Carbapenems and monobactams US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Carbapenems and monobactams. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Carbapenems and monobactams US Medical PG Question 1: You are seeing a patient in clinic who recently started treatment for active tuberculosis. The patient is currently being treated with rifampin, isoniazid, pyrazinamide, and ethambutol. The patient is not used to taking medicines and is very concerned about side effects. Specifically regarding the carbohydrate polymerization inhibiting medication, which of the following is a known side effect?
- A. Vision loss (Correct Answer)
- B. Paresthesias of the hands and feet
- C. Cutaneous flushing
- D. Arthralgias
- E. Elevated liver enzymes
Carbapenems and monobactams Explanation: ***Vision loss***
- The "carbohydrate polymerization inhibiting medication" refers to **ethambutol**, which inhibits **arabinosyl transferase** (involved in mycobacterial cell wall arabinogalactan synthesis)
- **Ethambutol** causes **optic neuritis**, leading to **decreased visual acuity**, **red-green color blindness**, and potentially **irreversible vision loss**
- **Regular ophthalmologic monitoring** is essential during ethambutol therapy
*Paresthesias of the hands and feet*
- This describes **peripheral neuropathy** caused by **isoniazid**
- Isoniazid interferes with **pyridoxine (vitamin B6) metabolism**, leading to neurotoxicity
- Risk factors include malnutrition, diabetes, alcoholism, and pregnancy
- Prevented by **pyridoxine supplementation**
*Cutaneous flushing*
- Not a characteristic side effect of first-line anti-tuberculosis medications
- More commonly associated with niacin or certain allergic/vasodilatory reactions
*Arthralgias*
- Classic side effect of **pyrazinamide**, often affecting small joints
- Caused by **pyrazinamide-induced hyperuricemia** (inhibits renal uric acid excretion)
- May require dose adjustment or discontinuation if severe
*Elevated liver enzymes*
- **Hepatotoxicity** can occur with **rifampin**, **isoniazid**, and **pyrazinamide**
- Requires regular monitoring of liver function tests during TB treatment
- Most common serious adverse effect of combination TB therapy
Carbapenems and monobactams US Medical PG Question 2: A 58-year-old man comes to the physician because of severe muscle aches and fatigue for 3 days. Last week he was diagnosed with atypical pneumonia and treated with clarithromycin. He has hyperlipidemia for which he takes lovastatin. Physical examination shows generalized tenderness of the proximal muscles in the upper and lower extremities. Serum studies show an elevated creatine kinase concentration. This patient's current symptoms are most likely caused by inhibition of which of the following hepatic enzymes?
- A. CYP2E1
- B. CYP3A4 (Correct Answer)
- C. CYP2C9
- D. CYP1A2
- E. CYP2C19
Carbapenems and monobactams Explanation: ***CYP3A4***
- The patient is taking **lovastatin**, which is metabolized by **CYP3A4**. **Clarithromycin** is a potent **CYP3A4 inhibitor**.
- Inhibition of **CYP3A4** by clarithromycin leads to increased lovastatin levels, causing statin-induced **myopathy** (muscle aches, fatigue, and elevated creatine kinase).
*CYP2E1*
- This enzyme is primarily involved in the metabolism of compounds like **ethanol** and **acetaminophen**, not lovastatin.
- Its inhibition would not explain the interaction between clarithromycin and lovastatin.
*CYP2C9*
- This enzyme metabolizes drugs such as **warfarin** and **NSAIDs**, but it is not the primary enzyme responsible for lovastatin metabolism or its interaction with clarithromycin.
- Inhibition of **CYP2C9** would not lead to the described myopathy in this context.
*CYP1A2*
- **CYP1A2** is involved in the metabolism of drugs like **caffeine** and **theophylline**.
- It does not play a significant role in the metabolism of lovastatin, and its inhibition would not cause the observed symptoms.
*CYP2C19*
- **CYP2C19** metabolizes drugs such as **clopidogrel** and **omeprazole**.
- It is not the target enzyme for the interaction between lovastatin and clarithromycin.
