Monoclonal antibodies in cancer US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Monoclonal antibodies in cancer. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Monoclonal antibodies in cancer US Medical PG Question 1: A 33-year-old woman with a history of multiple sclerosis is brought to the physician because of dizziness, urinary incontinence, loss of vision in her right eye, and numbness and weakness of the left leg. She has had recurrent episodes of neurological symptoms despite several changes in her medication regimen. An MRI of the brain shows several new enhancing lesions in the periventricular white matter and the brainstem. Treatment with a drug that binds to CD52 is initiated. Which of the following agents was most likely prescribed?
- A. Alemtuzumab (Correct Answer)
- B. Eculizumab
- C. Abciximab
- D. Rituximab
- E. Bevacizumab
Monoclonal antibodies in cancer Explanation: ***Alemtuzumab***
- **Alemtuzumab** is a monoclonal antibody that targets **CD52**, a glycoprotein found on the surface of mature lymphocytes (T and B cells), monocytes, and macrophages, leading to their depletion.
- It is used in **highly active relapsing-remitting multiple sclerosis (RRMS)**, especially when other disease-modifying therapies have failed, which aligns with the patient's history of recurrent neurological symptoms and new enhancing lesions.
*Eculizumab*
- **Eculizumab** targets the **C5 complement protein** and is used for conditions like **paroxysmal nocturnal hemoglobinuria** and **atypical hemolytic uremic syndrome**, not multiple sclerosis.
- It works by inhibiting the complement cascade, which is not the primary mechanism of action for MS treatment involving lymphocyte depletion.
*Abciximab*
- **Abciximab** is a **glycoprotein IIb/IIIa inhibitor** that prevents platelet aggregation and is used as an antiplatelet agent in acute coronary syndromes and percutaneous coronary intervention.
- Its mechanism of action and primary indication are unrelated to the immunological processes involved in multiple sclerosis.
*Rituximab*
- **Rituximab** targets **CD20** on B cells and is used in conditions like **non-Hodgkin lymphoma**, **chronic lymphocytic leukemia**, and certain autoimmune diseases like **rheumatoid arthritis** and **vasculitis**.
- While it's a B-cell depleting agent and has shown efficacy in MS, the question specifically asks for a drug that binds to **CD52**, not CD20.
*Bevacizumab*
- **Bevacizumab** is an anti-VEGF antibody that inhibits **angiogenesis** and is primarily used in the treatment of various cancers, such as colorectal, lung, and renal cell carcinoma.
- Its mechanism of action involving inhibition of vascular endothelial growth factor (VEGF) is not indicated for the management of multiple sclerosis.
Monoclonal antibodies in cancer US Medical PG Question 2: A 40-year-old male with a history of chronic alcoholism recently received a liver transplant. Two weeks following the transplant, the patient presents with a skin rash and frequent episodes of bloody diarrhea. A colonoscopy is performed and biopsy reveals apoptosis of colonic epithelial cells. What is most likely mediating these symptoms?
- A. Donor T-cells (Correct Answer)
- B. Recipient T-cells
- C. Recipient B-cells
- D. Recipient antibodies
- E. Donor B-cells
Monoclonal antibodies in cancer Explanation: ***Donor T-cells***
- This clinical presentation of **skin rash**, **bloody diarrhea**, and **colonic epithelial apoptosis** following an allogeneic transplant (like a liver transplant) is classic for **Graft-versus-Host Disease (GVHD)**.
- In GVHD, **immunocompetent T-cells from the donor** recognize the recipient's tissues as foreign and mount an immune attack, causing damage to organs like the skin, gastrointestinal tract, and liver.
*Recipient T-cells*
- **Recipient T-cells** are typically immunosuppressed following an organ transplant to prevent organ rejection.
- Furthermore, if activated, recipient T-cells would target the donor organ (the liver in this case), leading to **rejection**, rather than the systemic symptoms observed (skin rash, bloody diarrhea) which suggest an attack by donor cells on recipient tissues.
*Recipient B-cells*
- While recipient B-cells can be involved in **antibody-mediated rejection** of the transplanted organ, they are not the primary mediators of **cellular GVHD**.
- **Antibody-mediated rejection** would typically involve antibodies targeting the donor liver, leading to liver dysfunction, not the widespread GVHD symptoms described.
*Recipient antibodies*
- **Recipient antibodies** are primarily involved in **antibody-mediated rejection** of the transplanted organ, which would manifest as dysfunction of the transplanted liver.
