Respiratory distress assessment and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory distress assessment and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
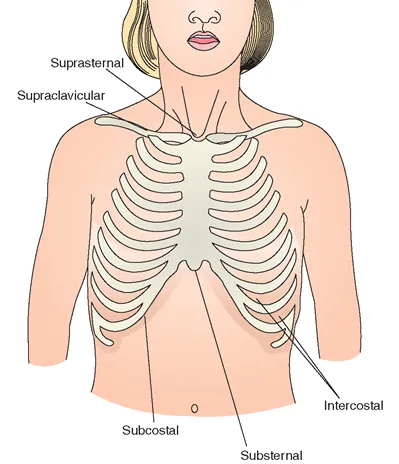
Respiratory distress assessment and management US Medical PG Question 1: An 8-year-old girl is brought to the emergency department by her parents with severe difficulty in breathing for an hour. She is struggling to breathe. She was playing outside with her friends, when she suddenly fell to the ground, out of breath. She was diagnosed with asthma one year before and has since been on treatment for it. At present, she is sitting leaning forward with severe retractions of the intercostal muscles. She is unable to lie down. Her parents mentioned that she has already taken several puffs of her inhaler since this episode began but without response. On physical examination, her lungs are hyperresonant to percussion and there is decreased air entry in both of her lungs. Her vital signs show: blood pressure 110/60 mm Hg, pulse 110/min, respirations 22/min, and a peak expiratory flow rate (PEFR) of 50%. She is having difficulty in communicating with the physician. Her blood is sent for evaluation and a chest X-ray is ordered. Her arterial blood gas reports are as follows:
PaO2 50 mm Hg
pH 7.38
PaCO2 47 mm Hg
HCO3 27 mEq/L
Which of the following is the most appropriate next step in management?
- A. Intravenous corticosteroid (Correct Answer)
- B. Inhaled corticosteroid
- C. Mechanical ventilation
- D. Methacholine challenge test
- E. Inhaled β-agonist
Respiratory distress assessment and management Explanation: ***Intravenous corticosteroid***
- The patient exhibits severe asthma exacerbation with **poor response to inhaled β-agonists**, marked respiratory distress, and an alarming **PEFR of 50%**.
- **Intravenous corticosteroids** are crucial in this scenario to reduce airway inflammation and prevent progression to respiratory failure.
*Inhaled corticosteroid*
- While essential for **long-term asthma control**, inhaled corticosteroids are **not effective enough for acute, severe exacerbations** due to their slower onset of action.
- The patient's inability to effectively inhale deeply due to distress also limits the utility of inhaled delivery in this emergency.
*Mechanical ventilation*
- Mechanical ventilation is a **last-resort intervention** for impending respiratory failure, indicated by signs like declining consciousness, hypercapnia, or respiratory arrest.
- While concerning, the patient's current ABG with a **near-normal pH (7.38)** despite hypercapnia suggests she is not yet in full respiratory failure, and less invasive measures should be initiated first.
*Methacholine challenge test*
- The methacholine challenge test is used to **diagnose asthma in stable patients** with normal spirometry, by assessing airway hyperresponsiveness.
- It is **absolutely contraindicated** in an acute, severe asthma exacerbation as it could worsen bronchoconstriction and respiratory distress.
*Inhaled β-agonist*
- The patient has **already taken several puffs of her inhaler** (likely a β-agonist) without response, indicating **refractory bronchospasm**.
- While initially appropriate, repeated administration when ineffective suggests the need for other therapeutic interventions to address the underlying inflammation.
Respiratory distress assessment and management US Medical PG Question 2: A 16-month-old male patient, with no significant past medical history, is brought into the emergency department for the second time in 5 days with tachypnea, expiratory wheezes and hypoxia. The patient presented to the emergency department initially due to rhinorrhea, fever and cough. He was treated with nasal suctioning and discharged home. The mother states that, over the past 5 days, the patient has started breathing faster with chest retractions. His vital signs are significant for a temperature of 100.7 F, respiratory rate of 45 and oxygen saturation of 90%. What is the most appropriate treatment for this patient?
