Toxicologic emergencies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Toxicologic emergencies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Toxicologic emergencies US Medical PG Question 1: A 25-year-old woman presents to the ED with nausea, vomiting, diarrhea, abdominal pain, and hematemesis after ingesting large quantities of a drug. Which of the following pairs a drug overdose with the correct antidote for this scenario?
- A. Iron; deferoxamine (Correct Answer)
- B. Organophosphate; physostigmine
- C. Atropine; fomepizole
- D. Aspirin; N-acetylcysteine
- E. Acetaminophen; naloxone
Toxicologic emergencies Explanation: ***Iron; deferoxamine***
- The symptoms of **nausea, vomiting, diarrhea, abdominal pain, and hematemesis** are classic signs of **iron overdose**, which causes direct corrosive injury to the GI mucosa.
- **Deferoxamine** is a **chelating agent** specifically used to bind iron ions and facilitate their excretion, thus reversing iron toxicity.
*Organophosphate; physostigmine*
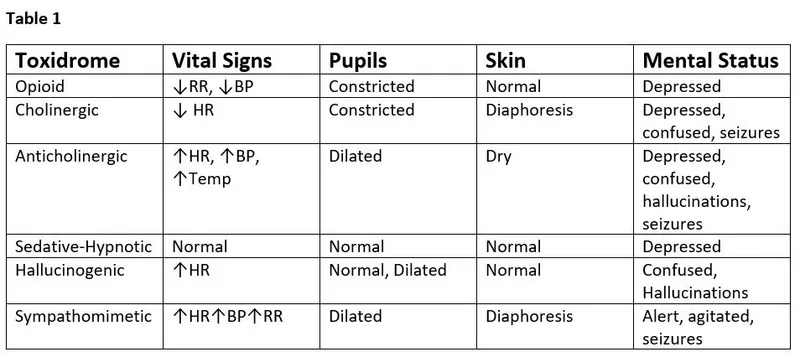
- **Organophosphate poisoning** presents with a **cholinergic crisis** (SLUDGE: salivation, lacrimation, urination, defecation, GI upset, emesis, miosis), but **hematemesis** is not a primary feature.
- **Physostigmine** is an acetylcholinesterase inhibitor used for atropine overdose, not organophosphate poisoning; **atropine** and **pralidoxime** are the antidotes for organophosphate.
*Atropine; fomepizole*
- **Atropine overdose** causes **anticholinergic symptoms** (dry mouth, blurred vision, tachycardia, urinary retention, delirium), not GI irritation and hematemesis.
- **Fomepizole** is an antidote for **methanol** or **ethylene glycol poisoning**, not atropine.
*Aspirin; N-acetylcysteine*
- **Aspirin overdose** (salicylate toxicity) results in **tinnitus, hyperventilation, metabolic acidosis, and altered mental status**, but **hematemesis** is less common than with iron.
- **N-acetylcysteine** is the antidote for acetaminophen overdose, not aspirin; aspirin overdose is treated with **alkalinization of urine** and **hemodialysis**.
*Acetaminophen; naloxone*
- **Acetaminophen overdose** primarily causes **hepatic toxicity**, initially presenting with non-specific GI symptoms, but **hematemesis** is atypical, and the main concern is liver damage.
- **Naloxone** is an opioid antagonist used to reverse opioid overdose, not acetaminophen.
Toxicologic emergencies US Medical PG Question 2: A 3-year-old girl swallowed a handful of pills after her grandmother dropped the bottle on the ground this afternoon. She presents to the ER in a very drowsy but agitated state. She is clutching her abdomen, as if in pain, her skin is dry and flushed, and she does not know her name or where she is. Her pupils are dilated. Her grandmother reports that she has not urinated in several hours. The grandmother's medical history is significant for allergic rhinitis and osteoarthritis, both of which are treated with over the counter medications. What is the appropriate treatment for this child?
