Antitumor antibiotics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antitumor antibiotics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antitumor antibiotics US Medical PG Question 1: A 42-year-old man with non-small cell lung cancer is enrolled in a clinical trial for a new chemotherapeutic drug. The drug prevents microtubule depolymerization by binding to the beta subunit of tubulin. The mechanism of action of this new drug is most similar to which of the following?
- A. Bleomycin
- B. Irinotecan
- C. Vincristine
- D. Cladribine
- E. Paclitaxel (Correct Answer)
Antitumor antibiotics Explanation: ***Paclitaxel***
- **Paclitaxel** is a **taxane** that stabilizes microtubules by binding to the **beta-tubulin subunit**, preventing their depolymerization and arresting cells in metaphase.
- This mechanism is consistent with the described drug's action of preventing **microtubule depolymerization**.
*Bleomycin*
- **Bleomycin** is an **antitumor antibiotic** that causes **DNA strand breaks** by forming free radicals.
- Its mechanism is entirely different from microtubule stabilization.
*Irinotecan*
- **Irinotecan** is a **topoisomerase I inhibitor** that prevents DNA unwinding, leading to DNA damage and cell death.
- This drug targets DNA replication and repair, not microtubule dynamics.
*Vincristine*
- **Vincristine** is a **vinca alkaloid** that inhibits microtubule formation by binding to **beta-tubulin**, preventing its polymerization (assembly).
- While it also targets microtubules, its action is to *prevent polymerization*, whereas the new drug prevents *depolymerization*.
*Cladribine*
- **Cladribine** is a **purine analog** that inhibits DNA synthesis by incorporating into DNA and RNA, leading to strand breaks and cell death.
- This drug primarily interferes with nucleic acid metabolism, not microtubule function.
Antitumor antibiotics US Medical PG Question 2: A 71-year-old woman presents to her hematologist-oncologist for follow up after having begun doxorubicin and cyclophosphamide in addition to radiation therapy for the treatment of her stage 3 breast cancer. Her past medical history is significant for preeclampsia, hypertension, polycystic ovarian syndrome, and hypercholesterolemia. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 111/min, and respiratory rate 23/min. On physical examination, the pulses are strong and irregular, she has a grade 3/6 holosystolic murmur heard best at the left upper sternal border, clear bilateral breath sounds, and erythema over her site of radiation. Which of the following statements regarding doxorubicin is true?
- A. Doxorubicin has a maximum lifetime dose, due to the risk of cardiac toxicity (Correct Answer)
- B. Doxorubicin has a maximum lifetime dose, due to the risk of pulmonary toxicity
- C. Doxorubicin will increase her risk for deep vein thrombosis (DVT) and pulmonary embolism (PE)
- D. Doxorubicin frequently causes an acneiform rash
- E. Doxorubicin frequently causes cystitis
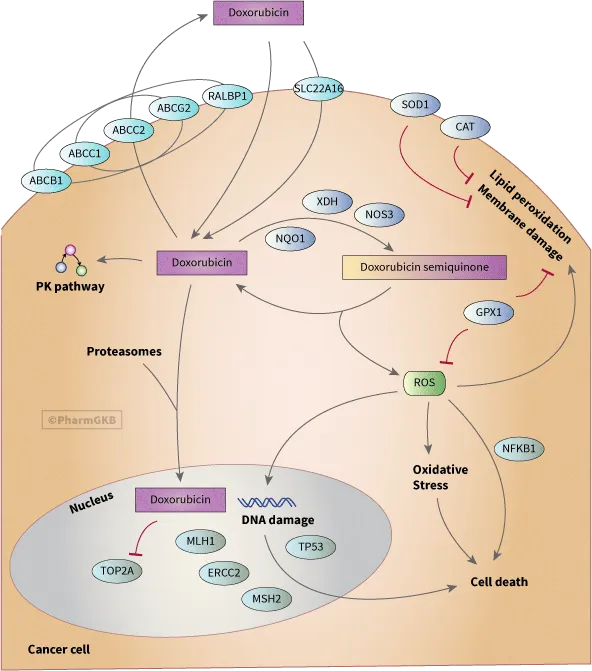
Antitumor antibiotics Explanation: ***Doxorubicin has a maximum lifetime dose, due to the risk of cardiac toxicity***
- **Doxorubicin** is a potent chemotherapy agent (anthracycline) with a well-known risk of **cardiotoxicity**, which can lead to **dilated cardiomyopathy** and heart failure.