- A. Albuterol, ipratropium and IV methylprednisolone
- B. IV cefotaxime and IV vancomycin
- C. Intubation and IV cefuroxime
- D. Humidified oxygen, racemic epinephrine and intravenous (IV) dexamethasone
- E. Nasal suctioning, oxygen therapy and IV fluids (Correct Answer)
Respiratory distress assessment and management Explanation: ***Nasal suctioning, oxygen therapy and IV fluids***
- This patient's presentation with rhinorrhea, fever, cough, tachypnea, expiratory wheezes, and hypoxia, particularly a 16-month-old, strongly suggests **bronchiolitis**, likely caused by **RSV**.
- Management of bronchiolitis is primarily **supportive care**, including maintaining airway patency via nasal suctioning, providing oxygen for hypoxia, and ensuring adequate hydration with IV fluids.
*Albuterol, ipratropium and IV methylprednisolone*
- **Bronchodilators** like albuterol and ipratropium are generally **not recommended** for routine management of bronchiolitis due to lack of consistent efficacy in infants.
- **Corticosteroids** (e.g., methylprednisolone) are also **not routinely indicated** for bronchiolitis and have not been shown to improve outcomes.
*IV cefotaxime and IV vancomycin*
- These are **broad-spectrum antibiotics** used to treat **bacterial infections**, such as severe pneumonia or sepsis.
- The clinical presentation is more consistent with a **viral respiratory infection** (bronchiolitis), and there is no evidence of a bacterial co-infection or sepsis.
*Intubation and IV cefuroxime*
- **Intubation** is an invasive procedure reserved for patients with impending respiratory failure and is not indicated at this stage given the current oxygen saturation of 90% with supportive measures.
- **Cefuroxime** is an antibiotic, and like other antibiotics, is not indicated for a viral illness like bronchiolitis.
*Humidified oxygen, racemic epinephrine and intravenous (IV) dexamethasone*
- **Racemic epinephrine** may be considered for severe bronchiolitis with significant bronchospasm, but its use is not routine and its efficacy is debated.
- **IV dexamethasone** is a corticosteroid, which is not recommended for routine bronchiolitis management. Humidified oxygen is helpful, but the overall regimen is not standard for bronchiolitis.
Respiratory distress assessment and management US Medical PG Question 3: A 26-year-old G1P0 female who is 39 weeks pregnant presents to the emergency department in labor. She reports following her primary care physician’s recommendations throughout her pregnancy and has not had any complications. During delivery, the baby’s head turtled back into the vaginal canal and did not advance any further. The neonatal intensivist was called for shoulder dystocia and a baby girl was able to be delivered vaginally 6 minutes later. Upon initial assessment, the baby appeared pale throughout, had her arms and legs flexed without active motion, and had some flexion of extremities when stimulated. Her pulse is 120/min and had irregular respirations. What is this baby’s initial APGAR score?
- A. 5 (Correct Answer)
- B. 6
- C. 7
- D. 4
- E. 3
Respiratory distress assessment and management Explanation: ***5***
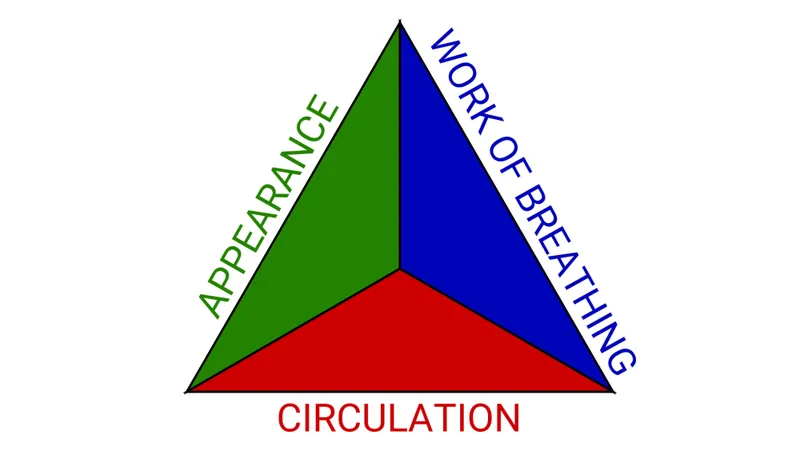
- The APGAR score is calculated based on five criteria: **Appearance**, **Pulse**, **Grimace**, **Activity**, and **Respiration**.
