Macrolides, ketolides, and lincosamides US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Macrolides, ketolides, and lincosamides. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Macrolides, ketolides, and lincosamides US Medical PG Question 1: A 60-year-old man with a history of coronary artery disease and hyperlipidemia presents to his internist for a follow-up visit 3 weeks after visiting an urgent care center for symptoms of cough, fever, and difficulty breathing. He had been prescribed erythromycin in addition to his usual regimen of rosuvastatin and aspirin. With which potential side effect or interaction should the internist be most concerned?
- A. Myalgia due to decreased rosuvastatin metabolism in the presence of erythromycin (Correct Answer)
- B. Gastric bleeding due to decreased aspirin metabolism in the presence of erythromycin
- C. Unstable angina due to decreased rosuvastatin metabolism in the presence of erythromycin
- D. Tinnitus due to decreased aspirin metabolism in the presence of erythromycin
- E. Metabolic acidosis due to decreased aspirin metabolism in the presence of erythromycin
Macrolides, ketolides, and lincosamides Explanation: ***Myalgia due to decreased rosuvastatin metabolism in the presence of erythromycin***
- **Rosuvastatin** is metabolized by **CYP3A4** to a lesser extent, but it's also a substrate for **organic anion transporting polypeptide (OATP) 1B1**. **Erythromycin** is a potent **CYP3A4 inhibitor** and can also inhibit **OATP1B1**.
- Inhibition of rosuvastatin metabolism/transport by erythromycin can lead to increased serum concentrations of rosuvastatin, increasing the risk of **statin-induced myopathy** and **rhabdomyolysis**, a severe adverse effect characterized by **myalgia**.
*Gastric bleeding due to decreased aspirin metabolism in the presence of erythromycin*
- **Aspirin's metabolism** is primarily through hydrolysis to salicylic acid; erythromycin does not significantly affect this pathway.
- Gastric bleeding with aspirin is related to its **antiplatelet effects** and direct gastrointestinal irritation, not typically altered metabolism by erythromycin.
*Unstable angina due to decreased rosuvastatin metabolism in the presence of erythromycin*
- While **rosuvastatin levels** might increase, leading to myalgia, this interaction does not directly cause **unstable angina**.
- Unstable angina is a cardiac event related to **coronary artery disease progression** or plaque rupture, not typically a direct drug-drug interaction with erythromycin and rosuvastatin.
*Tinnitus due to decreased aspirin metabolism in the presence of erythromycin*
- **Tinnitus** is a known side effect of **aspirin toxicity**, particularly at high doses (salicylism).
- Erythromycin does not significantly alter aspirin metabolism in a way that would lead to increased aspirin levels and associated tinnitus.
*Metabolic acidosis due to decreased aspirin metabolism in the presence of erythromycin*
- **Metabolic acidosis** can occur with **high-dose aspirin poisoning** (salicylate poisoning).
- There is no known direct interaction between erythromycin and aspirin metabolism that would lead to clinically significant changes in aspirin levels sufficient to cause metabolic acidosis.
Macrolides, ketolides, and lincosamides US Medical PG Question 2: An 8-year-old girl is brought to the emergency room for a 6-hour history of fever, sore throat, and difficulty swallowing. Physical examination shows pooling of oral secretions and inspiratory stridor. Lateral x-ray of the neck shows thickening of the epiglottis and aryepiglottic folds. Throat culture with chocolate agar shows small, gram-negative coccobacilli. The patient's brother is started on the recommended antibiotic for chemoprophylaxis. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of the 50S ribosomal subunit
- B. Inhibition of prokaryotic topoisomerase II
- C. Inhibition of DNA-dependent RNA-polymerase (Correct Answer)
- D. Inhibition of the 30S ribosomal subunit
- E. Inhibition of peptidoglycan crosslinking
Macrolides, ketolides, and lincosamides Explanation: ***Inhibition of DNA-dependent RNA-polymerase***
- The clinical picture strongly suggests **epiglottitis** caused by *Haemophilus influenzae type b* (Hib), characterized by **fever, sore throat, difficulty swallowing, pooling of oral secretions, inspiratory stridor**, and **epiglottic thickening** on X-ray.
