Management of chemotherapy toxicities US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Management of chemotherapy toxicities. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Management of chemotherapy toxicities US Medical PG Question 1: A 67-year-old man comes to the physician because of numbness and burning sensation of his legs for the past week. He also complains that his stools have been larger and rougher than usual. He has non-Hodgkin lymphoma and is currently receiving chemotherapy with prednisone, vincristine, rituximab, cyclophosphamide, and doxorubicin. He has received 4 cycles of chemotherapy, and his last chemotherapy cycle was 2 weeks ago. His temperature is 37.1°C (98.8°F), pulse is 89/min, and blood pressure is 122/80 mm Hg. Examination shows decreased muscle strength in the distal muscles of the lower extremities. Ankle jerk is 1+ bilaterally and knee reflex is 2+ bilaterally. Sensation to pain, vibration, and position is decreased over the lower extremities. Serum concentrations of glucose, creatinine, electrolytes, and calcium are within the reference range. Which of the following is the most likely cause of this patient's symptoms?
- A. Paraneoplastic autoantibodies
- B. Guillain-Barré syndrome
- C. Adverse effect of vincristine (Correct Answer)
- D. Charcot–Marie–Tooth disease
- E. Spinal cord compression
Management of chemotherapy toxicities Explanation: ***Adverse effect of vincristine***
- The patient's symptoms of **numbness, burning sensation, decreased distal muscle strength, and sensory deficits** (pain, vibration, position) are classic signs of **peripheral neuropathy**, a common and dose-limiting side effect of vincristine.
- **Vincristine** is known to disrupt **microtubule formation**, which is crucial for axonal transport in neurons, leading to nerve damage and constipation due to autonomic neuropathy (manifesting as larger, rougher stools).
*Paraneoplastic autoantibodies*
- While paraneoplastic syndromes can cause neuropathies, they typically develop **before or concurrently with cancer diagnosis** and tend to be progressive, rather than appearing after several cycles of chemotherapy in this pattern.
- The patient's symptoms are highly consistent with a known drug toxicity, making paraneoplastic antibodies a less likely primary cause.
*Guillain-Barré syndrome*
- **Guillain-Barré syndrome** typically presents as an **acute, ascending paralysis** often preceded by an infection, which is not described here.
- While it causes neuropathy, the temporal onset and the patient's ongoing chemotherapy make a drug-induced neuropathy more probable.
*Charcot–Marie–Tooth disease*
- **Charcot–Marie–Tooth disease** is a group of **hereditary neuropathies** that typically present in childhood or early adulthood with a *slowly progressive* course.
- The acute, subacute onset of symptoms within the past week, in an older patient receiving chemotherapy, makes this genetic condition highly unlikely.
*Spinal cord compression*
- **Spinal cord compression** would likely cause more prominent **motor weakness**, **spasticity**, and potentially a distinct sensory level or bowel/bladder dysfunction, which are not the primary features here.
- The diffuse sensory findings and distal predominance of weakness are more characteristic of a peripheral neuropathy rather than a myelopathy.
Management of chemotherapy toxicities US Medical PG Question 2: A 60-year-old man comes to the physician for the evaluation of nausea over the past week. During this period, he has also had several episodes of non-bloody vomiting. Last month, he was diagnosed with stage II Hodgkin lymphoma and was started on adriamycin, bleomycin, vinblastine, and dacarbazine. His temperature is 37°C (98.6°F), pulse is 95/min, and blood pressure is 105/70 mm Hg. Physical examination shows cervical lymphadenopathy. The liver is palpated 1 to 2 cm below the right costal margin, and the spleen is palpated 2 to 3 cm below the left costal margin. The remainder of the examination shows no abnormalities. The patient is started on an appropriate medication. Two weeks later, he develops headaches and states that his last bowel movement was 4 days ago. The patient was most likely treated with which of the following medications?
