New and emerging vaccines US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for New and emerging vaccines. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
New and emerging vaccines US Medical PG Question 1: A 40-year-old pregnant woman, G4 P3, visits your office at week 30 of gestation. She is very excited about her pregnancy and wants to be the healthiest she can be in preparation for labor and for her baby. What vaccination should she receive at this visit?
- A. Measles, mumps, and rubella (MMR)
- B. Varicella vaccine
- C. Herpes zoster vaccine
- D. Live attenuated influenza vaccine
- E. Tetanus, diphtheria, and acellular pertussis (Tdap) (Correct Answer)
New and emerging vaccines Explanation: ***Tetanus, diphtheria, and acellular pertussis (Tdap)***
- The Tdap vaccine is recommended during each pregnancy, preferably between **27 and 36 weeks of gestation**, to maximize maternal antibody response and passive antibody transfer to the fetus.
- This provides critical protection against **pertussis (whooping cough)** for the newborn, who is too young to be vaccinated.
*Measles, mumps, and rubella (MMR)*
- The **MMR vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital rubella syndrome, although no cases have been reported.
- It should be administered **postpartum** if the mother is not immune to rubella.
*Varicella vaccine*
- The **varicella vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital varicella syndrome.
- Like MMR, it should be offered in the **postpartum period** if the woman is not immune.
*Herpes zoster vaccine*
- The herpes zoster vaccine is typically recommended for **older adults** (50 years and older) for shingles prevention.
- It is **not routinely recommended during pregnancy**, and its safety and efficacy in this population have not been sufficiently established.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is **contraindicated during pregnancy** due to its live virus content.
- Pregnant women should receive the **inactivated influenza vaccine (IIV)**, which is safe and recommended during any trimester.
New and emerging vaccines US Medical PG Question 2: A 2-year-old boy is brought in by his parents to his pediatrician. The boy was born by spontaneous vaginal delivery at 39 weeks and 5 days after a normal pregnancy. The boy has received all age-appropriate vaccinations as of his last visit at 18 months of age. Of note, the boy has confirmed sickle cell disease and the only medication he takes is penicillin prophylaxis. The parents state that they plan on enrolling their son in a daycare, which requires documentation of up-to-date vaccinations. The pediatrician states that their son needs an additional vaccination at this visit, which is a polysaccharide vaccine that is not conjugated to protein. Which of the following matches this description?
- A. Pneumovax (Correct Answer)
- B. Menactra
- C. Prevnar
- D. Hib vaccine
- E. Live attenuated influenza vaccine
New and emerging vaccines Explanation: ***Pneumovax***
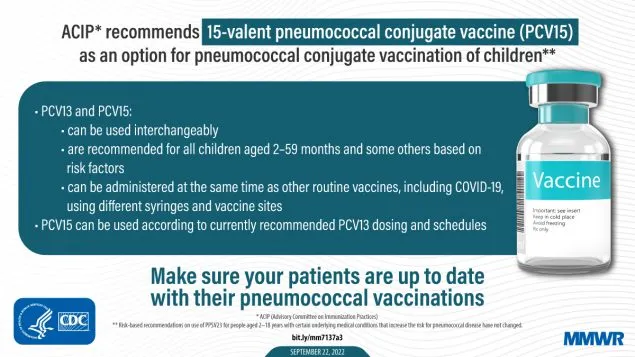
- **Pneumovax** (PCV23, PPSV23) is a **polysaccharide vaccine** that is not conjugated to a protein carrier. Children with **sickle cell disease** should receive this vaccine due to their immunocompromised state and increased risk of encapsulated bacterial infections.
- The Centers for Disease Control and Prevention (CDC) recommends PPSV23 for children aged 2 years and older with chronic medical conditions such as **sickle cell disease**, usually administered 8 weeks after their last PCV13 dose.
*Menactra*
- **Menactra** is a **quadrivalent meningococcal conjugate vaccine** (MCV4), meaning it contains a polysaccharide antigen conjugated to a protein carrier.