- **Rifampin** is the recommended antibiotic for chemoprophylaxis in close contacts of Hib patients; its primary mechanism of action is to inhibit bacterial **DNA-dependent RNA polymerase**, thereby preventing **mRNA synthesis**.
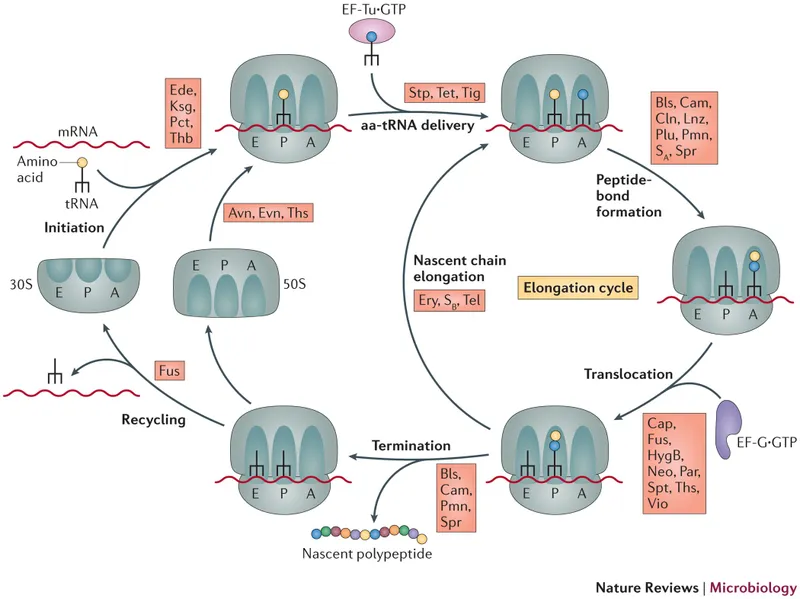
*Inhibition of the 50S ribosomal subunit*
- This mechanism is characteristic of **macrolides** (e.g., azithromycin, erythromycin) and **clindamycin**, which are not the primary choice for Hib chemoprophylaxis.
- These drugs prevent **protein synthesis** by interfering with translocation or peptide bond formation on the larger ribosomal subunit.
*Inhibition of prokaryotic topoisomerase II*
- This is the mechanism of action for **fluoroquinolones** (e.g., ciprofloxacin), which are typically reserved for specific infections due to potential side effects in children.
- Fluoroquinolones interfere with **DNA replication** and **transcription** by preventing DNA unwinding and supercoiling.
*Inhibition of the 30S ribosomal subunit*
- This mechanism is associated with **tetracyclines** and **aminoglycosides** (e.g., doxycycline, gentamicin).
- These antibiotics block **protein synthesis** by preventing tRNA attachment or causing misreading of mRNA.
*Inhibition of peptidoglycan crosslinking*
- This describes the mechanism of **beta-lactam antibiotics** (e.g., penicillin, amoxicillin, cephalosporins), which inhibit bacterial **cell wall synthesis**.
- While some beta-lactams are used to treat Hib infections, they are not the primary drug for **chemoprophylaxis**.
Macrolides, ketolides, and lincosamides US Medical PG Question 3: A 68-year-old man comes to the physician because of headache, fatigue, and nonproductive cough for 1 week. He appears pale. Pulmonary examination shows no abnormalities. Laboratory studies show a hemoglobin concentration of 9.5 g/dL and an elevated serum lactate dehydrogenase concentration. A peripheral blood smear shows normal red blood cells that are clumped together. Results of cold agglutinin titer testing show a 4-fold elevation above normal. An x-ray of the chest shows diffuse, patchy infiltrates bilaterally. Treatment is begun with an antibiotic that is also used to promote gut motility. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of bacterial RNA polymerase
- B. Inhibition of folic acid synthesis
- C. Free radical creation within bacterial cells
- D. Inhibition of transpeptidase cross-linking at the cell wall
- E. Inhibition of peptide translocation at the 50S ribosomal subunit (Correct Answer)
Macrolides, ketolides, and lincosamides Explanation: ***Inhibition of peptide translocation at the 50S ribosomal subunit***
- This drug described is likely **erythromycin** or another **macrolide antibiotic**, which inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit** and preventing translocation.