- A. N-acetylcysteine
- B. Naloxone
- C. Physostigmine (Correct Answer)
- D. Deferoxamine
- E. Atropine
Toxicologic emergencies Explanation: ***Physostigmine*** is the correct answer.
- The patient's presentation with **dry, flushed skin**, **dilated pupils**, agitation, drowsiness, abdominal pain, and urinary retention is highly suggestive of **anticholinergic toxicity**.
- **Physostigmine** is a **cholinesterase inhibitor** that increases acetylcholine levels, directly reversing the effects of anticholinergic poisoning.
*N-acetylcysteine*
- **N-acetylcysteine** is the specific antidote for **acetaminophen overdose**, which is not indicated by the patient's symptoms.
- The symptoms described do not match the typical presentation of acetaminophen toxicity (e.g., hepatic damage).
*Naloxone*
- **Naloxone** is used to reverse **opioid overdose**, which typically presents with respiratory depression and miosis (pinpoint pupils), contrary to this patient's dilated pupils and lack of respiratory compromise.
- The clinical picture does not suggest opioid intoxication.
*Deferoxamine*
- **Deferoxamine** is a chelating agent used to treat **iron overdose**, which can cause gastrointestinal symptoms but does not typically present with the anticholinergic signs seen here.
- There are no indications of iron toxicity in the patient's history or symptoms.
*Atropine*
- **Atropine** is an **anticholinergic agent** itself and would worsen the patient's symptoms by further blocking acetylcholine receptors.
- It is used to treat cholinergic crises, not overdose of anticholinergic drugs.
Toxicologic emergencies US Medical PG Question 3: A 6-year-old boy is brought to the emergency department 12 hours after ingesting multiple pills. The patient complains of noise in both his ears for the past 10 hours. The patient’s vital signs are as follows: pulse rate, 136/min; respirations, 39/min; and blood pressure, 108/72 mm Hg. The physical examination reveals diaphoresis. The serum laboratory parameters are as follows:
Na+ 136 mEq/L
Cl- 99 mEq/L
Arterial blood gas analysis under room air indicates the following results:
pH 7.39
PaCO2 25 mm HG
HCO3- 15 mEq/L
Which of the following is the most appropriate first step in the management of this patient?
- A. Hemodialysis
- B. Supportive care
- C. Gastrointestinal decontamination
- D. Urine alkalinization (Correct Answer)
- E. Multiple-dose activated charcoal
Toxicologic emergencies Explanation: ***Urine alkalinization***
- This patient likely has **salicylate toxicity** (suggested by **tinnitus**, hyperpnea leading to **respiratory alkalosis** followed by **metabolic acidosis**, and diaphoresis), for which **urine alkalinization** is a primary treatment.
- Making the urine alkaline helps to **ionize salicylates**, trapping them in the renal tubules and increasing their renal excretion.
*Hemodialysis*
- **Hemodialysis** is reserved for severe salicylate toxicity, such as refractory acidosis, severe central nervous system effects, renal failure, or very high salicylate levels, not as a first step.
- While it can remove salicylates, less invasive and effective options like urine alkalinization should be attempted first.
*Supportive care*
- While essential, **supportive care** alone (e.g., maintaining hydration, monitoring vital signs) is not sufficient for active management of significant salicylate overdose.
- It does not address the underlying toxicology, which requires specific interventions to enhance drug elimination.
*Gastrointestinal decontamination*
- **Single-dose activated charcoal** would be indicated if the ingestion was within 1-2 hours, but 12 hours have passed, making it less effective.
- Other GI decontamination methods like **gastric lavage** are rarely indicated and generally not recommended beyond 1 hour post-ingestion due to risks versus benefits.
*Multiple-dose activated charcoal*
- **Multiple-dose activated charcoal (MDAC)** is used for drugs that undergo enterohepatic recirculation or have delayed absorption, but its efficacy in salicylate poisoning, especially 12 hours post-ingestion, is debated and not a first-line intervention.
- Urine alkalinization is a more direct and effective method for accelerating salicylate elimination from the body.