- This baby's score is calculated as follows: **Appearance** (pale all over) = 0, **Pulse** (120/min) = 2, **Grimace** (some flexion of extremities with stimulation) = 1, **Activity** (arms and legs flexed without active motion) = 1, and **Respiration** (irregular) = 1.
- Total score: 0 + 2 + 1 + 1 + 1 = **5 points**
- A score of 5 indicates **moderate neonatal compromise** requiring close monitoring and possible intervention.
*4*
- A score of 4 would indicate more severe compromise, such as absent respirations (0 points) rather than irregular respirations (1 point).
- This baby has irregular respirations present, which earns 1 point, not 0 points.
*6*
- A score of 6 would require improvement in at least one category, such as **acrocyanosis** (blue extremities but pink body = 1 point for appearance) instead of pallor throughout.
- This baby's complete pallor limits the score to 5.
*7*
- A score of 7 or higher is generally considered reassuring and indicates a **healthy transition** from intrauterine to extrauterine life.
- This baby's concerning signs, including **complete pallor**, **irregular respirations**, and **poor muscle tone**, are inconsistent with a score of 7.
*3*
- A score of 3 would indicate severe depression with findings such as **heart rate less than 100 bpm**, completely absent reflexes, or flaccid muscle tone.
- This baby has a reassuring pulse of 120/min (2 points), some reflex response (1 point), and some muscle tone (1 point), making the total score higher than 3.
Respiratory distress assessment and management US Medical PG Question 4: Thirty minutes after delivery, a 1780-g (3-lb 15-oz) male newborn develops respiratory distress. He was born at 30 weeks' gestation via vaginal delivery. His temperature is 36.8C (98.2F), pulse is 140/min, respirations are 64/min, and blood pressure is 61/32 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 90%. Examination shows pale extremities. Grunting and moderate subcostal retractions are present. Pulmonary examination shows decreased breath sounds bilaterally. Supplemental oxygen is administered. Ten minutes later, his pulse is 148/min and respirations are 66/min. Pulse oximetry on 60% oxygen shows an oxygen saturation of 90%. Which of the following is the most likely diagnosis?
- A. Meconium aspiration syndrome
- B. Tracheomalacia
- C. Tracheoesophageal fistula
- D. Neonatal pneumonia
- E. Respiratory distress syndrome (Correct Answer)
Respiratory distress assessment and management Explanation: ***Respiratory distress syndrome***
- This premature newborn (30 weeks' gestation, 1780-g) with immediate **respiratory distress**, grunting, retractions, and poor oxygenation despite supplemental oxygen is highly indicative of **respiratory distress syndrome (RDS)** due to surfactant deficiency.
- The **decreased breath sounds bilaterally** are consistent with widespread atelectasis characteristic of RDS.
*Meconium aspiration syndrome*
- This typically occurs in **term or post-term infants** and is unlikely in a 30-week premature infant.
- It usually presents with a history of **meconium-stained amniotic fluid** and chest X-ray findings of patchy infiltrates and hyperinflation.
*Tracheomalacia*
- This condition involves **weakness of the tracheal walls** leading to airway collapse, often presenting with a **barking cough** or **stridor**.
- It does not typically cause the severe, rapidly worsening respiratory distress and diffuse lung findings seen in this case.
*Tracheoesophageal fistula*
- This typically presents with **choking, coughing, and cyanosis during feeding**, due to aspiration of milk into the trachea.
- Respiratory distress in this condition is usually associated with feeding, and there is no mention of feeding issues in this scenario.
*Neonatal pneumonia*
- While possible in a premature infant, pneumonia symptoms often include **fever** and specific chest X-ray findings (e.g., infiltrates), which are not emphasized here.
- The rapid onset immediately after birth and progressive nature in a preterm infant strongly point towards a primary respiratory developmental issue like RDS.
Respiratory distress assessment and management US Medical PG Question 5: A 3-year-old girl is brought to the physician for a well-child examination. She was born at term and has been healthy since. She can climb up and down the stairs and can pedal a tricycle. She has difficulty using a spoon to feed herself but can copy a line. She speaks in 2- to 3-word sentences that can be understood by most people. She is selfish while playing with children her age and throws tantrums quite often. She cannot put on her own shoes and socks. She does not tolerate separation from her parents. She is at 60th percentile for height and weight. Physical examination including neurologic examination reveals no abnormalities. Which of the following is the most appropriate assessment of her development?
