Fluoroquinolones US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fluoroquinolones. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fluoroquinolones US Medical PG Question 1: A 64-year-old woman with a past medical history of poorly managed diabetes presents to the emergency department with nausea and vomiting. Her symptoms started yesterday and have been progressively worsening. She is unable to eat given her symptoms. Her temperature is 102°F (38.9°C), blood pressure is 115/68 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for left-sided costovertebral angle tenderness, and urinalysis demonstrates bacteriuria and pyuria. The patient is admitted to the hospital and started on IV ceftriaxone. On day 3 of her hospital stay she is afebrile, able to eat and drink, and feels better. Which of the following antibiotic regimens should be started or continued as an outpatient upon discharge?
- A. Amoxicillin
- B. Nitrofurantoin
- C. Ciprofloxacin
- D. Ceftriaxone
- E. Trimethoprim-sulfamethoxazole (Correct Answer)
Fluoroquinolones Explanation: ***Trimethoprim-sulfamethoxazole***
- This patient presents with **acute pyelonephritis**, indicated by fever, CVA tenderness, bacteriuria, and pyuria, requiring a 7-14 day course of treatment.
- After 3 days of IV ceftriaxone with clinical improvement, **step-down to oral therapy** is appropriate.
- **Trimethoprim-sulfamethoxazole** is a first-line oral agent for completing treatment of uncomplicated pyelonephritis and is preferred when **local resistance rates are <20%** and no specific resistance data is available.
- It achieves adequate concentrations in renal tissue and is cost-effective for outpatient therapy.
*Amoxicillin*
- **Amoxicillin** is not recommended for pyelonephritis due to **high resistance rates** among common uropathogens like *E. coli* (often >30%).
- It does not achieve adequate concentrations in the renal parenchyma to effectively treat **upper urinary tract infections**.
*Nitrofurantoin*
- **Nitrofurantoin** is concentrated in the bladder and is highly effective for **lower urinary tract infections (cystitis)**.
- It is **contraindicated for pyelonephritis** because it does not reach therapeutic levels in the renal parenchyma or bloodstream.
- Additionally, it should be avoided in patients with impaired renal function.
*Ciprofloxacin*
- **Ciprofloxacin** is also a first-line oral agent for pyelonephritis and would be an appropriate choice for step-down therapy.
- However, when no culture or susceptibility data is available, **TMP-SMX is generally preferred** as an initial oral choice due to concerns about promoting fluoroquinolone resistance and potential adverse effects (tendonitis, QT prolongation, C. difficile).
- Fluoroquinolones are particularly valuable when reserved for cases with known resistance to other agents or specific patient contraindications.
*Ceftriaxone*
- **Ceftriaxone** is an IV third-generation cephalosporin used for initial empiric treatment of acute pyelonephritis in hospitalized patients.
- Once the patient is **clinically stable, afebrile, and tolerating oral intake**, transitioning to oral therapy is standard practice.
- Continued IV therapy as an outpatient is unnecessarily invasive and costly when oral options are effective.
Fluoroquinolones US Medical PG Question 2: An 8-year-old girl is brought to the emergency room for a 6-hour history of fever, sore throat, and difficulty swallowing. Physical examination shows pooling of oral secretions and inspiratory stridor. Lateral x-ray of the neck shows thickening of the epiglottis and aryepiglottic folds. Throat culture with chocolate agar shows small, gram-negative coccobacilli. The patient's brother is started on the recommended antibiotic for chemoprophylaxis. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of the 50S ribosomal subunit
- B. Inhibition of prokaryotic topoisomerase II
- C. Inhibition of DNA-dependent RNA-polymerase (Correct Answer)
- D. Inhibition of the 30S ribosomal subunit
- E. Inhibition of peptidoglycan crosslinking
Fluoroquinolones Explanation: ***Inhibition of DNA-dependent RNA-polymerase***
- The clinical picture strongly suggests **epiglottitis** caused by *Haemophilus influenzae type b* (Hib), characterized by **fever, sore throat, difficulty swallowing, pooling of oral secretions, inspiratory stridor**, and **epiglottic thickening** on X-ray.
- **Rifampin** is the recommended antibiotic for chemoprophylaxis in close contacts of Hib patients; its primary mechanism of action is to inhibit bacterial **DNA-dependent RNA polymerase**, thereby preventing **mRNA synthesis**.
*Inhibition of the 50S ribosomal subunit*
- This mechanism is characteristic of **macrolides** (e.g., azithromycin, erythromycin) and **clindamycin**, which are not the primary choice for Hib chemoprophylaxis.
