Trauma assessment in children US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Trauma assessment in children. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
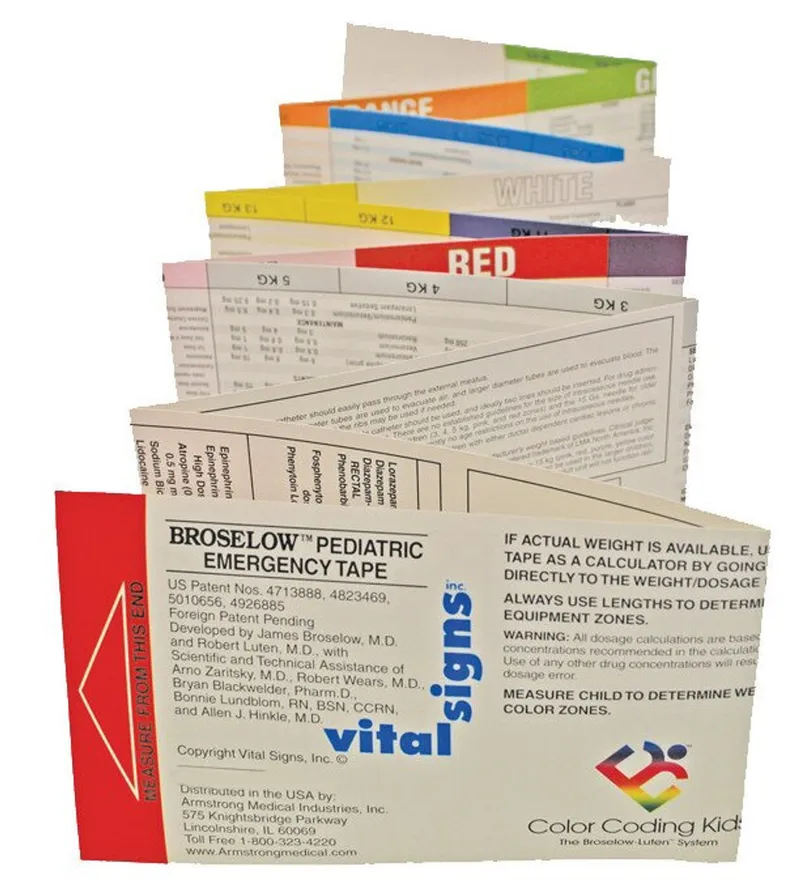
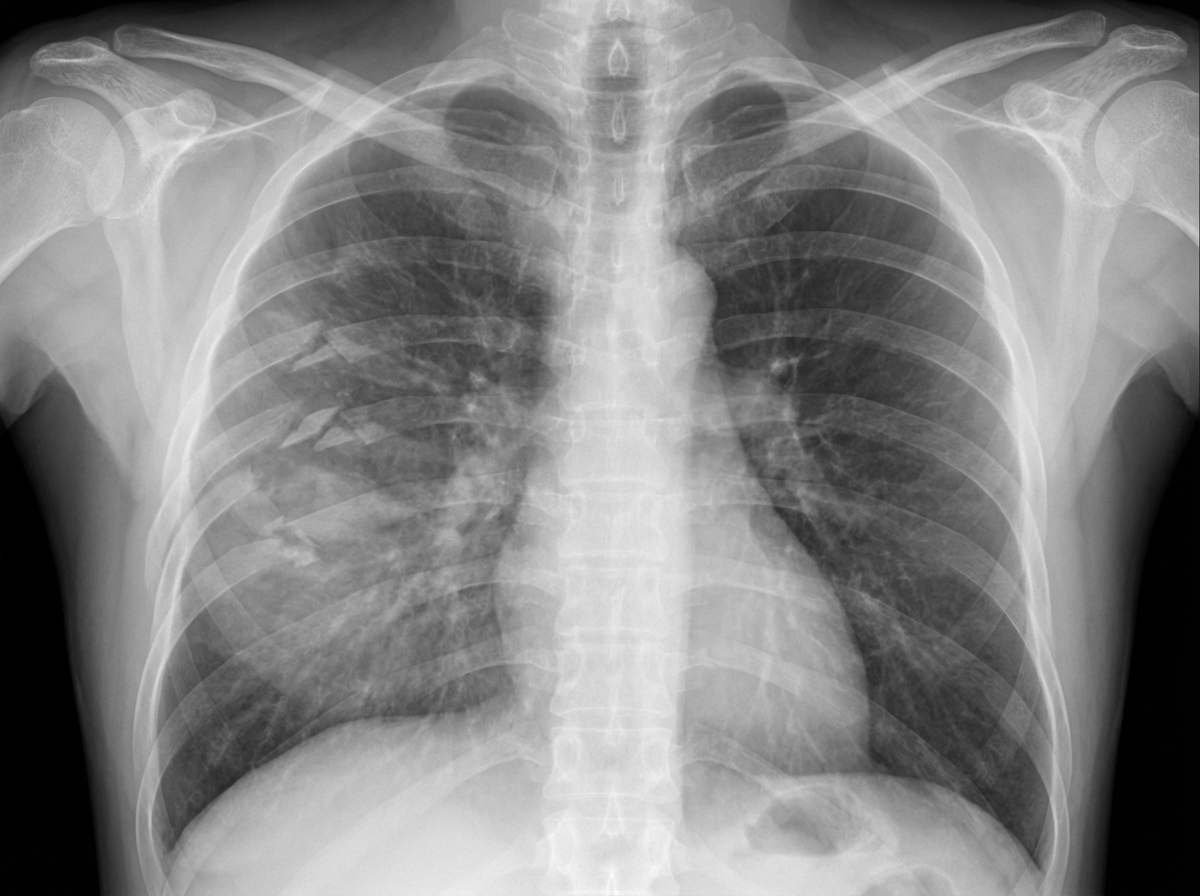
Trauma assessment in children US Medical PG Question 1: A 27-year-old man is brought to the emergency department 45 minutes after being involved in a motor vehicle collision. He is agitated. He has pain in his upper right arm, which he is cradling in his left arm. His temperature is 36.7°C (98°F), pulse is 135/min, respirations are 25/min, and blood pressure is 145/90 mm Hg. His breathing is shallow. Pulse oximetry on 100% oxygen via a non-rebreather face mask shows an oxygen saturation of 83%. He is confused and oriented only to person. Examination shows multiple bruises on the right anterior thoracic wall. The pupils are equal and reactive to light. On inspiration, his right chest wall demonstrates paradoxical inward movement while his left chest wall is expanding. There is pain to palpation and crepitus over his right anterior ribs. The remainder of the examination shows no abnormalities. An x-ray of the chest is shown. Two large-bore IVs are placed. After fluid resuscitation and analgesia, which of the following is the most appropriate next step in management?
- A. Bedside thoracotomy
- B. Surgical fixation of right third to sixth ribs