- A. 5-HT3 antagonist (Correct Answer)
- B. Cannabinoid receptor agonist
- C. H1 antagonist
- D. Muscarinic antagonist
- E. D2 antagonist
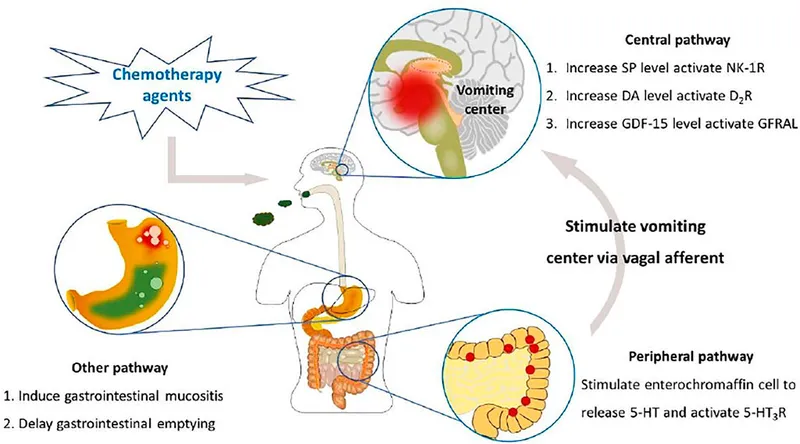
Management of chemotherapy toxicities Explanation: ***5-HT3 antagonist***
- The patient was likely treated with a **5-HT3 antagonist** due to symptoms of nausea and vomiting following chemotherapy. This class of antiemetics can cause dose-dependent **headache** and **constipation** as common side effects.
- The subsequent development of headaches and constipation (no bowel movement for 4 days) points to the known side effect profile of 5-HT3 antagonists, such as **ondansetron**.
*Cannabinoid receptor agonist*
- **Cannabinoid receptor agonists** (e.g., dronabinol) are used for chemotherapy-induced nausea and vomiting but are associated with side effects like **drowsiness**, **dizziness**, and **mood changes**, not typically headache and constipation.
- They also tend to have a slower onset of action compared to 5-HT3 antagonists.
*H1 antagonist*
- **H1 antagonists** (e.g., diphenhydramine) are used for motion sickness and mild nausea, often causing **sedation** and **anticholinergic effects** like dry mouth, blurred vision, and urinary retention.
- While they can cause constipation due to anticholinergic effects, headache is not a prominent side effect, and their primary role is not for severe chemotherapy-induced nausea.
*Muscarinic antagonist*
- **Muscarinic antagonists** (e.g., scopolamine) have antiemetic properties, particularly for motion sickness, but are not first-line for chemotherapy-induced nausea and vomiting.
- These anticholinergic drugs are associated with side effects such as **dry mouth**, **constipation**, **urinary retention**, and **blurred vision**, but they are not the most likely choice given the clinical scenario and the specific combination of headache and constipation.
*D2 antagonist*
- **D2 antagonists** (e.g., metoclopramide, prochlorperazine) are effective antiemetics but are primarily associated with **extrapyramidal symptoms** (e.g., dystonia, parkinsonism), sedation, and hyperprolactinemia.
- Although constipation can occur, the combination of headache and constipation in this context is more characteristic of 5-HT3 antagonists, which are commonly prescribed first-line for chemotherapy-induced nausea.
Management of chemotherapy toxicities US Medical PG Question 3: A 67-year-old woman with advanced bladder cancer comes to the physician for a follow-up examination. She is currently undergoing chemotherapy with an agent that forms cross-links between DNA strands. Serum studies show a creatinine concentration of 2.1 mg/dL and a blood urea nitrogen concentration of 30 mg/dL. Urine dipstick of a clean-catch midstream specimen shows 2+ protein and 1+ glucose. Prior to initiation of chemotherapy, her laboratory values were within the reference range. In addition to hydration, administration of which of the following would most likely have prevented this patient's current condition?
- A. Leucovorin
- B. Amifostine (Correct Answer)
- C. Aprepitant
- D. Mesna
- E. Rasburicase
Management of chemotherapy toxicities Explanation: **Amifostine**
- This patient's symptoms (elevated creatinine and BUN, 2+ protein, 1+ glucose in urine) suggest **renal tubular damage**, specifically acute tubular necrosis, likely caused by a nephrotoxic chemotherapeutic agent.