- These drugs prevent **protein synthesis** by interfering with translocation or peptide bond formation on the larger ribosomal subunit.
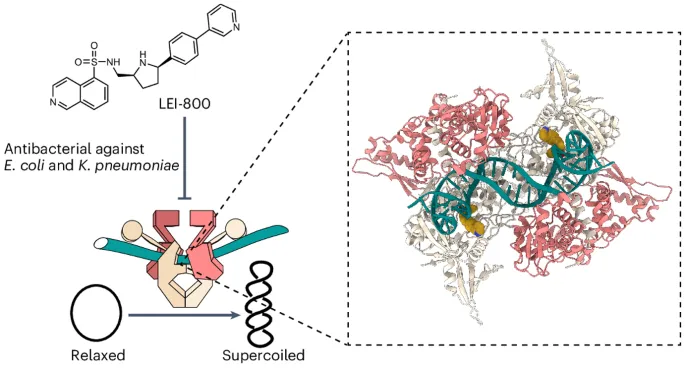
*Inhibition of prokaryotic topoisomerase II*
- This is the mechanism of action for **fluoroquinolones** (e.g., ciprofloxacin), which are typically reserved for specific infections due to potential side effects in children.
- Fluoroquinolones interfere with **DNA replication** and **transcription** by preventing DNA unwinding and supercoiling.
*Inhibition of the 30S ribosomal subunit*
- This mechanism is associated with **tetracyclines** and **aminoglycosides** (e.g., doxycycline, gentamicin).
- These antibiotics block **protein synthesis** by preventing tRNA attachment or causing misreading of mRNA.
*Inhibition of peptidoglycan crosslinking*
- This describes the mechanism of **beta-lactam antibiotics** (e.g., penicillin, amoxicillin, cephalosporins), which inhibit bacterial **cell wall synthesis**.
- While some beta-lactams are used to treat Hib infections, they are not the primary drug for **chemoprophylaxis**.
Fluoroquinolones US Medical PG Question 3: A 61-year-old woman is brought to the emergency department because of fever, chills, and flank pain for 8 hours. Her temperature is 39.1°C (102.4°F). Physical examination shows right costovertebral angle tenderness. Urine dipstick is positive for nitrites. Urinalysis shows gram-negative rods. The patient is admitted to the hospital and treatment with a drug that directly inhibits bacterial DNA replication is begun. This drug inhibits a protein that is normally responsible for which of the following steps of DNA replication?
- A. Excising RNA fragments in 5' to 3' direction
- B. Cleaving DNA to relieve supercoils (Correct Answer)
- C. Binding to single-stranded DNA to prevent reannealing
- D. Unwinding DNA at replication fork
- E. Joining of short DNA fragments
Fluoroquinolones Explanation: ***Cleaving DNA to relieve supercoils***
- The patient's symptoms (fever, chills, flank pain, CVA tenderness, nitrites in urine, gram-negative rods) are consistent with **pyelonephritis**, typically caused by **gram-negative bacteria**.
- The drug described is an **antibiotic** that inhibits bacterial **DNA replication**. This mechanism points towards **fluoroquinolones**, which inhibit **DNA gyrase (topoisomerase II)** and **topoisomerase IV**. These enzymes are responsible for **cleaving DNA** to relieve supercoils during replication and transcription.
*Excising RNA fragments in 5' to 3' direction*
- This function is primarily carried out by **DNA polymerase I** in prokaryotes, which removes **RNA primers** during replication.
- While essential for replication, it is not the direct target of antibiotics that inhibit overall bacterial DNA replication in the described scenario.
*Binding to single-stranded DNA to prevent reannealing*
- This role is performed by **single-stranded binding proteins (SSBs)**, which stabilize the separated DNA strands at the replication fork.
- These proteins are not typically targeted by antibiotics that inhibit DNA replication.
*Unwinding DNA at replication fork*
- The unwinding of DNA at the replication fork is primarily carried out by **DNA helicase**.
- While crucial for replication, antibiotics like fluoroquinolones target different enzymes involved in managing DNA topology.
*Joining of short DNA fragments*
- The joining of Okazaki fragments on the lagging strand is catalyzed by **DNA ligase**.
- This enzyme is not the primary target of antibiotics designed to broadly inhibit bacterial DNA replication by interfering with DNA gyrase or topoisomerase IV.