- To mitigate this severe side effect, a **cumulative lifetime dose limit** (usually 450-550 mg/m²) is established for doxorubicin.
*Doxorubicin has a maximum lifetime dose, due to the risk of pulmonary toxicity*
- While some chemotherapy agents can cause pulmonary toxicity, **doxorubicin** is not primarily associated with this as its main dose-limiting toxicity.
- The most significant and common dose-limiting toxicity of doxorubicin is **cardiotoxicity**, not pulmonary.
*Doxorubicin will increase her risk for deep vein thrombosis (DVT) and pulmonary embolism (PE)*
- Chemotherapy in general can increase the risk of **thromboembolic events**, but this is not a specific dose-limiting toxicity of **doxorubicin** that dictates a lifetime maximum dose.
- The concern for DVT/PE is a broader complication of cancer and its treatment, distinct from doxorubicin's specific cardiac risk.
*Doxorubicin frequently causes an acneiform rash*
- **Acneiform rash** is a common side effect of epidermal growth factor receptor (EGFR) inhibitors (e.g., cetuximab, erlotinib), not typically associated with **doxorubicin**.
- Doxorubicin's dermatologic side effects usually involve **alopecia**, hand-foot syndrome, and radiation recall, but not a predominant acneiform rash.
*Doxorubicin frequently causes cystitis*
- **Cystitis**, particularly hemorrhagic cystitis, is a well-known side effect of **cyclophosphamide** (another drug the patient is receiving), not **doxorubicin**.
- **Mesna** is often administered with cyclophosphamide to prevent this urological toxicity.
Antitumor antibiotics US Medical PG Question 3: A 38-year-old woman is diagnosed with a stage IIIa infiltrating ductal carcinoma involving the left breast. The tumor is ER/PR positive, HER-2 negative, poorly differentiated Bloom-Richardson grade 3. 4/20 regional nodes are positive. The patient undergoes a lumpectomy with axillary lymph node dissection, followed by chemotherapy and radiation therapy to the left breast and axilla. Her chemotherapy regimen involves doxorubicin, cyclophosphamide, and paclitaxel. Following completion of the intensive phase, she is started on tamoxifen as an adjuvant therapy. 6 months later, she presents with increasing fatigue, orthopnea, and paroxysmal nocturnal dyspnea. Physical examination reveals the presence of an S3 gallop, jugular venous distension (JVD), pedal edema, and ascites. She is diagnosed with congestive cardiac failure and admitted for further management. An echocardiogram confirms the diagnosis of dilated cardiomyopathy with severe systolic dysfunction and an ejection fraction of 10%. Her medical history prior to the diagnosis of breast cancer is negative for any cardiac conditions. The baseline echocardiogram prior to starting chemotherapy and a 12-lead electrocardiogram were normal. Which of the following is most likely responsible for her current cardiac condition?
- A. Cyclophosphamide
- B. Radiation therapy
- C. Myocarditis
- D. Doxorubicin (Correct Answer)
- E. Tamoxifen
Antitumor antibiotics Explanation: ***Doxorubicin***
- **Doxorubicin** is a well-known anthracycline chemotherapy agent with a dose-dependent and cumulative cardiotoxic effect, often leading to **dilated cardiomyopathy** and congestive heart failure.
- The patient's presentation with **severe heart failure** symptoms and a dramatic drop in ejection fraction after chemotherapy strongly implicates doxorubicin as the cause.
*Cyclophosphamide*
- While **cyclophosphamide** can cause cardiac toxicity, particularly at high doses, it more commonly manifests as **myocarditis** or pericarditis rather than chronic dilated cardiomyopathy with severe systolic dysfunction as described.
- The cardiotoxicity of cyclophosphamide is generally less common and less severe than that of doxorubicin in typical breast cancer chemotherapy regimens.
*Radiation therapy*
- **Radiation therapy** to the chest can cause cardiac damage, including **pericarditis**, accelerated atherosclerosis, and restrictive cardiomyopathy.
- However, the timeframe for significant radiation-induced cardiomyopathy leading to such severe dilated heart failure is typically much longer, often years after treatment, not 6 months.
*Myocarditis*
- **Myocarditis** can cause heart failure, but it is typically an **inflammatory process** of the myocardium, often triggered by viral infections, and is usually an acute rather than a cumulative, treatment-induced effect in this context.
- While some chemotherapies can cause myocarditis, the clinical picture of a delayed, progressive cardiomyopathy with significantly reduced ejection fraction after specific cardiotoxic drugs points away from acute myocarditis as the primary cause.