Toxicologic emergencies US Medical PG Question 4: A 30-year-old man is brought to the emergency department by his brother for the evaluation of progressive confusion over the past 6 hours. The patient is lethargic and unable to answer questions. His brother states that there is no personal or family history of serious illness. His temperature is 37°C (98.6°F), pulse is 110/min, and blood pressure 135/80 mm Hg. Physical examination shows warm, dry skin and dry mucous membranes. The pupils are dilated. The abdomen is distended and bowel sounds are hypoactive. Laboratory studies are within normal limits. An ECG shows no abnormalities. Intoxication with which of the following substances is the most likely cause of this patient's symptoms?
- A. Cannabis
- B. Amphetamine
- C. Opioid
- D. Carbon monoxide
- E. Antihistamine (Correct Answer)
Toxicologic emergencies Explanation: ***Antihistamine***
- The patient's symptoms, including **dilated pupils**, confusion, lethargy, dry skin and mucous membranes, distended abdomen, and hypoactive bowel sounds, are consistent with an **anticholinergic toxidrome**. This pattern is often seen with antihistamine overdose due to their anticholinergic properties.
- The elevated pulse despite normal blood pressure and temperature also aligns with anticholinergic effects.
*Cannabis*
- Cannabis intoxication typically causes **conjunctival injection**, xerostomia, increased appetite, and impaired coordination.
- While it can cause lethargy, it does not explain the dilated pupils, dry mucous membranes, or hypoactive bowel sounds.
*Amphetamine*
- Amphetamine intoxication usually presents with **tachycardia**, hypertension, agitation, paranoia, and diaphoresis, not dry skin or hypoactive bowel sounds.
- Though pupils are typically dilated, the overall clinical picture points away from amphetamine overdose.
*Opioid*
- Opioid overdose is characterized by **respiratory depression**, **miosis (pinpoint pupils)**, and altered mental status, which contradict the dilated pupils and normal respiratory effort (implied by normal oxygenation and stable vital signs) in this case.
- While it can cause lethargy and hypoactive bowel sounds, other key features are missing or are opposite.
*Carbon monoxide*
- Carbon monoxide poisoning classically presents with **headache**, nausea, vomiting, confusion, and sometimes the classic "**cherry-red skin**" (though this is rare and late).
- It does not cause dilated pupils, dry mucous membranes, or hypoactive bowel sounds as seen in this patient.
Toxicologic emergencies US Medical PG Question 5: A steel welder presents to his family physician with a one-week history of intense abdominal cramping with nausea, vomiting, constipation, headaches, myalgias, and arthralgias. He claims that the symptoms started about two months after he began work on replacing the pipes in an early 20th century house. Blood was taken and he was found to have a microcytic, hypochromic anemia with basophilic stippling. Which of the following is the best treatment for his symptoms?
- A. Prussian blue
- B. Deferasirox
- C. EDTA (Correct Answer)
- D. N-acetylcysteine
- E. Deferoxamine
Toxicologic emergencies Explanation: ***EDTA***
- The patient's symptoms (abdominal cramping, nausea, vomiting, constipation, headaches, myalgias, arthralgias), occupation (steel welder working on old pipes), and lab findings (**microcytic, hypochromic anemia** with **basophilic stippling**) are highly suggestive of **lead poisoning**.
- **EDTA (ethylenediaminetetraacetic acid)** is a chelating agent that binds to lead and promotes its excretion, making it the most appropriate treatment for severe lead poisoning.
*Prussian blue*
- This is an antidote for **thallium** and **radioactive cesium poisoning**, not lead.
- It works by trapping these ions in the gut, preventing their absorption and increasing their fecal excretion.
*Deferasirox*
- This is an **oral iron chelator** used for treating **iron overload**, particularly in patients with thalassemia who receive frequent blood transfusions.
- It is not indicated for lead poisoning.
*N-acetylcysteine*
- This agent is primarily used as an antidote for **acetaminophen overdose** by replenishing glutathione stores.