- This vaccine primarily targets *Neisseria meningitidis* and is different from the pneumococcal vaccine required here.
*Prevnar*
- **Prevnar** (PCV13) is a **pneumococcal conjugate vaccine**, meaning its polysaccharide antigens are conjugated to a protein carrier.
- While important for children with sickle cell disease, the question specifically asks for a vaccination that is a **polysaccharide vaccine that is not conjugated to protein**.
*Hib vaccine*
- The **Hib vaccine** (against *Haemophilus influenzae* type b) is a **conjugate vaccine**, meaning its polysaccharide capsule is linked to a protein carrier to enhance immunogenicity, particularly in infants.
- This vaccine is typically given earlier in childhood and is not the "additional" unconjugated polysaccharide vaccine described.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is a live virus vaccine, not a polysaccharide vaccine.
- It is also contraindicated in individuals with certain immunocompromising conditions, such as some patients with sickle cell disease.
New and emerging vaccines US Medical PG Question 3: A young man about to leave for his freshman year of college visits his physician in order to ensure that his immunizations are up-to-date. Because he is living in a college dormitory, his physician gives him a vaccine that prevents meningococcal disease. What type of vaccine did this patient likely receive?
- A. Live, attenuated
- B. Killed, attenuated
- C. Toxoid
- D. Conjugated polysaccharide (Correct Answer)
- E. Killed, inactivated
New and emerging vaccines Explanation: ***Conjugated polysaccharide***
- The **meningococcal vaccine** commonly administered to college students is a **polysaccharide vaccine** wherein the polysaccharide antigens are conjugated to a protein carrier.
- This **conjugation** improves the immune response by converting a T-independent antigen into a T-dependent one, inducing better memory responses and allowing for vaccination of infants.
*Live, attenuated*
- Live, attenuated vaccines contain a **weakened form of the pathogen** that can replicate but does not cause disease, such as the MMR or varicella vaccine.
- While they elicit strong, long-lasting immunity, the meningococcal vaccine is not typically of this type due to the risk of opportunistic infection, especially in immunocompromised individuals.
*Killed, attenuated*
- This term is a **contradiction**; vaccines are either **killed (inactivated)** or **live (attenuated)**, but not both.
- Attenuation implies weakening, for which the organism would still be alive.
*Toxoid*
- **Toxoid vaccines** are made from inactivated bacterial toxins, used to protect against diseases where the toxin, not the bacterium itself, causes the disease, such as diphtheria and tetanus.
- Meningococcal disease is primarily caused by **direct bacterial invasion and inflammation**, not solely by a toxin.
*Killed, inactivated*
- **Killed, inactivated vaccines** contain whole pathogens that have been killed and cannot replicate, such as the inactivated poliovirus vaccine.
- While there are inactivated meningococcal vaccines, the most common type for broad use, especially in college settings, is the conjugated polysaccharide vaccine, which elicits a stronger and more long-lasting immune response against multiple serotypes compared to plain inactivated whole-cell vaccines.
New and emerging vaccines US Medical PG Question 4: To protect against a potentially deadly infection, a 19-year-old female receives a vaccine containing capsular polysaccharide. This vaccine will stimulate her immune system to produce antibodies against which organism?
- A. Corynebacterium diphtheriae
- B. Neisseria meningitidis (Correct Answer)
- C. Streptococcus pneumoniae
- D. Clostridium tetani
- E. Haemophilus influenzae type b
New and emerging vaccines Explanation: ***Neisseria meningitidis***
- The vaccine described, containing **capsular polysaccharide**, targets the **polysaccharide capsule** of *Neisseria meningitidis*, which is a key virulence factor.
- This bacterium causes **meningococcal meningitis**, a potentially deadly infection, especially in adolescents and young adults.
- The **meningococcal vaccine** is specifically recommended for adolescents and college students due to increased risk in this population.
*Corynebacterium diphtheriae*
- The vaccine against *C. diphtheriae* is a **toxoid vaccine**, meaning it contains an inactivated form of the **diphtheria toxin**, not capsular polysaccharide.
