Vaccine adverse events US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vaccine adverse events. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vaccine adverse events US Medical PG Question 1: A 29-year-old man comes to the physician for a routine health maintenance examination. He feels well. He works as a nurse at a local hospital in the city. Three days ago, he had a needlestick injury from a patient whose serology is positive for hepatitis B. He completed the 3-dose regimen of the hepatitis B vaccine 2 years ago. His other immunizations are up-to-date. He appears healthy. Physical examination shows no abnormalities. He is concerned about his risk of being infected with hepatitis B following his needlestick injury. Serum studies show negative results for hepatitis B surface antigen, hepatitis B surface antibody, and hepatitis C antibody. Which of the following is the most appropriate next step in management?
- A. Revaccinate with 3-dose regimen of hepatitis B vaccine
- B. Revaccinate with two doses of hepatitis B vaccine
- C. Administer hepatitis B immunoglobulin
- D. Administer hepatitis B immunoglobulin and 3-dose regimen of hepatitis B vaccine (Correct Answer)
- E. Administer hepatitis B immunoglobulin and single dose hepatitis B vaccine
Vaccine adverse events Explanation: ***Administer hepatitis B immunoglobulin and 3-dose regimen of hepatitis B vaccine***
- This patient had prior vaccination but current serology shows **negative HBsAb**, indicating **non-response** to the vaccine (failure to develop protective antibodies).
- Given exposure to a hepatitis B positive patient, immediate post-exposure prophylaxis with **HBIG** is crucial for passive immunity and immediate protection.
- A **complete 3-dose revaccination series** should be initiated simultaneously, as per **CDC/ACIP guidelines** for vaccine non-responders with occupational exposure [1].
- This provides both immediate passive protection (HBIG) and attempts to establish active immunity through revaccination [1].
*Revaccinate with 3-dose regimen of hepatitis B vaccine*
- While revaccination is necessary due to the non-response, starting a 3-dose regimen alone without **HBIG** would leave the patient vulnerable during the initial period before vaccine response develops.
- After high-risk exposure in a non-responder, both passive (HBIG) and active (vaccine) immunity are required.
*Revaccinate with two doses of hepatitis B vaccine*
- A 2-dose regimen is insufficient; the standard revaccination schedule for non-responders is **3 doses** at 0, 1, and 6 months [1].
- Additionally, this option lacks **HBIG** for immediate protection after the high-risk exposure.
*Administer hepatitis B immunoglobulin*
- **HBIG** alone provides immediate passive immunity, which is crucial given the recent exposure and the patient's non-immune status.
- However, offering only HBIG without initiating active immunization (vaccine series) would leave the patient unprotected once the passive immunity wanes (approximately 3-6 months).
- This approach fails to address the need for long-term protection through revaccination.
*Administer hepatitis B immunoglobulin and single dose hepatitis B vaccine*
- While HBIG is appropriate for immediate protection, giving only a **single dose** of vaccine is inadequate.
- Standard post-exposure management for vaccine non-responders requires initiating a **complete 3-dose revaccination series**, not just one dose [1].
- A single dose would not provide adequate long-term protection for this non-responder.
Vaccine adverse events US Medical PG Question 2: An 18-year-old girl is brought to the emergency department because of a 1-day history of severe headache with photophobia and diffuse myalgias. She is a college student and lives in a dormitory in a large urban area. She has not traveled recently. On arrival, she is lethargic. Her temperature is 39.3°C (102.7°F), pulse is 120/min, and blood pressure is 88/58 mm Hg. Examination shows scattered petechiae and ecchymoses on the trunk and lower extremities. There is decreased range of motion of the neck. Cerebrospinal fluid analysis shows a cell count of 1,600/μL (80% neutrophils) and a lactate concentration of 5.1 mmol/L. Which of the following is most likely to have prevented this patient's condition?