- **Amifostine** is a cytoprotective agent that scavenges reactive oxygen species in local tissues, thereby reducing the nephrotoxic effects of **alkylating agents** like cisplatin, which forms cross-links between DNA strands.
*Leucovorin*
- **Leucovorin** (folinic acid) is used to rescue normal cells from the adverse effects of **methotrexate**, enhancing its excretion and reducing toxicity.
- It is not indicated for preventing kidney damage from DNA cross-linking agents.
*Aprepitant*
- **Aprepitant** is a neurokinin-1 (NK1) receptor antagonist used to prevent **chemotherapy-induced nausea and vomiting**.
- It does not have protective effects against nephrotoxicity.
*Mesna*
- **Mesna** (2-mercaptoethane sulfonate sodium) is used to prevent **hemorrhagic cystitis** caused by acrolein, a toxic metabolite of cyclophosphamide and ifosfamide.
- It does not prevent nephrotoxicity from other types of chemotherapy agents.
*Rasburicase*
- **Rasburicase** is a recombinant urate oxidase enzyme used to prevent or treat **tumor lysis syndrome** by converting uric acid to allantoin, which is more soluble and easily excreted.
- It is not used for preventing direct kidney damage from chemotherapeutic agents.
Management of chemotherapy toxicities US Medical PG Question 4: A 70-year-old man presents to a medical clinic reporting blood in his urine and lower abdominal pain for the past few days. He is also concerned about urinary frequency and urgency. He states that he recently completed a cycle of chemotherapy for non-Hodgkin lymphoma. Which medication in the chemotherapy regimen most likely caused his symptoms?
- A. Cyclophosphamide (Correct Answer)
- B. Rituximab
- C. Prednisone
- D. Methotrexate
- E. Cytarabine
Management of chemotherapy toxicities Explanation: ***Cyclophosphamide***
- **Cyclophosphamide** is an alkylating agent commonly used in the **R-CHOP regimen** (standard treatment for non-Hodgkin lymphoma) and is known to cause **hemorrhagic cystitis** due to the accumulation of its metabolite **acrolein** in the bladder.
- This leads to symptoms like **blood in urine (hematuria)**, lower abdominal pain, urinary frequency, and urgency.
- This toxicity can be mitigated by co-administering **mesna** (2-mercaptoethane sulfonate sodium) and ensuring adequate hydration to prevent bladder irritation.
*Rituximab*
- **Rituximab** is a **monoclonal antibody** targeting CD20 on B-cells, the "R" in R-CHOP, primarily associated with **infusion reactions**, B-cell depletion, and increased risk of infections.
- It does not typically cause direct **bladder toxicity** or hemorrhagic cystitis.
*Prednisone*
- **Prednisone** is a corticosteroid (the "P" in R-CHOP) commonly used in lymphoma regimens to induce apoptosis in lymphoid cells and manage side effects of chemotherapy.
- Its side effects include **immunosuppression**, hyperglycemia, and gastric irritation, but not usually hemorrhagic cystitis.
*Methotrexate*
- **Methotrexate** is an antimetabolite that inhibits dihydrofolate reductase and is commonly associated with **myelosuppression**, mucositis, and nephrotoxicity at high doses.
- While it can affect the kidneys and is sometimes used in certain lymphoma regimens, it is not a primary cause of **hemorrhagic cystitis**.
*Cytarabine*
- **Cytarabine** is an antimetabolite primarily used in leukemias and some aggressive lymphomas, known for causing **myelosuppression**, mucositis, and cerebellar toxicity at high doses.
- It is not typically associated with **hemorrhagic cystitis** or bladder irritation.
