Childhood immunization schedule US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Childhood immunization schedule. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Childhood immunization schedule US Medical PG Question 1: A 40-year-old pregnant woman, G4 P3, visits your office at week 30 of gestation. She is very excited about her pregnancy and wants to be the healthiest she can be in preparation for labor and for her baby. What vaccination should she receive at this visit?
- A. Measles, mumps, and rubella (MMR)
- B. Varicella vaccine
- C. Herpes zoster vaccine
- D. Live attenuated influenza vaccine
- E. Tetanus, diphtheria, and acellular pertussis (Tdap) (Correct Answer)
Childhood immunization schedule Explanation: ***Tetanus, diphtheria, and acellular pertussis (Tdap)***
- The Tdap vaccine is recommended during each pregnancy, preferably between **27 and 36 weeks of gestation**, to maximize maternal antibody response and passive antibody transfer to the fetus.
- This provides critical protection against **pertussis (whooping cough)** for the newborn, who is too young to be vaccinated.
*Measles, mumps, and rubella (MMR)*
- The **MMR vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital rubella syndrome, although no cases have been reported.
- It should be administered **postpartum** if the mother is not immune to rubella.
*Varicella vaccine*
- The **varicella vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital varicella syndrome.
- Like MMR, it should be offered in the **postpartum period** if the woman is not immune.
*Herpes zoster vaccine*
- The herpes zoster vaccine is typically recommended for **older adults** (50 years and older) for shingles prevention.
- It is **not routinely recommended during pregnancy**, and its safety and efficacy in this population have not been sufficiently established.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is **contraindicated during pregnancy** due to its live virus content.
- Pregnant women should receive the **inactivated influenza vaccine (IIV)**, which is safe and recommended during any trimester.
Childhood immunization schedule US Medical PG Question 2: An 11-year-old boy is brought to his pediatrician by his parents for the routine Tdap immunization booster dose that is given during adolescence. Upon reviewing the patient’s medical records, the pediatrician notes that he was immunized according to CDC recommendations, with the exception that he received a catch-up Tdap immunization at the age of 8 years. When the pediatrician asks the boy’s parents about this delay, they inform the doctor that they immigrated to this country 3 years ago from Southeast Asia, where the child had not been immunized against diphtheria, tetanus, and pertussis. Therefore, he received a catch-up series at 8 years of age, which included the first dose of the Tdap vaccine. Which of the following options should the pediatrician choose to continue the boy’s immunization schedule?
- A. A single dose of Td vaccine at 18 years of age
- B. A single dose of Td vaccine now
- C. No further vaccination needed
- D. A single dose of Tdap vaccine now
- E. A single dose of Tdap vaccine at 13 years of age (Correct Answer)
Childhood immunization schedule Explanation: ***A single dose of Tdap vaccine at 13 years of age***
- The CDC recommends a **minimum interval of 5 years** between Tdap doses when Tdap is given as part of a catch-up series.
- Since this patient received his first Tdap at age 8, the earliest he should receive the adolescent booster is at **age 13** (5 years later).
- This timing ensures adequate spacing while still providing the recommended adolescent booster for **pertussis, tetanus, and diphtheria** protection.
- The 5-year interval prevents excessive antigen exposure and optimizes immune response.
*A single dose of Tdap vaccine now*
- Giving Tdap now would result in only a **3-year interval** from the previous Tdap dose at age 8.
- This violates the CDC recommendation of a **minimum 5-year interval** between Tdap doses.
- Shorter intervals may increase local reactogenicity without improving protection.
*A single dose of Td vaccine now*
- While this would provide tetanus and diphtheria protection, it would **not protect against pertussis**, which is a critical component of adolescent vaccination.
- The Tdap vaccine is specifically recommended for adolescents to boost waning pertussis immunity.
- Additionally, giving it now would still be earlier than the recommended 5-year interval from the previous pertussis-containing vaccine.
*A single dose of Td vaccine at 18 years of age*
- This option would result in a **10-year gap** from the last pertussis-containing vaccine, leaving the adolescent vulnerable during high-risk years.
- The adolescent Tdap booster is specifically timed for ages 11-13 to protect during peak transmission periods in middle and high school.