- A. Intravenous vancomycin
- B. Polysaccharide conjugate vaccine (Correct Answer)
- C. Erythromycin therapy
- D. Doxycycline therapy
- E. Toxoid vaccine
Vaccine adverse events Explanation: ***Polysaccharide conjugate vaccine***
- This patient presents with symptoms highly suggestive of **bacterial meningitis** and **septic shock**, likely caused by *Neisseria meningitidis*, given the petechiae, ecchymoses, and rapid deterioration.
- A **meningococcal conjugate vaccine** would have provided protection against most common serogroups of *N. meningitidis* (A, C, W-135, Y) and is strongly recommended for college students living in dormitories due to increased risk of transmission.
*Intravenous vancomycin*
- This is an **acute treatment** for bacterial meningitis, specifically active against *Streptococcus pneumoniae* and some resistant strains.
- It would not have **prevented** the condition; preventative measures are typically vaccines or prophylactic antibiotics.
*Erythromycin therapy*
- Erythromycin is an antibiotic used for various bacterial infections, including atypical pneumonia and some skin infections.
- It is **not the primary prophylactic agent** for meningococcal disease and would not have prevented this specific condition.
*Doxycycline therapy*
- Doxycycline is a broad-spectrum antibiotic used for a range of infections, including tick-borne diseases and certain respiratory infections.
- It is **not indicated for the prevention** of meningococcal meningitis.
*Toxoid vaccine*
- **Toxoid vaccines** protect against diseases caused by bacterial toxins, such as tetanus and diphtheria.
- *Neisseria meningitidis* causes disease primarily through direct invasion and immune response to its capsular polysaccharides, not primarily exotoxins, so a toxoid vaccine would not be effective here.
Vaccine adverse events US Medical PG Question 3: A 12-month-old boy presents for a routine checkup. The patient immigrated from the Philippines with his parents a few months ago. No prior immunization records are available. The patient’s mother claims that he had a series of shots at 6 months of age which gave him a severe allergic reaction with swelling of the tongue and the face. She also remembers that he had the same reaction when she introduced solid foods to his diet, including carrots, eggs, and bananas. Which of the following vaccinations are not recommended for this patient?
- A. Measles, mumps, and rubella (MMR) vaccine
- B. Hepatitis B vaccine
- C. Varicella vaccine
- D. Intranasal influenza vaccine
- E. Intramuscular influenza vaccine (Correct Answer)
Vaccine adverse events Explanation: ***Important Note on Current Guidelines***
Based on **current CDC/ACIP guidelines (2023-2024)**, egg allergy alone is **no longer a contraindication** to influenza vaccines. However, this question tests knowledge of vaccine safety in the context of **severe anaphylaxis to a prior vaccination**.
***Intramuscular influenza vaccine***
- **Historically**, this was considered the most concerning option for patients with severe egg allergy, as many influenza vaccines were produced using egg-based culture methods
- **Current practice**: Per CDC guidelines, persons with egg allergy of any severity can receive any age-appropriate influenza vaccine, as egg protein content is minimal or absent in modern formulations
- However, if this patient had a **documented anaphylactic reaction to the influenza vaccine itself** (not just eggs), then it would be contraindicated
- Given the timing (6 months) and symptoms described, this represents the **historically correct answer**, though modern practice has evolved
*Measles, mumps, and rubella (MMR) vaccine*
- MMR vaccine is grown in **chick embryo fibroblast cells**, NOT in eggs, and contains **no egg protein**
- **Safe for patients with egg allergy** - no contraindication based on egg allergy
- Should be administered on schedule for catch-up immunization
*Hepatitis B vaccine*
- Produced using **recombinant DNA technology in yeast cells**
- Contains **no egg protein** and no animal-derived proteins
- **No contraindication** for this patient - safe to administer
*Varicella vaccine*
- Grown in **human diploid cell cultures**, NOT in eggs
- Contains **no egg protein**
- **Safe for patients with egg allergy** - no contraindication
- Should be administered as part of catch-up immunization
*Intranasal influenza vaccine (LAIV)*
- Like the intramuscular formulation, **current guidelines allow administration** to patients with egg allergy of any severity
- Contains similar or less egg protein than inactivated vaccines in modern formulations
- **Not contraindicated** based solely on egg allergy per current CDC guidelines
Vaccine adverse events US Medical PG Question 4: A 4-month-old boy is brought to the physician by his parents for a well-child examination. He has cystic fibrosis diagnosed by newborn screening. His parents report frequent feedings and large-volume and greasy stools. His 4-year-old brother has autism. Current medications include bronchodilators, pancreatic enzyme supplements, and fat-soluble vitamins. He is at the 18th percentile for height and 15th percentile for weight. Scattered wheezes are heard throughout both lung fields. Examination shows a distended and tympanic abdomen with no tenderness or guarding. Which of the following is a contraindication for administering one or more routine vaccinations?