*Tamoxifen*
- **Tamoxifen**, an antiestrogen used in ER/PR positive breast cancer, is generally not associated with significant **cardiotoxicity** or dilated cardiomyopathy.
- Its main cardiovascular side effects are usually related to an increased risk of **thromboembolic events**, not direct myocardial damage leading to heart failure.
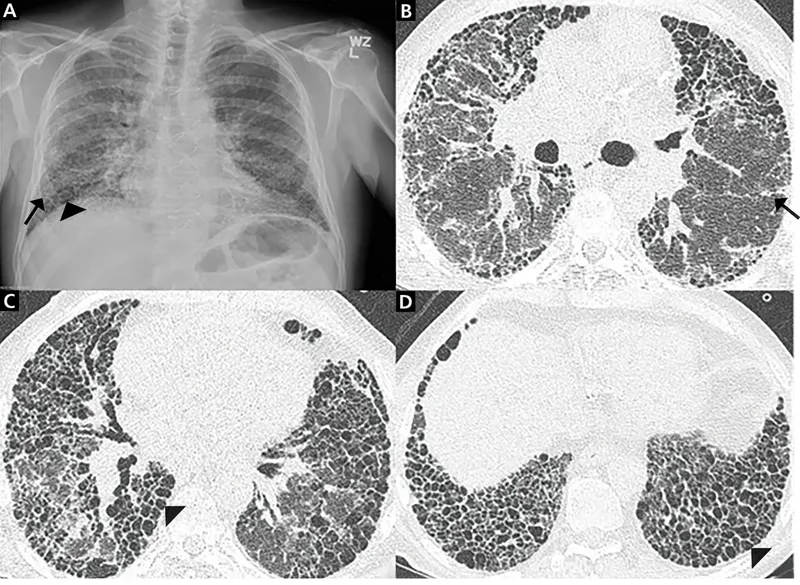
Antitumor antibiotics US Medical PG Question 4: A 27-year-old healthy college student presents to the clinic with her boyfriend complaining of a productive cough with rust-colored sputum associated with breathlessness for the past week. She also reports symptoms of the common cold which began about 1 week ago. She reports that her weekly routine has not changed despite feelings of being sick and generally weak. The vitals signs include a blood pressure 120/80 mm Hg, pulse rate 68/min, respiratory rate 12/min, and temperature 36.6°C (97.9°F). On pulmonary examination, inspiratory crackles were heard. The cardiac examination revealed an S3 sound but was otherwise normal. A chest X-ray was performed and is shown in the picture below. What medication is known to be associated with the same condition that she is suffering from?
- A. Metoprolol
- B. Quinidine
- C. Anthracyclines (Correct Answer)
- D. Vincristine
- E. Cisplatin
Antitumor antibiotics Explanation: ***Anthracyclines***
- The patient presents with symptoms of **heart failure**, specifically a productive cough with breathlessness, inspiratory crackles, and an **S3 heart sound**, suggestive of dilated cardiomyopathy potentially leading to pulmonary congestion. The Chest X-Ray and CT scans further corroborate the diagnosis of **pulmonary infiltrates and possible pulmonary edema**.
- **Anthracycline chemotherapy agents**, such as doxorubicin, are well-known for their cardiotoxic effects, leading to **dilated cardiomyopathy** and subsequent heart failure.
*Metoprolol*
- Metoprolol is a **beta-blocker** primarily used to treat hypertension, angina, and heart failure.
- It works by reducing heart workload and improving cardiac function, and is **not associated with causing heart failure** as a side effect.
*Quinidine*
- Quinidine is an **antiarrhythmic drug** (Class IA) used to treat various cardiac arrhythmias.
- Its main cardiac side effects include **prolongation of the QT interval** and potential for Torsades de Pointes, rather than dilated cardiomyopathy leading to heart failure.
*Vincristine*
- Vincristine is a **chemotherapeutic agent** (vinca alkaloid) primarily used in treating various cancers.
- Its main side effects include **neurotoxicity** (peripheral neuropathy) and myelosuppression, but it is not typically associated with cardiotoxicity or heart failure.
*Cisplatin*
- Cisplatin is a **platinum-based chemotherapeutic agent** used in a wide range of cancers.
- Its most common and significant side effects include **nephrotoxicity**, ototoxicity, and myelosuppression, with cardiotoxicity being rare and not its primary mode of adverse effect leading to heart failure.
Antitumor antibiotics US Medical PG Question 5: A 31-year-old female with a bacterial infection is prescribed a drug that binds the dipeptide D-Ala-D-Ala. Which of the following drugs was this patient prescribed?