- C. Intubation with positive pressure ventilation (Correct Answer)
- D. Placement of a chest tube
- E. CT scan of the chest
Trauma assessment in children Explanation: ***Intubation with positive pressure ventilation***
- The patient presents with **flail chest** (paradoxical chest wall movement with pain and crepitus), respiratory distress (tachypnea, shallow breathing), and **hypoxemia** (SpO2 83% on 100% oxygen) despite initial fluid resuscitation and analgesia. These are clear indications for **endotracheal intubation** and mechanical ventilation to stabilize the chest wall, improve oxygenation, and reduce the work of breathing.
- **Positive pressure ventilation** helps to internally splint the flail segment, enabling more effective gas exchange and preventing further atelectasis.
*Bedside thoracotomy*
- **Bedside thoracotomy** is typically reserved for patients in traumatic cardiac arrest who have witnessed signs of life on arrival or are in profound shock unresponsive to other resuscitative measures, making it inappropriate here.
- This patient is **hemodynamically stable** (BP 145/90 mmHg) and does not show signs of massive hemorrhage or cardiac tamponade requiring immediate thoracotomy.
*Surgical fixation of right third to sixth ribs*
- **Surgical fixation of rib fractures** is a more definitive treatment for flail chest but is not an immediate life-saving intervention in the setting of acute respiratory failure and hypoxemia.
