Hormonal therapies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hormonal therapies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hormonal therapies US Medical PG Question 1: A 68-year-old man presents to his primary care physician with a 4-week history of back pain. He says that the pain does not appear to be associated with activity and is somewhat relieved by taking an NSAID. Furthermore, he says that he has had increasing difficulty trying to urinate. His past medical history is significant for kidney stones and a 30-pack-year smoking history. Radiographs reveal osteoblastic lesions in the spine. Which of the following drugs would most likely be effective in treating this patient's disease?
- A. Imatinib
- B. Tamsulosin
- C. Pulsatile leuprolide
- D. Rituximab
- E. Continuous leuprolide (Correct Answer)
Hormonal therapies Explanation: ***Continuous leuprolide***
- The patient's presentation with **back pain**, urinary difficulties (**dysuria**), and **osteoblastic lesions** in an elderly male with a history of smoking is highly suggestive of **metastatic prostate cancer**.
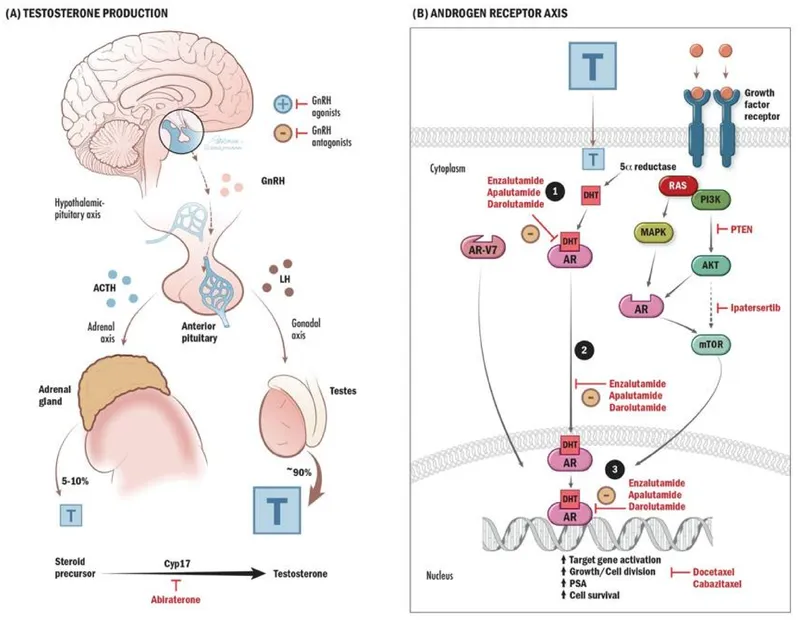
- **Continuous leuprolide** (a GnRH agonist) causes an initial surge in testosterone followed by downregulation of GnRH receptors leading to chemical castration, which is an effective treatment for hormone-sensitive prostate cancer.
*Imatinib*
- **Imatinib** is a **tyrosine kinase inhibitor** primarily used to treat **chronic myeloid leukemia (CML)** and gastrointestinal stromal tumors (GIST).
- It works by inhibiting the BCR-ABL tyrosine kinase in CML and KIT/PDGFRA in GIST, neither of which is relevant to prostate cancer.
*Tamsulosin*
- **Tamsulosin** is an **alpha-1 adrenergic antagonist** used to improve urinary flow in patients with **benign prostatic hyperplasia (BPH)**.
- While the patient has urinary difficulties, the presence of bone metastases (osteoblastic lesions) and back pain points towards malignancy, making BPH treatment alone insufficient.
*Pulsatile leuprolide*
- **Pulsatile leuprolide** administration (a GnRH agonist) mimics the natural pulsatile release of GnRH and is used to **stimulate gonadotropin release** for treating infertility.
- This would increase testosterone levels, which would be detrimental in the treatment of androgen-sensitive prostate cancer.
*Rituximab*
- **Rituximab** is a **monoclonal antibody** targeting the **CD20 antigen** found on B-lymphocytes.
- It is primarily used in the treatment of **non-Hodgkin lymphoma**, chronic lymphocytic leukemia, and certain autoimmune diseases, not prostate cancer.