- Macrolides are used to treat **atypical pneumonia** caused by *Mycoplasma pneumoniae*, which is indicated by the patient's symptoms (headache, fatigue, nonproductive cough, bilateral patchy infiltrates) and **cold agglutinin disease**.
*Inhibition of bacterial RNA polymerase*
- This is the mechanism of action of **rifampin**, which is primarily used for **tuberculosis** and **meningitis prophylaxis**, not for atypical pneumonia.
- Rifampin's side effects and spectrum of activity do not align with the implied clinical scenario, especially the gut motility promotion.
*Inhibition of folic acid synthesis*
- This is the mechanism for **sulfonamides** and **trimethoprim**, which are bacteriostatic and target different pathogens than those causing cold agglutinin positive pneumonia.
- These drugs are not known for promoting gut motility.
*Free radical creation within bacterial cells*
- This mechanism is characteristic of **metronidazole**, an antibiotic used for anaerobic bacterial and parasitic infections.
- Metronidazole does not fit the clinical context of atypical pneumonia with cold agglutinins, nor is it a macrolide that promotes gut motility.
*Inhibition of transpeptidase cross-linking at the cell wall*
- This describes the mechanism of **beta-lactam antibiotics** (e.g., penicillins, cephalosporins), which are ineffective against **atypical pneumonia** because *Mycoplasma* lacks a cell wall.
- Beta-lactams do not typically promote gut motility.
Macrolides, ketolides, and lincosamides US Medical PG Question 4: A 58-year-old man comes to the physician because of severe muscle aches and fatigue for 3 days. Last week he was diagnosed with atypical pneumonia and treated with clarithromycin. He has hyperlipidemia for which he takes lovastatin. Physical examination shows generalized tenderness of the proximal muscles in the upper and lower extremities. Serum studies show an elevated creatine kinase concentration. This patient's current symptoms are most likely caused by inhibition of which of the following hepatic enzymes?
- A. CYP2E1
- B. CYP3A4 (Correct Answer)
- C. CYP2C9
- D. CYP1A2
- E. CYP2C19
Macrolides, ketolides, and lincosamides Explanation: ***CYP3A4***
- The patient is taking **lovastatin**, which is metabolized by **CYP3A4**. **Clarithromycin** is a potent **CYP3A4 inhibitor**.
- Inhibition of **CYP3A4** by clarithromycin leads to increased lovastatin levels, causing statin-induced **myopathy** (muscle aches, fatigue, and elevated creatine kinase).
*CYP2E1*
- This enzyme is primarily involved in the metabolism of compounds like **ethanol** and **acetaminophen**, not lovastatin.
- Its inhibition would not explain the interaction between clarithromycin and lovastatin.
*CYP2C9*
- This enzyme metabolizes drugs such as **warfarin** and **NSAIDs**, but it is not the primary enzyme responsible for lovastatin metabolism or its interaction with clarithromycin.
- Inhibition of **CYP2C9** would not lead to the described myopathy in this context.
*CYP1A2*
- **CYP1A2** is involved in the metabolism of drugs like **caffeine** and **theophylline**.
- It does not play a significant role in the metabolism of lovastatin, and its inhibition would not cause the observed symptoms.
*CYP2C19*
- **CYP2C19** metabolizes drugs such as **clopidogrel** and **omeprazole**.
- It is not the target enzyme for the interaction between lovastatin and clarithromycin.
Macrolides, ketolides, and lincosamides US Medical PG Question 5: A pharmaceutical company has modified one of its existing antibiotics to have an improved toxicity profile. The new antibiotic blocks protein synthesis by first entering the cell and then binding to active ribosomes. The antibiotic mimics the structure of aminoacyl-tRNA. The drug is covalently bonded to the existing growing peptide chain via peptidyl transferase, thereby impairing the rest of protein synthesis and leading to early polypeptide truncation. Where is the most likely site that this process occurs?