- While it can be considered later to reduce pain and improve pulmonary mechanics, the priority is to stabilize the patient's respiratory status through **ventilation**.
*Placement of a chest tube*
- **Placement of a chest tube** is indicated for pneumothorax, hemothorax, or empyema. While a pneumothorax or hemothorax could be present given the trauma and rib fractures, the primary issue driving this patient's acute respiratory failure is the **flail chest leading to inadequate ventilation and oxygenation**.
- There is no mention of diminished breath sounds or hyperresonance/dullness to percussion, which would suggest pneumothorax or hemothorax as the primary and immediate problem after initial resuscitation.
*CT scan of the chest*
- A **CT scan of the chest** is an important diagnostic tool to assess the extent of injuries, but it is not an immediate therapeutic intervention for a patient in acute respiratory failure and severe hypoxemia.
- Delaying definitive airway management for a diagnostic test in an unstable patient is **inappropriate** and could worsen the patient's condition.
Trauma assessment in children US Medical PG Question 2: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
Trauma assessment in children Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
Trauma assessment in children US Medical PG Question 3: A 7-year-old boy presents to the pediatric emergency department for knee pain. The child fell while riding his skateboard yesterday. He claims that ever since then he has had swelling and knee pain that is severe. His parents state that he has trouble walking due to the pain. The child has a past medical history of seasonal allergies and asthma. His current medications include loratadine, albuterol, and fluticasone. His temperature is 99.5°F (37.5°C), blood pressure is 95/48 mmHg, pulse is 110/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note a young boy laying on the stretcher in pain. Cardiopulmonary exam is within normal limits. Inspection of the patient's left knee reveals an erythematous knee that is tender and warm to the touch. Passive movement of the knee elicits pain. The patient refuses to walk so you are unable to assess his gait. Which of the following is the best initial step in management?
- A. ESR, CRP, and CBC
- B. Arthrocentesis (Correct Answer)
- C. CT scan
- D. Antibiotics
- E. Supportive therapy and further physical exam
Trauma assessment in children Explanation: ***Arthrocentesis***
- The patient presents with classic signs of **septic arthritis**, including acute onset of severe knee pain, warmth, erythema, tenderness, and refusal to bear weight, especially following a minor trauma which can sometimes be a precipitating factor or merely draw attention to existing infection.
- **Arthrocentesis** is the most crucial diagnostic and therapeutic step in suspected septic arthritis, as it allows for fluid analysis (cell count, Gram stain, culture) to identify the causative organism and guide targeted antibiotic therapy.
*ESR, CRP, and CBC*
- While these labs (erythrocyte sedimentation rate, C-reactive protein, and complete blood count) are important for assessing the degree of **inflammation** and **infection**, they are not the definitive initial step for diagnosing septic arthritis.
- These tests support the suspicion of infection but do not provide the specific bacterial diagnosis or immediate relief of joint pressure that arthrocentesis offers.
*CT scan*
- A CT scan is generally not the initial diagnostic modality for **acute septic arthritis** unless there is a concern for osteomyelitis or other bony involvement not clearly visible on plain radiographs or if aspiration is difficult.
- **Plain radiographs** are usually the first imaging study to rule out fracture or other bony pathology, but they cannot diagnose joint infection.
*Antibiotics*
- While antibiotics are essential for treating septic arthritis, initiating them **before
arthrocentesis** can **sterilize the joint fluid**, making culture results negative and hindering the identification of the specific pathogen.
- Empirical antibiotics should only begin *after* joint fluid has been aspirated for diagnostic purposes.
*Supportive therapy and further physical exam*
- Supportive therapy (e.g., pain control, immobilization) is important but **insufficient** as the sole initial management for suspected septic arthritis, which is a **medical emergency**.
- Delaying definitive diagnosis and treatment (arthrocentesis) can lead to **rapid joint destruction** and long-term morbidity, outweighing the benefit of further physical exam beyond initial assessment.