- A. Allergy to egg protein
- B. History of cystic fibrosis
- C. History of febrile seizures
- D. Fever of 38.2°C (100.7°F) following previous vaccinations
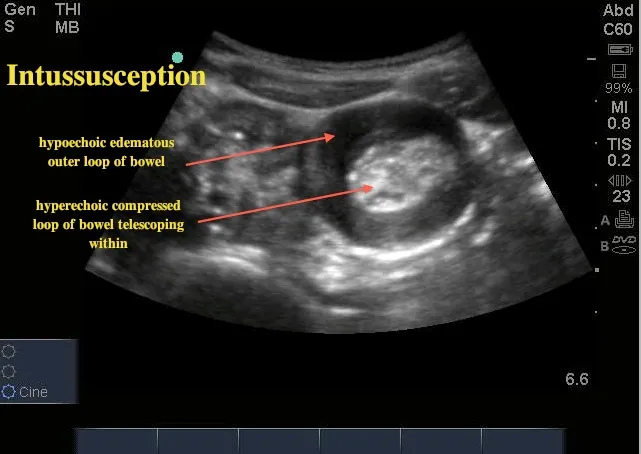
- E. History of intussusception (Correct Answer)
Vaccine adverse events Explanation: ***History of intussusception***
- A history of **intussusception** is a **contraindication for rotavirus vaccine** administration, as the vaccine itself has a small risk of intussusception, particularly with the first dose.
- The rotavirus vaccine is part of routine childhood immunizations, so this would be a contraindication for one of the routine vaccines.
*Allergy to egg protein*
- Egg allergy is a contraindication primarily for yellow fever vaccine and some influenza vaccines, which are typically not routine vaccinations for a 4-month-old. Many flu vaccines are egg-free or can be safely administered to those with egg allergy under supervision.
- The MMR vaccine is generally safe for those with egg allergy since the amount of egg protein is negligible.
*History of cystic fibrosis*
- **Cystic fibrosis** itself is **not a contraindication** to routine vaccinations; in fact, patients with chronic conditions like CF are often *more* encouraged to receive vaccinations to prevent severe infections.
- The patient's symptoms (poor growth, greasy stools, wheezing) are manifestations of CF, not reasons to defer vaccination.
*History of febrile seizures*
- A history of **febrile seizures** is generally **not a contraindication** to routine vaccinations.
- Parents should be counseled on fever management after vaccination, but the risk of recurrent febrile seizures is not increased by vaccination to a level that warrants deferral.
*Fever of 38.2°C (100.7°F) following previous vaccinations*
- A **low-grade fever** after vaccination is a common and **expected immune response**, not a contraindication for future doses.
- Only a **severe allergic reaction** (e.g., anaphylaxis) to a previous dose of a vaccine or one of its components is a contraindication to subsequent doses of that specific vaccine.
Vaccine adverse events US Medical PG Question 5: A young man about to leave for his freshman year of college visits his physician in order to ensure that his immunizations are up-to-date. Because he is living in a college dormitory, his physician gives him a vaccine that prevents meningococcal disease. What type of vaccine did this patient likely receive?
