitalized 45-year-old man has had mild flank pain since awakening 3 hours ago. He also reports a new generalized rash. Two weeks ago, he was diagnosed with pulmonary tuberculosis. Current medications include isoniazid, pyrazinamide, rifampin, ethambutol, and pyridoxine. His temperature is 38.3°C (100.9°F), pulse is 74/min, and blood pressure is 128/72 mm Hg. Examination of the skin shows diffuse erythema with confluent papules. There is no costovertebral angle tenderness. Laboratory studies show:
Leukocyte count 9,800/mm3
Segmented neutrophils 59%
Bands 3%
Eosinophils 4%
Lymphocytes 29%
Monocytes 5%
Serum
Urea nitrogen 25 mg/dL
Creatinine 1.9 mg/dL
Urine
WBC 8–10/hpf
Eosinophils numerous
RBC 5–6/hpf
RBC casts negative
WBC casts numerous
In addition to intravenous fluid resuscitation, which of the following is the most appropriate next step in management?
- A. Perform renal biopsy
- B. Initiate hemodialysis
- C. Discontinue rifampin (Correct Answer)
- D. Perform serum protein electrophoresis
- E. Administer ciprofloxacin
Penicillins and beta-lactamase inhibitors Explanation: ***Discontinue rifampin***
- The patient presents with **fever**, **rash**, **eosinophilia**, and **acute kidney injury** with **eosinophiluria** and **WBC casts**, which are classic signs of **acute interstitial nephritis (AIN)**.
- Among the anti-tuberculosis medications, **rifampin** is the most common cause of drug-induced AIN, particularly when presenting with the classic triad of fever, rash, and acute kidney injury.
- Discontinuing the offending agent is the most critical initial step in management of drug-induced AIN.
*Perform renal biopsy*
- A renal biopsy is generally reserved for cases where the diagnosis of **acute interstitial nephritis (AIN)** is unclear, or if there is no improvement after discontinuing the suspected drug and initiating corticosteroids.
- Given the clear clinical picture and classic laboratory findings, the immediate priority is to remove the likely causative agent rather than perform an invasive procedure.
*Initiate hemodialysis*
- Hemodialysis is indicated for patients with severe **acute kidney injury (AKI)** evidenced by intractable electrolyte imbalances, severe fluid overload, or uremic symptoms.
- Though the patient has **elevated creatinine (1.9 mg/dL)**, there is no indication of immediately life-threatening complications that would warrant urgent dialysis at this stage.
*Perform serum protein electrophoresis*
- Serum protein electrophoresis is used to diagnose conditions like **multiple myeloma**, which can cause **kidney disease (myeloma kidney)**.
- The patient's presentation with **fever, rash, eosinophilia**, and **WBC casts** is inconsistent with myeloma kidney, making this investigation less relevant than addressing the suspected drug-induced AIN.
*Administer ciprofloxacin*
- The patient's symptoms are highly suggestive of **drug-induced acute interstitial nephritis (AIN)**, an allergic reaction, rather than an infection.
- There is no clinical or laboratory evidence (e.g., specific infectious markers) to support the use of an antibiotic like ciprofloxacin, which could potentially worsen kidney function or cause further drug interactions.
Penicillins and beta-lactamase inhibitors US Medical PG Question 10: An 8-year-old boy is brought to the emergency department by his parents because of sudden onset of abdominal pain beginning an hour ago. The parents report that their son has also had an episode of dark urine earlier that morning. Three days ago, he was diagnosed with a urinary tract infection and was treated with trimethoprim-sulfamethoxazole. He emigrated from Liberia to the US with his family 3 years ago. There is no personal history of serious illness. His immunizations are up-to-date. Vital signs are within normal limits. Examination shows diffuse abdominal tenderness and scleral icterus. The spleen is palpated 1–2 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10 g/dL
Mean corpuscular volume 90 μm3
Reticulocyte count 3%
Serum
Bilirubin
Total 3 mg/dL
Direct 0.5 mg/dL
Haptoglobin 20 mg/dL (N=41–165 mg/dL)
Lactate dehydrogenase 160 U/L
Urine
Blood 3+
Protein 1+
RBC 2–3/hpf
WBC 2–3/hpf
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Production of hemoglobin S
- B. Deficient glucose-6-phosphate dehydrogenase (Correct Answer)
- C. Lead poisoning
- D. Cold agglutinins
- E. Defective RBC membrane proteins
Penicillins and beta-lactamase inhibitors Explanation: ***Deficient glucose-6-phosphate dehydrogenase***
- The patient's presentation with **hemolytic anemia** (low hemoglobin, elevated reticulocytes, low haptoglobin, elevated LDH, elevated indirect bilirubin) following **trimethoprim-sulfamethoxazole** administration, along with dark urine (hemoglobinuria), is highly suggestive of G6PD deficiency.
- G6PD deficiency is common in individuals of African descent (patient emigrated from Liberia) and certain medications like sulfa drugs can trigger **oxidative stress** leading to hemolysis in affected individuals.
*Production of hemoglobin S*
- While **sickle cell anemia** (due to hemoglobin S) can cause hemolytic anemia and abdominal pain (**vaso-occlusive crisis**), the sudden onset linked to a specific medication and the absence of a prior history of serious illness make G6PD deficiency more likely.
- Sickle cell disease typically presents with recurrent painful crises, dactylitis in infancy, and chronic hemolytic anemia, which are not described here.
*Lead poisoning*
- **Lead poisoning** can cause abdominal pain and anemia, but it typically presents with a **microcytic hypochromic anemia** and **basophilic stippling** on peripheral smear.
- It does not directly cause an acute hemolytic crisis triggered by trimethoprim-sulfamethoxazole.
*Cold agglutinins*
- **Cold agglutinin disease** involves hemolytic anemia triggered by cold exposure, and the antibodies react optimally at cold temperatures.
- The patient's symptoms are acute and triggered by a medication known to induce oxidative stress, which is not characteristic of cold agglutinin disease.
*Defective RBC membrane proteins*
- **Hereditary spherocytosis** (a defect in RBC membrane proteins like spectrin or ankyrin) causes chronic hemolytic anemia and splenomegaly.
- While it can manifest with jaundice, it typically does not cause an acute, drug-induced hemolytic crisis with hemoglobinuria as seen here.
More Penicillins and beta-lactamase inhibitors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.