Live vs inactivated vaccines US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Live vs inactivated vaccines. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Live vs inactivated vaccines US Medical PG Question 1: A 23-year-old woman presents to her physician requesting the chickenpox vaccine. She is also complaining of nausea, malaise, and moderate weight gain. She developed these symptoms gradually over the past 2 weeks. She reports no respiratory or cardiovascular disorders. Her last menstruation was about 6 weeks ago. She has one sexual partner and uses a natural planning method for contraception. Her vital signs include: blood pressure 110/70 mm Hg, heart rate 92/min, respiratory rate 14/min, and temperature 37.2℃ (99℉). The physical examination shows non-painful breast engorgement and nipple hyperpigmentation. There is no neck enlargement and no palpable nodules in the thyroid gland. The urine beta-hCG is positive. What is the proper recommendation regarding chickenpox vaccination in this patient?
- A. Confirm pregnancy with serum beta-hCG and if positive delay administration of the vaccine until the third trimester.
- B. Perform varicella viral load and schedule the vaccine based on these results.
- C. Confirm pregnancy with serum beta-hCG and if positive, postpone administration of the vaccine until after completion of the pregnancy. (Correct Answer)
- D. Schedule the vaccination.
- E. Confirm pregnancy with serum beta-hCG and if positive, schedule the patient for pregnancy termination.
Live vs inactivated vaccines Explanation: ***Confirm pregnancy with serum beta-hCG and if positive, postpone administration of the vaccine until after completion of the pregnancy.***
- The patient's symptoms (nausea, malaise, weight gain, breast engorgement, nipple hyperpigmentation, missed menses) and a **positive urine beta-hCG** are highly indicative of **pregnancy**.
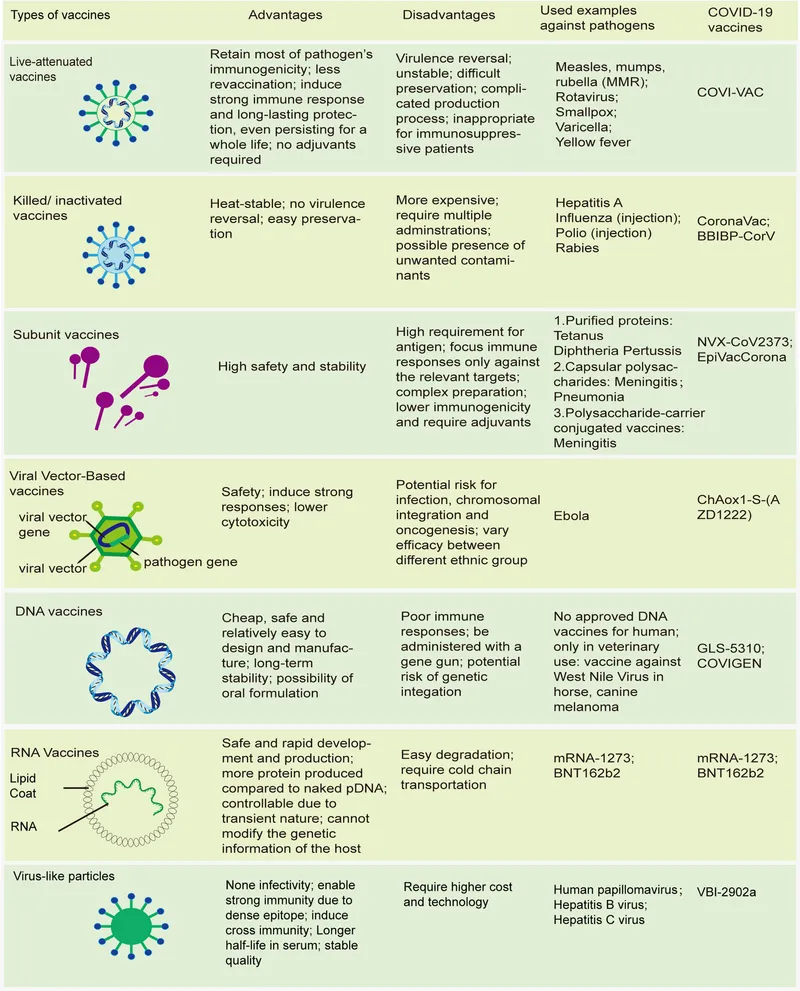
- The **chickenpox vaccine (varicella vaccine)** is a **live attenuated vaccine**, which is **contraindicated in pregnancy** due to the theoretical risk of fetal infection and congenital varicella syndrome. Vaccination should be deferred until after delivery.
