Shock recognition and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Shock recognition and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Shock recognition and management US Medical PG Question 1: A 51-year-old woman is brought into the emergency department following a motor vehicle accident. She is unconscious and was intubated in the field. Past medical history is unknown. Upon arrival, she is hypotensive and tachycardic. Her temperature is 37.2°C (99.1°F), the pulse is 110/min, the respiratory rate is 22/min, and the blood pressure is 85/60 mm Hg. There is no evidence of head trauma, she withdraws to pain and her pupils are 2mm and reactive to light. Her heart has a regular rhythm without any murmurs or rubs and her lungs are clear to auscultation. Her abdomen is firm and distended with decreased bowel sounds. Her extremities are cool and clammy with weak, thready pulses. There is no peripheral edema. Of the following, what is the likely cause of her presentation?
- A. Septic shock
- B. Neurogenic shock
- C. Obstructive shock
- D. Hypovolemic shock (Correct Answer)
- E. Cardiogenic shock
Shock recognition and management Explanation: ***Hypovolemic shock***
- The patient's presentation with ***hypotension*** (BP 85/60 mm Hg), ***tachycardia*** (pulse 110/min), ***cool and clammy extremities***, ***weak peripheral pulses***, and a ***firm, distended abdomen*** after a motor vehicle accident strongly suggests internal hemorrhage leading to hypovolemic shock.
- The ***firm and distended abdomen*** is a key indicator of potential intra-abdominal bleeding, significantly contributing to the loss of intravascular volume.
*Septic shock*
- Septic shock is characterized by signs of infection along with organ dysfunction and circulatory compromise, often presenting with **fever** or **hypothermia**, and sometimes **warm extremities** initially due to vasodilation. This patient's temperature is normal, and extremities are cool.
- While hypotension and tachycardia are present, the absence of clear signs of infection and the presence of a firm, distended abdomen make hypovolemia a more immediate concern following trauma.
*Neurogenic shock*
- Neurogenic shock typically follows severe spinal cord injury above T6, leading to a loss of sympathetic tone. This results in **hypotension with bradycardia** and **warm, dry skin** due to widespread vasodilation.
- This patient is tachycardic and has cool, clammy extremities, which contradicts the classic presentation of neurogenic shock.
*Obstructive shock*
- Obstructive shock occurs due to a physical obstruction to central circulation, such as **tension pneumothorax**, **cardiac tamponade**, or **pulmonary embolism**.
- There is no mention of absent breath sounds, jugular venous distention, muffled heart sounds, or other specific signs pointing to an obstructive cause. Lungs are clear to auscultation and heart rhythm is regular.
*Cardiogenic shock*
- Cardiogenic shock results from primary cardiac dysfunction, often presenting with signs of **heart failure**, such as **pulmonary edema** (rales), **jugular venous distention**, gallop rhythms, or new murmurs.
- The patient has clear lungs, a regular heart rhythm, and no murmurs, which makes primary cardiac dysfunction less likely as the immediate cause of shock in this trauma setting.