- A. Live, attenuated
- B. Killed, attenuated
- C. Toxoid
- D. Conjugated polysaccharide (Correct Answer)
- E. Killed, inactivated
Vaccine adverse events Explanation: ***Conjugated polysaccharide***
- The **meningococcal vaccine** commonly administered to college students is a **polysaccharide vaccine** wherein the polysaccharide antigens are conjugated to a protein carrier.
- This **conjugation** improves the immune response by converting a T-independent antigen into a T-dependent one, inducing better memory responses and allowing for vaccination of infants.
*Live, attenuated*
- Live, attenuated vaccines contain a **weakened form of the pathogen** that can replicate but does not cause disease, such as the MMR or varicella vaccine.
- While they elicit strong, long-lasting immunity, the meningococcal vaccine is not typically of this type due to the risk of opportunistic infection, especially in immunocompromised individuals.
*Killed, attenuated*
- This term is a **contradiction**; vaccines are either **killed (inactivated)** or **live (attenuated)**, but not both.
- Attenuation implies weakening, for which the organism would still be alive.
*Toxoid*
- **Toxoid vaccines** are made from inactivated bacterial toxins, used to protect against diseases where the toxin, not the bacterium itself, causes the disease, such as diphtheria and tetanus.
- Meningococcal disease is primarily caused by **direct bacterial invasion and inflammation**, not solely by a toxin.
*Killed, inactivated*
- **Killed, inactivated vaccines** contain whole pathogens that have been killed and cannot replicate, such as the inactivated poliovirus vaccine.
- While there are inactivated meningococcal vaccines, the most common type for broad use, especially in college settings, is the conjugated polysaccharide vaccine, which elicits a stronger and more long-lasting immune response against multiple serotypes compared to plain inactivated whole-cell vaccines.
Vaccine adverse events US Medical PG Question 6: A 14-year-old girl is brought to the physician after she accidentally cut her right forearm earlier that morning while working with her mother's embroidery scissors. She has no history of serious illness. The mother says she went to elementary and middle school abroad and is not sure if she received all of her childhood vaccinations. She appears healthy. Her temperature is 37°C (98.6 °F), pulse 90/min, and blood pressure is 102/68 mm Hg. Examination shows a clean 2-cm laceration on her right forearm with surrounding edema. There is no erythema or discharge. The wound is irrigated with water and washed with soap. Which of the following is the most appropriate next step in management?
- A. Administer Tdap only (Correct Answer)
- B. Administer DTaP only
- C. No further steps are necessary
- D. Administer TIG only
- E. Intravenous metronidazole
Vaccine adverse events Explanation: ***Administer Tdap only***
- A 14-year-old with an unknown or incomplete vaccination history requires a **Tdap (tetanus, diphtheria, acellular pertussis) booster** for **tetanus prophylaxis** after a wound.
- The wound is clean, and there are no signs of active infection or high-risk features that would necessitate tetanus immune globulin (TIG).
*Administer DTaP only*
- **DTaP (diphtheria, tetanus, acellular pertussis)** is typically administered to children younger than 7 years of age.
- This patient is 14 years old, making Tdap the more appropriate vaccine formulation for her age group.
*No further steps are necessary*
- Given the patient's **unknown vaccination history** and a laceration, tetanus prophylaxis is crucial to prevent **tetanus**, a potentially life-threatening condition.
- Simply cleaning the wound is insufficient protection without adequate vaccination status.
*Administer TIG only*
- **Tetanus immune globulin (TIG)** is typically reserved for patients with **dirty or severe wounds** and an unknown or incomplete vaccination history, or for those who are immunocompromised.
- This patient has a **clean laceration** with no indication of high-risk features that would warrant TIG.
*Intravenous metronidazole*
- **Metronidazole** is an antibiotic used to treat **anaerobic bacterial infections** and certain parasitic infections.
- The patient has no signs of infection (no erythema, discharge, or fever) that would necessitate antibiotic treatment at this time.