- A. E site
- B. 30S small subunit
- C. A site (Correct Answer)
- D. 40S small subunit
- E. P site
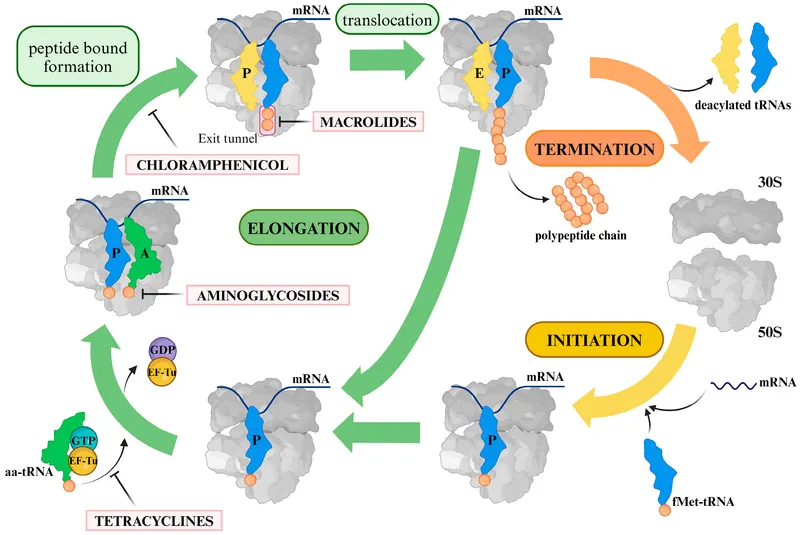
Macrolides, ketolides, and lincosamides Explanation: ***A site***
- The **A (aminoacyl) site** is where incoming aminoacyl-tRNAs bind during translation, bringing new amino acids to the ribosome. Since the antibiotic mimics **aminoacyl-tRNA** and is covalently bonded to the peptide chain by **peptidyl transferase**, its action must occur at the A site.
- Binding at the A site and subsequent peptide bond formation with the antibiotic would lead to premature polypeptide truncation, as no further amino acids can be added.
*E site*
- The **E (exit) site** is where deacylated tRNAs are released from the ribosome after having delivered their amino acid to the growing peptide chain in the P site.
- The antibiotic's mechanism of action, involving binding and covalent incorporation into the peptide, does not align with the function of the E site.
*30S small subunit*
- The **30S small ribosomal subunit** in prokaryotes is primarily involved in mRNA binding and decoding, ensuring the correct aminoacyl-tRNA binds to the mRNA codon.
- While the antibiotic binds to active ribosomes, its key action described as mimicking aminoacyl-tRNA and being incorporated by peptidyl transferase points to a specific binding site within the ribosome rather than the entire subunit's general function.
*40S small subunit*
- The **40S small ribosomal subunit** is found in **eukaryotic ribosomes**, not prokaryotic ones, and is involved in mRNA binding during initiation.
- The question implies an antibiotic targeting bacterial protein synthesis (given its discussion of modifying an existing antibiotic), making eukaryotic ribosomal subunits an unlikely target.
*P site*
- The **P (peptidyl) site** holds the tRNA carrying the growing polypeptide chain. Peptidyl transferase activity forms a peptide bond between the amino acid in the A site and the peptide in the P site.
- While peptidyl transferase is involved, the antibiotic *mimics* aminoacyl-tRNA, which is delivered to the A site for peptide bond formation, rather than the P site which already holds the growing chain.
Macrolides, ketolides, and lincosamides US Medical PG Question 6: An 18-year old college freshman presents to his university clinic because he has not been feeling well for the past two weeks. He has had a persistent headache, occasional cough, and chills without rigors. The patient’s vital signs are normal and physical exam is unremarkable. His radiograph shows patchy interstitial lung infiltrates and he is diagnosed with atypical pneumonia. The patient is prescribed azithromycin and takes his medication as instructed. Despite adherence to his drug regimen, he returns to the clinic one week later because his symptoms have not improved. The organism responsible for this infection is likely resistant to azithromycin through which mechanism?