Shock recognition and management US Medical PG Question 2: A 27-year-old man is brought to the emergency department after a motor vehicle accident. He was the unrestrained driver in a head on collision. The patient is responding incoherently and is complaining of being in pain. He has several large lacerations and has been impaled with a piece of metal. IV access is unable to be obtained and a FAST exam is performed. His temperature is 98.2°F (36.8°C), blood pressure is 90/48 mmHg, pulse is 150/min, respirations are 13/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Reattempt intravenous access
- B. Obtain intraosseous access (Correct Answer)
- C. Place a central line
- D. Administer oral fluids
- E. Exploratory laparotomy
Shock recognition and management Explanation: ***Obtain intraosseous access***
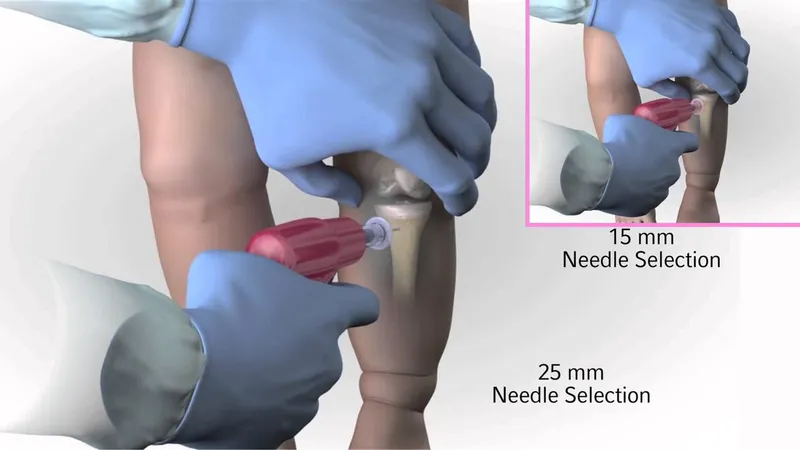
- The patient is in **hypotensive shock** (BP 90/48 mmHg, HR 150/min) after a severe trauma, and **IV access cannot be obtained**. **Intraosseous (IO) access** provides a rapid and reliable route for fluid and medication administration in emergent situations when peripheral IV access is difficult or impossible.
- While central line placement is also a viable option, **IO access is generally faster and easier to establish** in an emergency setting by a wide range of providers, making it the **best initial step** when peripheral IV fails.
*Reattempt intravenous access*
- Although obtaining IV access is critical, the question states that it "is unable to be obtained," implying initial attempts have failed or are proving too difficult/time-consuming given the patient's critical state.
- Persisting with repeated attempts risks significant delay in resuscitation, which is detrimental for a patient in shock.
*Place a central line*
- A central line provides reliable access for fluid and medication, but its placement is generally **more time-consuming** and technically challenging than IO access, especially in an agitated, unstable patient in a chaotic emergency setting.
- The immediate priority is rapid access for fluids to address the patient's shock, for which IO is superior in terms of speed of establishment.
*Administer oral fluids*
- The patient is **unstable**, **incoherently responding**, and likely has significant internal injuries given the mechanism of injury (head-on collision, impalement).
- Oral fluids would be **ineffective** and potentially dangerous (risk of aspiration) in this critical, hemodynamically unstable patient who requires immediate intravenous fluid resuscitation.
*Exploratory laparotomy*
- While the patient likely has significant internal injuries requiring surgical intervention (impalement, hypovolemic shock), an **exploratory laparotomy** is a definitive treatment step, not the *best next step in management* for immediate resuscitation.
- **Hemodynamic stabilization** with fluid resuscitation must occur *before* or *simultaneously with* definitive surgical intervention to improve survival chances.
Shock recognition and management US Medical PG Question 3: An 8-year-old girl is brought to the emergency department by her parents with severe difficulty in breathing for an hour. She is struggling to breathe. She was playing outside with her friends, when she suddenly fell to the ground, out of breath. She was diagnosed with asthma one year before and has since been on treatment for it. At present, she is sitting leaning forward with severe retractions of the intercostal muscles. She is unable to lie down. Her parents mentioned that she has already taken several puffs of her inhaler since this episode began but without response. On physical examination, her lungs are hyperresonant to percussion and there is decreased air entry in both of her lungs. Her vital signs show: blood pressure 110/60 mm Hg, pulse 110/min, respirations 22/min, and a peak expiratory flow rate (PEFR) of 50%. She is having difficulty in communicating with the physician. Her blood is sent for evaluation and a chest X-ray is ordered. Her arterial blood gas reports are as follows:
PaO2 50 mm Hg
pH 7.38
PaCO2 47 mm Hg
HCO3 27 mEq/L
Which of the following is the most appropriate next step in management?