- Waiting until 18 would miss the critical window for pertussis protection.
*No further vaccination needed*
- While the patient completed a catch-up series, the CDC still recommends an **adolescent Tdap booster** even for those who received Tdap in a catch-up series.
- The adolescent booster is important to maintain immunity against pertussis, which wanes significantly over time.
- The booster should be given at age 13 to maintain the 5-year minimum interval.
Childhood immunization schedule US Medical PG Question 3: A 2-year-old boy is brought in by his parents to his pediatrician. The boy was born by spontaneous vaginal delivery at 39 weeks and 5 days after a normal pregnancy. The boy has received all age-appropriate vaccinations as of his last visit at 18 months of age. Of note, the boy has confirmed sickle cell disease and the only medication he takes is penicillin prophylaxis. The parents state that they plan on enrolling their son in a daycare, which requires documentation of up-to-date vaccinations. The pediatrician states that their son needs an additional vaccination at this visit, which is a polysaccharide vaccine that is not conjugated to protein. Which of the following matches this description?
- A. Pneumovax (Correct Answer)
- B. Menactra
- C. Prevnar
- D. Hib vaccine
- E. Live attenuated influenza vaccine
Childhood immunization schedule Explanation: ***Pneumovax***
- **Pneumovax** (PCV23, PPSV23) is a **polysaccharide vaccine** that is not conjugated to a protein carrier. Children with **sickle cell disease** should receive this vaccine due to their immunocompromised state and increased risk of encapsulated bacterial infections.
- The Centers for Disease Control and Prevention (CDC) recommends PPSV23 for children aged 2 years and older with chronic medical conditions such as **sickle cell disease**, usually administered 8 weeks after their last PCV13 dose.
*Menactra*
- **Menactra** is a **quadrivalent meningococcal conjugate vaccine** (MCV4), meaning it contains a polysaccharide antigen conjugated to a protein carrier.
- This vaccine primarily targets *Neisseria meningitidis* and is different from the pneumococcal vaccine required here.
*Prevnar*
- **Prevnar** (PCV13) is a **pneumococcal conjugate vaccine**, meaning its polysaccharide antigens are conjugated to a protein carrier.
- While important for children with sickle cell disease, the question specifically asks for a vaccination that is a **polysaccharide vaccine that is not conjugated to protein**.
*Hib vaccine*
- The **Hib vaccine** (against *Haemophilus influenzae* type b) is a **conjugate vaccine**, meaning its polysaccharide capsule is linked to a protein carrier to enhance immunogenicity, particularly in infants.
- This vaccine is typically given earlier in childhood and is not the "additional" unconjugated polysaccharide vaccine described.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is a live virus vaccine, not a polysaccharide vaccine.
- It is also contraindicated in individuals with certain immunocompromising conditions, such as some patients with sickle cell disease.
Childhood immunization schedule US Medical PG Question 4: A 2-year-old boy presents for a routine checkup. The patient’s mother says that he has been ‘under the weather’ for the past few days. She did not measure his temperature at home but states that he has felt warm. She denies any episodes of diarrhea or vomiting. No significant past medical history or current medications. The patient attends daycare. He is due for a hepatitis A vaccine. The patient was born at term with no prenatal or perinatal complications. The vital signs include: temperature 37.8°C (100.1°F), blood pressure 112/62 mm Hg, pulse 80/min, respiratory rate 18/min, and oxygen saturation 99% on room air. The patient is alert and responsive. The physical exam is unremarkable. Which of the following is the most appropriate next step in the management of this patient?
- A. Order a complete blood count
- B. Order liver function tests
- C. Strep rapid antigen detection test
- D. Administer the hepatitis A vaccine (Correct Answer)
- E. Delay the hepatitis A immunization until next visit
Childhood immunization schedule Explanation: ***Administer the hepatitis A vaccine***
- The patient has a **low-grade fever** (37.8°C), which is generally **not considered a contraindication** for vaccination, especially if the child is otherwise well and active.
- The patient's presentation of being "under the weather" with an unremarkable physical exam and stable vitals suggests a **mild illness**, allowing for routine vaccinations to proceed.
*Order a complete blood count*
- A **CBC is not indicated** at this time, as the patient displays only mild, non-specific symptoms and has a normal physical exam.