- A. Fine motor: Normal | Gross motor: Normal | Language: Delayed | Social skills: Delayed
- B. Fine motor: Delayed | Gross motor: Delayed | Language: Normal | Social skills: Normal
- C. Fine motor: Delayed | Gross motor: Normal | Language: Normal | Social skills: Delayed (Correct Answer)
- D. Fine motor: Normal | Gross motor: Delayed | Language: Normal | Social skills: Delayed
- E. Fine motor: Normal | Gross motor: Delayed | Language: Delayed | Social skills: Normal
Respiratory distress assessment and management Explanation: ***Fine motor: Delayed | Gross motor: Normal | Language: Normal | Social skills: Delayed***
- The child can copy a line (expected at 3 years) and climb stairs and pedal a tricycle (expected for a 3-year-old), indicating **normal gross motor skills**. However, difficulty using a spoon and putting on shoes/socks suggests **delayed fine motor skills**.
- Speaking in 2- to 3-word sentences understood by most (expected for 2-3 years) indicates **normal language development**. Being selfish and throwing tantrums (normal for 2-3 years) but not tolerating separation (suggests earlier developmental stage for separation anxiety) point to **delayed social skills**.
*Fine motor: Normal | Gross motor: Normal | Language: Delayed | Social skills: Delayed*
- This option incorrectly assesses fine motor skills as normal when the child struggles with tasks like using a spoon and dressing herself.
- While language and social skills are correctly identified as delayed, the overall assessment of fine motor makes this option incorrect.
*Fine motor: Delayed | Gross motor: Delayed | Language: Normal | Social skills: Normal*
- This option incorrectly assesses gross motor skills as delayed, despite the child's ability to climb stairs and pedal a tricycle, which are age-appropriate.
- It also incorrectly assesses social skills as normal, overlooking the persistent separation anxiety and aggressive social play for her age.
*Fine motor: Normal | Gross motor: Delayed | Language: Normal | Social skills: Delayed*
- This option incorrectly describes fine motor skills as normal and gross motor skills as delayed.
- Her ability to pedal a tricycle and climb stairs indicates age-appropriate gross motor development, while her difficulty with a spoon suggests delayed fine motor skills.
*Fine motor: Normal | Gross motor: Delayed | Language: Delayed | Social skills: Normal*
- This option incorrectly states that both fine motor and gross motor skills are affected and also mischaracterizes social skills as normal.
- The child's language development is within the normal range for a 3-year-old, and her social behavior, particularly the separation anxiety, indicates a delay.
Respiratory distress assessment and management US Medical PG Question 6: A 5-year-old is brought into the emergency department for trouble breathing. He was at a family picnic playing when his symptoms began. The patient is currently struggling to breathe and has red, warm extremities. The patient has an unknown medical history and his only medications include herbs that his parents give him. His temperature is 99.5°F (37.5°C), pulse is 112/min, blood pressure is 70/40 mmHg, respirations are 18/min, and oxygen saturation is 82% on 100% O2. Which of the following is the best initial step in management?
- A. Intubation
- B. Albuterol
- C. Cricothyroidotomy
- D. Albuterol, ipratropium, and magnesium
- E. Epinephrine (Correct Answer)
Respiratory distress assessment and management Explanation: ***Epinephrine***
- This patient is exhibiting signs of **anaphylactic shock** (difficulty breathing, red/warm extremities, hypotension) likely triggered by an allergen at the picnic. **Epinephrine** is the first-line treatment for anaphylaxis due to its alpha and beta-adrenergic effects that counteract vasodilation, bronchoconstriction, and histamine release.
- The rapid onset of symptoms and cardiovascular collapse (hypotension) necessitate immediate administration of epinephrine to stabilize the patient.
*Intubation*
- While the patient is in respiratory distress, intubation is a more invasive procedure and not the *initial* best step for anaphylactic shock. **Epinephrine** should be administered first to address the underlying physiological derangements.
- Airway management, including intubation, may be necessary if epinephrine fails to improve respiratory status, but it is secondary to addressing the systemic allergic reaction.