- A. Intravenous corticosteroid (Correct Answer)
- B. Inhaled corticosteroid
- C. Mechanical ventilation
- D. Methacholine challenge test
- E. Inhaled β-agonist
Shock recognition and management Explanation: ***Intravenous corticosteroid***
- The patient exhibits severe asthma exacerbation with **poor response to inhaled β-agonists**, marked respiratory distress, and an alarming **PEFR of 50%**.
- **Intravenous corticosteroids** are crucial in this scenario to reduce airway inflammation and prevent progression to respiratory failure.
*Inhaled corticosteroid*
- While essential for **long-term asthma control**, inhaled corticosteroids are **not effective enough for acute, severe exacerbations** due to their slower onset of action.
- The patient's inability to effectively inhale deeply due to distress also limits the utility of inhaled delivery in this emergency.
*Mechanical ventilation*
- Mechanical ventilation is a **last-resort intervention** for impending respiratory failure, indicated by signs like declining consciousness, hypercapnia, or respiratory arrest.
- While concerning, the patient's current ABG with a **near-normal pH (7.38)** despite hypercapnia suggests she is not yet in full respiratory failure, and less invasive measures should be initiated first.
*Methacholine challenge test*
- The methacholine challenge test is used to **diagnose asthma in stable patients** with normal spirometry, by assessing airway hyperresponsiveness.
- It is **absolutely contraindicated** in an acute, severe asthma exacerbation as it could worsen bronchoconstriction and respiratory distress.
*Inhaled β-agonist*
- The patient has **already taken several puffs of her inhaler** (likely a β-agonist) without response, indicating **refractory bronchospasm**.
- While initially appropriate, repeated administration when ineffective suggests the need for other therapeutic interventions to address the underlying inflammation.
Shock recognition and management US Medical PG Question 4: A 7-month-old boy is brought to the ED by his mother because of abdominal pain. Two weeks ago, she noticed he had a fever and looser stools, but both resolved after a few days. One week ago, he began to experience periodic episodes during which he would curl up into a ball, scream, and cry. The episodes lasted a few minutes, and were occasionally followed by vomiting. Between events, he was completely normal. She says the episodes have become more frequent over time, and this morning, she noticed blood in his diaper. In the ED, his vitals are within normal ranges, and his physical exam is normal. After confirming the diagnosis with an abdominal ultrasound, what is the next step in management?
- A. Supportive care
- B. Broad-spectrum antibiotics
- C. Air contrast enema (Correct Answer)
- D. Abdominal laparotomy
- E. Abdominal CT scan
Shock recognition and management Explanation: ***Air contrast enema***
- An **air contrast enema** is both diagnostic and therapeutic for **intussusception**, which is strongly suggested by the patient's symptoms (colicky abdominal pain, drawing legs to chest, currant jelly stools).
- It uses air pressure to **reduce the intussusception**, avoiding surgery if successful and the bowel is not compromised.
*Supportive care*
- While supportive care (IV fluids, pain control) is important, it does not address the underlying mechanical issue of **intussusception** and would not resolve the condition.
- Delaying definitive treatment for intussusception can lead to **bowel ischemia, necrosis, and perforation**, which are life-threatening.
*Broad-spectrum antibiotics*
- Antibiotics are not the primary treatment for **intussusception**, as it is a mechanical obstruction, not typically a primary infection.
- They might be considered if there are signs of **perforation or peritonitis**, but the immediate goal is reduction.
*Abdominal laparotomy*
- An **abdominal laparotomy** is a surgical intervention reserved for cases where **non-operative reduction** (like an air enema) fails or if there are signs of **bowel perforation or gangrene**.
- It is not the *first-line* next step after diagnosis, especially if non-invasive options remain viable.
*Abdominal CT scan*
- An **abdominal CT scan** can diagnose intussusception but is typically not the preferred initial imaging because it involves **radiation exposure** and **does not offer therapeutic benefit**, unlike an air contrast enema.
- Abdominal ultrasound is usually sufficient for diagnosis and safer for pediatric patients.