- This would be reserved for cases with more concerning signs of infection or systemic illness, such as persistent high fever, lethargy, or specific clinical findings.
*Order liver function tests*
- **Liver function tests are not warranted** as the patient has no symptoms or signs suggestive of liver disease (e.g., jaundice, right upper quadrant pain, dark urine).
- While the patient is due for a hepatitis A vaccine, there is no clinical evidence of active hepatitis or liver dysfunction requiring diagnostic workup.
*Strep rapid antigen detection test*
- The patient has **no symptoms consistent with streptococcal pharyngitis**, such as sore throat, tonsillar exudates, or cervical lymphadenopathy.
- Given the lack of specific symptoms, testing for strep throat would be inappropriate and potentially lead to unnecessary antibiotic use.
*Delay the hepatitis A immunization until next visit*
- Delaying vaccination is only recommended for **moderate to severe acute illnesses** with or without fever, or for certain contraindications.
- A mild illness with low-grade fever, as in this case, is generally **not a reason to postpone** routine immunizations, as per CDC guidelines.
Childhood immunization schedule US Medical PG Question 5: A 20-year-old primigravid woman comes to the physician in October for her first prenatal visit. She has delayed the visit because she wanted a “natural birth” but was recently convinced to get a checkup after feeling more tired than usual. She feels well. Menarche was at the age of 12 years and menses used to occur at regular 28-day intervals and last 3–7 days. The patient emigrated from Mexico 2 years ago. Her immunization records are unavailable. Pelvic examination shows a uterus consistent in size with a 28-week gestation. Laboratory studies show:
Hemoglobin 12.4 g/dL
Leukocyte count 8,000/mm3
Blood group B negative
Serum
Glucose 88 mg/dL
Creatinine 1.1 mg/dL
TSH 3.8 μU/mL
Rapid plasma reagin negative
HIV antibody negative
Hepatitis B surface antigen negative
Urinalysis shows no abnormalities. Urine culture is negative. Chlamydia and gonorrhea testing are negative. A Pap smear is normal. Administration of which of the following vaccines is most appropriate at this time?
- A. Varicella and influenza
- B. Varicella and Tdap
- C. Influenza only
- D. Tdap and influenza (Correct Answer)
- E. Hepatitis B and MMR
Childhood immunization schedule Explanation: ***Tdap and influenza***
- The **Tdap vaccine** is recommended for pregnant women during each pregnancy, preferably between **27 and 36 weeks gestation**, to provide passive immunity to the newborn against pertussis. The patient is at 28 weeks gestation.
- The **influenza vaccine** is recommended for all pregnant women, regardless of trimester, during flu season (October in this case) to protect both the mother and the newborn.
*Varicella and influenza*
- The **varicella vaccine is contraindicated in pregnancy** because it is a live attenuated vaccine.
- While influenza vaccine is appropriate, administering varicella vaccine is not.
*Varicella and Tdap*
- As mentioned, the **varicella vaccine is contraindicated in pregnancy** due to its live attenuated nature.
- Although Tdap is appropriate, varicella is not.
*Influenza only*
- While the **influenza vaccine is appropriate**, the **Tdap vaccine** is also indicated for this patient given her gestational age and the benefits for the newborn.
- Administering only influenza would miss an opportunity to provide crucial pertussis protection.
*Hepatitis B and MMR*
- The **Hepatitis B vaccine** is safe in pregnancy if indicated, but the patient tested **Hepatitis B surface antigen negative**, suggesting no current infection and no immediate need for vaccination based on the provided information.
- The **MMR vaccine is contraindicated in pregnancy** because it is a live attenuated vaccine.
Childhood immunization schedule US Medical PG Question 6: To protect against a potentially deadly infection, a 19-year-old female receives a vaccine containing capsular polysaccharide. This vaccine will stimulate her immune system to produce antibodies against which organism?
- A. Corynebacterium diphtheriae
- B. Neisseria meningitidis (Correct Answer)
- C. Streptococcus pneumoniae
- D. Clostridium tetani
- E. Haemophilus influenzae type b
Childhood immunization schedule Explanation: ***Neisseria meningitidis***
- The vaccine described, containing **capsular polysaccharide**, targets the **polysaccharide capsule** of *Neisseria meningitidis*, which is a key virulence factor.