- A. Mutation in topoisomerase II
- B. Methylation of ribosomal binding site
- C. Presence of a beta-lactamase
- D. Decreased binding to RNA polymerase
- E. Insertion of drug efflux pumps (Correct Answer)
Macrolides, ketolides, and lincosamides Explanation: ***Insertion of drug efflux pumps***
- **Azithromycin** is a macrolide antibiotic that inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit**.
- In **Mycoplasma pneumoniae** (the most common cause of atypical pneumonia in young adults), the **most common** mechanism of macrolide resistance is through **efflux pumps**, particularly the **mef genes**.
- These efflux pumps actively transport macrolides out of the bacterial cell, reducing intracellular drug concentration and conferring resistance.
- This mechanism is responsible for the majority of macrolide-resistant *M. pneumoniae* isolates worldwide.
*Methylation of ribosomal binding site*
- **Methylation** of the ribosomal binding site (specifically the **23S rRNA** via erm genes) does prevent azithromycin from binding effectively.
- While this is a valid macrolide resistance mechanism seen in organisms like *Streptococcus pneumoniae* and *Streptococcus pyogenes*, it is **less common** in *Mycoplasma pneumoniae*.
- Efflux pumps (mef) are the predominant mechanism in *M. pneumoniae* resistant strains.
*Mutation in topoisomerase II*
- **Topoisomerase II** (DNA gyrase) is the target of **fluoroquinolone antibiotics**, not macrolides.
- Mutations in this enzyme lead to resistance against fluoroquinolones, such as **ciprofloxacin**.
*Presence of a beta-lactamase*
- **Beta-lactamase enzymes** inactivate **beta-lactam antibiotics** (e.g., penicillin, cephalosporins) by hydrolyzing their beta-lactam ring.
- Additionally, *Mycoplasma pneumoniae* **lacks a cell wall**, making it inherently resistant to all beta-lactam antibiotics regardless of beta-lactamase production.
*Decreased binding to RNA polymerase*
- **RNA polymerase** is the target for antibiotics like **rifampin**, which inhibits bacterial transcription.
- Decreased binding to RNA polymerase would lead to rifampin resistance, not azithromycin resistance.
Macrolides, ketolides, and lincosamides US Medical PG Question 7: A 47-year-old man comes to the physician because of abdominal pain and foul-smelling, watery diarrhea for several days. He has not had nausea, vomiting, or blood in the stool. He has a history of alcohol use disorder and recently completed a 7-day course of clindamycin for pneumonia. He has not traveled out of the United States. Which of the following toxins is most likely to be involved in the pathogenesis of this patient's symptoms?
- A. Cereulide toxin
- B. Cholera toxin
- C. Clostridioides difficile cytotoxin (Correct Answer)
- D. Shiga toxin
- E. Alpha toxin
Macrolides, ketolides, and lincosamides Explanation: ***Clostridioides difficile cytotoxin***
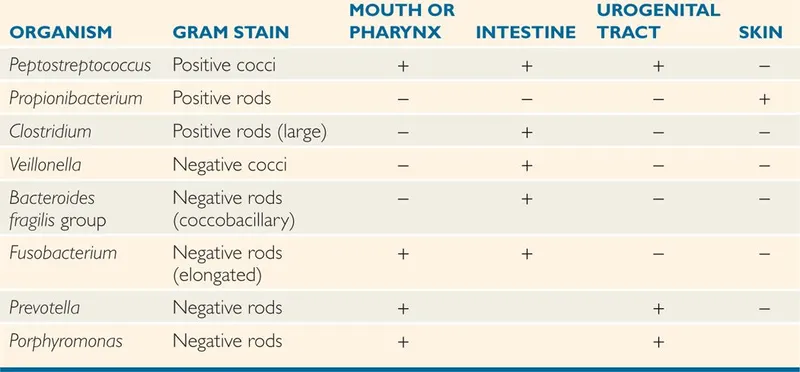
- The patient's history of recent **clindamycin** use, followed by **abdominal pain** and **foul-smelling, watery diarrhea**, is highly suggestive of *Clostridioides difficile* infection.