Trauma assessment in children US Medical PG Question 4: A 6-month-old male presents to the emergency department with his parents after his three-year-old brother hit him on the arm with a toy truck. His parents are concerned that the minor trauma caused an unusual amount of bruising. The patient has otherwise been developing well and meeting all his milestones. His parents report that he sleeps throughout the night and has just started to experiment with solid food. The patient’s older brother is in good health, but the patient’s mother reports that some members of her family have an unknown blood disorder. On physical exam, the patient is agitated and difficult to soothe. He has 2-3 inches of ecchymoses and swelling on the lateral aspect of the left forearm. The patient has a neurological exam within normal limits and pale skin with blue irises. An ophthalmologic evaluation is deferred.
Which of the following is the best initial step?
- A. Genetic testing
- B. Complete blood count and coagulation panel (Correct Answer)
- C. Ensure the child's safety and alert the police
- D. Peripheral blood smear
- E. Hemoglobin electrophoresis
Trauma assessment in children Explanation: ***Complete blood count and coagulation panel***
- The unusual amount of **bruising** after minor trauma, along with a family history of an unknown blood disorder, strongly suggests a potential **bleeding disorder**. A **CBC** and a **coagulation panel** (PT, aPTT, fibrinogen) are essential initial steps to evaluate for abnormalities in platelets, clotting factors, or other hematologic conditions.
- These tests can help narrow down the differential diagnosis between **platelet dysfunction**, **coagulopathies** (like hemophilia or von Willebrand disease), or other less common bleeding disorders, guiding further specific investigations.
- **Important consideration:** The presence of **blue sclera** (described as "blue irises") raises concern for **osteogenesis imperfecta (OI)**, a connective tissue disorder causing bone fragility. However, initial hematologic screening is still appropriate given the family history of blood disorder and presentation of excessive bruising. If coagulation studies are normal, imaging and further workup for OI would be indicated.
*Genetic testing*
- While a genetic component is plausible given the patient's family history and clinical presentation (blue sclera may suggest osteogenesis imperfecta), **genetic testing** is typically performed *after* initial laboratory workup has identified a specific type of bleeding or inherited disorder.
- Starting with genetic testing without basic hematologic parameters is not the most efficient or cost-effective initial diagnostic approach.
*Ensure the child's safety and alert the police*
- While child abuse should always be considered in cases of unexplained or excessive bruising, the presence of a **family history of a blood disorder** and the **blue sclera** (suggesting possible osteogenesis imperfecta) make **medical causes** more immediate concerns for initial investigation.
- Pursuing a medical workup first often clarifies whether abuse is the primary explanation, although child protective services should be notified if suspicion remains high after medical evaluation.
*Peripheral blood smear*
- A **peripheral blood smear** provides information on red blood cell morphology, platelet size and number, and white blood cell differential. While useful in assessing for some hematologic conditions, it is often performed *after* a CBC has indicated abnormalities or in conjunction with specialized testing.
- It would not be the *best initial step* as it doesn't directly assess clotting factor function, which is critical in evaluating significant bruising severity.
*Hemoglobin electrophoresis*
- **Hemoglobin electrophoresis** is used to diagnose **hemoglobinopathies** like sickle cell anemia or thalassemia.
- The patient's symptoms (easy bruising) are not characteristic of hemoglobinopathies, and while he has pale skin, this test would not be the initial step to investigate a bleeding disorder.
Trauma assessment in children US Medical PG Question 5: A 1-minute-old newborn is being examined by the pediatric nurse. The nurse auscultates the heart and determines that the heart rate is 89/min. The respirations are spontaneous and regular. The chest and abdomen are both pink while the tips of the fingers and toes are blue. When the newborn’s foot is slapped the face grimaces and he cries loud and strong. When the arms are extended by the nurse they flex back quickly. What is this patient’s Apgar score?
- A. 5
- B. 10
- C. 8 (Correct Answer)
- D. 6
- E. 9
Trauma assessment in children Explanation: ***8***
- The Apgar score is calculated by assigning 0, 1, or 2 points to five criteria: **Appearance**, **Pulse**, **Grimace (reflex irritability)**, **Activity (muscle tone)**, and **Respiration**.
- This newborn scores 1 point for **Appearance** (pink body, blue extremities/acrocyanosis), 1 point for **Pulse** (89/min, which is below 100), 2 points for **Grimace** (cries loud and strong), 2 points for **Activity** (arms flex back quickly), and 2 points for **Respiration** (spontaneous and regular), totaling **8**.