*Confirm pregnancy with serum beta-hCG and if positive delay administration of the vaccine until the third trimester.*
- While confirming pregnancy with **serum beta-hCG** is appropriate, delaying vaccination only until the **third trimester** is still inappropriate for a live attenuated vaccine.
- Live attenuated vaccines are generally **contraindicated throughout pregnancy** due to potential fetal risks.
*Perform varicella viral load and schedule the vaccine based on these results.*
- A **varicella viral load** test is used to detect active viral infections, not to determine immunity or the need for vaccination in an uninfected individual.
- The primary concern here is the patient's likely pregnancy, not current varicella infection status.
*Schedule the vaccination.*
- Given the strong suspicion of **pregnancy** and a **positive urine beta-hCG**, immediately scheduling a live attenuated vaccine like the chickenpox vaccine would be **medically inappropriate and potentially harmful** to the fetus.
- Vaccination must be deferred until pregnancy status is confirmed and, if positive, until after delivery.
*Confirm pregnancy with serum beta-hCG and if positive, schedule the patient for pregnancy termination.*
- A potential need for a chickenpox vaccine, even if the patient is pregnant, is not an indication for **pregnancy termination**.
- This option is ethically and medically unsound, as exposure to the varicella vaccine in pregnancy does not warrant termination.
Live vs inactivated vaccines US Medical PG Question 2: A 28-year-old woman presents to her physician for follow-up. She was found to be HIV-positive 9 months ago. Currently she is on ART with lamivudine, tenofovir, and efavirenz. She has no complaints and only reports a history of mild respiratory infection since the last follow-up. She is also allergic to egg whites. Her vital signs are as follows: the blood pressure is 120/75 mm Hg, the heart rate is 73/min, the respiratory rate is 13/min, and the temperature is 36.7°C (98.0°F). She weighs 68 kg (150 lb), and there is no change in her weight since the last visit. On physical examination, she appears to be pale, her lymph nodes are not enlarged, her heart sounds are normal, and her lungs are clear to auscultation. Her total blood count shows the following findings:
Erythrocytes 3.2 x 106/mm3
Hematocrit 36%
Hgb 10 g/dL
Total leukocyte count 3,900/mm3
Neutrophils 66%
Lymphocytes 24%
Eosinophils 3%
Basophils 1%
Monocytes 7%
Platelet count 280,000/mm3
Her CD4+ cell count is 430 cells/µL. The patient tells you she would like to get an influenza vaccination as flu season is coming. Which of the following statements is true regarding influenza vaccination in this patient?
- A. As long as the patient is anemic, she should not be vaccinated.
- B. Influenza vaccination is contraindicated in HIV-positive patients because of the serious complications they can cause in immunocompromised people.
- C. Inactivated or recombinant influenza vaccines fail to induce a sufficient immune response in patients with CD4+ cell counts under 500 cells/µL.
- D. Nasal-spray influenza vaccine is the best option for vaccination in this patient.
- E. The patient can receive approved recombinant or inactivated influenza vaccines, with egg-free formulations preferred due to her egg allergy. (Correct Answer)
Live vs inactivated vaccines Explanation: **The patient can receive approved recombinant or inactivated influenza vaccines, with egg-free formulations preferred due to her egg allergy.**
- Patients with HIV, regardless of their CD4+ count, should receive the **inactivated influenza vaccine** annually due to their increased risk of severe influenza complications.
- Given the patient's reported egg allergy, an **egg-free vaccine formulation**, such as a recombinant injectable influenza vaccine (RIV4) or cell-culture-based inactivated influenza vaccine (ccIIV4), is the preferred choice to minimize allergic reactions.
*As long as the patient is anemic, she should not be vaccinated.*
- **Anemia** is not a contraindication for receiving the influenza vaccine; the benefits of vaccination typically outweigh any risks associated with mild anemia.
- While the patient is anemic (Hgb 10 g/dL), this condition does not prevent her from safely receiving an **inactivated influenza vaccine**.
*Influenza vaccination is contraindicated in HIV-positive patients because of the serious complications they can cause in immunocompromised people.*
- This statement is incorrect; **inactivated influenza vaccines** are recommended for HIV-positive individuals, as they are not live vaccines and cannot cause influenza.
- HIV-positive patients are at higher risk for severe influenza complications, making vaccination even more crucial, not contraindicated.