- It also has applications in certain respiratory conditions as a mucolytic, but not in lead poisoning.
*Deferoxamine*
- This is another **iron chelator**, administered intravenously or subcutaneously, primarily used for acute iron intoxication or chronic iron overload (e.g., hemochromatosis).
- Like deferasirox, it is specific for iron and not used for lead poisoning.
Toxicologic emergencies US Medical PG Question 6: A 55-year-old man presents to the emergency department with hematemesis that started 1 hour ago but has subsided. His past medical history is significant for cirrhosis with known esophageal varices which have been previously banded. His temperature is 97.5°F (36.4°C), blood pressure is 114/64 mmHg, pulse is 130/min, respirations are 12/min, and oxygen saturation is 98% on room air. During the patient's physical exam, he begins vomiting again and his heart rate increases with a worsening blood pressure. He develops mental status changes and on exam he opens his eyes and flexes his arms only to sternal rub and is muttering incoherent words. Which of the following is the most appropriate next step in management?
- A. Transfuse blood products
- B. Intubation (Correct Answer)
- C. Emergency surgery
- D. IV fluids and fresh frozen plasma
- E. Emergency variceal banding
Toxicologic emergencies Explanation: ***Intubation***
- The patient exhibits signs of **airway compromise** and hypoxemic respiratory failure due to continuous vomiting and worsening mental status, indicated by a GCS score consistent with severe neurological impairment (GCS < 8).
- **Securing the airway via intubation** is the priority to prevent aspiration and ensure adequate ventilation and oxygenation in a patient with active hematemesis and altered mental status.
*Transfuse blood products*
- While transfusion is often necessary for significant bleeding in variceal hemorrhage, the immediate priority in this deteriorating patient is **airway protection and stabilization**.
- Transfusion alone will not address the immediate risk of **aspiration** or progressive respiratory compromise.
*Emergency surgery*
- Emergency surgery (e.g., portosystemic shunt) for variceal bleeding is typically considered only after **endoscopic and pharmacological therapies have failed** to control hemorrhage.
- It is a **more invasive** and higher-risk procedure that is not the immediate first-line intervention for acute variceal bleeding.
*IV fluids and fresh frozen plasma*
- **IV fluids** are crucial for initial resuscitation in hypovolemic shock, and **fresh frozen plasma (FFP)** can help correct coagulopathy in cirrhotic patients.
- However, these interventions do not address the immediate and critical need for **airway protection** in a patient with active vomiting and declining mental status.
*Emergency variceal banding*
- **Endoscopic variceal banding** is a primary treatment for acute variceal bleeding but requires a **secured airway** and patient cooperation.
- Given the patient's deteriorating mental status and ongoing hematemesis, performing endoscopy immediately without prior intubation carries a high risk of **aspiration**.
Toxicologic emergencies US Medical PG Question 7: A 23-year-old man is brought to the emergency department from a college party because of a 1-hour history of a crawling sensation under his skin. He appears anxious and is markedly pale. His temperature is 38°C (100.4°F), pulse is 104/min, respirations are 18/min, and blood pressure is 145/90 mm Hg. Physical examination shows diaphoretic skin, moist mucous membranes, and dilated pupils. Which of the following substances is most likely the cause of this patient's symptoms?
- A. Scopolamine
- B. Phencyclidine
- C. Cocaine (Correct Answer)
- D. Oxycodone
- E. Lysergic acid diethylamide
Toxicologic emergencies Explanation: ***Cocaine***
- The patient's symptoms of **anxiety**, **diaphoresis**, **mydriasis (dilated pupils)**, and **tachycardia** are consistent with **sympathomimetic toxicity**, commonly seen with cocaine use.
- The **crawling sensation under the skin (formication)**, also known as "cocaine bugs," is a classic symptom of significant cocaine intoxication.