Vaccine adverse events US Medical PG Question 7: A 9-month-old boy is brought to a pediatrician by his parents for routine immunization. The parents say they have recently immigrated to the United States from a developing country, where the infant was receiving immunizations as per the national immunization schedule for that country. The pediatrician prepares a plan for the infant’s immunizations as per standard US guidelines. Looking at the plan, the parents ask why the infant needs to be vaccinated with injectable polio vaccine, as he had already received an oral polio vaccine back in their home country. The pediatrician explains to them that, as per the recommended immunization schedule for children and adolescents in the United States, it is important to complete the schedule of immunizations using the injectable polio vaccine (IPV). He also mentions that IPV is considered safer than OPV, and IPV has some distinct advantages over OPV. Which of the following statements best explains the advantage of IPV over OPV to which the pediatrician is referring?
- A. IPV is known to produce higher titers of mucosal IgG antibodies than OPV
- B. IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses
- C. IPV is known to produce higher titers of mucosal IgA antibodies than OPV
- D. IPV is known to produce higher titers of serum IgG antibodies than OPV (Correct Answer)
- E. IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells
Vaccine adverse events Explanation: ***IPV is known to produce higher titers of serum IgG antibodies than OPV***
- The **injectable polio vaccine (IPV)** is an **inactivated vaccine** that primarily induces a systemic immune response, leading to high levels of **serum IgG antibodies**. These antibodies are crucial for preventing **viremia** and subsequently protecting against paralytic poliomyelitis.
- While OPV (oral polio vaccine) induces both mucosal and humoral immunity, IPV's strength lies in its ability to generate robust systemic immunity without the risk of vaccine-associated paralytic polio (VAPP), a rare but serious complication of OPV.
*IPV is known to produce higher titers of mucosal IgG antibodies than OPV*
- IPV primarily stimulates **systemic immunity** rather than strong mucosal immunity, meaning it does not typically produce higher titers of mucosal IgG antibodies than OPV.
- Mucosal immunity, especially IgA, is better stimulated by vaccines administered orally, like **OPV**, as it directly interacts with the gut-associated lymphoid tissue.
*IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses*
- Both IPV and OPV can induce **CD4+ T cell responses**, but this statement does not highlight a distinct advantage of IPV over OPV.
- While CD4+ T cells are important for immune coordination and antibody production, the primary advantage of IPV is its **safety profile** and systemic antibody levels, not necessarily a superior CD4+ T cell response.
*IPV is known to produce higher titers of mucosal IgA antibodies than OPV*
- **OPV**, being an oral vaccine, is highly effective at inducing a strong **mucosal IgA response** in the gut, which is important for preventing viral shedding and transmission.
- **IPV**, administered parenterally, produces minimal to no mucosal IgA response, making this statement incorrect.
*IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells*
- **Cytotoxic CD8+ T cells** are primarily involved in clearing cells infected with intracellular pathogens.
- While both vaccines may induce some cellular immunity, their primary mechanism for protecting against polio is through **neutralizing antibodies**, and the induction of CD8+ T cells is not the principal advantage of IPV over OPV.
Vaccine adverse events US Medical PG Question 8: A 12-year-old boy, otherwise healthy, presents with frequent nosebleeds and lower extremity bruising. His mother reports that his symptoms started about 2 weeks ago and have not improved. The patient received the Tdap vaccine 2 weeks ago. He has no current medications. The review of systems is significant for the patient having a stomach ache after winning a hamburger eating competition 2 weeks ago. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 110/75 mm Hg, pulse 95/min, respirations 15/min, and oxygen saturation 99% on room air. On physical exam, the patient is alert and cooperative. The cardiac exam is normal. The lungs are clear to auscultation bilaterally. The lower extremities findings are shown in the image. Laboratory results are pending. Which of the following best describes the pathogenesis of this patient’s condition?