*Inactivated or recombinant influenza vaccines fail to induce a sufficient immune response in patients with CD4+ cell counts under 500 cells/µL.*
- While the immune response to vaccines can be attenuated in HIV patients with lower CD4+ counts, even a partial response offers some protection and is better than no vaccination.
- The **guidelines for HIV patients** recommend influenza vaccination regardless of CD4+ count, emphasizing the importance of any induced immunity.
*Nasal-spray influenza vaccine is the best option for vaccination in this patient.*
- The **nasal-spray influenza vaccine (LAIV)** is a **live-attenuated vaccine**, which is generally contraindicated in immunocompromised individuals, including those with HIV, due to the risk of active infection.
- HIV patients should receive **inactivated or recombinant influenza vaccines**, not live-attenuated formulations.
Live vs inactivated vaccines US Medical PG Question 3: A 40-year-old pregnant woman, G4 P3, visits your office at week 30 of gestation. She is very excited about her pregnancy and wants to be the healthiest she can be in preparation for labor and for her baby. What vaccination should she receive at this visit?
- A. Measles, mumps, and rubella (MMR)
- B. Varicella vaccine
- C. Herpes zoster vaccine
- D. Live attenuated influenza vaccine
- E. Tetanus, diphtheria, and acellular pertussis (Tdap) (Correct Answer)
Live vs inactivated vaccines Explanation: ***Tetanus, diphtheria, and acellular pertussis (Tdap)***
- The Tdap vaccine is recommended during each pregnancy, preferably between **27 and 36 weeks of gestation**, to maximize maternal antibody response and passive antibody transfer to the fetus.
- This provides critical protection against **pertussis (whooping cough)** for the newborn, who is too young to be vaccinated.
*Measles, mumps, and rubella (MMR)*
- The **MMR vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital rubella syndrome, although no cases have been reported.
- It should be administered **postpartum** if the mother is not immune to rubella.
*Varicella vaccine*
- The **varicella vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital varicella syndrome.
- Like MMR, it should be offered in the **postpartum period** if the woman is not immune.
*Herpes zoster vaccine*
- The herpes zoster vaccine is typically recommended for **older adults** (50 years and older) for shingles prevention.
- It is **not routinely recommended during pregnancy**, and its safety and efficacy in this population have not been sufficiently established.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is **contraindicated during pregnancy** due to its live virus content.
- Pregnant women should receive the **inactivated influenza vaccine (IIV)**, which is safe and recommended during any trimester.
Live vs inactivated vaccines US Medical PG Question 4: A 24-year-old woman with HIV infection comes to the physician for a follow-up examination. She has been inconsistently taking combined antiretroviral therapy for the past 5 years. She did not receive any childhood vaccinations because her parents were against them. During the consultation, the patient says that she wants to catch up on the missed vaccinations. Laboratory studies show a CD4+ T lymphocyte cell count of 180/mm3. Administration of the vaccine against which of the following agents should be avoided in this patient?
- A. Clostridium tetani
- B. Human papillomavirus
- C. Varicella zoster virus (Correct Answer)
- D. Bordetella pertussis
- E. Haemophilus influenzae
Live vs inactivated vaccines Explanation: ***Varicella zoster virus***
- The **varicella zoster vaccine is a live attenuated vaccine**, which is generally contraindicated in individuals with severe **immunodeficiency**, such as HIV patients with a **CD4+ count below 200 cells/mm³**.
- Administering a live vaccine to an immunocompromised patient can lead to **uncontrolled viral replication** and potentially cause the disease it is meant to prevent.
*Clostridium tetani*
- The **tetanus vaccine** is a **toxoid vaccine**, meaning it contains inactivated bacterial toxins, not live organisms.
- It is **safe and recommended** for individuals with HIV, regardless of their CD4+ count, to provide protection against tetanus.
*Human papillomavirus*
- The **HPV vaccine** is a **recombinant vaccine**, consisting of viral-like particles (VLPs) and containing no live virus.
- It is **safe and recommended** for HIV-positive individuals and helps prevent HPV-related cancers.
*Bordetella pertussis*
- The **pertussis vaccine** (part of DTaP or Tdap) is an **acellular vaccine**, containing purified bacterial components, not live bacteria.
- It is **safe and recommended** for HIV patients to protect against whooping cough.
*Haemophilus influenzae*
- The **Haemophilus influenzae type b (Hib) vaccine** is a **conjugate vaccine**, made from bacterial capsular polysaccharide linked to a carrier protein.