Shock recognition and management US Medical PG Question 5: An infant boy of unknown age and medical history is dropped off in the emergency department. The infant appears lethargic and has a large protruding tongue. Although the infant exhibits signs of neglect, he is in no apparent distress. The heart rate is 70/min, the respiratory rate is 30/min, and the temperature is 35.7°C (96.2°F). Which of the following is the most likely cause of the patient’s physical exam findings?
- A. Autosomal dominant mutation in the SERPING1 gene
- B. Genetic imprinting disorder affecting chromosome 11p15.5
- C. Type I hypersensitivity reaction
- D. Excess growth hormone secondary to pituitary gland tumor
- E. Congenital agenesis of an endocrine gland in the anterior neck (Correct Answer)
Shock recognition and management Explanation: ***Congenital agenesis of an endocrine gland in the anterior neck***
- This description is highly suggestive of **congenital hypothyroidism**, caused by **thyroid dysgenesis** (agenesis or hypoplasia of the thyroid gland).
- Symptoms include **lethargy**, **macroglossia** (large protruding tongue), **hypotonia**, **feeding difficulties**, **umbilical hernia**, and **hypothermia**, all consistent with the clinical picture.
*Autosomal dominant mutation in the SERPING1 gene*
- A mutation in the **SERPING1 gene** causes **hereditary angioedema**, characterized by recurrent episodes of unpredictable swelling in various body parts.
- While swelling can affect the tongue, it is typically episodic, painful, and often triggered, which is not suggested by the chronic lethargy and physical signs described.
*Genetic imprinting disorder affecting chromosome 11p15.5*
- This describes **Beckwith-Wiedemann syndrome**, an overgrowth disorder caused by imprinting defects involving genes like **IGF2**, **H19**, and **CDKN1C** on chromosome 11p15.5.
- Features include **macroglossia**, **macrosomia**, **umbilical hernia**, **hemihyperplasia**, and increased risk of embryonal tumors like **Wilms tumor**.
- However, Beckwith-Wiedemann syndrome does not typically present with profound **lethargy** and **hypothermia** as seen in congenital hypothyroidism.
*Type I hypersensitivity reaction*
- A **Type I hypersensitivity reaction** (e.g., anaphylaxis) could cause acute **angioedema** of the tongue, but this would be an acute, rapidly progressing, and life-threatening event.
- The infant's description of being "in no apparent distress" and exhibiting chronic signs like lethargy and hypothermia makes an acute allergic reaction unlikely.
*Excess growth hormone secondary to pituitary gland tumor*
- **Excess growth hormone** (gigantism in children, acromegaly in adults) can cause **macroglossia** and coarse facial features in the long term.
- However, it does not explain the associated **lethargia**, **hypothermia**, and profound developmental delay seen in congenital hypothyroidism in an infant.
Shock recognition and management US Medical PG Question 6: A 6-year-old boy is brought to the emergency room by ambulance, accompanied by his kindergarten teacher. Emergency department staff attempt to call his parents, but they cannot be reached. The boy’s medical history is unknown. According to his teacher, the boy was eating in the cafeteria with friends when he suddenly complained of itching and developed a widespread rash. Physical exam is notable for diffuse hives and tongue edema. His pulse is 100/min and blood pressure is 90/60 mmHg. The boy appears frightened and tells you that he does not want any treatment until his parents arrive. Which of the following is the next best step in the management of this patient?
- A. Immediately administer epinephrine and provide supportive care (Correct Answer)
- B. Continue calling the patient’s parents and do not intubate until verbal consent is obtained over the phone
- C. Obtain written consent to intubate from the patient’s teacher
- D. Wait for the patient's parents to arrive, calm the patient, and provide written consent before intubating
- E. Obtain written consent to intubate from the patient
Shock recognition and management Explanation: ***Immediately administer epinephrine and provide supportive care***
- This patient is experiencing **anaphylaxis**, characterized by diffuse hives, tongue edema, and hypotension (BP 90/60 mmHg in a 6-year-old). **Epinephrine** is the first-line treatment for anaphylaxis and should be administered immediately.