- *C. difficile* produces **cytotoxin (TcdB)** and **enterotoxin (TcdA)**, which lead to colitis and diarrhea, often after antimicrobial therapy.
*Cereulide toxin*
- This preformed toxin is produced by *Bacillus cereus* and typically causes a **short-incubation** emetic type of food poisoning, characterized by **nausea and vomiting**.
- The patient's symptoms are primarily diarrhea, and nausea/vomiting are absent, making this less likely.
*Cholera toxin*
- Produced by *Vibrio cholerae*, this toxin causes profuse, **"rice-water" diarrhea** with rapid dehydration.
- The patient has not traveled to endemic areas, and there is no mention of the characteristic severe dehydration or "rice-water" stool.
*Shiga toxin*
- This toxin, produced by *Shigella dysenteriae* and enterohemorrhagic *E. coli* (EHEC), typically causes **bloody diarrhea** and can lead to **hemolytic uremic syndrome (HUS)**.
- The patient's diarrhea is watery and explicitly stated to be without blood, ruling out Shiga toxin as the cause.
*Alpha toxin*
- This toxin is produced by *Clostridium perfringens* and is primarily associated with **gas gangrene** (myonecrosis) and some forms of food poisoning.
- While *C. perfringens* can cause diarrhea, it's typically mild and self-limiting, and the clinical picture in this patient, especially with recent antibiotic use, points more strongly to *C. difficile*.
Macrolides, ketolides, and lincosamides US Medical PG Question 8: A 61-year-old woman who recently emigrated from India comes to the physician because of a 2-month history of fever, fatigue, night sweats, and a productive cough. She has had a 5-kg (11-lb) weight loss during this period. She has a history of type 2 diabetes mellitus and poorly controlled asthma. She has had multiple asthma exacerbations in the past year that were treated with glucocorticoids. An x-ray of the chest shows a cavitary lesion of the posterior apical segment of the left upper lobe with consolidation of the surrounding parenchyma. The pathogen identified on sputum culture is found to be resistant to multiple drugs, including streptomycin. Which of the following mechanisms is most likely involved in bacterial resistance to this drug?
- A. Alteration in the sequence of gyrA genes
- B. Upregulation of arabinosyl transferase production
- C. Upregulation of mycolic acid synthesis
- D. Alteration in 30S ribosomal subunit (Correct Answer)
- E. Inhibition of bacterial synthesis of RNA
Macrolides, ketolides, and lincosamides Explanation: ***Alteration in 30S ribosomal subunit***
- Streptomycin is an **aminoglycoside antibiotic** that acts by binding to the **16S rRNA of the 30S ribosomal subunit**, which interferes with bacterial protein synthesis.
- **Resistance to streptomycin** most commonly arises from mutations in the genes encoding ribosomal proteins (e.g., *rpsL*) or the 16S rRNA that alter the drug's binding site on the 30S ribosomal subunit, preventing its inhibitory effect.
*Alteration in the sequence of gyrA genes*
- Mutations in the *gyrA* gene typically confer resistance to **fluoroquinolone antibiotics**, such as ciprofloxacin and levofloxacin.
- Fluoroquinolones target **DNA gyrase (topoisomerase II)**, which is encoded by *gyrA*, not the ribosomes.
*Upregulation of arabinosyl transferase production*
- **Arabinogalactan**, a major component of the mycobacterial cell wall, is synthesized by **arabinosyl transferases** (e.g., EmbB).
- Resistance to **ethambutol** is often associated with mutations or upregulation of these enzymes, leading to increased synthesis of the arabinogalactan layer.
*Upregulation of mycolic acid synthesis*
- **Mycolic acid** is a crucial component of the mycobacterial cell wall, and its synthesis is inhibited by drugs like **isoniazid**.
- Upregulation of mycolic acid synthesis or mutations in genes related to its production (e.g., *kasA*) can lead to **isoniazid resistance**, but not directly to streptomycin resistance.
*Inhibition of bacterial synthesis of RNA*
- **Rifampin** is an antibiotic that inhibits bacterial RNA synthesis by binding to the **DNA-dependent RNA polymerase**.