- They do not mediate the symptoms of **Graft-versus-Host Disease (GVHD)**, which is a cell-mediated immune response.
*Donor B-cells*
- **Donor B-cells** are generally not the primary mediators of GVHD.
- While donor immune cells are crucial for GVHD, the major players are **donor T-cells**, which directly recognize and attack host tissues.
Monoclonal antibodies in cancer US Medical PG Question 3: A 55-year-old Caucasian male presents for a routine colonoscopy. A polyp is found in the patient's transverse colon and is found to be cancerous on histological evaluation. Upon examination, it is found that these cancerous cells have decreased MHC class I expression on their surface. Which immune system cell is most capable of killing these tumor cells?
- A. Cytotoxic T-cells
- B. B-cells
- C. Macrophages
- D. Natural killer cells (Correct Answer)
- E. Eosinophils
Monoclonal antibodies in cancer Explanation: ***Natural killer cells***
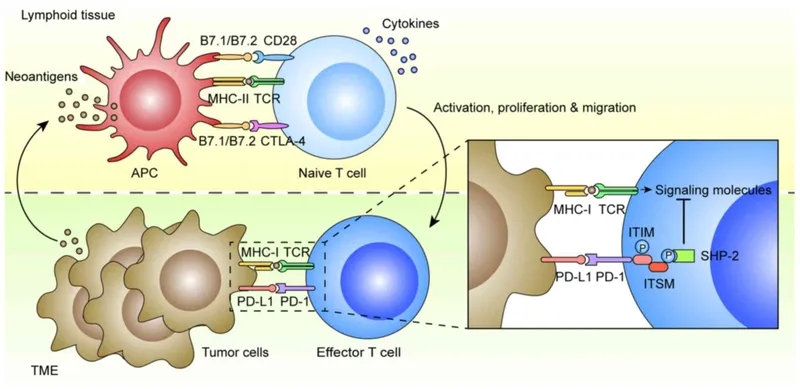
- **Natural killer (NK) cells** are specialized lymphocytes that identify and kill cells with **decreased or absent MHC class I expression**, a common feature of tumor cells and virus-infected cells.
- They provide a rapid, non-specific immune response without prior sensitization.
*Cytotoxic T-cells*
- **Cytotoxic T-cells (CTLs)** recognize and kill target cells by binding to specific **antigens presented by MHC class I molecules**.
- Since these cancer cells have **decreased MHC class I expression**, CTLs would be less effective at recognizing and killing them.
*B-cells*
- **B-cells** are primarily involved in humoral immunity, producing **antibodies** that can neutralize pathogens or mark cells for destruction.
- They do not directly kill target cells, and their activation typically requires specific antigen recognition, often with T-cell help.
*Macrophages*
- **Macrophages** are phagocytic cells that engulf and digest cellular debris, pathogens, and some tumor cells.
- While they can kill tumor cells, their primary mechanism involves **phagocytosis** or antigen presentation, not direct cytotoxicity based on MHC I expression levels.
*Eosinophils*
- **Eosinophils** are granulocytes primarily involved in the defense against **parasitic infections** and in allergic reactions.
- They are not a primary defense mechanism against tumor cells, especially not based on MHC class I expression.
Monoclonal antibodies in cancer US Medical PG Question 4: A patient is infected with a pathogen and produces many antibodies to many antigens associated with that pathogen via Th cell-activated B cells. This takes place in the germinal center of the lymphoid tissues. If the same patient is later re-infected with the same pathogen, the immune system will respond with a much stronger response, producing antibodies with greater specificity for that pathogen in a shorter amount of time. What is the term for this process that allows the B cells to produce antibodies specific to that antigen?
- A. Affinity maturation (Correct Answer)
- B. Avidity
- C. Immunoglobulin class switching
- D. T cell negative selection
- E. T cell positive selection
Monoclonal antibodies in cancer Explanation: ***Affinity maturation***
- **Affinity maturation** is the process by which B cells produce antibodies with progressively higher affinity for an antigen over the course of an immune response, allowing for a more specific and potent response upon re-exposure.
- This process occurs primarily in the **germinal centers** of lymphoid organs, driven by somatic hypermutation of antibody genes and subsequent selection of B cells exhibiting increased binding affinity.
*Avidity*
- **Avidity** refers to the overall strength of binding between a multivalent antibody and a multivalent antigen, taking into account the combined strength of multiple binding sites.