- A. Polymyxin B
- B. Nalidixic acid
- C. Chloramphenicol
- D. Vancomycin (Correct Answer)
- E. Penicillin
Antitumor antibiotics Explanation: ***Vancomycin***
- **Vancomycin** is a glycopeptide antibiotic that directly binds to the **D-Ala-D-Ala** terminus of peptidoglycan precursors.
- This binding prevents the **transpeptidation** and **transglycosylation** steps required for bacterial cell wall synthesis, leading to cell lysis.
*Polymyxin B*
- **Polymyxins** are **cationic detergents** that disrupt the integrity of the bacterial **outer membrane** in Gram-negative bacteria.
- They bind to **lipopolysaccharide (LPS)**, causing increased permeability and leakage of intracellular components, but do not target D-Ala-D-Ala.
*Nalidixic acid*
- **Nalidixic acid** is a **quinolone antibiotic** that inhibits bacterial **DNA gyrase (topoisomerase II)** and **topoisomerase IV**.
- Its mechanism of action involves preventing DNA replication and transcription, not cell wall synthesis or D-Ala-D-Ala binding.
*Chloramphenicol*
- **Chloramphenicol** is an antibiotic that inhibits bacterial **protein synthesis** by binding to the **50S ribosomal subunit**.
- It prevents the formation of **peptide bonds** by inhibiting peptidyl transferase, an entirely different target from D-Ala-D-Ala in the cell wall.
*Penicillin*
- **Penicillin** is a beta-lactam antibiotic that inhibits bacterial cell wall synthesis by binding to and inactivating **penicillin-binding proteins (PBPs)**.
- PBPs are **transpeptidases** involved in cross-linking peptidoglycan, but penicillin does not directly bind to the D-Ala-D-Ala substrate itself; instead, it prevents the enzymes from using it.
Antitumor antibiotics US Medical PG Question 6: A 55-year-old male with a 60 pack-year smoking history presents to his oncologist for ongoing management of his recently diagnosed small cell lung cancer. His oncologist discusses several options and decides to start the chemotherapeutic medication, etoposide. The patient is warned that one side effect of this drug is myelosuppression so he should be vigilant for development of any infectious symptoms. The beneficial effect of this drug in treating cancer is most likely due to which of the following effects?
- A. DNA intercalation
- B. Crosslinking of DNA
- C. Stabilization of microtubules
- D. Alkylation of DNA
- E. Inhibition of supercoil relaxation (Correct Answer)
Antitumor antibiotics Explanation: ***Inhibition of supercoil relaxation***
- **Etoposide** is a **topoisomerase II inhibitor**, preventing DNA uncoiling and replication, thus causing DNA strand breaks and **apoptosis** in rapidly dividing cancer cells.
- This mechanism specifically targets the enzyme responsible for managing the topological state of DNA, a crucial process during cell division.
*DNA intercalation*
- **DNA intercalation** involves drugs inserting themselves between the base pairs of DNA, distorting its structure and inhibiting replication and transcription (e.g., **doxorubicin**).
- This is not the primary mechanism of action for **etoposide**, which directly interferes with topoisomerase II enzymes.
*Crosslinking of DNA*
- **Crosslinking of DNA** involves forming covalent bonds within or between DNA strands, preventing DNA replication and transcription (e.g., **cisplatin**, **cyclophosphamide**).
- While effective in chemotherapy, this mechanism is characteristic of **alkylating agents** and is distinct from how etoposide operates.
*Stabilization of microtubules*
- **Stabilization of microtubules** (e.g., **paclitaxel**, **docetaxel**) or destabilization (e.g., **vincristine**, **vinblastine**) are mechanisms of **microtubule-targeting agents** that disrupt cell division.
- **Etoposide** does not primarily affect microtubules but rather targets **DNA topoisomerases**.
*Alkylation of DNA*
- **Alkylation of DNA** involves the addition of an alkyl group to DNA bases, leading to DNA damage, miscoding, and ultimately cell death.
- This mechanism is typical of **alkylating agents** like **cyclophosphamide** and **busulfan**, but it is not the primary mode of action for **etoposide**.
Antitumor antibiotics US Medical PG Question 7: A 29-year-old female presents to her gynecologist complaining of a painful rash around her genitals. She has multiple sexual partners and uses condoms intermittently. Her last STD screen one year ago was negative. On examination, she has bilateral erosive vesicles on her labia majora and painful inguinal lymphadenopathy. She is started on an oral medication that requires a specific thymidine kinase for activation. Which of the following adverse effects is associated with this drug?