- While resistance to rifampin often involves mutations in the *rpoB* gene, this mechanism is specific to rifampin and not streptomycin.
Macrolides, ketolides, and lincosamides US Medical PG Question 9: Six days after undergoing an elective hip replacement surgery, a 79-year-old man develops dysuria, flank pain, and fever. His temperature is 38.5°C (101.3°F). Examination shows marked tenderness in the right costovertebral area. Treatment with an antibiotic is begun, but his symptoms do not improve. Further evaluation shows that the causal organism produces an enzyme that inactivates the antibiotic via phosphorylation. An agent from which of the following classes of antibiotics was most likely administered?
- A. Macrolides
- B. Tetracyclines
- C. Aminoglycosides (Correct Answer)
- D. Glycopeptides
- E. Fluoroquinolones
Macrolides, ketolides, and lincosamides Explanation: ***Aminoglycosides***
- **Aminoglycosides** are commonly inactivated by bacterial enzymes through **phosphorylation**, acetylation, or adenylation, leading to resistance.
- The patient's lack of improvement despite antibiotic treatment and the mechanism of inactivation point towards this class of antibiotics.
*Macrolides*
- **Macrolide resistance** typically involves mechanisms such as modification of the ribosomal binding site (e.g., methylation), drug efflux pumps, or enzymatic inactivation by esterases, not phosphorylation.
- While macrolides can treat various infections, their inactivation mechanism is different from what is described.
*Tetracyclines*
- **Tetracycline resistance** is primarily mediated by bacterial efflux pumps that actively transport the antibiotic out of the cell, or by ribosomal protection proteins that interfere with drug binding.
- **Enzymatic inactivation via phosphorylation** is not a characteristic resistance mechanism for tetracyclines.
*Glycopeptides*
- **Glycopeptide resistance**, particularly to vancomycin, is mainly associated with alterations in the cell wall precursor target (e.g., D-Ala-D-Lac modification), which prevents the antibiotic from binding.
- This mechanism is distinct from enzymatic phosphorylation of the antibiotic molecule itself.
*Fluoroquinolones*
- **Fluoroquinolone resistance** primarily arises from mutations in the genes encoding bacterial DNA gyrase and topoisomerase IV, or via efflux pumps.
- There is no significant mechanism of resistance involving direct enzymatic phosphorylation of fluoroquinolone drugs.
Macrolides, ketolides, and lincosamides US Medical PG Question 10: A 54-year-old man with a past medical history significant for hypertension, type 2 diabetes, and chronic obstructive pulmonary disease presents with complaints of nausea and abdominal pain for the past month. The pain is located in the epigastric region and is described as “burning” in quality, often following food intake. The patient denies any changes in bowel movements, fever, or significant weight loss. Medications include metformin, lisinopril, hydrochlorothiazide, albuterol inhaler, and fluconazole for a recent fungal infection. Physical examination was unremarkable except for a mildly distended abdomen that is diffusely tender to palpation and decreased sensation at lower extremities bilaterally. A medication was started for the symptoms. Two days later, the patient reports heart palpitations. An EKG is shown below. Which of the following is the medication most likely prescribed?