Fluoroquinolones US Medical PG Question 4: A 25-year-old woman has dysuria, pyuria, increased frequency of urination, and fever of 1-day duration. She is sexually active. Urine cultures show gram-positive bacteria in clusters that are catalase-positive and coagulase-negative. The patient is started on trimethoprim-sulfamethoxazole. Which of the following characteristics is used to identify the offending organism?
- A. Resistance to bacitracin
- B. Beta hemolysis
- C. Sensitivity to novobiocin
- D. Resistance to novobiocin (Correct Answer)
- E. Sensitivity to bacitracin
Fluoroquinolones Explanation: ***Resistance to novobiocin***
- The patient's symptoms (dysuria, pyuria, frequency, fever) and urine culture results (gram-positive cocci in clusters, catalase-positive, coagulase-negative) are highly suggestive of a **Staphylococcus saprophyticus** urinary tract infection (UTI).
- A key distinguishing characteristic of **Staphylococcus saprophyticus** from other coagulase-negative staphylococci (especially *Staphylococcus epidermidis*) is its **resistance to novobiocin**.
*Resistance to bacitracin*
- This characteristic is used to differentiate Group A Streptococcus (Streptococcus pyogenes), which is sensitive to bacitracin, from other beta-hemolytic streptococci.
- However, in this case, the organism is described as gram-positive cocci in clusters and catalase-positive, indicating Staphylococcus, not Streptococcus.
*Beta hemolysis*
- While beta hemolysis is a characteristic of certain bacteria, such as *Streptococcus pyogenes* or *Staphylococcus aureus*, it is not the primary diagnostic feature for the coagulase-negative, catalase-positive staphylococcus described here.
- Furthermore, *Staphylococcus saprophyticus* is typically non-hemolytic or weakly hemolytic.
*Sensitivity to novobiocin*
- **Sensitivity to novobiocin** is a characteristic of *Staphylococcus epidermidis* and other coagulase-negative staphylococci, but not *Staphylococcus saprophyticus*.
- Since the clinical picture points strongly to *Staphylococcus saprophyticus* in a young, sexually active female with a UTI, novobiocin resistance is the expected finding.
*Sensitivity to bacitracin*
- **Sensitivity to bacitracin** is a key characteristic used to identify *Streptococcus pyogenes* (Group A Strep).
- The organism in this scenario is a gram-positive cocci in clusters and catalase-positive, indicating a Staphylococcus species, not Streptococcus.
Fluoroquinolones US Medical PG Question 5: An experimental drug, ES 62, is being studied. It prohibits the growth of vancomycin-resistant Staphylococcus aureus. It is highly lipid-soluble. The experimental design is dependent on a certain plasma concentration of the drug. The target plasma concentration is 100 mmol/dL. Which of the following factors is most important for calculating the appropriate loading dose?
- A. Volume of distribution (Correct Answer)
- B. Half-life of the drug
- C. Therapeutic index
- D. Clearance of the drug
- E. Rate of administration
Fluoroquinolones Explanation: **Volume of distribution**
- The **loading dose** is primarily determined by the desired **plasma concentration** and the **volume of distribution (Vd)**, as it reflects how extensively a drug is distributed in the body.
- The formula for loading dose is: Loading Dose = (Target Plasma Concentration × Vd).
*Half-life of the drug*
- The **half-life** is crucial for determining the **dosing interval** and the time it takes to reach **steady-state concentrations**, not the initial loading dose.
- It reflects the rate at which the drug is eliminated from the body.
*Therapeutic index*
- The **therapeutic index** is a measure of a drug's relative safety, indicating the ratio between the **toxic dose** and the **effective dose**.
- While important for drug safety, it does not directly determine the magnitude of the loading dose itself.
*Clearance of the drug*
- **Clearance** is the rate at which the drug is removed from the body and is a primary determinant of the **maintenance dose** required to sustain a desired plasma concentration.
- It does not directly calculate the initial loading dose needed to achieve an immediate target concentration.
*Rate of administration*
- The **rate of administration** (e.g., infusion rate) primarily influences how quickly the drug reaches its target concentration, but not the total quantity of drug needed for the initial loading dose.
- It affects the kinetics of how the loading dose achieves the target concentration, rather than defining the dose amount.
Fluoroquinolones US Medical PG Question 6: A 62-year-old woman presents to her oncologist to discuss the chemotherapy options for her newly diagnosed breast cancer. During the meeting, they discuss a drug that inhibits the breakdown of mitotic spindles in cells. Her oncologist explains that this will be more toxic to cancer cells because those cells are dividing more rapidly. Which of the following side effects is closely associated with the use of this chemotherapeutic agent?