Hormonal therapies US Medical PG Question 2: A 57-year-old presents to your clinic complaining of baldness. He is overweight, has been diagnosed with BPH, and is currently taking atorvastatin for hyperlipidemia. The patient has tried several over-the-counter products for hair-loss; however, none have been effective. After discussing several options, the patient is prescribed a medication to treat his baldness that has the additional benefit of treating symptoms of BPH as well. Synthesis of which of the following compounds would be expected to decrease in response to this therapy?
- A. Testosterone
- B. FSH
- C. LH
- D. GnRH
- E. DHT (Correct Answer)
Hormonal therapies Explanation: ***DHT***
- The medication described is likely **finasteride**, a **5-alpha-reductase inhibitor**. This enzyme converts **testosterone** to **dihydrotestosterone (DHT)**.
- Decreased DHT levels are beneficial for treating both **androgenetic alopecia (baldness)** and **benign prostatic hyperplasia (BPH)** due to its potent androgenic effects on hair follicles and prostate growth.
*Testosterone*
- While finasteride inhibits the conversion of testosterone to DHT, it does not directly decrease testosterone synthesis. In fact, **testosterone levels may slightly increase** as its conversion to DHT is blocked.
- Testosterone itself is not the primary androgen responsible for male pattern baldness or BPH; it's its more potent metabolite, DHT.
*FSH*
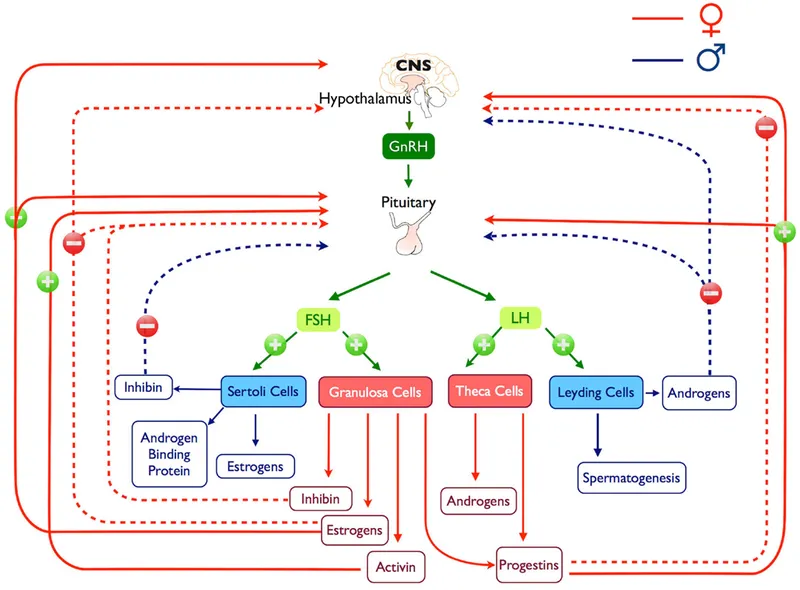
- **Follicle-stimulating hormone (FSH)** is a gonadotropin released from the anterior pituitary that stimulates sperm production and ovarian follicle development.
- The medication prescribed does not directly affect FSH synthesis or release; its action is peripheral, affecting androgen metabolism.
*LH*
- **Luteinizing hormone (LH)** is another gonadotropin that stimulates testosterone production in Leydig cells.
- The drug's mechanism of action is local inhibition of an enzyme, not a central regulation of pituitary hormones like LH.
*GnRH*
- **Gonadotropin-releasing hormone (GnRH)** is released from the hypothalamus and stimulates the anterior pituitary to release FSH and LH.
- This therapy specifically targets the conversion of an androgen and does not impact the hypothalamic-pituitary-gonadal axis at the level of GnRH.
Hormonal therapies US Medical PG Question 3: A 57-year-old woman comes to the physician for evaluation of a lump in the right breast that she first noticed a week ago. Biopsy of the mass confirms a diagnosis of a pleomorphic lobular carcinoma-in-situ that is estrogen receptor-positive. The patient undergoes lumpectomy, and treatment with tamoxifen is initiated. Which of the following conditions is most likely to occur as a result of tamoxifen therapy?