- This vaccine primarily protects against the effects of the **exotoxin**, which causes major symptoms like myocarditis and neuropathy.
*Streptococcus pneumoniae*
- While *S. pneumoniae* also has a **capsular polysaccharide vaccine** (PPSV23 and PCV13), it is primarily recommended for **young children, elderly adults, and immunocompromised patients**.
- A **19-year-old healthy female** would not routinely receive pneumococcal vaccine unless she had specific risk factors.
- The question context of a "potentially deadly infection" in this age group more specifically points to meningococcus.
*Clostridium tetani*
- The vaccine for *C. tetani* is a **tetanus toxoid vaccine**, similar to diphtheria, targeting the inactivated **tetanospasmin toxin** produced by the bacterium.
- This vaccine prevents the neurological symptoms of tetanus by neutralizing the toxin, not by targeting capsular polysaccharides.
*Haemophilus influenzae type b*
- While *H. influenzae* type b also has a **capsular polysaccharide-based vaccine** (conjugate vaccine), it is primarily given to **infants and young children** as part of routine childhood immunization.
- A 19-year-old would have already received this vaccine in childhood, and it is not routinely given to adolescents or adults.
- The age group and clinical context make meningococcus the more likely answer.
New and emerging vaccines US Medical PG Question 5: A 9-month-old boy is brought to a pediatrician by his parents for routine immunization. The parents say they have recently immigrated to the United States from a developing country, where the infant was receiving immunizations as per the national immunization schedule for that country. The pediatrician prepares a plan for the infant’s immunizations as per standard US guidelines. Looking at the plan, the parents ask why the infant needs to be vaccinated with injectable polio vaccine, as he had already received an oral polio vaccine back in their home country. The pediatrician explains to them that, as per the recommended immunization schedule for children and adolescents in the United States, it is important to complete the schedule of immunizations using the injectable polio vaccine (IPV). He also mentions that IPV is considered safer than OPV, and IPV has some distinct advantages over OPV. Which of the following statements best explains the advantage of IPV over OPV to which the pediatrician is referring?
- A. IPV is known to produce higher titers of mucosal IgG antibodies than OPV
- B. IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses
- C. IPV is known to produce higher titers of mucosal IgA antibodies than OPV
- D. IPV is known to produce higher titers of serum IgG antibodies than OPV (Correct Answer)
- E. IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells
New and emerging vaccines Explanation: ***IPV is known to produce higher titers of serum IgG antibodies than OPV***
- The **injectable polio vaccine (IPV)** is an **inactivated vaccine** that primarily induces a systemic immune response, leading to high levels of **serum IgG antibodies**. These antibodies are crucial for preventing **viremia** and subsequently protecting against paralytic poliomyelitis.
- While OPV (oral polio vaccine) induces both mucosal and humoral immunity, IPV's strength lies in its ability to generate robust systemic immunity without the risk of vaccine-associated paralytic polio (VAPP), a rare but serious complication of OPV.
*IPV is known to produce higher titers of mucosal IgG antibodies than OPV*
- IPV primarily stimulates **systemic immunity** rather than strong mucosal immunity, meaning it does not typically produce higher titers of mucosal IgG antibodies than OPV.
- Mucosal immunity, especially IgA, is better stimulated by vaccines administered orally, like **OPV**, as it directly interacts with the gut-associated lymphoid tissue.
*IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses*
- Both IPV and OPV can induce **CD4+ T cell responses**, but this statement does not highlight a distinct advantage of IPV over OPV.
- While CD4+ T cells are important for immune coordination and antibody production, the primary advantage of IPV is its **safety profile** and systemic antibody levels, not necessarily a superior CD4+ T cell response.
*IPV is known to produce higher titers of mucosal IgA antibodies than OPV*
- **OPV**, being an oral vaccine, is highly effective at inducing a strong **mucosal IgA response** in the gut, which is important for preventing viral shedding and transmission.
- **IPV**, administered parenterally, produces minimal to no mucosal IgA response, making this statement incorrect.
*IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells*
- **Cytotoxic CD8+ T cells** are primarily involved in clearing cells infected with intracellular pathogens.
- While both vaccines may induce some cellular immunity, their primary mechanism for protecting against polio is through **neutralizing antibodies**, and the induction of CD8+ T cells is not the principal advantage of IPV over OPV.
New and emerging vaccines US Medical PG Question 6: An 18-year-old woman presents for a routine check-up. She is a college student with no complaints. She has a 2 pack-year history of smoking and consumes alcohol occasionally. Her sexual debut was at 15 years of age and has had 2 sexual partners. She takes oral contraceptives and uses barrier contraception. Her family history is significant for cervical cancer in her aunt. Which of the following statements regarding cervical cancer screening in this patient is correct?
- A. The patient requires annual Pap testing due to her family history of cervical cancer.
- B. HPV testing is more preferable than Pap testing in sexually active women under 21 years of age.
- C. It is reasonable to start Pap-test screening at the current visit and repeat it every 3 years.
- D. The patient should undergo screening every 3 years after she turns 21 years of age. (Correct Answer)
- E. The patient does not require Pap testing as long as she uses barrier contraception.
New and emerging vaccines Explanation: **The patient should undergo screening every 3 years after she turns 21 years of age.**
- Current guidelines recommend initiating cervical cancer screening at **age 21**, regardless of sexual activity.
- The recommended interval for cytology-only screening is **every 3 years** for women aged 21-29.
*The patient requires annual Pap testing due to her family history of cervical cancer.*
- **Family history of cervical cancer** is generally not considered a reason for earlier or more frequent screening in individuals under 21 years of age, unless specific genetic syndromes are suspected, which is not mentioned here.
- The primary risk factor for cervical cancer is **HPV infection**, not direct family history.
*HPV testing is more preferable than Pap testing in sexually active women under 21 years of age.*
- **HPV testing** as a primary screening method is **not recommended for women younger than 25** due to the high prevalence of transient HPV infections that resolve spontaneously in this age group.
- Over-screening and subsequent interventions could lead to unnecessary anxiety and procedures for conditions that would likely resolve on their own.
*It is reasonable to start Pap-test screening at the current visit and repeat it every 3 years.*
- Starting screening at the current age of **18 years is not recommended** according to current guidelines, as screening typically begins at age 21.
- Early screening in this age group often leads to the detection of **transient HPV infections** that would otherwise resolve without intervention, causing undue stress and follow-up.
*The patient does not require Pap testing as long as she uses barrier contraception.*
- While **barrier contraception** (condoms) reduces the risk of HPV transmission, it does not eliminate it entirely and therefore **does not negate the need for cervical cancer screening.**
- Regular screening is still recommended to detect any persistent HPV infections and associated cervical changes early.
New and emerging vaccines US Medical PG Question 7: A 2-month-old girl is brought to the physician by her father for a routine well-child examination. She is given a vaccine that contains polyribosylribitol phosphate conjugated to a toxoid carrier. The vaccine is most likely to provide immunity against which of the following pathogens?
- A. Haemophilus influenzae (Correct Answer)
- B. Neisseria meningitidis
- C. Bordetella pertussis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae
New and emerging vaccines Explanation: **Haemophilus influenzae**
- The vaccine described, containing **polyribosylribitol phosphate (PRP)** conjugated to a toxoid carrier, is characteristic of the **Haemophilus influenzae type b (Hib) vaccine**.
- PRP is the **polysaccharide capsule** of *H. influenzae* type b, and conjugating it to a protein (toxoid carrier) allows for T-cell dependent immunity, effective in infants.
*Neisseria meningitidis*
- While *N. meningitidis* also has a **polysaccharide capsule** and vaccines are available, their capsular components differ (e.g., serogroups A, C, Y, W-135, or B outer membrane protein).
- The description of **polyribosylribitol phosphate** is specific to *H. influenzae* type b.