Carbapenems and monobactams US Medical PG Question 3: A 7-year-old boy comes to the physician because of a generalized rash for 3 days. Over the past 5 days, he has also had a high fever and a sore throat. His 16-year-old sister was treated for infectious mononucleosis 2 weeks ago. He returned from a summer camp a week ago. His immunizations are up-to-date. Three years ago, he required intubation after an allergic reaction to dicloxacillin. The patient appears ill. His temperature is 38.2°C (100.8°F). Examination shows circumferential oral pallor. Cervical lymphadenopathy is present. There is tonsillar erythema and exudate. A confluent, blanching, punctate erythematous rash with a rough texture is spread over his trunk and extremities. His hemoglobin concentration is 13.3 g/dL, leukocyte count is 12,000/mm3, and erythrocyte sedimentation rate is 43 mm/h. Which of the following is the most appropriate next step in management?
- A. Amoxicillin therapy
- B. Doxycycline therapy
- C. Azithromycin therapy (Correct Answer)
- D. Cephalexin therapy
- E. Acyclovir therapy
Carbapenems and monobactams Explanation: ***Azithromycin therapy***
- This patient presents with symptoms highly suggestive of **streptococcal pharyngitis** (sore throat, fever, tonsillar exudates, cervical lymphadenopathy) complicated by **scarlet fever** (confluent, blanching, punctate erythematous rash with a rough texture, circumferential oral pallor).
- Given his **history of severe allergic reaction (intubation) to dicloxacillin**, a penicillin-class antibiotic, azithromycin (a macrolide) is the appropriate choice for treating **Group A Streptococcus** (GAS) infection in a penicillin-allergic patient.
*Amoxicillin therapy*
- **Amoxicillin** is a penicillin-class antibiotic and is **contraindicated** due to the patient's severe allergic reaction (intubation) to dicloxacillin, another penicillin.
- Cross-reactivity between penicillins, especially in severe allergic reactions, is a significant concern, making this an unsafe choice.
*Doxycycline therapy*
- **Doxycycline**, a tetracycline, is not a first-line treatment for **streptococcal pharyngitis** and is primarily used for atypical bacterial infections or in specific cases of penicillin allergy where other agents are not suitable.
- While it has some activity against GAS, macrolides like azithromycin are preferred alternatives for penicillin-allergic patients.
*Cephalexin therapy*
- **Cephalexin** is a first-generation cephalosporin, and while it can be used for GAS, roughly 5-10% of patients with a penicillin allergy may have a **cross-reaction** to cephalosporins, especially with a history of severe reactions.
- Therefore, it is generally avoided in patients with a history of anaphylaxis or other severe reactions to penicillin.
*Acyclovir therapy*
- **Acyclovir** is an antiviral medication used to treat herpes simplex and varicella-zoster virus infections.
- The patient's symptoms (pharyngitis, rash consistent with scarlet fever) are indicative of a **bacterial infection (GAS)**, not a viral infection that would respond to acyclovir.
Carbapenems and monobactams US Medical PG Question 4: An 18-year old college freshman presents to his university clinic because he has not been feeling well for the past two weeks. He has had a persistent headache, occasional cough, and chills without rigors. The patient’s vital signs are normal and physical exam is unremarkable. His radiograph shows patchy interstitial lung infiltrates and he is diagnosed with atypical pneumonia. The patient is prescribed azithromycin and takes his medication as instructed. Despite adherence to his drug regimen, he returns to the clinic one week later because his symptoms have not improved. The organism responsible for this infection is likely resistant to azithromycin through which mechanism?
- A. Mutation in topoisomerase II
- B. Methylation of ribosomal binding site
- C. Presence of a beta-lactamase
- D. Decreased binding to RNA polymerase
- E. Insertion of drug efflux pumps (Correct Answer)
Carbapenems and monobactams Explanation: ***Insertion of drug efflux pumps***
- **Azithromycin** is a macrolide antibiotic that inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit**.
- In **Mycoplasma pneumoniae** (the most common cause of atypical pneumonia in young adults), the **most common** mechanism of macrolide resistance is through **efflux pumps**, particularly the **mef genes**.
- These efflux pumps actively transport macrolides out of the bacterial cell, reducing intracellular drug concentration and conferring resistance.
- This mechanism is responsible for the majority of macrolide-resistant *M. pneumoniae* isolates worldwide.