- While high avidity is a characteristic of effective antibody responses, it describes the strength of binding rather than the *process* of improving specificity and affinity over time.
*Immunoglobulin class switching*
- **Immunoglobulin class switching** (or isotype switching) is the process by which B cells change the class of antibody they produce (e.g., from IgM to IgG, IgA, or IgE), while retaining the same antigen specificity.
- This process diversifies the effector functions of antibodies but does not directly describe the *improvement in antigen binding affinity* or specificity.
*T cell negative selection*
- **T cell negative selection** is a critical process in the thymus where T cells that react too strongly to self-antigens are eliminated or inactivated to prevent autoimmunity.
- This process is fundamental for establishing central tolerance in T cells and is separate from the B cell-mediated improvement in antibody specificity described.
*T cell positive selection*
- **T cell positive selection** also occurs in the thymus, ensuring that only T cells capable of recognizing self-MHC molecules survive and mature.
- This process is essential for T cell function (MHC restriction) but is distinct from the described mechanism of B cell antibody refinement.
Monoclonal antibodies in cancer US Medical PG Question 5: A 38-year-old woman comes to the physician for a follow-up examination. Two years ago, she was diagnosed with multiple sclerosis. Three weeks ago, she was admitted and treated for right lower leg weakness with high-dose methylprednisone for 5 days. She has had 4 exacerbations over the past 6 months. Current medications include interferon beta and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 116/74 mm Hg. Examination shows pallor of the right optic disk. Neurologic examination shows no focal findings. She is anxious about the number of exacerbations and repeated hospitalizations. She is counseled about the second-line treatment options available to her. She consents to treatment with natalizumab. However, she has read online about its adverse effects and is concerned. This patient is at increased risk for which of the following complications?
- A. Tuberculosis
- B. Syndrome of inappropriate antidiuretic hormone
- C. Parkinsonism
- D. Progressive multifocal leukoencephalopathy (Correct Answer)
- E. Aplastic anemia
Monoclonal antibodies in cancer Explanation: ***Progressive multifocal leukoencephalopathy***
- **Natalizumab** is a monoclonal antibody that blocks the binding of leukocytes to endothelial cells, preventing their entry into the central nervous system. This immunosuppressive effect increases the risk of **progressive multifocal leukoencephalopathy (PML)**, especially in patients who are positive for the **JC virus**.
- PML is a serious and often fatal opportunistic infection of the brain caused by the **JC virus**, which demyelinates axons and leads to severe neurological deficits.
*Tuberculosis*
- While some immunosuppressants can reactivate **latent tuberculosis**, natalizumab is not typically associated with an increased risk of TB compared to other immunomodulatory drugs like TNF-alpha inhibitors.
- The mechanism of action of natalizumab (alpha-4 integrin blocker) does not directly impede the immune response responsible for containing mycobacterial infections to the same extent as other treatments.
*Syndrome of inappropriate antidiuretic hormone*
- **SIADH** is not a known adverse effect of natalizumab.
- SIADH is characterized by excessive secretion of **antidiuretic hormone**, leading to hyponatremia, and is often associated with certain medications (e.g., SSRIs, carbamazepine) or underlying conditions like malignancy or pulmonary disease.
*Parkinsonism*
- Parkinsonism involves symptoms like **bradykinesia**, rigidity, and tremor, and is a neurodegenerative disorder.
- There is **no evidence** suggesting a causal link between natalizumab treatment and the development of Parkinsonism.
*Aplastic anemia*
- **Aplastic anemia** is a rare but severe condition where the bone marrow fails to produce blood cells.
- This adverse effect is not associated with natalizumab; it is more commonly linked to certain **chemotherapeutic agents**, radiation, or specific antimicrobial drugs like chloramphenicol.
Monoclonal antibodies in cancer US Medical PG Question 6: A 66-year-old man comes to the physician because of a 3-month history of constipation and streaks of blood in his stool. He has had a 10-kg (22-lb) weight loss during this period. Colonoscopy shows an exophytic tumor in the sigmoid colon. A CT scan of the abdomen shows liver metastases and enlarged mesenteric and para-aortic lymph nodes. A diagnosis of stage IV colorectal cancer is made, and palliative chemotherapy is initiated. The chemotherapy regimen includes a monoclonal antibody that inhibits tumor growth by preventing ligand binding to a protein directly responsible for epithelial cell proliferation and organogenesis. Which of the following proteins is most likely inhibited by this drug?