- It is **safe and recommended** for HIV-positive individuals, as they are at increased risk for invasive Hib disease.
Live vs inactivated vaccines US Medical PG Question 5: A young man about to leave for his freshman year of college visits his physician in order to ensure that his immunizations are up-to-date. Because he is living in a college dormitory, his physician gives him a vaccine that prevents meningococcal disease. What type of vaccine did this patient likely receive?
- A. Live, attenuated
- B. Killed, attenuated
- C. Toxoid
- D. Conjugated polysaccharide (Correct Answer)
- E. Killed, inactivated
Live vs inactivated vaccines Explanation: ***Conjugated polysaccharide***
- The **meningococcal vaccine** commonly administered to college students is a **polysaccharide vaccine** wherein the polysaccharide antigens are conjugated to a protein carrier.
- This **conjugation** improves the immune response by converting a T-independent antigen into a T-dependent one, inducing better memory responses and allowing for vaccination of infants.
*Live, attenuated*
- Live, attenuated vaccines contain a **weakened form of the pathogen** that can replicate but does not cause disease, such as the MMR or varicella vaccine.
- While they elicit strong, long-lasting immunity, the meningococcal vaccine is not typically of this type due to the risk of opportunistic infection, especially in immunocompromised individuals.
*Killed, attenuated*
- This term is a **contradiction**; vaccines are either **killed (inactivated)** or **live (attenuated)**, but not both.
- Attenuation implies weakening, for which the organism would still be alive.
*Toxoid*
- **Toxoid vaccines** are made from inactivated bacterial toxins, used to protect against diseases where the toxin, not the bacterium itself, causes the disease, such as diphtheria and tetanus.
- Meningococcal disease is primarily caused by **direct bacterial invasion and inflammation**, not solely by a toxin.
*Killed, inactivated*
- **Killed, inactivated vaccines** contain whole pathogens that have been killed and cannot replicate, such as the inactivated poliovirus vaccine.
- While there are inactivated meningococcal vaccines, the most common type for broad use, especially in college settings, is the conjugated polysaccharide vaccine, which elicits a stronger and more long-lasting immune response against multiple serotypes compared to plain inactivated whole-cell vaccines.
Live vs inactivated vaccines US Medical PG Question 6: A 20-year-old man who is a biology major presents to his physician for a simple check-up. He is informed that he hasn't received a hepatitis B vaccine. When the first injection is applied, the medical professional informs him that he will need to come back 2 more times on assigned days, since the vaccine is given in 3 doses. Which of the following antibodies is produced first in the college student as a result of the first vaccination?
- A. IgE
- B. IgG
- C. IgM (Correct Answer)
- D. IgD
- E. IgA
Live vs inactivated vaccines Explanation: ***IgM***
- Upon initial exposure to an antigen (like in the first vaccine dose), **IgM antibodies** are the first class to be produced and secreted by plasma cells.
- This **primary immune response** is characterized by a rapid, but short-lived, **IgM** peak.
*IgE*
- **IgE antibodies** are primarily involved in **allergic reactions** and defense against parasites, not the initial response to vaccination.
- Their production is typically triggered by exposure to specific allergens or parasites and mediated by Th2 helper T cells.
*IgG*
- **IgG antibodies** are the most abundant class in serum and are produced later in the primary response and predominantly during the **secondary immune response**.
- They provide **long-term immunity** and can cross the placenta, but are not the first antibody produced after initial antigen exposure.
*IgD*
- **IgD antibodies** are mainly found on the surface of **naive B cells** and act as B-cell receptors, playing a role in B-cell activation.
- They are not secreted in significant amounts into the serum and thus are not the first circulating antibody produced after vaccination.
*IgA*
- **IgA antibodies** are primarily found in **mucosal secretions** (e.g., saliva, tears, breast milk, gastrointestinal fluid) and play a key role in mucosal immunity.
- They are not the first antibody produced systemically in response to an initial vaccine exposure.
Live vs inactivated vaccines US Medical PG Question 7: A 2-month-old girl is brought to the physician by her father for a routine well-child examination. She is given a vaccine that contains polyribosylribitol phosphate conjugated to a toxoid carrier. The vaccine is most likely to provide immunity against which of the following pathogens?
- A. Haemophilus influenzae (Correct Answer)
- B. Neisseria meningitidis
- C. Bordetella pertussis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae
Live vs inactivated vaccines Explanation: **Haemophilus influenzae**
- The vaccine described, containing **polyribosylribitol phosphate (PRP)** conjugated to a toxoid carrier, is characteristic of the **Haemophilus influenzae type b (Hib) vaccine**.