- A. Shiga-toxin mediated damage to vascular endothelium, resulting in microthrombi formation
- B. Systemic activation of clotting cascade resulting in platelet and coagulation factor consumption
- C. IgG autoantibodies against platelet glycoproteins (Correct Answer)
- D. Deposition of IgA immune complexes
- E. Deficiency of ADAMTS13
Vaccine adverse events Explanation: ***IgG autoantibodies against platelet glycoproteins***
- The patient's symptoms of **nosebleeds** and **bruising** (petechiae/purpura on lower extremities) following a recent **infection/illness** (stomach ache) and/or **vaccination** (Tdap) are highly suggestive of **immune thrombocytopenia (ITP)**.
- ITP involves the production of **autoantibodies**, usually IgG, that target **platelet glycoproteins** (e.g., GP IIb/IIIa), leading to accelerated platelet destruction by macrophages in the spleen.
*Shiga-toxin mediated damage to vascular endothelium, resulting in microthrombi formation*
- This describes the pathogenesis of **hemolytic uremic syndrome (HUS)**, typically caused by E. coli O157:H7 infection, leading to **thrombocytopenia**, microangiopathic hemolytic anemia, and acute kidney injury.
- While the patient had a stomach ache, there's no mention of **bloody diarrhea**, renal symptoms, or anemia to suggest HUS.
*Systemic activation of clotting cascade resulting in platelet and coagulation factor consumption*
- This describes **disseminated intravascular coagulation (DIC)**, a severe condition characterized by widespread activation of the coagulation system, leading to both **thrombosis** and bleeding.
- DIC is usually associated with severe underlying conditions like **sepsis**, trauma, or malignancy, and would typically present with more systemic involvement and deranged coagulation studies, which are not described.
*Deposition of IgA immune complexes*
- This is characteristic of **IgA vasculitis (Henoch-Schönlein purpura)**, which presents with a classic tetrad of **palpable purpura**, arthritis/arthralgia, abdominal pain, and renal disease.
- While the patient has lower extremity bruising and a history of abdominal pain, the absence of **palpable purpura** and systemic features like arthritis or renal involvement makes IgA vasculitis less likely than ITP given the prominent bleeding symptoms.
*Deficiency of ADAMTS13*
- A deficiency in **ADAMTS13** (a metalloprotease that cleaves vWF multimers) is the hallmark of **thrombotic thrombocytopenic purpura (TTP)**.
- TTP presents with the classic pentad of **thrombocytopenia**, microangiopathic hemolytic anemia, renal failure, neurological symptoms, and fever, none of which are fully described in this patient.
Vaccine adverse events US Medical PG Question 9: A 15-month-old girl is brought to her primary care physician for a follow-up visit to receive the 4th dose of her DTaP vaccine. She is up-to-date on her vaccinations. She received her 1st dose of MMR, 1st dose of varicella, 3rd dose of HiB, 4th dose of PCV13, and 3rd dose of polio vaccine 3 months ago. Thirteen days after receiving these vaccinations, the child developed a fever up to 40.5°C (104.9°F) and had one generalized seizure that lasted for 2 minutes. She was taken to the emergency department. The girl was sent home after workup for the seizure was unremarkable and her temperature subsided with acetaminophen therapy. She has not had any other symptoms since then. She has no history of serious illness and takes no medications. Her mother is concerned about receiving further vaccinations because she is afraid of the girl having more seizures. Her vital signs are within normal limits. Examination shows no abnormalities. Which of the following is the most appropriate recommendation at this time?
- A. Administration of the DTaP vaccine as scheduled (Correct Answer)
- B. Administration of the DTaP vaccine with valproic acid
- C. Administration of a reduced-dose DTaP vaccine
- D. Refrain from administration of the DTaP vaccine
- E. Administration of the DTaP vaccine with prophylactic aspirin
Vaccine adverse events Explanation: ***Administration of the DTaP vaccine as scheduled***
- The seizure experienced by the child was a **febrile seizure**, triggered by a fever following vaccination, and not a contraindication to future DTaP doses.