*5*
- An Apgar score of 5 would indicate a more compromised state, with lower scores in multiple categories.
- This newborn demonstrates strong respiratory effort, vigorous cry, and active muscle tone, all inconsistent with a score of 5.
*10*
- A perfect score of 10 is rare and would require the newborn to have a **pink appearance throughout** (including extremities), a heart rate over 100 bpm, strong cry, active movement, and vigorous breathing.
- This newborn has two findings preventing a score of 10: **acrocyanosis** (blue extremities) and **heart rate of 89/min** (below 100).
*6*
- An Apgar score of 6 would imply more significant compromise, such as weak respiratory effort, minimal response to stimulation, or poor muscle tone.
- This newborn's strong cry, vigorous grimace response, and quick flexion indicate better performance than a score of 6.
*9*
- A score of 9 would mean only one parameter scores 1 point, with all others scoring 2 points.
- This newborn has **two parameters scoring 1 point**: **Appearance** (acrocyanosis) and **Pulse** (89/min, below 100), making the maximum possible score 8, not 9.
Trauma assessment in children US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Trauma assessment in children Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Trauma assessment in children US Medical PG Question 7: A mother brings her 6-month-old boy to the emergency department. She reports that her son has been breathing faster than usual for the past 2 days, and she has noted occasional wheezing. She states that prior to the difficulty breathing, she noticed some clear nasal discharge for several days. The infant was born full-term, with no complications, and no significant medical history. His temperature is 100°F (37.8°C), blood pressure is 60/30 mmHg, pulse is 120/min, respirations are 40/min, and oxygen saturation is 95% on room air. Physical exam reveals expiratory wheezing, crackles diffusely, and intercostal retractions. The child is currently playing with toys. Which of the following is the most appropriate next step in management?
- A. Monitoring (Correct Answer)
- B. Intubation
- C. Albuterol
- D. Chest radiograph
- E. Azithromycin and ceftriaxone
Trauma assessment in children Explanation: ***Monitoring (Supportive Care)***
- This infant presents with classic **viral bronchiolitis** (tachypnea, wheezing, crackles, retractions following upper respiratory symptoms)
- The child is **clinically stable**: O2 saturation 95% on room air, alert and playing with toys
- **Current AAP guidelines** recommend **supportive care only** for bronchiolitis, which includes monitoring vital signs, assessing work of breathing, ensuring adequate hydration, and oxygen supplementation if saturation drops below 90%
- This patient requires close observation but no immediate intervention given stable vital signs and reassuring clinical appearance
*Albuterol*
- **Bronchodilators are NOT recommended** for routine use in bronchiolitis per current AAP clinical practice guidelines
- Multiple randomized controlled trials have shown **no significant benefit** from albuterol in bronchiolitis
- While a trial may be considered in select cases with strong family history of asthma, routine use is discouraged
- Bronchiolitis is caused by **small airway inflammation and mucus plugging**, not bronchospasm
*Intubation*
- **Intubation** is reserved for severe respiratory failure with impending respiratory arrest, persistent hypoxemia despite high-flow oxygen, apnea, or altered mental status
- This child has adequate oxygenation (95%), is alert, and playing—**no indication for intubation**
- Signs that would warrant intubation include lethargy, severe retractions with fatigue, O2 sat <90% despite supplementation
*Chest radiograph*
- **Not routinely indicated** in typical bronchiolitis
- Consider only if there's diagnostic uncertainty, concern for complications (pneumothorax, lobar consolidation suggesting bacterial pneumonia), or failure to improve with supportive care
- The clinical presentation is clearly consistent with bronchiolitis, and imaging would not change initial management
*Azithromycin and ceftriaxone*
- Bronchiolitis is a **viral infection** (most commonly RSV), and **antibiotics provide no benefit**
- Antibiotics should only be used if there is clear evidence of **bacterial superinfection** (high fever, focal consolidation, elevated inflammatory markers)
- Routine antibiotic use contributes to antimicrobial resistance and adverse effects
Trauma assessment in children US Medical PG Question 8: A 2-year-old girl is brought to the emergency department after swallowing a button battery that was lying on the table 1 hour ago. She has no shortness of breath or chest discomfort. Her pulse is 112/min and respirations are 30/min. Pulse oximetry on room air shows an oxygen saturation of 98%. Physical examination shows no abnormalities. An x-ray of the chest shows the battery lodged in the esophagus at the level of T2. Which of the following is the most appropriate next step in management?