- A. Photosensitivity
- B. Deafness
- C. Renal failure (Correct Answer)
- D. Gingival hyperplasia
- E. Pulmonary fibrosis
Antitumor antibiotics Explanation: ***Renal failure***
- The patient's symptoms (painful genital rash, erosive vesicles, inguinal lymphadenopathy) are highly suggestive of **herpes simplex virus (HSV) infection**, likely genital herpes.
- The drug described is an antiviral agent like **acyclovir, valacyclovir, or famciclovir**, which require **viral thymidine kinase** for activation and are known to cause **renal impairment** (nephrotoxicity) as an adverse effect, especially with high doses or in dehydrated patients due to crystal nephropathy.
*Photosensitivity*
- **Photosensitivity** is a common side effect of some antibiotics (e.g., tetracyclines, sulfonamides), diuretics (e.g., thiazides), and antifungals, but it is **not a prominent adverse effect of acyclovir or its derivatives**.
- While theoretical, it is not a clinically significant or frequently observed adverse effect associated with the class of antiviral drugs used for HSV.
*Deafness*
- **Ototoxicity**, leading to deafness or hearing loss, is a well-known adverse effect of certain classes of drugs, such as **aminoglycoside antibiotics** (e.g., gentamicin) and **loop diuretics** (e.g., furosemide).
- It is **not an adverse effect** associated with antiviral medications like acyclovir.
*Gingival hyperplasia*
- **Gingival hyperplasia** (overgrowth of gum tissue) is a recognized side effect of specific medications including **phenytoin** (an anticonvulsant), **cyclosporine** (an immunosuppressant), and **calcium channel blockers** (e.g., nifedipine, amlodipine).
- This adverse effect is **not associated with antiviral drugs** used to treat herpes simplex.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a serious adverse effect linked to various drugs like **amiodarone** (an antiarrhythmic), **bleomycin** (a chemotherapeutic agent), **methotrexate** (an immunosuppressant/chemotherapeutic), and **nitrofurantoin** (an antibiotic).
- **Antiviral medications for HSV** do not typically cause pulmonary fibrosis.
Antitumor antibiotics US Medical PG Question 8: A 54-year-old woman is diagnosed with locally-advanced invasive ductal carcinoma of the breast. She undergoes surgical resection, radiation therapy, and is now being started on adjunctive chemotherapy with cyclophosphamide and doxorubicin. The patient is scheduled for follow up by her primary care provider. Which of the following tests should be performed regularly to monitor her current treatment regimen?
- A. No regular monitoring indicated
- B. Chest radiograph
- C. Cardiac MRI
- D. ECG
- E. Echocardiography (Correct Answer)
Antitumor antibiotics Explanation: ***Echocardiography***
- **Doxorubicin** is an anthracycline chemotherapy agent known for its dose-dependent **cardiotoxicity**, which can lead to **dilated cardiomyopathy** and heart failure.
- Regular echocardiography is crucial to monitor **left ventricular ejection fraction (LVEF)** and detect early signs of cardiac dysfunction, allowing for timely intervention or adjustment of treatment.
*No regular monitoring indicated*
- This is incorrect as **doxorubicin**, a component of the chemotherapy regimen, has significant cardiotoxic effects that require close monitoring to prevent severe cardiac complications.
- Neglecting monitoring could lead to irreversible cardiac damage.
*Chest radiograph*
- A chest radiograph primarily assesses lung fields and cardiac silhouette, but it is not sensitive enough to detect early-stage **doxorubicin-induced myocardial damage** or changes in **LVEF**.
- While useful for detecting pulmonary complications or metastases, it is not the primary tool for monitoring cardiotoxicity.
*Cardiac MRI*
- Cardiac MRI is a highly sensitive and specific imaging modality for assessing cardiac function and structure, but it is typically reserved for cases where echocardiography findings are equivocal or more detailed assessment is needed.
- It is not the routine or initial test for monitoring cardiotoxicity due to its higher cost and complexity.
*ECG*
- An ECG assesses the electrical activity of the heart and can detect arrhythmias or signs of ischemia, but it is generally not sufficient for monitoring **doxorubicin-induced cardiotoxicity**.
- While it can show nonspecific changes, it does not directly measure changes in **LVEF** or structural heart damage, which are key indicators of cardiotoxicity.