- PRP is the **polysaccharide capsule** of *H. influenzae* type b, and conjugating it to a protein (toxoid carrier) allows for T-cell dependent immunity, effective in infants.
*Neisseria meningitidis*
- While *N. meningitidis* also has a **polysaccharide capsule** and vaccines are available, their capsular components differ (e.g., serogroups A, C, Y, W-135, or B outer membrane protein).
- The description of **polyribosylribitol phosphate** is specific to *H. influenzae* type b.
*Bordetella pertussis*
- Vaccines against *Bordetella pertussis* are typically **acellular pertussis vaccines (aP)**, which contain purified components like pertussis toxoid, filamentous hemagglutinin, and pertactin, not a PRP conjugate.
- These vaccines target bacterial toxins and adhesins, not a polysaccharide capsule unique to PRP.
*Streptococcus pneumoniae*
- Vaccines for *S. pneumoniae* (pneumococcal vaccines) use **capsular polysaccharides** from various serotypes, often conjugated to a protein carrier (e.g., diphtheria toxoid), but the specific polysaccharide is not PRP.
- The structure and serotypes of pneumococcal capsular polysaccharides are distinct from PRP.
*Corynebacterium diphtheriae*
- The vaccine for *C. diphtheriae* is the **diphtheria toxoid**, which is an inactivated form of the diphtheria toxin, not a polysaccharide conjugate.
- It provides immunity by inducing antibodies against the toxin, preventing its harmful effects.
Live vs inactivated vaccines US Medical PG Question 8: A 35-year-old man is brought to the emergency department by his wife because of a 1-week history of progressive confusion, myalgia, and nausea. His wife says that he first reported headaches and fatigue 10 days ago, and since then “he has not been himself”. He has refused to drink any liquids for the last day. Two months ago, he helped his neighbor remove a raccoon's den from her backyard. He appears agitated. His temperature is 100.8°F (38.2°C). Examination shows excessive drooling. Muscle tone and deep tendon reflexes are increased bilaterally. Administration of which of the following is most likely to have prevented this patient's condition?
- A. Inosine monophosphate dehydrogenase inhibitor
- B. RNA-dependent DNA polymerase inhibitor
- C. Live attenuated vaccine
- D. Chemically-inactivated virus (Correct Answer)
- E. Immunoglobulin against a bacterial protein
Live vs inactivated vaccines Explanation: ***Chemically-inactivated virus***
- This patient presents with symptoms highly suggestive of **rabies**, including progressive confusion, myalgias, agitation, excessive drooling, and increased muscle tone, following exposure to a raccoon.
- The rabies vaccine is a **chemically-inactivated virus** type that induces active immunity, and post-exposure prophylaxis with this vaccine (along with rabies immunoglobulin) would have prevented the disease.
*Inosine monophosphate dehydrogenase inhibitor*
- **Inosine monophosphate dehydrogenase inhibitors** (e.g., mycophenolate mofetil) are immunosuppressants used to prevent organ transplant rejection or treat autoimmune diseases.
- They do not have a role in preventing or treating viral infections like rabies.
*RNA-dependent DNA polymerase inhibitor*
- **RNA-dependent DNA polymerase inhibitors** (e.g., reverse transcriptase inhibitors) are mainly used in the treatment of **HIV infection**, a retrovirus that uses reverse transcriptase.
- Rabies virus is an RNA virus (rhabdovirus), but it does not use reverse transcriptase, and these inhibitors are not effective against it.
*Live attenuated vaccine*
- While many effective viral vaccines are **live attenuated** (e.g., MMR, varicella), the rabies vaccine used for post-exposure prophylaxis and prevention is not live attenuated, due to safety concerns.
- A live attenuated vaccine, if available and safe, would induce a strong immune response, but it is not the type of vaccine used for rabies in humans.
*Immunoglobulin against a bacterial protein*
- This describes antitoxins or immunoglobulins used against **bacterial infections** or their toxins (e.g., tetanus antitoxin).
- Rabies is a viral infection, and while passive immunization with **rabies immunoglobulin** is part of post-exposure prophylaxis, it is specific to the rabies virus and not a bacterial protein.