- A. Photosensitivity
- B. Peripheral neuropathy (Correct Answer)
- C. Paralytic ileus
- D. Hemorrhagic cystitis
- E. Pulmonary fibrosis
Fluoroquinolones Explanation: ***Peripheral neuropathy***
- Drugs that inhibit the breakdown of **mitotic spindles** are **microtubule-targeting agents** (e.g., **taxanes** like paclitaxel/docetaxel, **vinca alkaloids** like vincristine/vinblastine).
- These agents interfere with **microtubule function** in neurons, leading to **axonal damage** and **peripheral neuropathy**.
- This is the **most characteristic and common dose-limiting toxicity** of microtubule inhibitors, affecting sensory and motor nerves (numbness, tingling, weakness in extremities).
*Photosensitivity*
- **Photosensitivity** is a common adverse effect associated with certain chemotherapeutic agents like **fluorouracil** (5-FU) or **methotrexate**, but is not linked to microtubule inhibitors.
- It involves an increased sensitivity to UV light, often manifesting as a rash or exaggerated sunburn.
*Paralytic ileus*
- **Paralytic ileus** can occur with **vinca alkaloids** (especially vincristine) due to autonomic neuropathy affecting the **enteric nervous system**.
- However, this is **less common** than peripheral neuropathy and occurs more specifically with vincristine rather than taxanes.
- **Peripheral neuropathy** is the more pervasive, dose-limiting, and universally characteristic side effect across all microtubule inhibitors.
*Hemorrhagic cystitis*
- **Hemorrhagic cystitis** is a classic side effect of **alkylating agents** like **cyclophosphamide** and **ifosfamide**, which produce the toxic metabolite **acrolein**.
- It is prevented/managed with **mesna**, which inactivates acrolein.
- Not associated with microtubule inhibitors.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a known side effect of certain chemotherapeutic drugs, most notably **bleomycin** and **busulfan**.
- This adverse effect is not associated with agents that target **mitotic spindle breakdown**.
Fluoroquinolones US Medical PG Question 7: A 72-year-old patient presents to the emergency department because of abdominal pain, diarrhea, and fever. He was started on levofloxacin for community-acquired pneumonia 2 weeks prior with resolution of his pulmonary symptoms. He has had hypertension for 20 years, for which he takes amlodipine. His temperature is 38.3°C (101.0°F), pulse is 90/min, and blood pressure is 110/70 mm Hg. On examination, mild abdominal distension with minimal tenderness was found. Laboratory tests reveal a peripheral white blood cell count of 12.000/mm3 and a stool guaiac mildly positive for occult blood. Which of the following best describe the mechanism of this patient illness?
- A. Damage to the gastrointestinal tract by enteropathogenic viruses
- B. Autoimmune inflammation of the rectum
- C. Disruption of normal bowel flora and infection by spore-forming rods (Correct Answer)
- D. Decreased blood flow to the gastrointestinal tract
- E. Presence of osmotically active, poorly absorbed solutes in the bowel lumen
Fluoroquinolones Explanation: ***Disruption of normal bowel flora and infection by spore-forming rods***
- This describes **Clostridioides difficile infection (CDI)**, which is strongly suggested by the patient's recent antibiotic use (levofloxacin, a fluoroquinolone) followed by abdominal pain, diarrhea, fever, and leukocytosis.
- Antibiotics disrupt the normal gut microbiome, allowing **C. difficile (spore-forming rods)** to proliferate and produce toxins that cause colitis.
*Damage to the gastrointestinal tract by enteropathogenic viruses*
- While viral gastroenteritis can cause these symptoms, the **recent history of antibiotic use** makes CDI a much more likely diagnosis.
- Viral infections typically resolve spontaneously and are less likely to cause a significant **leukocytosis** and **occult blood in stool** in this context.
*Autoimmune inflammation of the rectum*
- Conditions like **ulcerative colitis**, an autoimmune disease, can cause similar symptoms but typically have a **chronic or relapsing course** and are not usually triggered by recent antibiotic use.
- The acute presentation following antibiotics strongly points away from an autoimmune process.
*Decreased blood flow to the gastrointestinal tract*
- **Ischemic colitis** can cause abdominal pain and bloody diarrhea, especially in older patients with vascular risk factors (like hypertension).
- However, the prominent **fever** and **leukocytosis**, coupled with recent antibiotic use, are more indicative of an infectious process like CDI than ischemia.