- A. VEGF
- B. TNF-α
- C. EGFR (Correct Answer)
- D. ALK
- E. CD52
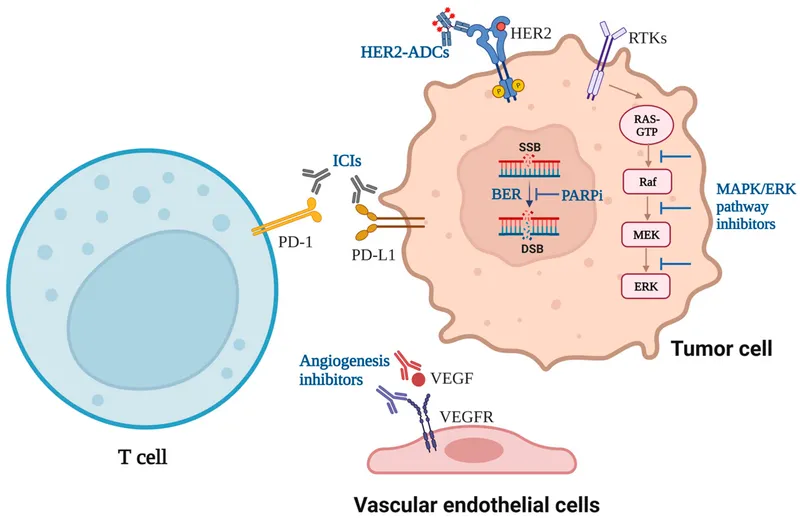
Monoclonal antibodies in cancer Explanation: ***EGFR***
- The description of a monoclonal antibody preventing ligand binding to a protein responsible for **epithelial cell proliferation** and organogenesis strongly points to the **epidermal growth factor receptor (EGFR)**.
- EGFR is highly expressed in many colorectal cancers and its activation by ligands like EGF promotes cell growth, survival, and metastasis. Inhibiting it reduces tumor progression.
*VEGF*
- **Vascular endothelial growth factor (VEGF)** is primarily involved in **angiogenesis**, the formation of new blood vessels.
- While anti-VEGF therapies (e.g., bevacizumab) are used in colorectal cancer, their mechanism is inhibiting blood supply to the tumor, not directly blocking a receptor responsible for epithelial cell proliferation as described.
*TNF-α*
- **Tumor necrosis factor-alpha (TNF-α)** is a **cytokine** primarily involved in inflammation and immune responses.
- Antibodies against TNF-α (e.g., infliximab) are used in inflammatory conditions like Crohn's disease, not typically as targeted therapy for colorectal cancer directly inhibiting epithelial proliferation.
*ALK*
- **Anaplastic lymphoma kinase (ALK)** is a **receptor tyrosine kinase** often implicated in lung cancer and lymphomas.
- ALK rearrangements lead to oncogenic fusion proteins, but it is not a primary target for widespread epithelial cell proliferation in colorectal cancer.
*CD52*
- **CD52** is a glycoprotein found on the surface of various immune cells, including lymphocytes.
- Antibodies targeting CD52 (e.g., alemtuzumab) are used in certain leukemias and lymphomas to deplete these cells, not for inhibiting epithelial cell proliferation in solid tumors.
Monoclonal antibodies in cancer US Medical PG Question 7: A 72-year-old woman is brought to the emergency department for right hip pain 1 hour after she fell while walking around in her house. She has been unable to stand or walk since the fall. She has hypertension and gout. Her sister died of multiple myeloma at the age of 55 years. Current medications include amlodipine and febuxostat. She does not smoke cigarettes. She drinks a glass of wine daily. Her temperature is 37.3°C (99.1°F), pulse is 101/min, and blood pressure is 128/86 mm Hg. Examination shows right groin tenderness. Range of motion of the right hip is limited by pain. The remainder of the examination shows no abnormalities. A complete blood count and serum creatinine concentration are within the reference range. An x-ray of the hip shows a linear fracture of the right femoral neck. She is scheduled for surgery. Which of the following is the most likely underlying cause of this patient's fracture?
- A. Defective osteoclast function
- B. Impaired bone mineralization
- C. Monoclonal antibody production
- D. Interrupted vascular supply
- E. Reduced osteoblastic activity (Correct Answer)
Monoclonal antibodies in cancer Explanation: ***Reduced osteoblastic activity***
- In a 72-year-old woman, a **femoral neck fracture** following a fall typically indicates underlying **osteoporosis**, which is characterized by reduced **osteoblastic activity** and overall bone density loss.