- A. Aspirin
- B. Metformin
- C. Omeprazole
- D. Ranitidine
- E. Erythromycin (Correct Answer)
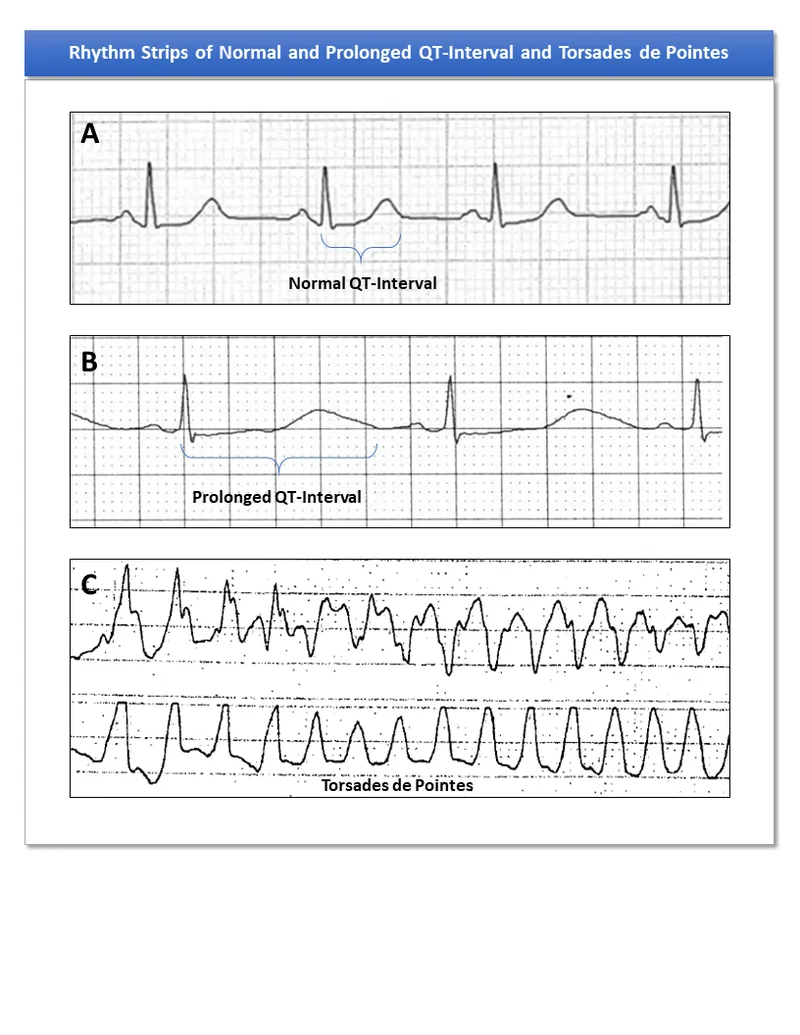
Macrolides, ketolides, and lincosamides Explanation: ***Erythromycin***
- The EKG shows **QT prolongation** (long QT interval), which can lead to **torsades de pointes** and palpitations. Erythromycin is a macrolide antibiotic known to cause QT prolongation.
- **Critical drug interaction:** The patient is taking **fluconazole**, a strong **CYP3A4 inhibitor**, which increases erythromycin levels (a CYP3A4 substrate), significantly enhancing the risk of QT prolongation and cardiac arrhythmias.
- Given the patient's complaints of burning epigastric pain following food intake and diabetic neuropathy, a diagnosis of **diabetic gastroparesis** is suggested. Erythromycin can be used as a **prokinetic agent** for gastroparesis due to its agonistic effect on motilin receptors, thus explaining its prescription.
*Aspirin*
- Aspirin is a **non-steroidal anti-inflammatory drug (NSAID)** and an antiplatelet agent. While it can cause epigastric pain and is often used in cardiovascular disease patients, it does not typically cause QT prolongation or palpitations.
- It is unlikely to be prescribed for the patient's symptoms of nausea and burning epigastric pain, as it can **exacerbate gastric irritation**.
*Metformin*
- Metformin is an oral hypoglycemic agent already listed in the patient's current medication list and used for type 2 diabetes. Its primary side effects relate to **gastrointestinal upset** (e.g., nausea, diarrhea) but it doesn't cause QT prolongation.
- The question implies a *new* medication was started, and metformin is an existing medication *for diabetes*, not specifically for the new burning epigastric pain.
*Omeprazole*
- Omeprazole is a **proton pump inhibitor (PPI)** commonly prescribed for acid reflux and peptic ulcer disease, which might align with the burning epigastric pain.
- However, PPIs are generally not associated with **QT prolongation** or palpitations.
*Ranitidine*
- Ranitidine is an **H2 receptor antagonist** used to reduce stomach acid, similar to omeprazole, and could be prescribed for the epigastric pain.
- Like omeprazole, ranitidine is not known to cause **QT prolongation** or cardiac arrhythmias like palpitations.
More Macrolides, ketolides, and lincosamides US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.