*Methylation of ribosomal binding site*
- **Methylation** of the ribosomal binding site (specifically the **23S rRNA** via erm genes) does prevent azithromycin from binding effectively.
- While this is a valid macrolide resistance mechanism seen in organisms like *Streptococcus pneumoniae* and *Streptococcus pyogenes*, it is **less common** in *Mycoplasma pneumoniae*.
- Efflux pumps (mef) are the predominant mechanism in *M. pneumoniae* resistant strains.
*Mutation in topoisomerase II*
- **Topoisomerase II** (DNA gyrase) is the target of **fluoroquinolone antibiotics**, not macrolides.
- Mutations in this enzyme lead to resistance against fluoroquinolones, such as **ciprofloxacin**.
*Presence of a beta-lactamase*
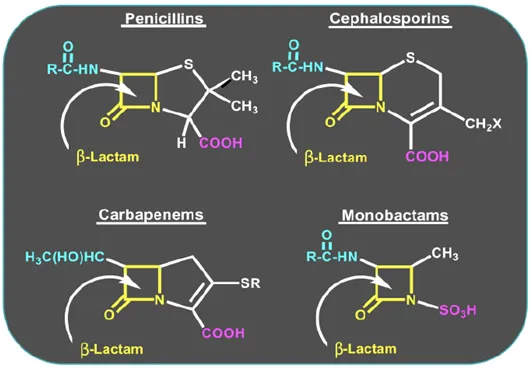
- **Beta-lactamase enzymes** inactivate **beta-lactam antibiotics** (e.g., penicillin, cephalosporins) by hydrolyzing their beta-lactam ring.
- Additionally, *Mycoplasma pneumoniae* **lacks a cell wall**, making it inherently resistant to all beta-lactam antibiotics regardless of beta-lactamase production.
*Decreased binding to RNA polymerase*
- **RNA polymerase** is the target for antibiotics like **rifampin**, which inhibits bacterial transcription.
- Decreased binding to RNA polymerase would lead to rifampin resistance, not azithromycin resistance.
Carbapenems and monobactams US Medical PG Question 5: A 31-year-old female with a bacterial infection is prescribed a drug that binds the dipeptide D-Ala-D-Ala. Which of the following drugs was this patient prescribed?
- A. Polymyxin B
- B. Nalidixic acid
- C. Chloramphenicol
- D. Vancomycin (Correct Answer)
- E. Penicillin
Carbapenems and monobactams Explanation: ***Vancomycin***
- **Vancomycin** is a glycopeptide antibiotic that directly binds to the **D-Ala-D-Ala** terminus of peptidoglycan precursors.
- This binding prevents the **transpeptidation** and **transglycosylation** steps required for bacterial cell wall synthesis, leading to cell lysis.
*Polymyxin B*
- **Polymyxins** are **cationic detergents** that disrupt the integrity of the bacterial **outer membrane** in Gram-negative bacteria.
- They bind to **lipopolysaccharide (LPS)**, causing increased permeability and leakage of intracellular components, but do not target D-Ala-D-Ala.
*Nalidixic acid*
- **Nalidixic acid** is a **quinolone antibiotic** that inhibits bacterial **DNA gyrase (topoisomerase II)** and **topoisomerase IV**.
- Its mechanism of action involves preventing DNA replication and transcription, not cell wall synthesis or D-Ala-D-Ala binding.
*Chloramphenicol*
- **Chloramphenicol** is an antibiotic that inhibits bacterial **protein synthesis** by binding to the **50S ribosomal subunit**.
- It prevents the formation of **peptide bonds** by inhibiting peptidyl transferase, an entirely different target from D-Ala-D-Ala in the cell wall.
*Penicillin*
- **Penicillin** is a beta-lactam antibiotic that inhibits bacterial cell wall synthesis by binding to and inactivating **penicillin-binding proteins (PBPs)**.
- PBPs are **transpeptidases** involved in cross-linking peptidoglycan, but penicillin does not directly bind to the D-Ala-D-Ala substrate itself; instead, it prevents the enzymes from using it.