- The timing of the seizure (**13 days post-vaccination**) suggests it was most likely related to the **MMR vaccine**, which commonly causes delayed fever (5-12 days) and febrile seizures, rather than the pertussis component or other vaccines given simultaneously.
- Since the child did **not receive DTaP** at the visit when the febrile seizure occurred, there is no evidence that pertussis-containing vaccines trigger seizures in this patient.
- The **unremarkable workup** and the child's return to normal health indicate the seizure was benign and not indicative of an underlying seizure disorder or severe adverse reaction.
- **Simple febrile seizures are not a contraindication** to DTaP vaccination per CDC/ACIP guidelines.
*Administration of the DTaP vaccine with valproic acid*
- **Valproic acid** is an anti-epileptic drug and is not indicated for the prevention of simple febrile seizures following vaccination.
- Prophylactic use of anti-epileptic drugs for vaccination-related febrile seizures is generally not recommended due to potential side effects and lack of clear benefit.
*Administration of a reduced-dose DTaP vaccine*
- There is **no such thing as a reduced-dose DTaP vaccine** for standard administration in children of this age.
- Reducing the vaccine dose would compromise its efficacy and protective immunity.
*Refrain from administration of the DTaP vaccine*
- **Febrile seizures are not a contraindication** to receiving further DTaP vaccination.
- Withholding the vaccine would leave the child unprotected against **diphtheria, tetanus, and pertussis**, which are serious and potentially life-threatening diseases.
*Administration of the DTaP vaccine with prophylactic aspirin*
- **Aspirin is contraindicated in children** due to the risk of **Reye's syndrome**, especially during viral illnesses or when fever is present.
- It should not be used as a prophylactic measure for vaccination-related fever or seizures.
Vaccine adverse events US Medical PG Question 10: A 4-year-old boy is brought to the emergency department with difficulty breathing. His mother reports that he developed a fever last night and began to have trouble breathing this morning. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is unvaccinated (conscientious objection by the family) and is meeting all developmental milestones. At the hospital, his vitals are temperature 39.8°C (103.6°F), pulse 122/min, respiration rate 33/min, blood pressure 110/66 mm Hg, and SpO2 93% on room air. On physical examination, he appears ill with his neck hyperextended and chin protruding. His voice is muffled and is drooling. The pediatrician explains that there is one particular bacteria that commonly causes these symptoms. At what age should the patient have first received vaccination to prevent this condition from this particular bacteria?
- A. At birth
- B. At 2-months-old (Correct Answer)
- C. Between 9- and 12-months-old
- D. At 6-months-old
- E. Between 12- and 15-months-old
Vaccine adverse events Explanation: ***At 2-months-old***
- The clinical presentation with **high fever**, **difficulty breathing**, **neck hyperextension**, **muffled voice**, and **drooling** in an unvaccinated child strongly suggests **epiglottitis**, likely caused by *Haemophilus influenzae type b* (Hib).
- The **Hib vaccine** is routinely given starting at **2 months of age** as part of the multi-dose primary series to protect against this life-threatening condition.
*At birth*
- While some vaccines like **Hepatitis B** are given at birth, the Hib vaccine is not typically administered at this age.
- Vaccinating at birth would not align with the standard immunization schedule for *Haemophilus influenzae type b*.
*Between 9- and 12-months-old*
- This age range typically corresponds to the **measles, mumps, and rubella (MMR)** and **varicella** vaccines, or a booster dose of other vaccines, not the initial primary series for Hib.
- Delaying the first Hib vaccination until this age would leave infants vulnerable during a critical period.
*At 6-months-old*
- By 6 months, a child should have already received at least **two doses** of the Hib vaccine if following the recommended schedule.
- Administering the first dose at 6 months would significantly delay protection against invasive Hib disease.
*Between 12- and 15-months-old*
- This age range is typically when the **final booster dose** of the Hib vaccine is given, not the initial vaccination.
- The primary series for Hib should have been completed much earlier to provide timely protection.
More Vaccine adverse events US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.