Live vs inactivated vaccines US Medical PG Question 9: A 4-month-old boy is brought to the physician by his parents for a well-child examination. He has cystic fibrosis diagnosed by newborn screening. His parents report frequent feedings and large-volume and greasy stools. His 4-year-old brother has autism. Current medications include bronchodilators, pancreatic enzyme supplements, and fat-soluble vitamins. He is at the 18th percentile for height and 15th percentile for weight. Scattered wheezes are heard throughout both lung fields. Examination shows a distended and tympanic abdomen with no tenderness or guarding. Which of the following is a contraindication for administering one or more routine vaccinations?
- A. Allergy to egg protein
- B. History of cystic fibrosis
- C. History of febrile seizures
- D. Fever of 38.2°C (100.7°F) following previous vaccinations
- E. History of intussusception (Correct Answer)
Live vs inactivated vaccines Explanation: ***History of intussusception***
- A history of **intussusception** is a **contraindication for rotavirus vaccine** administration, as the vaccine itself has a small risk of intussusception, particularly with the first dose.
- The rotavirus vaccine is part of routine childhood immunizations, so this would be a contraindication for one of the routine vaccines.
*Allergy to egg protein*
- Egg allergy is a contraindication primarily for yellow fever vaccine and some influenza vaccines, which are typically not routine vaccinations for a 4-month-old. Many flu vaccines are egg-free or can be safely administered to those with egg allergy under supervision.
- The MMR vaccine is generally safe for those with egg allergy since the amount of egg protein is negligible.
*History of cystic fibrosis*
- **Cystic fibrosis** itself is **not a contraindication** to routine vaccinations; in fact, patients with chronic conditions like CF are often *more* encouraged to receive vaccinations to prevent severe infections.
- The patient's symptoms (poor growth, greasy stools, wheezing) are manifestations of CF, not reasons to defer vaccination.
*History of febrile seizures*
- A history of **febrile seizures** is generally **not a contraindication** to routine vaccinations.
- Parents should be counseled on fever management after vaccination, but the risk of recurrent febrile seizures is not increased by vaccination to a level that warrants deferral.
*Fever of 38.2°C (100.7°F) following previous vaccinations*
- A **low-grade fever** after vaccination is a common and **expected immune response**, not a contraindication for future doses.
- Only a **severe allergic reaction** (e.g., anaphylaxis) to a previous dose of a vaccine or one of its components is a contraindication to subsequent doses of that specific vaccine.
Live vs inactivated vaccines US Medical PG Question 10: A 4-year-old boy is brought to the emergency department with difficulty breathing. His mother reports that he developed a fever last night and began to have trouble breathing this morning. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is unvaccinated (conscientious objection by the family) and is meeting all developmental milestones. At the hospital, his vitals are temperature 39.8°C (103.6°F), pulse 122/min, respiration rate 33/min, blood pressure 110/66 mm Hg, and SpO2 93% on room air. On physical examination, he appears ill with his neck hyperextended and chin protruding. His voice is muffled and is drooling. The pediatrician explains that there is one particular bacteria that commonly causes these symptoms. At what age should the patient have first received vaccination to prevent this condition from this particular bacteria?
- A. At birth
- B. At 2-months-old (Correct Answer)
- C. Between 9- and 12-months-old
- D. At 6-months-old
- E. Between 12- and 15-months-old
Live vs inactivated vaccines Explanation: ***At 2-months-old***
- The clinical presentation with **high fever**, **difficulty breathing**, **neck hyperextension**, **muffled voice**, and **drooling** in an unvaccinated child strongly suggests **epiglottitis**, likely caused by *Haemophilus influenzae type b* (Hib).
- The **Hib vaccine** is routinely given starting at **2 months of age** as part of the multi-dose primary series to protect against this life-threatening condition.
*At birth*
- While some vaccines like **Hepatitis B** are given at birth, the Hib vaccine is not typically administered at this age.
- Vaccinating at birth would not align with the standard immunization schedule for *Haemophilus influenzae type b*.
*Between 9- and 12-months-old*
- This age range typically corresponds to the **measles, mumps, and rubella (MMR)** and **varicella** vaccines, or a booster dose of other vaccines, not the initial primary series for Hib.
- Delaying the first Hib vaccination until this age would leave infants vulnerable during a critical period.
*At 6-months-old*
- By 6 months, a child should have already received at least **two doses** of the Hib vaccine if following the recommended schedule.
- Administering the first dose at 6 months would significantly delay protection against invasive Hib disease.
*Between 12- and 15-months-old*
- This age range is typically when the **final booster dose** of the Hib vaccine is given, not the initial vaccination.
- The primary series for Hib should have been completed much earlier to provide timely protection.
More Live vs inactivated vaccines US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.