- This bacterium causes **meningococcal meningitis**, a potentially deadly infection, especially in adolescents and young adults.
- The **meningococcal vaccine** is specifically recommended for adolescents and college students due to increased risk in this population.
*Corynebacterium diphtheriae*
- The vaccine against *C. diphtheriae* is a **toxoid vaccine**, meaning it contains an inactivated form of the **diphtheria toxin**, not capsular polysaccharide.
- This vaccine primarily protects against the effects of the **exotoxin**, which causes major symptoms like myocarditis and neuropathy.
*Streptococcus pneumoniae*
- While *S. pneumoniae* also has a **capsular polysaccharide vaccine** (PPSV23 and PCV13), it is primarily recommended for **young children, elderly adults, and immunocompromised patients**.
- A **19-year-old healthy female** would not routinely receive pneumococcal vaccine unless she had specific risk factors.
- The question context of a "potentially deadly infection" in this age group more specifically points to meningococcus.
*Clostridium tetani*
- The vaccine for *C. tetani* is a **tetanus toxoid vaccine**, similar to diphtheria, targeting the inactivated **tetanospasmin toxin** produced by the bacterium.
- This vaccine prevents the neurological symptoms of tetanus by neutralizing the toxin, not by targeting capsular polysaccharides.
*Haemophilus influenzae type b*
- While *H. influenzae* type b also has a **capsular polysaccharide-based vaccine** (conjugate vaccine), it is primarily given to **infants and young children** as part of routine childhood immunization.
- A 19-year-old would have already received this vaccine in childhood, and it is not routinely given to adolescents or adults.
- The age group and clinical context make meningococcus the more likely answer.
Childhood immunization schedule US Medical PG Question 7: A 3-month-old African American boy presents to his pediatrician’s office for his routine well visit. He was born full-term from an uncomplicated vaginal delivery. He is exclusively breastfeeding and not receiving any medications or supplements. Today, his parents report no issues or concerns with their child. He is lifting his head for brief periods and smiling. He has received only 2 hepatitis B vaccines. Which of the following is the correct advice for this patient’s parents?
- A. He should be sleeping more.
- B. He should have his serum lead level checked to screen for lead intoxication.
- C. He should start vitamin D supplementation. (Correct Answer)
- D. He should start rice cereal.
- E. He needs a 3rd hepatitis B vaccine.
Childhood immunization schedule Explanation: ***He should start vitamin D supplementation.***
- **Exclusively breastfed** infants, regardless of maternal vitamin D intake, require **vitamin D supplementation** due to insufficient amounts in breast milk.
- The recommended daily dose is **400 IU** starting from the first few days of life, to prevent **rickets** and promote bone health.
- **African American infants** have an additional risk factor due to increased skin melanin content, which reduces cutaneous vitamin D synthesis from sunlight exposure.
*He should be sleeping more.*
- A 3-month-old infant typically sleeps between **14-17 hours per day**, with **waking periods to feed** and interact.
- The case description does not indicate any concerns with the child's sleep patterns, and **developmental milestones** like lifting his head and smiling are being met.
*He should have his serum lead level checked to screen for lead intoxication.*
- **Lead screening** is not routinely recommended for all infants unless specific **risk factors** are present, such as living in an older home with lead paint, or having siblings with elevated lead levels.
- There are no reported risk factors for lead exposure in this patient's history.
*He should start rice cereal.*
- Introduction of solid foods, such as rice cereal, is typically recommended around **6 months of age**, when the infant shows signs of **developmental readiness**.
- These signs include **head control**, sitting with support, and showing interest in food.
*He needs a 3rd hepatitis B vaccine.*
- The **third dose of the hepatitis B vaccine** is typically administered between **6 and 18 months of age**.
- At 3 months old, the infant is not yet due for his third dose.
Childhood immunization schedule US Medical PG Question 8: A 20-year-old man who is a biology major presents to his physician for a simple check-up. He is informed that he hasn't received a hepatitis B vaccine. When the first injection is applied, the medical professional informs him that he will need to come back 2 more times on assigned days, since the vaccine is given in 3 doses. Which of the following antibodies is produced first in the college student as a result of the first vaccination?