- A. Removal of the battery with magnet and nasogastric tube
- B. Administer syrup of ipecac
- C. Administer chelation therapy
- D. Endoscopic removal of the battery (Correct Answer)
- E. Reassurance and observation
Trauma assessment in children Explanation: ***Endoscopic removal of the battery***
- A button battery lodged in the esophagus is a **medical emergency** requiring prompt removal due to the risk of **corrosive injury, perforation, and fistula formation**.
- **Endoscopic removal** allows direct visualization and controlled extraction, minimizing further damage.
*Removal of the battery with magnet and nasogastric tube*
- While magnets can be used for foreign body removal in some cases, a **nasogastric tube is not an appropriate tool for safely extracting a button battery from the esophagus**.
- This method poses a risk of further trauma to the esophageal wall or dislodging the battery into the airway.
*Administer syrup of ipecac*
- **Syrup of ipecac induces emesis**, which is contraindicated here as it could lead to further esophageal damage, aspiration, or lodging the battery elsewhere in the GI tract.
- Its use for ingested foreign bodies is generally **discouraged**.
*Administer chelation therapy*
- **Chelation therapy is used for heavy metal poisoning**, such as lead or mercury, not for the direct removal of an ingested foreign body like a battery.
- The primary concern with button batteries is **local corrosive injury**, not systemic toxicity from metal absorption (unless it perforates).
*Reassurance and observation*
- This approach is dangerously inappropriate for an esophageal button battery, as **damage can occur within hours**, leading to strictures, perforation, and even death.
- Immediate intervention is crucial, even if the patient appears asymptomatic initially.
Trauma assessment in children US Medical PG Question 9: A 5-year-old boy is brought to the emergency department by his grandmother because of difficulty breathing. Over the past two hours, the grandmother has noticed his voice getting progressively hoarser and occasionally muffled, with persistent drooling. He has not had a cough. The child recently immigrated from Africa, and the grandmother is unsure if his immunizations are up-to-date. He appears uncomfortable and is sitting up and leaning forward with his chin hyperextended. His temperature is 39.5°C (103.1°F), pulse is 110/min, and blood pressure is 90/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 95%. Pulmonary examination shows inspiratory stridor and scattered rhonchi throughout both lung fields, along with poor air movement. Which of the following is the most appropriate next step in management?
- A. Nebulized albuterol
- B. Direct laryngoscopy and pharyngoscopy
- C. Immediate nasotracheal intubation in the emergency department
- D. Prepare for emergency airway management in the operating room with anesthesia and ENT backup (Correct Answer)
- E. Intravenous administration of antibiotics
Trauma assessment in children Explanation: ***Prepare for emergency airway management in the operating room with anesthesia and ENT backup***
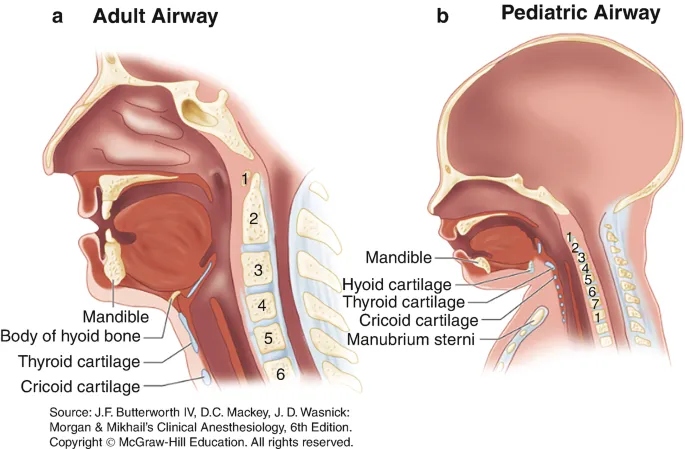
- The constellation of **hoarseness**, **muffled voice**, **drooling**, **inspiratory stridor**, **fever**, and the classic **tripod position** (sitting up, leaning forward, hyperextended chin) in an unimmunized child strongly indicates **epiglottitis**.