*Presence of osmotically active, poorly absorbed solutes in the bowel lumen*
- This mechanism describes **osmotic diarrhea**, which can be caused by malabsorption (e.g., lactose intolerance) or certain laxatives.
- Osmotic diarrhea typically **resolves with fasting** and is not usually associated with fever, significant leukocytosis, or occult blood in the stool, which are present here.
Fluoroquinolones US Medical PG Question 8: A 47-year-old woman presents to the physician with complaints of fatigue accompanied by symmetric pain, swelling, and stiffness in her wrists, fingers, knees, and other joints. She describes the stiffness as being particularly severe upon awakening, but gradually improves as she moves throughout her day. Her physician initially suggests that she take NSAIDs. However, after a few months of minimal symptomatic improvement, she is prescribed an immunosuppressive drug that has a mechanism of preventing IL-2 transcription. What is the main toxicity that the patient must be aware of with this particular class of drugs?
- A. Pancytopenia
- B. Osteoporosis
- C. Hepatotoxicity
- D. Nephrotoxicity (Correct Answer)
- E. Hyperglycemia
Fluoroquinolones Explanation: ***Nephrotoxicity***
- The drug described, which prevents **IL-2 transcription**, is likely a **calcineurin inhibitor** like cyclosporine or tacrolimus, often used in autoimmune diseases.
- **Nephrotoxicity** (kidney damage) is a major dose-limiting toxicity of calcineurin inhibitors, causing both acute and chronic kidney injury.
*Pancytopenia*
- While some immunosuppressants can cause **pancytopenia** (e.g., azathioprine, methotrexate), it is not the classic or primary toxicity associated with calcineurin inhibitors.
- Calcineurin inhibitors primarily affect **renal function** and can cause other side effects like hypertension or neurotoxicity.
*Osteoporosis*
- **Osteoporosis** is a known side effect of long-term glucocorticoid use, but not typically a primary toxicity of calcineurin inhibitors.
- Glucocorticoids reduce bone formation and increase bone resorption, leading to bone density loss.
*Hepatotoxicity*
- **Hepatotoxicity** (liver damage) can occur with various immunosuppressants, such as methotrexate, but it is not the most prominent or defining toxicity for calcineurin inhibitors.
- While cyclosporine can cause some liver enzyme elevation, **nephrotoxicity** is far more common and severe.
*Hyperglycemia*
- **Hyperglycemia** can be a side effect of some immunosuppressants, particularly **glucocorticoids** and **tacrolimus** (another calcineurin inhibitor).
- However, for the class of drugs that prevent IL-2 transcription (calcineurin inhibitors), **nephrotoxicity** remains the most significant and common major toxicity to be aware of.
Fluoroquinolones US Medical PG Question 9: A 15-year-old boy presents with his father to the urgent care with 5 days of frequent diarrhea, occasionally with streaks of blood mixed in. Stool cultures are pending, but preliminary stool samples demonstrate fecal leukocytes and erythrocytes. His vital signs are as follows: blood pressure is 126/83 mm Hg, heart rate is 97/min, and respiratory rate is 15/min. He is started on outpatient therapy for presumed Shigella infection. Which of the following is the most appropriate therapy?
- A. Oral doxycycline
- B. Oral vancomycin
- C. Oral TMP-SMX
- D. Oral azithromycin (Correct Answer)
- E. Oral ciprofloxacin
Fluoroquinolones Explanation: ***Oral azithromycin***
- **Azithromycin** is the **first-line empiric treatment** for suspected **Shigella infection** based on current CDC and WHO guidelines, particularly in pediatric and adolescent patients.
- The presence of **fecal leukocytes and erythrocytes** indicates an invasive bacterial infection, which warrants antibiotic therapy to shorten the course of illness and reduce transmission risks.
- Azithromycin has excellent efficacy against Shigella with relatively low resistance rates compared to older agents, and it is well-tolerated in adolescents.
*Oral TMP-SMX*
- **TMP-SMX (trimethoprim-sulfamethoxazole)** was historically first-line for Shigella, but **widespread resistance** (often >50% globally) has made it no longer recommended for empiric therapy.
- It may still be used if culture and susceptibility testing confirm sensitivity, but should not be chosen empirically.
*Oral ciprofloxacin*
- **Ciprofloxacin**, a fluoroquinolone, is highly effective against **Shigella** and is first-line in adults.
- However, its use in **pediatric patients under 18 years** is generally limited due to potential adverse effects on **cartilage development** and risk of tendinopathy.