- A. Ovarian cancer
- B. Endometrial cancer (Correct Answer)
- C. Osteoporosis
- D. Myelosuppression
- E. Cardiotoxicity
Hormonal therapies Explanation: ***Endometrial cancer***
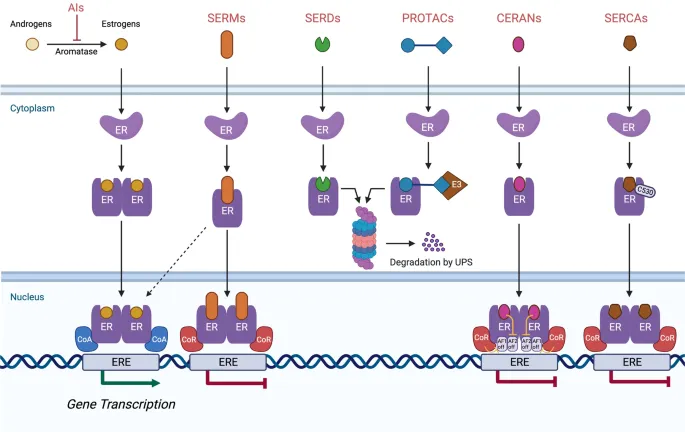
- Tamoxifen acts as an **estrogen receptor agonist** in the **endometrium**, stimulating endometrial proliferation.
- This proliferative effect significantly **increases the risk of endometrial hyperplasia** and **endometrial cancer** in postmenopausal women.
*Ovarian cancer*
- Tamoxifen is not directly linked to an increased risk of ovarian cancer.
- While it affects estrogen receptors, its primary oncogenic risk is specific to the endometrium due to its agonist activity there.
*Osteoporosis*
- Tamoxifen acts as an **estrogen receptor agonist in bone**, which has a protective effect against bone loss.
- Therefore, it typically **reduces the risk of osteoporosis**, especially in postmenopausal women, rather than causing it.
*Myelosuppression*
- Myelosuppression (bone marrow suppression) is a common side effect of many **chemotherapeutic agents**, but it is **not a typical side effect of tamoxifen**.
- Tamoxifen's mechanism of action as a selective estrogen receptor modulator (SERM) does not primarily target rapidly dividing hematopoietic cells.
*Cardiotoxicity*
- **Cardiotoxicity**, such as **cardiomyopathy** or **heart failure**, is a known side effect of certain oncology drugs like **anthracyclines** (e.g., doxorubicin) and some **HER2-targeted therapies** (e.g., trastuzumab).
- Tamoxifen is **not associated with significant cardiotoxicity**.
Hormonal therapies US Medical PG Question 4: A 27-year-old woman comes to the physician for the evaluation of infertility. She has been unable to conceive for the past 2 years. Menses occur at 45 to 80-day intervals. She is 168 cm (5 ft 6 in) tall and weighs 77 kg (170 lb); BMI is 27.4 kg/m2. Physical examination shows facial acne and pigmented hair on the upper lip. Serum studies show elevated levels of testosterone and an LH:FSH ratio of 4:1. Treatment with the appropriate drug for this patient's infertility is begun. Which of the following is the primary mechanism of action of this drug?
- A. Activation of pituitary dopamine receptors
- B. Activation of granulosa cell aromatase
- C. Activation of ovarian luteinizing hormone receptors
- D. Inhibition of hypothalamic estrogen receptors (Correct Answer)
- E. Inhibition of endometrial progesterone receptors
Hormonal therapies Explanation: ***Inhibition of hypothalamic estrogen receptors***
- The patient presents with classic symptoms of **polycystic ovarian syndrome (PCOS)**, including **oligomenorrhea** (menses every 45-80 days), **hirsutism**, **acne**, **elevated BMI**, **elevated testosterone**, and an **elevated LH:FSH ratio (4:1)**.
- **Clomiphene citrate** is the first-line drug for ovulation induction in PCOS patients with infertility.