- In an emergency where a child's life is at risk and parents are unreachable, **implied consent** allows for life-saving treatment without explicit parental permission. Delaying treatment for consent would put the child's life at severe risk.
*Continue calling the patient’s parents and do not intubate until verbal consent is obtained over the phone*
- Delaying life-saving treatment like **epinephrine** or potential intubation for anaphylaxis while waiting for parental consent over the phone is unethical and could lead to irreversible harm or death.
- Anaphylaxis with tongue edema and hypotension is a **medical emergency** requiring immediate intervention, irrespective of consent if the patient is a minor and parents are unavailable.
*Obtain written consent to intubate from the patient’s teacher*
- A kindergarten teacher typically **does not have legal authority** to provide consent for invasive medical procedures like intubation for a student.
- The immediate priority is to treat the anaphylaxis with **epinephrine**, not to focus on intubation consent from an unauthorized party.
*Wait for the patient's parents to arrive, calm the patient, and provide written consent before intubating*
- Waiting for parents to arrive for written consent in a rapidly progressing anaphylactic reaction with **airway compromise** (tongue edema) and **hypotension** is extremely dangerous and potentially fatal.
- The patient's expressed wishes or fear do not supersede the immediate need for **life-saving intervention** when a minor's life is at risk and they lack the capacity to make such decisions.
*Obtain written consent to intubate from the patient*
- A 6-year-old child is considered a **minor** and does not have the legal capacity to give informed consent for complex medical procedures like intubation.
- While a child's assent is important, in a life-threatening emergency, the medical team is obligated to provide necessary treatment under the principle of **implied consent**.
Shock recognition and management US Medical PG Question 7: A 57-year-old man is admitted to the burn unit after he was brought to the emergency room following an accidental fire in his house. His past medical history is unknown due to his current clinical condition. Currently, his blood pressure is 75/40 mmHg, pulse rate is 140/min, and respiratory rate is 17/min. The patient is subsequently intubated and started on aggressive fluid resuscitation. A Swan-Ganz catheter is inserted to clarify his volume status. Which of the following hemodynamic parameters would you expect to see in this patient?
- A. Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
- B. Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔
- C. Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔
- D. Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓ (Correct Answer)
- E. Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
Shock recognition and management Explanation: ***Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓***
- The patient's **hypotension (75/40 mmHg)** and **tachycardia (140/min)**, combined with severe burns, indicate **hypovolemic shock** due to massive fluid loss from damaged capillaries.
- In response to decreased cardiac output and hypovolemia, the body compensates by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, and **pulmonary artery wedge pressure (PAWP)** will be low due to reduced intravascular volume.
*Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This option incorrectly suggests that systemic vascular resistance and pulmonary artery wedge pressure would be normal, which is inconsistent with **hypovolemic shock**.
- In shock, the body's compensatory mechanisms would lead to significant changes in SVR and PAWP, not maintain them at baseline.
*Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔*
- Increased cardiac output is usually seen in **distributive shock** (e.g., septic shock) where vasodilation leads to reduced SVR, not increased SVR as suggested here.
- An elevated SVR coupled with an increased cardiac output would typically result in a higher blood pressure unless there is a compensatory drop in other parameters.
*Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔*
- This pattern (high cardiac output, low SVR) is characteristic of **distributive shock**, such as **septic shock** or anaphylactic shock, rather than the hypovolemic shock expected in a burn patient.
- Severe burns primarily cause massive fluid shifts, leading to hypovolemia and a reduced cardiac output, not an elevated one.
*Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This scenario represents **normal hemodynamic parameters**, which would not be expected in a patient experiencing severe shock from extensive burns.
- The patient's clinical presentation (hypotension, tachycardia) clearly indicates a state of hemodynamic instability.