*Scopolamine*
- Scopolamine is an **anticholinergic** agent, causing symptoms like **dry mouth**, **dilated pupils**, and **tachycardia**, but typically also causes dry skin and urinary retention.
- It would not usually present with diaphoresis or the specific crawling sensation.
*Phencyclidine*
- **Phencyclidine (PCP)** intoxication characteristically causes **nystagmus**, **ataxia**, and often leads to **violent behavior** or **agitation**, which are not the primary features described here.
- While it can cause hallucinations and psychosis, the "crawling sensation" is less typical for PCP compared to cocaine.
*Oxycodone*
- **Oxycodone** is an **opioid**, which would typically cause **miosis (constricted pupils)**, **respiratory depression**, and **sedation**, directly contradicting the patient's symptoms.
- It would not lead to anxiety, tachycardia, or diaphoresis in the manner described.
*Lysergic acid diethylamide*
- **Lysergic acid diethylamide (LSD)** is a **hallucinogen** known for causing marked perceptual distortions, vivid hallucinations, and altered thought processes.
- While it can cause autonomic symptoms like sweating and tachycardia, the specific "crawling sensation" is not a hallmark symptom of LSD, and the clinical picture is more suggestive of sympathomimetic overload.
Toxicologic emergencies US Medical PG Question 8: A 27-year-old man is witnessed falling off his bicycle. The patient rode his bicycle into a curb and hit his face against a rail. The patient did not lose consciousness and is ambulatory at the scene. There is blood in the patient's mouth and one of the patient's teeth is found on the sidewalk. The patient is transferred to the local emergency department. Which of the following is the best method to transport this patient's tooth?
- A. Wrapped in gauze soaked in normal saline
- B. Submerged in normal saline
- C. Submerged in milk (Correct Answer)
- D. Wrapped in sterile gauze
- E. Submerged in water
Toxicologic emergencies Explanation: ***Submerged in milk***
- **Milk** is the ideal solution for transporting an avulsed tooth because it has a pH and osmolality that is compatible with the **vitality of the periodontal ligament (PDL) cells**.
- Its nutrient content also helps to sustain these cells, increasing the likelihood of successful **replantation**.
*Wrapped in gauze soaked in normal saline*
- While **normal saline** can keep the tooth moist, its osmolality is not optimal for maintaining the **viability of PDL cells** for an extended period.
- Wrapping in gauze may also cause the tooth to dry out if not kept adequately saturated, which can damage the **periodontal ligament**.
*Submerged in normal saline*
- Submerging in **normal saline** is better than dry storage but is still **suboptimal** compared to milk.
- The tonicity and pH of normal saline are not as beneficial for the **long-term survival of PDL cells** as milk.
*Wrapped in sterile gauze*
- **Sterile gauze** alone does not provide moisture or nutrients, leading to **rapid desiccation and death of PDL cells**.
- A dry environment dramatically reduces the chances of successful **replantation** and increases the risk of **ankylosis** or **resorption**.
*Submerged in water*
- **Water** is a **hypotonic solution** that can cause **lysis of PDL cells** due to osmotic pressure differences.
- This significantly compromises the tooth's viability and success of **replantation**.
Toxicologic emergencies US Medical PG Question 9: A 29-year-old woman, gravida 1, para 0, at 33 weeks' gestation comes to her doctor for a routine visit. Her pregnancy has been uncomplicated. She has systemic lupus erythematosus and has had no flares during her pregnancy. She does not smoke cigarettes, drink alcohol, or use illicit drugs. Current medications include iron, vitamin supplements, and hydroxychloroquine. Her temperature is 37.2°C (98.9°F), pulse is 70/min, respirations are 17/min, and blood pressure is 134/70 mm Hg. She appears well. Physical examination shows no abnormalities. Ultrasound demonstrates fetal rhythmic breathing for > 30 seconds, amniotic fluid with deepest vertical pocket of 1 cm, one distinct fetal body movement over 30 minutes, and no episodes of extremity extension over 30 minutes. Nonstress test is reactive and reassuring. Which of the following is the next best step in management?