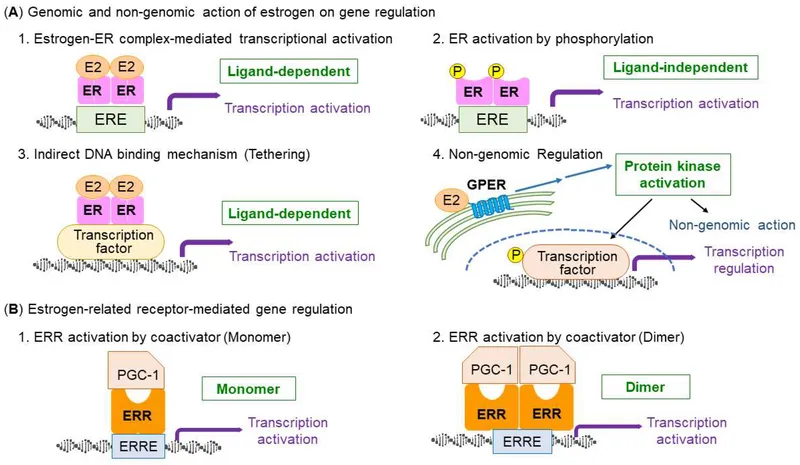
- Clomiphene is a **selective estrogen receptor modulator (SERM)** that acts as a **competitive antagonist at estrogen receptors in the hypothalamus**.
- By blocking estrogen receptors, clomiphene prevents normal **negative feedback inhibition** of GnRH release.
- This results in increased **GnRH pulsatility**, leading to increased **FSH and LH secretion** from the anterior pituitary, which promotes **follicular development and ovulation**.
*Activation of pituitary dopamine receptors*
- This mechanism is characteristic of **dopamine agonists** (e.g., **bromocriptine**, **cabergoline**), which are used to treat infertility due to **hyperprolactinemia**.
- These agents activate D2 receptors in lactotroph cells, inhibiting prolactin secretion.
- The patient shows no signs of hyperprolactinemia (e.g., galactorrhea, amenorrhea from elevated prolactin).
*Activation of granulosa cell aromatase*
- Aromatase converts androgens to estrogens in granulosa cells.
- While aromatase activity is important in follicular development, **activating aromatase is not a mechanism of any standard ovulation-inducing drug**.
- In PCOS, there is often relative aromatase insufficiency, but drugs do not directly activate this enzyme for fertility treatment.
*Activation of ovarian luteinizing hormone receptors*
- While **exogenous LH or hCG** (which acts on LH receptors) may be used in assisted reproductive technology, this is not the mechanism of **first-line ovulation induction** in PCOS.
- Clomiphene works by increasing endogenous LH/FSH release, not by directly activating ovarian receptors.
*Inhibition of endometrial progesterone receptors*
- This is the mechanism of **mifepristone** (RU-486), an antiprogestin used for medical abortion and occasionally for **endometriosis** or **uterine fibroids**.
- Inhibiting progesterone receptors would **prevent implantation** or disrupt pregnancy, which is opposite to the goal of fertility treatment.
Hormonal therapies US Medical PG Question 5: A 65-year-old woman arrives for her annual physical. She has no specific complaints. She has seasonal allergies and takes loratadine. She had a cholecystectomy 15 years ago. Her last menstrual period was 9 years ago. Both her mother and her maternal aunt had breast cancer. A physical examination is unremarkable. The patient is given the pneumococcal conjugate vaccine and the shingles vaccine. A dual-energy x-ray absorptiometry (DEXA) scan is obtained. Her T-score is -2.6. She is prescribed a new medication. The next month the patient returns to her primary care physician complaining of hot flashes. Which of the following is the most likely medication the patient was prescribed?
- A. Raloxifene (Correct Answer)
- B. Denosumab
- C. Teriparatide
- D. Zoledronic acid
- E. Alendronate
Hormonal therapies Explanation: ***Raloxifene***
- This patient has osteoporosis (T-score -2.6), increased **breast cancer risk** (family history), and postmenopausal status. **Raloxifene** is a **selective estrogen receptor modulator (SERM)** that treats osteoporosis and reduces breast cancer risk.
- The medication's **estrogen-antagonist effect** in the hypothalamus can cause or worsen **hot flashes**, a known side effect that explains her new complaint.
*Denosumab*
- **Denosumab** is a **monoclonal antibody** that inhibits osteoclast function, effectively treating osteoporosis.
- It works differently from SERMs and is **not associated with hot flashes** as a side effect.
*Teriparatide*
- **Teriparatide** is a **parathyroid hormone analog** that promotes bone formation, used for severe osteoporosis.