Management of chemotherapy toxicities US Medical PG Question 5: A 64-year-old woman comes to the physician for her routine health maintenance examination. She feels well. She had cervical cancer and received radiotherapy 8 years ago. Her vital signs are within normal limits. On percussion, the spleen size is 15 cm. Otherwise, the physical examination shows no abnormalities. The laboratory test results are as follows:
Hemoglobin 10 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 65,000/mm3
Platelet count 500,000/mm3
Two images of the peripheral blood smear are shown on the image. Which of the following is the most appropriate next step in management?
- A. Phlebotomy
- B. Rituximab
- C. Watchful waiting
- D. Allogeneic stem cell transplantation
- E. Dasatinib (Correct Answer)
Management of chemotherapy toxicities Explanation: ***Dasatinib***
- The patient's presentation with **anemia**, **marked leukocytosis (65,000/mm³) with predominantly myeloid cells**, **thrombocytosis (500,000/mm³)**, and **splenomegaly (15 cm)** is highly suggestive of **Chronic Myeloid Leukemia (CML)**. The peripheral smear showing **myelocytes, metamyelocytes, and basophils** (indicated by arrows on the image) further supports this diagnosis.
- **Dasatinib** is a second-generation **tyrosine kinase inhibitor (TKI)** that targets the **BCR-ABL fusion protein**, which is the hallmark of CML. TKIs are the first-line treatment for CML.
*Phlebotomy*
- This is primarily used for **polycythemia vera** to reduce red blood cell mass and hematocrit.
- It is not indicated for CML, which is characterized by an overproduction of myeloid cells, not primarily red blood cells.
*Rituximab*
- **Rituximab** is a monoclonal antibody targeting the **CD20 antigen** on B-lymphocytes.
- It is used in the treatment of **B-cell non-Hodgkin lymphoma** and some autoimmune diseases, not CML.
*Watchful waiting*
- Given the patient's clear signs of **CML (leukocytosis, thrombocytosis, splenomegaly, and characteristic peripheral smear)**, active treatment is indicated, not watchful waiting.
- CML, if left untreated, progresses from the chronic phase to accelerated phase and then to **blast crisis**, which is rapidly fatal.
*Allogeneic stem cell transplantation*
- **Allogeneic stem cell transplantation** is a potentially curative treatment for CML.
- However, it is typically reserved for patients who have **failed TKI therapy** or have high-risk features, as **TKIs are the initial first-line treatment** due to their effectiveness and lower toxicity compared to transplantation.
Management of chemotherapy toxicities US Medical PG Question 6: A 71-year-old woman presents to her hematologist-oncologist for follow up after having begun doxorubicin and cyclophosphamide in addition to radiation therapy for the treatment of her stage 3 breast cancer. Her past medical history is significant for preeclampsia, hypertension, polycystic ovarian syndrome, and hypercholesterolemia. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 111/min, and respiratory rate 23/min. On physical examination, the pulses are strong and irregular, she has a grade 3/6 holosystolic murmur heard best at the left upper sternal border, clear bilateral breath sounds, and erythema over her site of radiation. Which of the following statements regarding doxorubicin is true?
- A. Doxorubicin has a maximum lifetime dose, due to the risk of cardiac toxicity (Correct Answer)
- B. Doxorubicin has a maximum lifetime dose, due to the risk of pulmonary toxicity
- C. Doxorubicin will increase her risk for deep vein thrombosis (DVT) and pulmonary embolism (PE)
- D. Doxorubicin frequently causes an acneiform rash
- E. Doxorubicin frequently causes cystitis
Management of chemotherapy toxicities Explanation: ***Doxorubicin has a maximum lifetime dose, due to the risk of cardiac toxicity***
- **Doxorubicin** is a potent chemotherapy agent (anthracycline) with a well-known risk of **cardiotoxicity**, which can lead to **dilated cardiomyopathy** and heart failure.
- To mitigate this severe side effect, a **cumulative lifetime dose limit** (usually 450-550 mg/m²) is established for doxorubicin.
*Doxorubicin has a maximum lifetime dose, due to the risk of pulmonary toxicity*
- While some chemotherapy agents can cause pulmonary toxicity, **doxorubicin** is not primarily associated with this as its main dose-limiting toxicity.