- A. Administer corticosteroids and continue close monitoring (Correct Answer)
- B. Perform cesarean delivery
- C. Discontinue hydroxychloroquine and continue close monitoring
- D. Induction of labor
- E. Reassurance with expectant management
Toxicologic emergencies Explanation: ***Administer corticosteroids and continue close monitoring***
- The combination of a **nonreactive nonstress test (NST)** and an **amniotic fluid index (AFI) < 5 cm** (deepest vertical pocket of 1 cm) indicates **oligohydramnios** and potential fetal compromise, necessitating corticosteroid administration for lung maturity and close monitoring.
- While the NST is reassuring, the oligohydramnios is a significant concern that warrants intervention to optimize fetal outcomes and prepare for potential preterm delivery.
*Perform cesarean delivery*
- This step is **overly aggressive** given the reactive nonstress test and stable maternal condition.
- There are no immediate signs of **acute fetal distress** that would necessitate emergent delivery.
*Discontinue hydroxychloroquine and continue close monitoring*
- **Hydroxychloroquine** is safe and often continued during pregnancy for patients with systemic lupus erythematosus, as it helps prevent flares and is not associated with adverse fetal outcomes.
- Discontinuing it without a clear indication could lead to a **maternal SLE flare**, which could be detrimental to both mother and fetus.
*Induction of labor*
- Induction of labor is not indicated at this gestational age (33 weeks) unless there is clear evidence of **significant fetal distress** or maternal complications.
- While there is oligohydramnios, the **reactive NST** suggests sufficient fetal reserve to allow for corticosteroid administration to promote lung maturity first.
*Reassurance with expectant management*
- The finding of **oligohydramnios** (deepest vertical pocket of 1 cm) is a significant concern, as it is associated with increased risks of **cord compression**, fetal growth restriction, and adverse perinatal outcomes.
- Therefore, expectant management without intervention would be **inappropriate** given this finding.
Toxicologic emergencies US Medical PG Question 10: A 38-year-old project manager is told by her boss that her team will need to work on an additional project in the coming week for a very important client. This frustrates the woman, who already feels that she works too many hours. Instead of discussing her feelings directly with her boss, the woman leaves a voice message for her boss the next day and deceitfully says she cannot come to work for the next week because of a family emergency. Which of the following psychological defense mechanisms is this individual demonstrating?
- A. Displacement
- B. Acting out
- C. Malingering
- D. Passive aggression (Correct Answer)
- E. Blocking
Toxicologic emergencies Explanation: ***Passive aggression***
- This defense mechanism involves expressing negative feelings indirectly instead of openly addressing the conflict or frustrating situation. The woman's **deceitful excuse** avoids confrontation while still 'punishing' the boss by not being available.
- It often stems from a fear of direct confrontation and a need to control the situation without appearing openly hostile, manifesting as **procrastination, stubbornness, or intentional inefficiency**.
*Displacement*
- **Displacement** occurs when a person redirects uncomfortable feelings from the source of frustration to a safer, less threatening target.
- In this scenario, the woman did not redirect her frustration onto another person or object; instead, she acted on the source of the frustration indirectly.
*Acting out*
- **Acting out** involves expressing unconscious emotional conflicts or stressors through immediate physical actions, often impulsive or destructive.
- The woman's behavior, while deceitful, is a calculated avoidance rather than an uncontrolled emotional outburst.
*Malingering*
- **Malingering** is the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives like avoiding work or obtaining financial compensation.
- While there is an element of deceit, the primary motivation described is her frustration and desire to avoid the extra work, not necessarily an external material gain typically associated with malingering.
*Blocking*
- **Blocking** is a defense mechanism characterized by a temporary but sudden and complete loss of thought, often due to an emotional conflict. The individual's mind goes blank.
- The woman is not experiencing a loss of thought but is actively fabricating an excuse to avoid a difficult situation.
More Toxicologic emergencies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.