- A. IgE
- B. IgG
- C. IgM (Correct Answer)
- D. IgD
- E. IgA
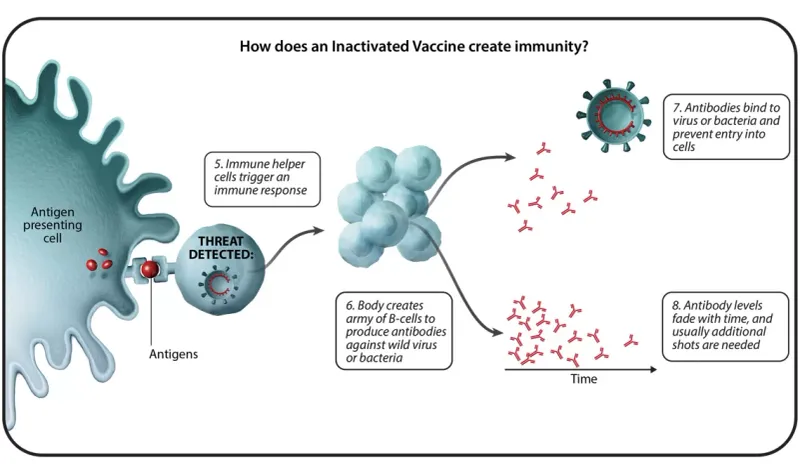
Childhood immunization schedule Explanation: ***IgM***
- Upon initial exposure to an antigen (like in the first vaccine dose), **IgM antibodies** are the first class to be produced and secreted by plasma cells.
- This **primary immune response** is characterized by a rapid, but short-lived, **IgM** peak.
*IgE*
- **IgE antibodies** are primarily involved in **allergic reactions** and defense against parasites, not the initial response to vaccination.
- Their production is typically triggered by exposure to specific allergens or parasites and mediated by Th2 helper T cells.
*IgG*
- **IgG antibodies** are the most abundant class in serum and are produced later in the primary response and predominantly during the **secondary immune response**.
- They provide **long-term immunity** and can cross the placenta, but are not the first antibody produced after initial antigen exposure.
*IgD*
- **IgD antibodies** are mainly found on the surface of **naive B cells** and act as B-cell receptors, playing a role in B-cell activation.
- They are not secreted in significant amounts into the serum and thus are not the first circulating antibody produced after vaccination.
*IgA*
- **IgA antibodies** are primarily found in **mucosal secretions** (e.g., saliva, tears, breast milk, gastrointestinal fluid) and play a key role in mucosal immunity.
- They are not the first antibody produced systemically in response to an initial vaccine exposure.
Childhood immunization schedule US Medical PG Question 9: A 19-year-old male arrives to student health for an annual check up. He is up to date on his infant and childhood vaccinations up to age 10. At age 12, he received a single dose of the tetanus, diphtheria, and acellular pertussis vaccine, and a quadrivalent meningococcal conjugate vaccine. A month ago, he received the influenza vaccine. The patient has no significant medical history. He takes over the counter ibuprofen for occasional headaches. He has a father with hypertension and hyperlipidemia, and his brother has asthma. He is sexually active with his current girlfriend. He denies tobacco use, illicit drug use, and recent or future travel. The patient’s temperature is 98°F (36.7°C), blood pressure is 118/78 mmHg, pulse is 70/min, and respirations are 14/min with an oxygen saturation of 99% O2 on room air. A physical examination is normal. What of the following is the best recommendation for vaccination?
- A. Human papillomavirus vaccine (Correct Answer)
- B. Hepatitis A vaccine
- C. Herpes zoster vaccine
- D. Pneumococcal vaccine
- E. Tetanus and reduced diphtheria toxoid booster
Childhood immunization schedule Explanation: ***Human papilloma virus***
- This patient, being 19 years old and **sexually active**, is a prime candidate for the **HPV vaccine** to prevent infections that can lead to various cancers.
- The CDC recommends routine HPV vaccination at age 11-12, but catch-up vaccination is recommended for individuals up to age 26 if not adequately vaccinated previously.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is generally recommended for individuals at **increased risk** of infection, such as travelers to endemic areas, men who have sex with men, or those with chronic liver disease, none of which apply to this patient.