- The most significant and common dose-limiting toxicity of doxorubicin is **cardiotoxicity**, not pulmonary.
*Doxorubicin will increase her risk for deep vein thrombosis (DVT) and pulmonary embolism (PE)*
- Chemotherapy in general can increase the risk of **thromboembolic events**, but this is not a specific dose-limiting toxicity of **doxorubicin** that dictates a lifetime maximum dose.
- The concern for DVT/PE is a broader complication of cancer and its treatment, distinct from doxorubicin's specific cardiac risk.
*Doxorubicin frequently causes an acneiform rash*
- **Acneiform rash** is a common side effect of epidermal growth factor receptor (EGFR) inhibitors (e.g., cetuximab, erlotinib), not typically associated with **doxorubicin**.
- Doxorubicin's dermatologic side effects usually involve **alopecia**, hand-foot syndrome, and radiation recall, but not a predominant acneiform rash.
*Doxorubicin frequently causes cystitis*
- **Cystitis**, particularly hemorrhagic cystitis, is a well-known side effect of **cyclophosphamide** (another drug the patient is receiving), not **doxorubicin**.
- **Mesna** is often administered with cyclophosphamide to prevent this urological toxicity.
Management of chemotherapy toxicities US Medical PG Question 7: A 60-year-old man comes to the physician because of a 2-day history of blood in his urine, lower abdominal pain, and a burning sensation while micturating. Five months ago, he was diagnosed with high-grade non-Hodgkin lymphoma and a deep vein thrombosis of his right popliteal vein. His medications include polychemotherapy every 3 weeks and a daily subcutaneous dose of low molecular weight heparin. The last cycle of chemotherapy was 2 weeks ago. His temperature is 37°C (98.6°F), pulse is 94/min, and blood pressure is 110/76 mm Hg. Examination shows bilateral axillary and inguinal lymphadenopathy, hepatosplenomegaly, and mild suprapubic tenderness. Laboratory studies show:
Hemoglobin 10.2 g/dL
Leukocytes 4,300/mm3
Platelet count 145,000/mm3
Partial thromboplastin time 55 seconds
Prothrombin time 11 seconds (INR=1)
Urine
RBCs 50–55/hpf
RBC casts negative
WBCs 7/hpf
Epithelial cells 5/hpf
Bacteria occasional
Administration of which of the following is most likely to have prevented this patient's current condition?
- A. Ciprofloxacin
- B. Palifermin
- C. Mercaptoethane sulfonate (Correct Answer)
- D. Protamine sulfate
- E. Dexrazoxane
Management of chemotherapy toxicities Explanation: ***Mercaptoethane sulfonate***
- The patient's symptoms of **hematuria**, **lower abdominal pain**, and **dysuria** in the context of recent chemotherapy strongly suggest **hemorrhagic cystitis**. This is a known side effect of cyclophosphamide (or ifosfamide), which is often part of polychemotherapy for lymphoma.
- **Mercaptoethane sulfonate (MESNA)** is a chemoprotectant specifically used to detoxify the urotoxic metabolites (acrolein) of cyclophosphamide and ifosfamide, thereby preventing hemorrhagic cystitis.
*Ciprofloxacin*
- **Ciprofloxacin** is an antibiotic used to treat bacterial infections, particularly urinary tract infections. While the patient has some WBCs and occasional bacteria in his urine, his primary condition is most likely drug-induced hemorrhagic cystitis, not a bacterial UTI that would be prevented by ciprofloxacin.
- The context of recent chemotherapy points away from a primary bacterial infection as the cause of hematuria.
*Palifermin*
- **Palifermin** is a recombinant human keratinocyte growth factor used to prevent and treat **oral mucositis**, a common side effect of chemotherapy and radiation.
- It does not have any protective effect against hemorrhagic cystitis.
*Protamine sulfate*
- **Protamine sulfate** is used to reverse the anticoagulant effects of **heparin** and **low molecular weight heparin (LMWH)**. While the patient is on LMWH, the hematuria is more likely due to chemotherapy-induced cystitis rather than LMWH overdose, as his platelet count is reasonable and he has no other signs of widespread bleeding attributable to LMWH.