Antitumor antibiotics US Medical PG Question 9: A 72-year-old man has been recently diagnosed with stage 3 squamous cell carcinoma of the oral cavity. After the necessary laboratory workup, concurrent chemoradiation therapy has been planned. Radiation therapy is planned to take place over 7 weeks and he will receive radiation doses daily, Monday–Friday, in 2.0 Gy fractions. For concurrent chemotherapy, he will receive intravenous cisplatin at a dosage of 50 mg/m2 weekly for 7 weeks. Which of the following best explains the mechanism of action of the antineoplastic drug that the patient will receive?
- A. Free radical-mediated lipid peroxidation
- B. Inhibition of polymerization of tubulin
- C. Inhibition of topoisomerase 1
- D. Inhibition of topoisomerase 2
- E. Formation of interstrand DNA cross-links (Correct Answer)
Antitumor antibiotics Explanation: ***Formation of interstrand DNA cross-links***
- **Cisplatin** is a **platinum-based chemotherapeutic agent** that acts by forming **interstrand and intrastrand DNA cross-links**.
- These cross-links interfere with **DNA replication and transcription**, leading to **DNA damage** and ultimately **apoptosis** in cancer cells.
*Free radical-mediated lipid peroxidation*
- While some chemotherapeutic agents, like **anthracyclines**, can induce **free radical formation** and subsequent damage, this is not the primary mechanism of action for cisplatin.
- **Lipid peroxidation** primarily affects cell membranes, whereas cisplatin's main target is DNA.
*Inhibition of polymerization of tubulin*
- This mechanism of action is characteristic of **vinca alkaloids** (e.g., vincristine, vinblastine) and **taxanes** (e.g., paclitaxel, docetaxel), which disrupt microtubule formation and function.
- Cisplatin does not target **tubulin polymerization**.
*Inhibition of topoisomerase 1*
- **Topoisomerase 1 inhibitors** such as **irinotecan** and **topotecan** prevent DNA unwinding by stabilizing the cleavable complex, leading to DNA breaks.
- This is not how cisplatin exerts its therapeutic effects.
*Inhibition of topoisomerase 2*
- **Topoisomerase 2 inhibitors** like **etoposide** and **doxorubicin** interfere with DNA replication and repair by preventing the religation of DNA strands.
- Cisplatin's mechanism is distinct from topoisomerase inhibition.
Antitumor antibiotics US Medical PG Question 10: A 67-year-old woman with advanced bladder cancer comes to the physician for a follow-up examination. She is currently undergoing chemotherapy with an agent that forms cross-links between DNA strands. Serum studies show a creatinine concentration of 2.1 mg/dL and a blood urea nitrogen concentration of 30 mg/dL. Urine dipstick of a clean-catch midstream specimen shows 2+ protein and 1+ glucose. Prior to initiation of chemotherapy, her laboratory values were within the reference range. In addition to hydration, administration of which of the following would most likely have prevented this patient's current condition?
- A. Leucovorin
- B. Amifostine (Correct Answer)
- C. Aprepitant
- D. Mesna
- E. Rasburicase
Antitumor antibiotics Explanation: **Amifostine**
- This patient's symptoms (elevated creatinine and BUN, 2+ protein, 1+ glucose in urine) suggest **renal tubular damage**, specifically acute tubular necrosis, likely caused by a nephrotoxic chemotherapeutic agent.
- **Amifostine** is a cytoprotective agent that scavenges reactive oxygen species in local tissues, thereby reducing the nephrotoxic effects of **alkylating agents** like cisplatin, which forms cross-links between DNA strands.
*Leucovorin*
- **Leucovorin** (folinic acid) is used to rescue normal cells from the adverse effects of **methotrexate**, enhancing its excretion and reducing toxicity.
- It is not indicated for preventing kidney damage from DNA cross-linking agents.
*Aprepitant*
- **Aprepitant** is a neurokinin-1 (NK1) receptor antagonist used to prevent **chemotherapy-induced nausea and vomiting**.
- It does not have protective effects against nephrotoxicity.
*Mesna*
- **Mesna** (2-mercaptoethane sulfonate sodium) is used to prevent **hemorrhagic cystitis** caused by acrolein, a toxic metabolite of cyclophosphamide and ifosfamide.
- It does not prevent nephrotoxicity from other types of chemotherapy agents.
*Rasburicase*
- **Rasburicase** is a recombinant urate oxidase enzyme used to prevent or treat **tumor lysis syndrome** by converting uric acid to allantoin, which is more soluble and easily excreted.
- It is not used for preventing direct kidney damage from chemotherapeutic agents.
More Antitumor antibiotics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.