*Albuterol*
- **Albuterol** is a bronchodilator that helps with bronchospasm, but it does not address the widespread vasodilation, hypotension, or other systemic effects of anaphylaxis.
- While it might provide some symptomatic relief for breathing, it is insufficient as a standalone treatment for anaphylactic shock and would not prevent cardiovascular collapse.
*Cricothyroidotomy*
- **Cricothyroidotomy** is an emergency airway procedure used when conventional intubation is impossible due to upper airway obstruction.
- In this scenario, the primary issue is systemic anaphylaxis causing bronchospasm and shock, not an isolated upper airway obstruction, making epinephrine the more appropriate initial intervention.
*Albuterol, ipratropium, and magnesium*
- This combination is typically used for severe asthma exacerbations, focusing on bronchodilation and smooth muscle relaxation.
- Like albuterol alone, this combination does not address the underlying systemic vasodilation and hypotension characteristic of anaphylactic shock, which requires **epinephrine**.
Respiratory distress assessment and management US Medical PG Question 7: A mother brings her 6-month-old boy to the emergency department. She reports that her son has been breathing faster than usual for the past 2 days, and she has noted occasional wheezing. She states that prior to the difficulty breathing, she noticed some clear nasal discharge for several days. The infant was born full-term, with no complications, and no significant medical history. His temperature is 100°F (37.8°C), blood pressure is 60/30 mmHg, pulse is 120/min, respirations are 40/min, and oxygen saturation is 95% on room air. Physical exam reveals expiratory wheezing, crackles diffusely, and intercostal retractions. The child is currently playing with toys. Which of the following is the most appropriate next step in management?
- A. Monitoring (Correct Answer)
- B. Intubation
- C. Albuterol
- D. Chest radiograph
- E. Azithromycin and ceftriaxone
Respiratory distress assessment and management Explanation: ***Monitoring (Supportive Care)***
- This infant presents with classic **viral bronchiolitis** (tachypnea, wheezing, crackles, retractions following upper respiratory symptoms)
- The child is **clinically stable**: O2 saturation 95% on room air, alert and playing with toys
- **Current AAP guidelines** recommend **supportive care only** for bronchiolitis, which includes monitoring vital signs, assessing work of breathing, ensuring adequate hydration, and oxygen supplementation if saturation drops below 90%
- This patient requires close observation but no immediate intervention given stable vital signs and reassuring clinical appearance
*Albuterol*
- **Bronchodilators are NOT recommended** for routine use in bronchiolitis per current AAP clinical practice guidelines
- Multiple randomized controlled trials have shown **no significant benefit** from albuterol in bronchiolitis
- While a trial may be considered in select cases with strong family history of asthma, routine use is discouraged
- Bronchiolitis is caused by **small airway inflammation and mucus plugging**, not bronchospasm
*Intubation*
- **Intubation** is reserved for severe respiratory failure with impending respiratory arrest, persistent hypoxemia despite high-flow oxygen, apnea, or altered mental status
- This child has adequate oxygenation (95%), is alert, and playing—**no indication for intubation**
- Signs that would warrant intubation include lethargy, severe retractions with fatigue, O2 sat <90% despite supplementation
*Chest radiograph*
- **Not routinely indicated** in typical bronchiolitis
- Consider only if there's diagnostic uncertainty, concern for complications (pneumothorax, lobar consolidation suggesting bacterial pneumonia), or failure to improve with supportive care
- The clinical presentation is clearly consistent with bronchiolitis, and imaging would not change initial management
*Azithromycin and ceftriaxone*
- Bronchiolitis is a **viral infection** (most commonly RSV), and **antibiotics provide no benefit**
- Antibiotics should only be used if there is clear evidence of **bacterial superinfection** (high fever, focal consolidation, elevated inflammatory markers)
- Routine antibiotic use contributes to antimicrobial resistance and adverse effects
Respiratory distress assessment and management US Medical PG Question 8: A 3-year-old boy is brought to the emergency department by his mother because of a cough and mild shortness of breath for the past 12 hours. He has not had fever. He has been to the emergency department 4 times during the past 6 months for treatment of asthma exacerbations. His 9-month-old sister was treated for bronchiolitis a week ago. His father has allergic rhinitis. Current medications include an albuterol inhaler and a formoterol-fluticasone inhaler. He appears in mild distress. His temperature is 37.5°C (99.5°F), pulse is 101/min, respirations are 28/min, and blood pressure is 86/60 mm Hg. Examination shows mild intercostal and subcostal retractions. Pulmonary examination shows decreased breath sounds and mild expiratory wheezing throughout the right lung field. Cardiac examination shows no abnormalities. An x-ray of the chest shows hyperlucency of the right lung field with decreased pulmonary markings. Which of the following is the next best step in management?