- Administering protamine sulfate would not prevent hemorrhagic cystitis.
*Dexrazoxane*
- **Dexrazoxane** is a cardioprotective agent used to reduce the incidence and severity of **anthracycline-induced cardiotoxicity** (e.g., from doxorubicin).
- It does not prevent or treat hemorrhagic cystitis caused by cyclophosphamide or ifosfamide.
Management of chemotherapy toxicities US Medical PG Question 8: A 67-year-old woman who was diagnosed with cancer 2 months ago presents to her oncologist with a 6-day history of numbness and tingling in her hands and feet. She is concerned that these symptoms may be related to progression of her cancer even though she has been faithfully following her chemotherapy regimen. She is not currently taking any other medications and has never previously experienced these symptoms. On physical exam, she is found to have decreased sensation to pinprick and fine touch over hands, wrists, ankles, and feet. Furthermore, she is found to have decreased reflexes throughout. Her oncologist assures her that these symptoms are a side effect from her chemotherapy regimen rather than progression of the cancer. The drug most likely responsible for her symptoms has which of the following mechanisms?
- A. Alkylation of DNA
- B. Inhibit folate metabolism
- C. DNA strand breaking
- D. Inhibit microtubule formation (Correct Answer)
- E. Prevention of nucleotide synthesis
Management of chemotherapy toxicities Explanation: ***Inhibit microtubule formation***
- The patient's symptoms of **numbness**, **tingling**, **decreased sensation** to pinprick and fine touch in a **stocking-glove distribution**, and **decreased reflexes** are characteristic of **peripheral neuropathy**.
- **Vinca alkaloids** (e.g., vincristine) and **taxanes** (e.g., paclitaxel, docetaxel) are chemotherapy agents that **inhibit microtubule formation**, and **peripheral neuropathy is their classic dose-limiting toxicity**.
- These agents are the **most strongly associated** with this specific adverse effect pattern among chemotherapy drugs.
*Alkylation of DNA*
- **Alkylating agents** (e.g., cyclophosphamide) and **platinum-based agents** (e.g., cisplatin, oxaliplatin) exert their cytotoxic effects by **cross-linking DNA strands**, preventing DNA replication and transcription.
- While **cisplatin and oxaliplatin can cause significant peripheral neuropathy**, the **microtubule inhibitors** (vinca alkaloids and taxanes) are **more classically associated** with this side effect and are the expected answer in this clinical context.
*Inhibit folate metabolism*
- This mechanism is characteristic of **antimetabolites** like **methotrexate**, which **inhibits dihydrofolate reductase**, thereby disrupting DNA synthesis.
- While methotrexate can have neurological side effects (particularly intrathecal administration causing neurotoxicity), **typical peripheral neuropathy is not its most common or direct adverse effect** related to this mechanism.
*DNA strand breaking*
- This mechanism is associated with agents like **etoposide** (a topoisomerase inhibitor) or **bleomycin** (which generates free radicals causing DNA strand breaks).
- While these drugs have various toxicities, they are **not typically associated with peripheral neuropathy** as their primary or most prominent side effect.
*Prevention of nucleotide synthesis*
- This is a broad mechanism shared by many **antimetabolites** (e.g., 5-fluorouracil, hydroxyurea, cytarabine) that interfere with the synthesis of purines or pyrimidines.
- While these agents can cause various adverse effects, **peripheral neuropathy is not a hallmark toxicity** as it is with drugs that target microtubules.
Management of chemotherapy toxicities US Medical PG Question 9: A 73-year-old woman recently diagnosed with colonic adenocarcinoma comes to the physician because of a 1-week history of nausea and multiple episodes of vomiting. These symptoms started shortly after her first infusion of oxaliplatin and fluorouracil. The patient is started on an appropriate medication. Three weeks later, at a follow-up appointment, she states that she has developed headaches and constipation. The patient was most likely treated with a drug with which of the following mechanisms of action?