Shock recognition and management US Medical PG Question 8: A previously healthy 5-year-old girl is brought to the emergency department because of difficulty breathing and vomiting that began 1 hour after she took an amoxicillin tablet. She appears anxious. Her pulse is 140/min, respirations are 40/min, and blood pressure is 72/39 mmHg. She has several well-circumscribed, raised, erythematous plaques scattered diffusely over her trunk and extremities. Pulmonary examination shows diffuse, bilateral wheezing. Which of the following is the most appropriate initial pharmacotherapy?
- A. Norepinephrine
- B. Dobutamine
- C. Methylprednisolone
- D. Epinephrine (Correct Answer)
- E. Diphenhydramine
Shock recognition and management Explanation: ***Epinephrine***
- This patient presents with **anaphylaxis** due to amoxicillin, characterized by rapidly developing **respiratory distress** (wheezing, tachypnea), **circulatory compromise** (hypotension, tachycardia), and **cutaneous manifestations** (urticaria).
- **Epinephrine** is the first-line treatment for anaphylaxis because it stabilizes mast cells, causes **vasoconstriction** to improve blood pressure, and promotes **bronchodilation** to alleviate respiratory symptoms.
*Norepinephrine*
- **Norepinephrine** is a potent **vasopressor** primarily used for septic shock or conditions requiring significant vasoconstriction.
- It lacks the bronchodilatory effects and mast cell-stabilizing properties that are crucial in managing the respiratory and systemic inflammatory components of anaphylaxis.
*Dobutamine*
- **Dobutamine** is a **beta-1 adrenergic agonist** primarily used to increase cardiac contractility and heart rate in cases of cardiogenic shock or heart failure.
- It would not address the systemic vasodilation, bronchospasm, or immune-mediated aspects of anaphylaxis effectively.
*Methylprednisolone*
- **Methylprednisolone** is a **corticosteroid** that acts to reduce inflammation and prevent biphasic anaphylactic reactions.
- While important in the overall management of anaphylaxis, it has a delayed onset of action and is not the appropriate initial therapy for acute life-threatening symptoms; **epinephrine** is critical for immediate stabilization.
*Diphenhydramine*
- **Diphenhydramine** is an **antihistamine** that blocks histamine H1 receptors, helping to reduce symptoms such as urticaria and pruritus.
- It does not address the life-threatening aspects of anaphylaxis, such as hypotension and bronchospasm, and should be used as an adjunct rather than initial monotherapy.
Shock recognition and management US Medical PG Question 9: A 3-week-old boy is brought to the emergency department by his parents because of a 3-day history of progressive lethargy and difficulty feeding. He was born at term and did not have difficulty feeding previously. His temperature is 39.4°C (103°F), pulse is 220/min, respirations are 45/min, and blood pressure is 50/30 mm Hg. Pulse oximetry on 100% oxygen shows an oxygen saturation of 97%. Examination shows dry mucous membranes, delayed capillary refill time, and cool skin with poor turgor. Despite multiple attempts by the nursing staff, they are unable to establish peripheral intravenous access. Which of the following is the most appropriate next step in management?
- A. Intraosseous cannulation (Correct Answer)
- B. Ultrasound-guided antecubital vein cannulation
- C. Internal jugular vein cannulation
- D. Intramuscular epinephrine
- E. Rapid sequence intubation
Shock recognition and management Explanation: ***Intraosseous cannulation***
- This infant is in **pediatric septic shock** with signs of **poor perfusion** (delayed capillary refill, cool skin, poor turgor, hypotension) and **difficulty obtaining peripheral intravenous access**.
- **Intraosseous (IO) access** is recommended in pediatric emergencies when IV access cannot be established rapidly, providing a route for fluids, medications, and blood products.
*Ultrasound-guided antecubital vein cannulation*
- While ultrasound can improve success rates for peripheral IVs, the **critical condition** of this infant necessitates immediate vascular access, making IO a faster and more reliable option when peripheral attempts fail.