- It is not a SERM and does **not cause hot flashes** as a typical side effect.
*Zoledronic acid*
- **Zoledronic acid** is a **bisphosphonate** that inhibits osteoclast activity, effectively treating osteoporosis.
- While intravenous administration can cause flu-like symptoms, it is **not associated with hot flashes**.
*Alendronate*
- **Alendronate** is an **oral bisphosphonate** that reduces bone resorption in osteoporosis.
- Its side effect profile mainly involves gastrointestinal issues and esophageal irritation, and it does **not cause hot flashes**.
Hormonal therapies US Medical PG Question 6: A 46-year-old female with estrogen receptor positive invasive ductal carcinoma is prescribed tamoxifen. Which of the following is the MOST concerning side effect that requires patient counseling regarding potentially life-threatening complications?
- A. Increased risk of deep vein thrombosis (Correct Answer)
- B. Hot flashes and menopausal symptoms
- C. Improved bone density in postmenopausal women
- D. Increased risk of endometrial cancer
- E. Increased risk of hypertension
Hormonal therapies Explanation: ***Increased risk of deep vein thrombosis***
- Tamoxifen, a **selective estrogen receptor modulator (SERM)**, has estrogen receptor agonist effects in some tissues, including the coagulation system.
- This can lead to an increased risk of **thromboembolic events**, such as **deep vein thrombosis (DVT)** and **pulmonary embolism (PE)**, which are potentially life-threatening cardiovascular/hematologic complications.
*Hot flashes and menopausal symptoms*
- While tamoxifen commonly causes **hot flashes**, night sweats, and vaginal dryness due to its anti-estrogenic effects in the hypothalamus and vaginal tissue, these are generally a quality-of-life issue and not the **most concerning cardiovascular/hematologic side effect** requiring immediate intervention or counseling regarding life-threatening complications.
- These symptoms are usually manageable and anticipated but do not pose the same acute danger as a thromboembolic event.
*Improved bone density in postmenopausal women*
- Tamoxifen has **estrogen-agonist effects on bone**, leading to improved bone mineral density in postmenopausal women.
- This is generally considered a **beneficial side effect** rather than a concerning one, especially in women at risk for osteoporosis.
*Increased risk of hypertension*
- While cardiovascular side effects can occur with tamoxifen, a significantly increased risk of **hypertension** is not one of its primary or most concerning cardiovascular/hematologic complications.
- Blood pressure needs to be monitored, but DVT/PE risk is a far greater concern.
*Increased risk of endometrial cancer*
- Tamoxifen has **estrogen-agonist effects on the endometrium**, increasing the risk of **endometrial hyperplasia** and **endometrial cancer**.
- While this is a serious and well-known side effect that requires patient counseling and monitoring, it is an oncologic complication, not a cardiovascular or hematologic one.
Hormonal therapies US Medical PG Question 7: A 69-year-old man comes to the physician because of a 3-month history of urinary urgency, nocturia, and progressive pain in his lower back. The pain is worse at night and does not respond to ibuprofen. Rectal examination shows an enlarged, asymmetric prostate with a nodular surface. Prostate-specific antigen concentration is 11 ng/ml (N < 4). A biopsy of the prostate shows a high-grade adenocarcinoma. A CT scan of the pelvis shows multiple osteoblastic lesions of the lumbar spine. The patient is started on a drug that competes with androgens for interaction with the testosterone receptors. Treatment with which of the following drugs was most likely initiated in this patient?
- A. Docetaxel
- B. Flutamide (Correct Answer)
- C. Finasteride
- D. Degarelix
- E. Leuprolide
Hormonal therapies Explanation: ***Flutamide***
- The patient has **metastatic prostate cancer** with osteoblastic lesions, indicating a need for **androgen-deprivation therapy**. Flutamide is an **androgen receptor antagonist** that competes with androgens for binding to testosterone receptors.
- It is often used in combination with **GnRH agonists** (like leuprolide) to prevent **tumor flare** caused by the initial surge in testosterone, or as monotherapy in some cases.
*Docetaxel*
- **Docetaxel** is a **chemotherapeutic agent** (a taxane) used primarily for patients with **castration-resistant prostate cancer** or when hormonal therapies are no longer effective.