- As women age, particularly after menopause, **estrogen deficiency** leads to an imbalance in bone remodeling, with bone resorption outpacing bone formation, thus leading to weaker bones.
*Defective osteoclast function*
- **Defective osteoclast function** is primarily associated with conditions like **osteopetrosis**, where bones become dense and brittle due to impaired bone resorption, making them prone to fracture, which is not consistent with the typical presentation of a hip fracture in an elderly woman.
- This condition is rare and usually presents earlier in life, often with symptoms such as **anemia**, **hepatosplenomegaly**, and **cranial nerve compression**.
*Impaired bone mineralization*
- **Impaired bone mineralization** is characteristic of **osteomalacia** (in adults) or **rickets** (in children), usually due to **vitamin D deficiency** or phosphate imbalances.
- While it can lead to bone pain and increased fracture risk, osteoporosis due to aging is a much more common cause of hip fractures in this demographic, and there are no signs of osteomalacia such as **pseudofractures** or specific biochemical abnormalities like **hypophosphatemia** or **elevated alkaline phosphatase** without other causes.
*Monoclonal antibody production*
- **Monoclonal antibody production** is associated with **multiple myeloma**, a plasma cell malignancy that causes **lytic bone lesions** and diffuse osteopenia.
- While the patient's sister died of multiple myeloma, her normal complete blood count and creatinine, and the absence of specific myeloma-related symptoms (e.g., **hypercalcemia**, **renal failure**, **anemia**, or **CRAB criteria**) make this diagnosis less likely for her acute hip fracture.
*Interrupted vascular supply*
- **Interrupted vascular supply** can lead to **avascular necrosis (AVN)**, which weakens the bone and can cause collapse, eventually leading to a fracture.
- However, for an acute traumatic hip fracture, especially in the femoral neck, the primary underlying cause in an elderly person is generally **osteoporosis**, and AVN would typically present with chronic pain and characteristic imaging findings prior to an acute traumatic event.
Monoclonal antibodies in cancer US Medical PG Question 8: A 68-year-old man is brought to the emergency department 25 minutes after he was found shaking violently on the bathroom floor. His wife reports that he has become increasingly confused over the past 2 days and that he has been sleeping more than usual. He was started on chemotherapy 4 months ago for chronic lymphocytic leukemia. He is confused and oriented to person only. Neurological examination shows right-sided ptosis and diffuse hyperreflexia. An MRI of the brain shows disseminated, nonenhancing white matter lesions with no mass effect. A polymerase chain reaction assay of the cerebrospinal fluid confirms infection with a virus that has double-stranded, circular DNA. An antineoplastic drug with which of the following mechanisms of action is most likely responsible for this patient's current condition?
- A. Monoclonal antibody against CD20+ (Correct Answer)
- B. Monoclonal antibody against EGFR
- C. Tyrosine kinase inhibitor
- D. Topoisomerase II inhibitor
- E. Free radical formation
Monoclonal antibodies in cancer Explanation: **Monoclonal antibody against CD20+**
- The patient's presentation with **progressive multifocal leukoencephalopathy (PML)**, characterized by neurological deficits, white matter lesions, and a positive PCR for a **double-stranded, circular DNA virus (JC virus)**, strongly suggests a compromised immune system, likely due to chronic lymphocytic leukemia (CLL) treatment.
- **Rituximab**, a monoclonal antibody that targets **CD20+ B-lymphocytes**, is a common treatment for CLL and is associated with an increased risk of PML due to its immunosuppressive effects.
*Monoclonal antibody against EGFR*
- **Epidermal growth factor receptor (EGFR) inhibitors** (e.g., cetuximab, erlotinib) are used in various cancers but are not typically associated with the development of PML.
- Side effects of EGFR inhibitors commonly include skin rashes, diarrhea, and stomatitis, not the neurological symptoms seen here.
*Tyrosine kinase inhibitor*
- **Tyrosine kinase inhibitors (TKIs)**, such as imatinib or ibrutinib, are used in certain leukemias and other cancers.
- While TKIs can have various side effects, they are not primarily known for causing B-cell depletion or an increased risk of PML like rituximab.
*Topoisomerase II inhibitor*
- **Topoisomerase II inhibitors** (e.g., etoposide, doxorubicin) are chemotherapy agents that induce DNA damage.
- Their primary toxicities include myelosuppression, cardiotoxicity (for anthracyclines), and secondary malignancies, not opportunistic viral infections like PML.