*Bordetella pertussis*
- Vaccines against *Bordetella pertussis* are typically **acellular pertussis vaccines (aP)**, which contain purified components like pertussis toxoid, filamentous hemagglutinin, and pertactin, not a PRP conjugate.
- These vaccines target bacterial toxins and adhesins, not a polysaccharide capsule unique to PRP.
*Streptococcus pneumoniae*
- Vaccines for *S. pneumoniae* (pneumococcal vaccines) use **capsular polysaccharides** from various serotypes, often conjugated to a protein carrier (e.g., diphtheria toxoid), but the specific polysaccharide is not PRP.
- The structure and serotypes of pneumococcal capsular polysaccharides are distinct from PRP.
*Corynebacterium diphtheriae*
- The vaccine for *C. diphtheriae* is the **diphtheria toxoid**, which is an inactivated form of the diphtheria toxin, not a polysaccharide conjugate.
- It provides immunity by inducing antibodies against the toxin, preventing its harmful effects.
New and emerging vaccines US Medical PG Question 8: A 4-year-old girl is brought to her pediatrician for a routine check-up. She was diagnosed with sickle cell disease last year after an episode of dactylitis. She was started on hydroxyurea, with no painful crises or acute chest episodes since starting the medication. Which of the following is an appropriate preventive measure for this patient?
- A. Splenectomy
- B. Intranasal influenza vaccine
- C. Human papillomavirus vaccine
- D. Pneumococcal vaccine (Correct Answer)
- E. Parenteral penicillin G
New and emerging vaccines Explanation: ***Pneumococcal vaccine***
- Children with **sickle cell disease** are at high risk of severe **pneumococcal infections** due to functional asplenia, making vaccination crucial.
- The **pneumococcal conjugate vaccine (PCV13)** and **pneumococcal polysaccharide vaccine (PPSV23)** are recommended to protect against *Streptococcus pneumoniae*.
*Splenectomy*
- Although **functional asplenia** is common in sickle cell disease, prophylactic splenectomy is *not* a routine recommendation due to the associated risks and the availability of other preventive measures.
- **Splenectomy** is generally reserved for specific indications such as refractory **splenic sequestration crises** or hypersplenism.
*Intranasal influenza vaccine*
- The **intranasal live attenuated influenza vaccine (LAIV)** is **contraindicated** in children with sickle cell disease because of concerns about the live virus potentially exacerbating disease complications.
- The **inactivated influenza vaccine (IIV)**, given intramuscularly, is recommended annually for these patients.
*Human papillomavirus vaccine*
- The **HPV vaccine** is important for preventing cervical cancer and other HPV-related conditions, but it is typically indicated for adolescents starting at age 11 or 12, not a 4-year-old.
- It is not a primary or immediate preventive measure for the acute complications associated with **sickle cell disease** in early childhood.
*Parenteral penicillin G*
- While **oral penicillin prophylaxis** (penicillin V) is indeed recommended for children with sickle cell disease from infancy until at least age 5 to prevent pneumococcal sepsis, this question asks about **parenteral** penicillin G.
- **Parenteral penicillin G** (given by injection) is reserved for treating active infections or specific situations where oral administration is not feasible, not for routine daily prophylaxis in a stable outpatient.
- The standard prophylaxis is **oral penicillin V**, taken twice daily at home.
New and emerging vaccines US Medical PG Question 9: A 2-year-old girl is brought to her pediatrician’s office with intermittent and severe stomach ache and vomiting for the last 2 days. Last week the whole family had a stomach bug involving a few days of mild fever, lack of appetite, and diarrhea but they have all made a full recovery since. This current pain is different from the type she had during infection. With the onset of pain, the child cries and kicks her legs up in the air or pulls them to her chest. The parents have also observed mucousy stools and occasional bloody stools that are bright red and mucousy. After a while, the pain subsides and she returns to her normal activity. Which of the following would be the next step in the management of this patient?