- It works by stabilizing microtubules, preventing cell division, and does not compete with androgens for testosterone receptors.
*Finasteride*
- **Finasteride** is a **5-alpha reductase inhibitor** that blocks the conversion of testosterone to **dihydrotestosterone (DHT)**, which is the more potent androgen in the prostate.
- It is used for **benign prostatic hyperplasia (BPH)** and **androgenic alopecia**, but not typically for metastatic prostate cancer as the primary treatment mechanism described.
*Degarelix*
- **Degarelix** is a **GnRH receptor antagonist** that directly suppresses the release of LH and FSH, leading to a rapid and sustained reduction in testosterone levels without an initial flare.
- While it causes androgen deprivation, it does not directly compete with androgens for binding to the testosterone receptors on cancer cells; its action is upstream.
*Leuprolide*
- **Leuprolide** is a **GnRH agonist** that initially causes a surge in LH and FSH, followed by downregulation and desensitization of the GnRH receptors, leading to reduced testosterone production.
- Like degarelix, it causes androgen deprivation, but it does not directly compete with androgens at the receptor level; its action is also upstream.
Hormonal therapies US Medical PG Question 8: A 40-year-old man presents with a painless firm mass in the right breast. Examination shows retraction of the nipple and the skin is fixed to the underlying mass. The axillary nodes are palpable. Which of the following statements is FALSE regarding the above condition?
- A. Lobular cancer is the most common breast cancer in males (Correct Answer)
- B. BRCA2 mutations are associated with increased risk
- C. These are positive for estrogen receptor
- D. Endocrine therapy plays an important role in treatment
- E. Gynecomastia may be caused by certain medications
Hormonal therapies Explanation: ***Lobular cancer is the most common breast cancer in males***
- This statement is **FALSE** and is the correct answer. The most common type of breast cancer in males is **invasive ductal carcinoma (IDC)**, accounting for about 80-90% of cases.
- **Invasive lobular carcinoma** is rare in men because men have very few lobules in their breast tissue.
*Gynecomastia may be caused by certain medications*
- This statement is **TRUE**. Medications such as spironolactone, cimetidine, finasteride, antipsychotics, and anabolic steroids can cause gynecomastia.
- However, the clinical presentation described (firm mass, nipple retraction, skin fixation, axillary nodes) is consistent with **malignancy**, not gynecomastia.
*BRCA2 mutations are associated with increased risk*
- This statement is **TRUE**. Male breast cancer is strongly associated with **BRCA2 mutations** (and less commonly BRCA1), which are hereditary.
- Men with BRCA2 mutations have a 5-10% lifetime risk of developing breast cancer, compared to less than 0.1% in the general male population.
*These are positive for estrogen receptor*
- This statement is **TRUE**. A vast majority (over 90%) of male breast cancers are **estrogen receptor (ER) positive**, which makes them responsive to endocrine therapy.
- This high rate of ER positivity is even greater than in female breast cancers.
*Endocrine therapy plays an important role in treatment*
- This statement is **TRUE**. Given the high prevalence of ER positivity (over 90%), endocrine therapy such as **tamoxifen** or aromatase inhibitors is a cornerstone of treatment for male breast cancer.
- Endocrine therapy is used in both adjuvant and metastatic settings for hormone receptor-positive disease.
Hormonal therapies US Medical PG Question 9: A 19-year-old South Asian male presents to the family physician concerned that he is beginning to go bald. He is especially troubled because his father and grandfather "went completely bald by the age of 25," and he is willing to try anything to prevent his hair loss. The family physician prescribes a medication that prevents the conversion of testosterone to dihydrotestosterone. Which of the following enzymes is inhibited by this medication?
- A. Cyclooxygenase 2
- B. Desmolase
- C. Aromatase
- D. cGMP phosphodiesterase
- E. 5-alpha-reductase (Correct Answer)
Hormonal therapies Explanation: ***5-alpha-reductase***
- The medication described inhibits the conversion of **testosterone to dihydrotestosterone (DHT)**, which is catalyzed by the enzyme **5-alpha-reductase**.