*Free radical formation*
- **Free radical formation** is a mechanism of action for certain chemotherapeutic agents like **bleomycin** or **anthracyclines**, which cause DNA damage.
- While these drugs have significant side effects, they are not typically linked to the selective immunosuppression that leads to PML in the context of CLL treatment.
Monoclonal antibodies in cancer US Medical PG Question 9: A 45-year-old male reports several years of asbestos exposure while working in the construction industry. He reports smoking 2 packs of cigarettes per day for over 20 years. Smoking and asbestos exposure increase the incidence of which of the following diseases?
- A. Emphysema
- B. Malignant pulmonary mesothelioma
- C. Multiple myeloma
- D. Bronchogenic carcinoma (Correct Answer)
- E. Chronic bronchitis
Monoclonal antibodies in cancer Explanation: ***Bronchogenic carcinoma***
- **Smoking** is the leading cause of **bronchogenic carcinoma**, and **asbestos exposure** significantly *multiplies* its risk, rather than simply adding to it.
- This synergistic effect means that smokers exposed to asbestos have a **much higher incidence** of lung cancer compared to those with either exposure alone.
*Emphysema*
- Primarily linked to **smoking** and chronic exposure to irritants, but asbestos exposure does not significantly increase its incidence.
- While both smoking and asbestos can cause pulmonary issues, their primary mechanisms for emphysema are distinct.
*Malignant pulmonary mesothelioma*
- **Malignant mesothelioma** is strongly associated with **asbestos exposure**, but its incidence is *not significantly increased* by smoking.
- Smoking is a risk factor for lung cancer, but not a primary risk factor for mesothelioma itself.
*Multiple myeloma*
- This is a **hematologic malignancy** (cancer of plasma cells) and has no established link with either **smoking** or **asbestos exposure**.
- Its risk factors are largely genetic and related to other environmental factors, but not directly linked to respiratory toxins.
*Chronic bronchitis*
- **Chronic bronchitis** is primarily caused by **smoking** and exposure to environmental pollutants.
- While asbestos exposure can cause lung damage, it doesn't directly or significantly increase the incidence of chronic bronchitis.
Monoclonal antibodies in cancer US Medical PG Question 10: An otherwise healthy 13-year-old boy is brought to the physician because of asthma attacks that have been increasing in frequency and severity over the past 4 weeks. He was first diagnosed with asthma 6 months ago. Current medications include high-dose inhaled fluticasone and salmeterol daily, with additional albuterol as needed. He has required several courses of oral corticosteroids. A medication is added to his therapy regimen that results in downregulation of the high-affinity IgE receptor (FcεRI) on mast cells and basophils. Which of the following drugs was most likely added to the patient's medication regimen?
- A. Infliximab
- B. Theophylline
- C. Zileuton
- D. Nedocromil
- E. Omalizumab (Correct Answer)
Monoclonal antibodies in cancer Explanation: ***Omalizumab***
- **Omalizumab** is a **monoclonal antibody** that targets and binds to free IgE, preventing its binding to **FcεRI receptors** on mast cells and basophils.
- By reducing free IgE, it leads to a **downregulation of FcεRI receptors**, thereby decreasing mediator release and reducing asthma symptoms in severe, persistent asthma.
*Infliximab*
- **Infliximab** is an **anti-TNF-α monoclonal antibody** used primarily in inflammatory conditions like **rheumatoid arthritis**, **Crohn's disease**, and **ankylosing spondylitis**.
- It does not directly affect IgE or its receptors, thus it is not indicated for the treatment of **asthma**.
*Theophylline*
- **Theophylline** is a **phosphodiesterase inhibitor** that causes bronchodilation by increasing intracellular cAMP.
- It does not modulate IgE or its receptors, and its use is limited by a narrow **therapeutic index** and potential for side effects.
*Zileuton*
- **Zileuton** is a **5-lipoxygenase inhibitor** that blocks the synthesis of **leukotrienes**, potent bronchoconstrictors and inflammatory mediators in asthma.
- While effective in some asthma patients, it does not act on IgE or its receptors.
*Nedocromil*
- **Nedocromil** is a **mast cell stabilizer** that inhibits the release of inflammatory mediators from mast cells.
- It does not directly impact IgE levels or the expression of **FcεRI receptors** on mast cells and basophils, making it less suitable for severe, refractory asthma requiring IgE-pathway modulation.
More Monoclonal antibodies in cancer US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.