Carbapenems and monobactams US Medical PG Question 6: You are a resident in the surgical ICU. One of the patients you are covering is a 35-year-old pregnant G1P0 in her first trimester admitted for complicated appendicitis and awaiting appendectomy. Your attending surgeon would like you to start the patient on moxifloxacin IV preoperatively. You remember from your obstetrics clerkship, however, that moxifloxacin is Pregnancy Category C, and animal studies have shown that immature animals exposed to fluoroquinolones like moxifloxacin may experience cartilage damage. You know that there are potentially safer antibiotics, such as piperacillin/tazobactam, which is in Pregnancy Category B. What should you do?
- A. Administer moxifloxacin since it is only Pregnancy Category C and, although studies may have revealed adverse effects in animals, there is no definite evidence that it causes risk in humans.
- B. Administer piperacillin/tazobactam instead of moxifloxacin without discussing with the attending since your obligation is to "first, do no harm" and both are acceptable antibiotics for complicated appendicitis.
- C. Discuss the adverse effects of each antibiotic with the patient, and then let the patient decide which antibiotic she would prefer.
- D. Wait to administer any antibiotics until you discuss your safety concerns with your attending. (Correct Answer)
- E. Administer moxifloxacin since the attending is the executive decision maker and had to know the patient was pregnant when deciding on an antibiotic.
Carbapenems and monobactams Explanation: **Wait to administer any antibiotics until you discuss your safety concerns with your attending.**
- As a resident, you have a **professional and ethical obligation** to voice concerns about patient safety, especially regarding medication choices in vulnerable populations like pregnant women.
- Discussing your concerns with the attending physician allows for a **re-evaluation of the treatment plan** based on current evidence and patient-specific factors, ensuring the safest care.
*Administer moxifloxacin since it is only Pregnancy Category C and, although studies may have revealed adverse effects in animals, there is no definite evidence that it causes risk in humans.*
- While Category C means risk cannot be ruled out and benefits *may* outweigh risks, the presence of **known adverse effects in animal studies** and the availability of a safer alternative warrant reconsideration.
- Administering a drug with known potential harm without discussing alternatives or concerns goes against the principle of **prudence and patient safety**.
*Administer piperacillin/tazobactam instead of moxifloxacin without discussing with the attending since your obligation is to "first, do no harm" and both are acceptable antibiotics for complicated appendicitis.*
- While "first, do no harm" is paramount, **unilaterally changing a treatment plan** ordered by an attending physician is inappropriate and breaches professional hierarchy and communication protocols.
- The correct approach is to **communicate concerns** to the attending, allowing for a collaborative decision, rather than making independent substitutions.
*Discuss the adverse effects of each antibiotic with the patient, and then let the patient decide which antibiotic she would prefer.*
- While patient autonomy and informed consent are crucial, decisions about specific antibiotic choices, especially for a complicated condition like appendicitis, require **medical expertise**.
- As a resident, it is your role to present information but not to delegate such complex medical decisions to a patient, particularly when you yourself have **unresolved concerns** with the attending's order.
*Administer moxifloxacin since the attending is the executive decision maker and had to know the patient was pregnant when deciding on an antibiotic.*
- While the attending is the senior decision-maker, it is possible for **oversights or errors to occur**, even with experienced physicians.
- Assuming the attending "had to know" and therefore dismissing your own clinical judgment and knowledge of potential harm is **irresponsible** and compromises patient safety.
Carbapenems and monobactams US Medical PG Question 7: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Carbapenems and monobactams Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Carbapenems and monobactams US Medical PG Question 8: A 44-year-old woman presents to her primary care physician for worsening dysuria, hematuria, and lower abdominal pain. Her symptoms began approximately 2 days ago and have progressively worsened. She denies headache, nausea, vomiting, or diarrhea. She endorses feeling "feverish" and notes to having foul smelling urine. She has a past medical history of Romano-Ward syndrome and is not on any treatment. She experiences profuse diarrhea and nausea when taking carbapenems and develops a severe rash with cephalosporins. Her temperature is 100.4°F (38C), blood pressure is 138/93 mmHg, pulse is 100/min, and respirations are 18/min. On physical exam, the patient appears uncomfortable and there is tenderness to palpation around the bilateral flanks and costovertebral angle. A urinalysis and urine culture is obtained and appropriate antibiotics are administered. On her next clinical visit urine studies and a basic metabolic panel is obtained, which is shown below:
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.2 mEq/L
HCO3-: 22 mEq/L
BUN: 20 mg/dL
Glucose: 94 mg/dL
Creatinine: 2.4 mg/dL
Urinalysis
Color: Yellow
Appearance: Clear
Blood: Negative
pH: 7 (Normal 5-8)
Protein: Negative
Nitrite: Negative
Leukocyte esterase: Negative
Cast: Epithelial casts
FeNa: 3%
Urine culture
Preliminary report: 10,000 CFU/mL E. coli
Which of the following antibiotics was most likely given to this patient?