- A. Abdominal radiograph
- B. Air enema (Correct Answer)
- C. Abdominal CT scan
- D. Surgical reduction
- E. Observe for 24 hours
New and emerging vaccines Explanation: ***Air enema***
- The clinical presentation with intermittent abdominal pain, leg drawing to the chest, "currant jelly" stools (bloody and mucousy), and a recent viral illness is highly suggestive of **intussusception**. An **air enema** is the diagnostic and therapeutic modality of choice for intussusception.
- It uses pneumatic pressure to reduce the telescoping of the bowel, and if successful, avoids the need for surgery.
*Abdominal radiograph*
- An **abdominal radiograph** may show signs of obstruction or a "target sign" (if present), but it is not sensitive or specific enough to definitively diagnose intussusception.
- It is primarily used to rule out perforation before performing an air enema if there are concerns about peritonitis.
*Abdominal CT scan*
- While an **abdominal CT scan** can diagnose intussusception, it exposes the child to significant radiation and is not typically the first-line imaging modality.
- It is usually reserved for cases where other diagnostic methods are inconclusive or if complications like perforation are suspected.
*Surgical reduction*
- **Surgical reduction** is indicated if an air enema fails to reduce the intussusception, if there are signs of bowel perforation or peritonitis, or if the patient is unstable.
- It is an invasive procedure and should not be the initial step in management unless there are clear contraindications to pneumatic reduction.
*Observe for 24 hours*
- Observing the child for 24 hours without intervention is inappropriate and can lead to serious complications, such as **bowel ischemia, necrosis, perforation, and sepsis**.
- Intussusception is a medical emergency that requires prompt diagnosis and treatment.
New and emerging vaccines US Medical PG Question 10: A 7-month-old boy presents to the emergency room with three episodes of vomiting and severe abdominal pain that comes and goes for the past two hours. The patient's most recent vomit in the hospital appears bilious, and the patient had one stool that appears bloody and full of mucous. The mother explains that one stool at home appears to be "jelly-like." On physical exam, a palpable mass is felt in the right lower quadrant of the abdomen. What is the next best diagnostic test for this patient?
- A. Peripheral blood culture
- B. Exploratory laparotomy
- C. Kidney, ureter, bladder radiograph
- D. Complete blood count with differential
- E. Abdominal ultrasound (Correct Answer)
New and emerging vaccines Explanation: ***Abdominal ultrasound***
- An abdominal ultrasound is the **next best diagnostic test** for this patient, as the clinical presentation (sudden onset of severe, intermittent abdominal pain, bilious vomiting, **currant jelly stool**, and a palpable **sausage-shaped mass in the right lower quadrant**) is highly suggestive of **intussusception**.
- Ultrasound is **non-invasive**, provides real-time imaging, and can confirm the diagnosis by visualizing the characteristic **"target sign" or "donut sign"**, indicating one segment of the bowel telescoping into another.
*Peripheral blood culture*
- A peripheral blood culture would be considered if there were strong signs of **sepsis or bacteremia**, such as fever, lethargy, or other systemic inflammatory responses, which are not the primary concern here.
- While infection could cause abdominal pain, the classic signs of intussusception (currant jelly stool, palpable mass) point away from an initial bacterial infection requiring blood cultures.
*Exploratory laparotomy*
- Exploratory laparotomy is a surgical procedure and would be considered an **intervention or treatment**, not the initial diagnostic test, especially when less invasive options are available.
- It is typically reserved for cases where non-invasive diagnostics are inconclusive or when there are signs of **perforation or peritonitis** requiring immediate surgical intervention.
*Kidney, ureter, bladder radiograph*
- A KUB radiograph might show signs of obstruction like dilated bowel loops or absence of gas in the colon, but it is **not definitive for intussusception** and has low sensitivity for diagnosing it.
- It would not provide the detailed soft tissue visualization necessary to confirm the telescoping of the bowel that an ultrasound would.
*Complete blood count with differential*
- A CBC with differential would provide information about the patient's **hemoglobin, white blood cell count**, and platelet count, which can indicate infection or anemia.
- While it may show elevated white blood cells in response to inflammation or ischemia, it is a **non-specific test** and would not definitively diagnose intussusception.
More New and emerging vaccines US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.