- In a 15-year-old, while approaching adult age, azithromycin remains preferred unless there are specific contraindications.
*Oral doxycycline*
- **Doxycycline** has limited activity against **Shigella** and is not considered appropriate empiric therapy for this infection.
- It is more commonly used for atypical pathogens, certain sexually transmitted infections, or specific tick-borne diseases.
*Oral vancomycin*
- **Oral vancomycin** is primarily used to treat **Clostridioides difficile infection** (CDI) and is completely ineffective against **Shigella**.
- Vancomycin acts only on gram-positive bacteria and does not penetrate the systemic circulation when given orally, making it unsuitable for gram-negative enteric infections.
Fluoroquinolones US Medical PG Question 10: An 82-year-old man is brought to the emergency department because of severe pain and joint stiffness in his right knee. The pain started 3 days ago and has worsened despite acetaminophen intake. He has benign prostatic hyperplasia and hypertension. One week ago, he had a urinary tract infection and was treated with nitrofurantoin. He does not smoke or drink alcohol. His current medications include enalapril, hydrochlorothiazide, and tamsulosin. He appears to be in severe pain and has trouble moving his right knee. His temperature is 38.7°C (101.5°F), pulse is 92/min, and blood pressure is 135/90 mm Hg. Physical examination shows a swollen, erythematous, warm right knee; range of motion is limited by pain. Synovial fluid aspiration shows a yellow-green turbid fluid. Gram stain of the synovial aspirate shows numerous leukocytes and multiple gram-negative rods. An x-ray of the right knee shows no abnormalities. Which of the following is the most appropriate pharmacotherapy?
- A. IV ceftazidime and gentamicin
- B. IV cefepime (Correct Answer)
- C. IV vancomycin and ceftazidime
- D. IV vancomycin
- E. IV nafcillin
Fluoroquinolones Explanation: ***IV cefepime***
- This patient presents with **septic arthritis** due to **gram-negative rods**, likely originating from a recent **urinary tract infection** given his history of BPH. **Cefepime** is a **fourth-generation cephalosporin** with broad-spectrum activity against many gram-negative bacteria, including *Pseudomonas aeruginosa*, and provides excellent coverage for this suspected etiology.
- The patient's presentation with **fever**, a **hot, swollen, painful joint**, and **turbid synovial fluid** with **numerous leukocytes** and **gram-negative rods** on Gram stain points to severe bacterial infection requiring empiric broad-spectrum intravenous antibiotic coverage targeting gram-negative organisms.
*IV ceftazidime and gentamicin*
- **Ceftazidime** is a **third-generation cephalosporin** with good activity against gram-negative bacteria, including *Pseudomonas*. However, adding **gentamicin**, an **aminoglycoside**, could increase the risk of **nephrotoxicity** in an elderly patient with potential underlying renal impairment due to hypertension and multiple medications, especially when a single agent like cefepime might suffice initially.
- While this combination offers broad gram-negative coverage, **monotherapy with cefepime** is often preferred for empiric treatment of suspected gram-negative sepsis or osteomyelitis to minimize potential adverse effects and simplify treatment, especially in an elderly patient.
*IV vancomycin and ceftazidime*
- **Vancomycin** is primarily used for **gram-positive organisms**, particularly **MRSA**. While it addresses potential *Staphylococcus* infection if gram stain was equivocal or negative, the presence of **gram-negative rods** makes it less critical as an initial empiric therapy for this specific presentation.
- The combination would provide very broad coverage, but the primary pathology involves gram-negative rods, making the inclusion of vancomycin less targeted than alternatives, and risking unnecessary antibiotic exposure while not optimally covering common UTI-related gram-negative pathogens as effectively as cefepime.
*IV vancomycin*
- **Vancomycin** provides excellent coverage for **methicillin-resistant *Staphylococcus aureus* (MRSA)** and other gram-positive organisms, but it has **no activity against gram-negative rods**.
- Since the Gram stain specifically shows **gram-negative rods**, vancomycin monotherapy would be ineffective against the identified pathogen and is therefore an inappropriate choice.
*IV nafcillin*
- **Nafcillin** is a **penicillinase-resistant penicillin** primarily used for **methicillin-sensitive *Staphylococcus aureus* (MSSA)** and other gram-positive infections.
- It has **no significant activity against gram-negative rods**, making it an ineffective treatment option for an infection caused by gram-negative organisms.
More Fluoroquinolones US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.