- Given the risk of **complete airway obstruction**, securing the airway in a controlled environment like the **operating room** with specialized personnel (**anesthesia**, **ENT**) is the safest and most appropriate immediate step.
*Nebulized albuterol*
- This medication is a **bronchodilator** primarily used for conditions like **asthma** or **bronchiolitis** that involve bronchospasm.
- It would not alleviate airway obstruction caused by supraglottic swelling in epiglottitis and could potentially worsen the child's distress.
*Direct laryngoscopy and pharyngoscopy*
- Performing a direct laryngoscopy or pharyngoscopy in the emergency department, especially without immediate intubation capabilities, could precipitate **laryngospasm** and **complete airway obstruction** in a child with suspected epiglottitis.
- Visualization of the airway should only be attempted in a controlled setting where immediate intubation or tracheostomy can be performed.
*Immediate nasotracheal intubation in the emergency department*
- While intubation is necessary, attempting it immediately in the emergency department without the controlled environment of an operating room and without the full support of anesthesia and ENT specialists carries significant risks.
- The swelling can make intubation extremely difficult and increase the likelihood of failed attempts or trauma, further compromising the airway.
*Intravenous administration of antibiotics*
- Although antibiotics are a crucial part of epiglottitis treatment (typically **ceftriaxone** or **cefotaxime** to cover *Haemophilus influenzae* type b), they are not the immediate priority.
- The most urgent threat is airway compromise; therefore, securing the airway takes precedence over initiating antibiotic therapy.
Trauma assessment in children US Medical PG Question 10: A 2-year-old girl is brought to her pediatrician’s office with intermittent and severe stomach ache and vomiting for the last 2 days. Last week the whole family had a stomach bug involving a few days of mild fever, lack of appetite, and diarrhea but they have all made a full recovery since. This current pain is different from the type she had during infection. With the onset of pain, the child cries and kicks her legs up in the air or pulls them to her chest. The parents have also observed mucousy stools and occasional bloody stools that are bright red and mucousy. After a while, the pain subsides and she returns to her normal activity. Which of the following would be the next step in the management of this patient?
- A. Abdominal radiograph
- B. Air enema (Correct Answer)
- C. Abdominal CT scan
- D. Surgical reduction
- E. Observe for 24 hours
Trauma assessment in children Explanation: ***Air enema***
- The clinical presentation with intermittent abdominal pain, leg drawing to the chest, "currant jelly" stools (bloody and mucousy), and a recent viral illness is highly suggestive of **intussusception**. An **air enema** is the diagnostic and therapeutic modality of choice for intussusception.
- It uses pneumatic pressure to reduce the telescoping of the bowel, and if successful, avoids the need for surgery.
*Abdominal radiograph*
- An **abdominal radiograph** may show signs of obstruction or a "target sign" (if present), but it is not sensitive or specific enough to definitively diagnose intussusception.
- It is primarily used to rule out perforation before performing an air enema if there are concerns about peritonitis.
*Abdominal CT scan*
- While an **abdominal CT scan** can diagnose intussusception, it exposes the child to significant radiation and is not typically the first-line imaging modality.
- It is usually reserved for cases where other diagnostic methods are inconclusive or if complications like perforation are suspected.
*Surgical reduction*
- **Surgical reduction** is indicated if an air enema fails to reduce the intussusception, if there are signs of bowel perforation or peritonitis, or if the patient is unstable.
- It is an invasive procedure and should not be the initial step in management unless there are clear contraindications to pneumatic reduction.
*Observe for 24 hours*
- Observing the child for 24 hours without intervention is inappropriate and can lead to serious complications, such as **bowel ischemia, necrosis, perforation, and sepsis**.
- Intussusception is a medical emergency that requires prompt diagnosis and treatment.
More Trauma assessment in children US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.