- There is no indication for routine vaccination without specific risk factors in this otherwise healthy young male.
*Herpes zoster vaccine*
- The herpes zoster (shingles) vaccine is recommended for adults **age 50 years and older** to prevent shingles.
- This patient is only 19 years old, making him too young for this vaccine recommendation.
*Pneumococcal vaccine*
- Pneumococcal vaccines (PCV13 and PPSV23) are typically recommended for **young children**, adults **65 years and older**, or individuals with **certain underlying medical conditions** (e.g., chronic heart, lung, or kidney disease, or immunocompromised states).
- This 19-year-old patient has no such risk factors for pneumococcal disease.
*Tetanus and reduced diphtheria toxoid booster*
- The patient received a Tdap vaccine at age 12. A Td booster is recommended **every 10 years** for adults.
- Since it has been only 7 years since his last Tdap vaccine, he is not due for a Td booster at this time.
Childhood immunization schedule US Medical PG Question 10: A 38-year-old man comes to the physician because of severe muscle pain and swelling of his eyelids for 3 days. He has also had fever and chills during this period. For the last 2 days, he has had severe pain in his mouth while chewing. He had an episode of diarrhea a month ago for which he did not seek medical care. He has no history of serious illness. His sister has dermatomyositis. He returned from a hunting trip to eastern Europe 45 days ago. His temperature is 38.1°C (100.6°F), pulse is 80/min, and blood pressure is 130/70 mm Hg. Examination shows periorbital edema and severe generalized muscle tenderness. There are splinter hemorrhages on both hands. Laboratory studies show:
Hemoglobin 14.2 g/dL
Leukocyte count 12,500/mm3
Segmented neutrophils 60%
Eosinophils 18%
Lymphocytes 20%
Monocytes 2%
Serum
Glucose 117 mg/dL
Creatinine 1.1 mg/dL
Alkaline phosphatase 72 U/L
Creatine kinase 765 U/L
Urinalysis is within normal limits. Which of the following is most likely to have prevented this patient's condition?
- A. Consume pasteurized dairy products
- B. Clean drinking water
- C. Cooking meat to 71°C (160°F) (Correct Answer)
- D. Metronidazole at the onset of diarrhea
- E. Influenza vaccine
Childhood immunization schedule Explanation: ***Cooking meat to 71°C (160°F)***
- This patient's symptoms (fever, **periorbital edema**, **severe myalgia**, **eosinophilia**, elevated CK) after a hunting trip to eastern Europe are highly suggestive of **Trichinellosis**, caused by consuming undercooked meat infected with *Trichinella* larvae.
- **Thoroughly cooking meat** (especially wild game or pork) to an internal temperature of 71°C (160°F) is a primary preventative measure against *Trichinella* infection, as it kills the larvae.
*Consume pasteurized dairy products*
- Consuming pasteurized dairy products prevents infections such as **brucellosis** or **listeriosis**.
- These infections typically present with different clinical features, and their transmission is not associated with hunting wild game in Eastern Europe in the context of the patient's symptoms.
*Clean drinking water*
- Access to clean drinking water is crucial for preventing waterborne diseases like **giardiasis**, **cholera**, or **typhoid fever**.
- While the patient had diarrhea, the subsequent systemic symptoms with muscle involvement and eosinophilia point away from typical waterborne illnesses as the primary cause of his current condition.
*Metronidazole at the onset of diarrhea*
- **Metronidazole** is an antibiotic used to treat parasitic infections like **Giardia** or bacterial infections such as those caused by *Clostridium difficile*.
- Treating diarrhea with metronidazole, even if effective for the initial gastrointestinal issue, would not prevent a subsequent *Trichinella* infection which is acquired through undercooked meat.
*Influenza vaccine*
- The **influenza vaccine** protects against the **influenza virus**, which causes respiratory symptoms, fever, and generalized myalgia.
- However, the absence of prominent respiratory symptoms, the presence of marked eosinophilia, periorbital edema, and the history of recent exposure to wild game make influenza an unlikely diagnosis.
More Childhood immunization schedule US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.