- A. Aztreonam (Correct Answer)
- B. Vancomycin
- C. Clindamycin
- D. Levofloxacin
- E. Tobramycin
Carbapenems and monobactams Explanation: ***Aztreonam***
- This patient presents with **pyelonephritis** (fever, flank pain, dysuria, hematuria, CVA tenderness) with confirmed *E. coli* urinary tract infection
- She has **severe allergies to both carbapenems and cephalosporins**, eliminating most beta-lactam options
- **Aztreonam** is a monobactam antibiotic with excellent activity against **gram-negative bacteria** including *E. coli*
- Critically, aztreonam **does not cross-react** with other beta-lactams due to its unique monocyclic structure, making it safe in patients with penicillin/cephalosporin allergies
- **No QT prolongation** - safe in Romano-Ward syndrome
*Vancomycin*
- Primarily effective against **gram-positive bacteria** (MRSA, enterococci)
- **No activity against gram-negative organisms** like *E. coli*
- Would not be appropriate for this urinary tract infection
*Clindamycin*
- Used primarily for **anaerobic infections** and some gram-positive bacteria
- **Limited to no activity against *E. coli*** and other gram-negative organisms
- Not an effective choice for gram-negative pyelonephritis
*Levofloxacin*
- Fluoroquinolone with excellent gram-negative coverage and urinary penetration
- Generally a good choice for *E. coli* pyelonephritis
- **CONTRAINDICATED in this patient**: Fluoroquinolones cause **QT interval prolongation**, which is dangerous in patients with **Romano-Ward syndrome (congenital long QT syndrome)**
- This critical drug-disease interaction eliminates fluoroquinolones as an option
*Tobramycin*
- Aminoglycoside with good gram-negative coverage including *E. coli*
- **Highly nephrotoxic** - contraindicated in this patient with **acute kidney injury** (elevated creatinine 2.4 mg/dL, epithelial casts, FENa 3%)
- Risk of worsening renal function and ototoxicity makes it a poor choice
Carbapenems and monobactams US Medical PG Question 9: A 56-year-old man presents with breathlessness and altered mental status. The patient’s daughter says that he has been having high fever and cough for the last 3 days. Past medical history is significant for a recent hospitalization 5 days ago, following a successful coronary artery bypass grafting (CABG). In the post-operative period, he was in an intensive care unit (ICU) for 6 days, including 12 hours on mechanical ventilation. Current medications are aspirin and rosuvastatin. The patient’s daughter mentions that he has had anaphylactic reactions to penicillin in the past. His temperature is 39.4°C (103°F), pulse rate is 110/min, blood pressure is 104/78 mm Hg, and respiratory rate is 30/min. On physical examination, the patient is confused and disoriented and shows signs of respiratory distress and cyanosis. On chest auscultation, there is crepitus in the right lung. The patient is immediately started on oxygen therapy, intravenous fluids, and supportive care. After the collection of appropriate samples for bacteriological culture, treatment with empirical intravenous antibiotics are started. After 24 hours of treatment, the microbiology results indicate Pseudomonas aeruginosa infection. Antibiotic therapy is changed to a combination of aztreonam and tobramycin. Which of the following best describes the rationale for choosing this antibiotic combination?
- A. Broad-spectrum coverage against anaerobes by adding tobramycin to aztreonam
- B. Synergism of aztreonam with tobramycin (Correct Answer)
- C. Reduction of the side-effects of both aztreonam and tobramycin
- D. Broad-spectrum coverage against gram-positive cocci by adding tobramycin to aztreonam
- E. Effective combination of a bactericidal and a bacteriostatic antimicrobial against Pseudomonas aeruginosa
Carbapenems and monobactams Explanation: ***Synergism of aztreonam with tobramycin***
- This combination provides a **synergistic effect** against *Pseudomonas aeruginosa*, meaning their combined action is greater than the sum of their individual effects.