- A. 5-HT3 receptor antagonist (Correct Answer)
- B. H1 receptor antagonist
- C. NK1 receptor antagonist
- D. Cannabinoid receptor agonist
- E. M2 receptor antagonist
Management of chemotherapy toxicities Explanation: ***5-HT3 receptor antagonist***
- The patient's symptoms of nausea and vomiting after **oxaliplatin and fluorouracil** chemotherapy are consistent with **chemotherapy-induced nausea and vomiting (CINV)**.
- **5-HT3 receptor antagonists** (e.g., ondansetron) are the primary treatment for CINV, and their common side effects include **headache and constipation**.
*H1 receptor antagonist*
- **H1 receptor antagonists** (e.g., diphenhydramine) can be used as antiemetics, but they are generally less effective for severe CINV and are associated with side effects such as **sedation and anticholinergic effects** (e.g., dry mouth), not typically headache and constipation as the primary concern.
- They work by blocking histamine-1 receptors in the **vomiting center**, but their efficacy in CINV is limited compared to 5-HT3 antagonists.
*NK1 receptor antagonist*
- **NK1 receptor antagonists** (e.g., aprepitant) are often used in combination with 5-HT3 antagonists and corticosteroids for highly emetogenic chemotherapy.
- While effective, their common side effect profile does not typically highlight **headache and constipation** as prominently as 5-HT3 antagonists do, and they are usually not chosen as a monotherapy first-line for moderate CINV.
*Cannabinoid receptor agonist*
- **Cannabinoid receptor agonists** (e.g., dronabinol) are used for CINV, especially in patients who do not respond to other antiemetics, and also to stimulate appetite.
- Their common side effects include **dizziness, euphoria, dysphoria**, and **hypotension**, but not typically headache and constipation as the most prominent adverse effects.
*M2 receptor antagonist*
- **M2 receptor antagonists** target muscarinic acetylcholine receptors, and while some anticholinergics might have antiemetic properties, using an M2-specific antagonist as a primary antiemetic for CINV is not standard practice.
- There are no commonly used antiemetics for CINV that specifically act as **M2 receptor antagonists**, and this class of drugs is more relevant in contexts such as heart rate regulation.
Management of chemotherapy toxicities US Medical PG Question 10: A 65-year-old male with diffuse large B cell lymphoma is treated with a chemotherapy regimen including 6-mercaptopurine. Administration of which of the following agents would increase this patient’s risk for mercaptopurine toxicity?
- A. Allopurinol (Correct Answer)
- B. Mesna
- C. Leucovorin
- D. Dexrazoxane
- E. Amifostine
Management of chemotherapy toxicities Explanation: ***Allopurinol***
- **Allopurinol** inhibits **xanthine oxidase**, an enzyme responsible for metabolizing **6-mercaptopurine (6-MP)** into inactive metabolites.
- Concurrent administration significantly increases **6-MP levels**, leading to enhanced myelotoxicity and other severe adverse effects.
*Mesna*
- **Mesna** (2-mercaptoethane sulfonate) is a uroprotectant used to prevent **hemorrhagic cystitis** caused by oxazaphosphorine chemotherapy agents like **ifosfamide** and **cyclophosphamide**.
- It does not interact with the metabolism of **6-mercaptopurine**.
*Leucovorin*
- **Leucovorin** (folinic acid) is a rescue agent for **methotrexate toxicity** and enhances the efficacy of **5-fluorouracil**.
- It does not have a direct interaction with the metabolism or toxicity of **6-mercaptopurine**.
*Dexrazoxane*
- **Dexrazoxane** is a cardioprotective agent used to prevent **doxorubicin-induced cardiotoxicity**.
- It does not interact with the metabolic pathways of **6-mercaptopurine**.
*Amifostine*
- **Amifostine** is a cytoprotective agent that reduces the toxicity of **cisplatin** and **radiation therapy** to normal tissues, particularly the kidneys and salivary glands.
- It is not involved in the metabolism or potentiation of **6-mercaptopurine toxicity**.
More Management of chemotherapy toxicities US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.