- Delaying definitive fluid resuscitation and medication administration to attempt a more technically challenging peripheral IV could worsen the patient's outcome.
*Internal jugular vein cannulation*
- **Central venous access (e.g., internal jugular)** is a more invasive and time-consuming procedure with higher risks (e.g., pneumothorax) and is not the first-line access in an emergent, unstable pediatric patient due to the time constraint.
- **IO access** is a quicker and safer route for immediate life-saving interventions in pediatric emergencies.
*Intramuscular epinephrine*
- **Intramuscular epinephrine** is primarily used for the treatment of **anaphylaxis** or in certain cardiac arrest algorithms, neither of which is the primary concern here.
- This patient is in septic shock requiring fluid resuscitation and likely antibiotics, which cannot be adequately delivered via intramuscular injection.
*Rapid sequence intubation*
- While intubation might be considered if the patient's respiratory status deteriorates further or for airway protection, the **immediate priority** is to address the **shock** and **poor perfusion** through vascular access and fluid resuscitation.
- **Intubation** alone will not correct the underlying circulatory collapse and shock state.
Shock recognition and management US Medical PG Question 10: A 68-year-old woman is brought to the emergency department by ambulance after she was found down by her daughter. She lives alone in her apartment so it is unclear when she began to develop symptoms. Her medical history is significant for cardiac arrhythmias, diabetes, pericarditis, and a stroke 2 years ago. On presentation her temperature is 98.1°F (36.7°C), blood pressure is 88/51 mmHg, pulse is 137/min, and respirations are 18/min. On physical exam her skin is cold and clammy. If special tests were obtained, they would reveal dramatically decreased pulmonary capillary wedge pressure, increased systemic vascular resistance, and mildly decreased cardiac output. Which of the following treatments would most directly target the cause of this patient's low blood pressure?
- A. Vasopressors
- B. Intravenous fluids (Correct Answer)
- C. Antibiotic administration
- D. Relieve obstruction
- E. Intravenous inotropes
Shock recognition and management Explanation: ***Intravenous fluids***
- The patient exhibits signs of **hypovolemic shock**, including **hypotension** (BP 88/51 mmHg), **tachycardia** (pulse 137/min), and **cold, clammy skin**. The dramatically decreased **pulmonary capillary wedge pressure (PCWP)** indicates low preload, which is characteristic of hypovolemia.
- Administration of intravenous fluids directly addresses the underlying cause of this patient's low blood pressure by increasing intravascular volume, thereby improving **cardiac preload** and ultimately **cardiac output** and blood pressure.
*Vasopressors*
- While vasopressors can temporarily increase blood pressure by causing **vasoconstriction**, they do not address the root cause of hypovolemic shock, which is insufficient circulating blood volume.
- Using vasopressors without adequate fluid resuscitation in hypovolemic shock can lead to further **organ hypoperfusion** due to increased afterload on an already compromised heart.
*Antibiotic administration*
- Although the patient's presentation with hypotension and tachycardia could raise suspicion for **sepsis**, there is no explicit evidence of infection presented (e.g., fever, focal source).
- The **decreased PCWP** points more strongly towards hypovolemic shock rather than septic shock, where PCWP can be variable or even normal/elevated.
*Relieve obstruction*
- Obstruction, such as in **cardiac tamponade** or **pulmonary embolism**, can cause obstructive shock, which presents with hypotension.
- However, the dramatically **decreased PCWP** is not typically seen in obstructive shock, where PCWP would likely be normal or elevated due to impedance to cardiac filling or outflow.
*Intravenous inotropes*
- **Inotropes** like dobutamine increase myocardial contractility and are primarily indicated in **cardiogenic shock** or severe heart failure with reduced ejection fraction to improve cardiac output.
- While cardiac output is mildly decreased, the primary issue is reduced preload as indicated by the very low PCWP, making fluid resuscitation a more appropriate initial step than directly increasing contractility.
More Shock recognition and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.