- Aztreonam is a **monobactam** that targets gram-negative bacteria, and tobramycin is an **aminoglycoside**; their co-administration often enhances bactericidal activity and helps overcome resistance.
*Broad-spectrum coverage against anaerobes by adding tobramycin to aztreonam*
- Tobramycin is an **aminoglycoside** primarily effective against aerobic gram-negative bacteria and has **no significant activity against anaerobes**.
- Aztreonam also **lacks activity against anaerobic bacteria**, making this option incorrect.
*Reduction of the side-effects of both aztreanam and tobramycin*
- Both aztreonam and tobramycin have distinct side effects, including **nephrotoxicity and ototoxicity** for tobramycin.
- Combining them, especially tobramycin, generally **increases the risk of side effects** rather than reducing them, necessitating careful monitoring.
*Broad-spectrum coverage against gram-positive cocci by adding tobramycin to aztreonam*
- Aztreonam has a **narrow spectrum** focusing on gram-negative bacteria, and **lacks activity against gram-positive cocci**.
- Tobramycin (an aminoglycoside) also has **limited activity against gram-positive cocci** when used alone, and adding it to aztreonam does not significantly broaden coverage in this regard.
*Effective combination of a bactericidal and a bacteriostatic antimicrobial against Pseudomonas aeruginosa*
- Both aztreonam (a beta-lactam) and tobramycin (an aminoglycoside) are **bactericidal antibiotics**, meaning they kill bacteria.
- This option is incorrect because it inaccurately categorizes one of the drugs as bacteriostatic; the combination consists of two bactericidal agents.
Carbapenems and monobactams US Medical PG Question 10: A 70-year-old man presents to his primary care physician for a general checkup. He states that he has been doing well and taking his medications as prescribed. He recently started a new diet and supplement to improve his health and has started exercising. The patient has a past medical history of diabetes, a myocardial infarction, and hypertension. He denies any shortness of breath at rest or with exertion. An ECG is performed and is within normal limits. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 6.7 mEq/L
HCO3-: 25 mEq/L
Glucose: 133 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most likely cause of this patient's presentation?
- A. Medication (Correct Answer)
- B. Acute renal failure
- C. Hemolysis
- D. Dietary changes
- E. Rhabdomyolysis
Carbapenems and monobactams Explanation: ***Medication***
- The patient's **hyperkalemia** (K+ 6.7 mEq/L) despite feeling well, suggests a common side effect of medications, particularly those used for his pre-existing conditions like **hypertension** (**ACE inhibitors**, **ARBs**, **spironolactone**) and **diabetes**.
- Medications are a frequent cause of asymptomatic electrolyte abnormalities, and given his complex medical history and the absence of acute symptoms, this is the most likely culprit.
*Acute renal failure*
- While acute renal failure can cause **hyperkalemia**, it typically presents with other symptoms such as **oliguria**, **fluid retention**, or other signs of organ dysfunction, which are not described.
- The patient is reported to be "doing well" without **shortness of breath** or other acute complaints, making acute renal failure less likely as the primary cause of isolated hyperkalemia.
*Hemolysis*
- **Hemolysis** can release intracellular potassium, leading to **pseudohyperkalemia**, but it would typically be suspected in cases of **blood draw errors** or conditions causing red blood cell breakdown, none of which are indicated.
- The patient's presentation does not include any signs or symptoms suggestive of red cell destruction.
*Dietary changes*
- While an extremely **high-potassium diet** or certain **supplements** could contribute to hyperkalemia, it is less common for dietary changes alone to cause such a significant elevation in a patient with normal organ function.
- Given his medical history, medication-induced hyperkalemia is a more direct and common explanation.
*Rhabdomyolysis*
- **Rhabdomyolysis** involves the breakdown of muscle tissue, releasing potassium and other intracellular contents, but it is usually associated with significant **muscle pain**, **weakness**, and elevated **creatine kinase**.
- The patient denies these symptoms and has no other indicators pointing towards severe muscle injury.
More Carbapenems and monobactams US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.