- **Androgenetic alopecia** (male pattern baldness) is driven by DHT, and inhibiting this enzyme reduces DHT levels in the scalp, thereby slowing hair loss.
*Cyclooxygenase 2*
- **Cyclooxygenase 2 (COX-2)** is involved in the synthesis of **prostaglandins** from arachidonic acid, mediating inflammation and pain.
- COX-2 inhibitors are used as anti-inflammatory drugs (e.g., celecoxib), not for male pattern baldness.
*Desmolase*
- **Cholesterol desmolase** (CYP11A1) is an enzyme that catalyzes the first committed step in **steroidogenesis**, converting cholesterol to pregnenolone.
- Inhibition of desmolase would affect the synthesis of all steroid hormones, not specifically target the conversion of testosterone to DHT for hair loss treatment.
*Aromatase*
- **Aromatase** is an enzyme responsible for converting androgens (like testosterone) into **estrogens**.
- Aromatase inhibitors are used in the treatment of estrogen-receptor positive breast cancer, not male pattern baldness.
*cGMP phosphodiesterase*
- **cGMP phosphodiesterase (PDE5)** is an enzyme that breaks down cyclic GMP (cGMP), which is involved in smooth muscle relaxation.
- PDE5 inhibitors (e.g., sildenafil) are used to treat **erectile dysfunction** and **pulmonary hypertension**, not hair loss.
Hormonal therapies US Medical PG Question 10: A 64-year-old woman presents to the clinic with a history of 3 fractures in the past year with the last one being last month. Her bone-density screening from last year reported a T-score of -3.1 and she was diagnosed with osteoporosis. She was advised to quit smoking and was asked to adapt to a healthy lifestyle to which she complied. She was also given calcium and vitamin D supplements. After a detailed discussion with the patient, the physician decides to start her on weekly alendronate. Which of the following statements best describes this patient’s new therapy?
- A. It should be stopped after 10 years due to the risk of esophageal cancer
- B. It is typically used as a second-line therapy for her condition after raloxifene
- C. It can cause hot flashes, flu-like symptoms, and peripheral edema
- D. It must be taken with the first meal of the day due to the significant risk of GI upset
- E. The patient must stay upright for at least 30 minutes after taking this medication (Correct Answer)
Hormonal therapies Explanation: ***The patient must stay upright for at least 30 minutes after taking this medication***
- This instruction is crucial for **alendronate** (a bisphosphonate) to prevent **esophageal irritation** and potential esophagitis or ulcers.
- Alendronate must be taken with a full glass of plain water on an **empty stomach** at least 30-60 minutes before the first food, beverage, or other medication of the day, and the patient must remain upright.
*It should be stopped after 10 years due to the risk of esophageal cancer*
- The main concern with long-term bisphosphonate use (usually >5 years for oral agents) is the risk of **atypical femoral fractures** and **osteonecrosis of the jaw**, not esophageal cancer.
- While esophageal irritation is a known side effect, the risk of esophageal cancer is **not the primary reason** for treatment discontinuation after 10 years.
*It is typically used as a second-line therapy for her condition after raloxifene*
- **Alendronate** (an oral bisphosphonate) is considered a **first-line therapy** for postmenopausal osteoporosis, especially in patients with a history of fractures and low T-scores.
- **Raloxifene** is a selective estrogen receptor modulator (SERM) typically used when bisphosphonates are contraindicated or not tolerated, or there is a need to also treat breast cancer risk, and it is **less potent** in reducing non-vertebral fractures.
*It can cause hot flashes, flu-like symptoms, and peripheral edema*
- These side effects (hot flashes, flu-like symptoms, peripheral edema) are **not typically associated** with alendronate.
- **Hot flashes** are more common with estrogen-modulating drugs like raloxifene, while **flu-like symptoms** can occur with IV bisphosphonates (like zoledronic acid) or certain anabolic agents.
*It must be taken with the first meal of the day due to the significant risk of GI upset*
- This statement is incorrect; alendronate must be taken on an **empty stomach** (at least 30-60 minutes before the first food or drink) to ensure adequate absorption.
- Taking it with food or other beverages significantly **reduces its absorption**, making it less effective, and the risk of GI upset (specifically esophageal irritation) is why remaining upright and taking with water are stressed.
More Hormonal therapies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.