- A. Azithromycin therapy
- B. Racemic epinephrine
- C. Albuterol nebulization
- D. CT of the lung
- E. Bronchoscopy (Correct Answer)
Respiratory distress assessment and management Explanation: ***Bronchoscopy***
- The patient's history of recurrent respiratory symptoms, unilateral wheezing and decreased breath sounds, and radiological findings of **unilateral hyperlucency** and **decreased pulmonary markings** strongly suggest a **foreign body aspiration**.
- **Bronchoscopy** is both diagnostic and therapeutic in this situation, allowing for direct visualization and removal of the foreign body.
*Azithromycin therapy*
- This is an **antibiotic** and would be used for bacterial infections, which are not indicated here given the clinical picture of a suspected foreign body.
- Antibiotics are not effective for mechanical obstruction of the airway.
*Racemic epinephrine*
- Racemic epinephrine is used for conditions like **croup** to reduce airway edema.
- It would not address an inhaled **foreign body**, which is a mechanical obstruction.
*Albuterol nebulization*
- While albuterol is used for bronchospasm, the unilateral nature of the findings and the history of recurrent issues point away from simple asthma exacerbation.
- Albuterol would likely not relieve the obstruction caused by a **foreign body**.
*CT of the lung*
- While CT could help identify a foreign body, it exposes the child to **radiation** and is not the definitive treatment.
- Bronchoscopy offers both diagnosis and immediate treatment, making it superior to CT as the *next best step*.
Respiratory distress assessment and management US Medical PG Question 9: Five weeks after delivery, a 1350-g (3-lb 0-oz) male newborn has respiratory distress. He was born at 26 weeks' gestation. He required intubation and mechanical ventilation for a month following delivery and has been on noninvasive pressure ventilation for 5 days. His temperature is 36.8°C (98.2°F), pulse is 148/min, respirations are 63/min, and blood pressure is 60/32 mm Hg. Pulse oximetry on 40% oxygen shows an oxygen saturation of 91%. Examination shows moderate intercostal and subcostal retractions. Scattered crackles are heard in the thorax. An x-ray of the chest shows diffuse granular densities and basal atelectasis. Which of the following is the most likely diagnosis?
- A. Bronchopulmonary dysplasia (Correct Answer)
- B. Tracheomalacia
- C. Bronchiolitis obliterans
- D. Interstitial emphysema
- E. Pneumonia
Respiratory distress assessment and management Explanation: ***Bronchopulmonary dysplasia***
- The presentation of a premature infant (26 weeks' gestation) with persistent respiratory distress requiring prolonged mechanical ventilation and oxygen, along with characteristic chest X-ray findings (diffuse granular densities and basal atelectasis), is highly indicative of **bronchopulmonary dysplasia (BPD)**.
- BPD is a chronic lung disease of prematurity defined by the need for supplemental oxygen and/or positive pressure ventilation for at least 28 days after birth, with severity classified at 36 weeks postmenstrual age (or discharge if earlier).
- The pathophysiology involves ventilator-induced injury, oxygen toxicity, and inflammation in the developing lung, leading to impaired alveolarization and abnormal vascular development.
*Tracheomalacia*
- While **tracheomalacia** can cause respiratory symptoms, it typically presents with expiratory stridor, a characteristic "barking" cough, or wheezing that may improve with neck extension or prone positioning.
- It is a structural abnormality of the trachea involving weakness of the tracheal wall, and would not typically manifest with diffuse granular densities or basal atelectasis on chest X-ray in this context.
*Bronchiolitis obliterans*
- **Bronchiolitis obliterans** is irreversible obstruction of the small airways, often occurring after severe viral infections (especially adenovirus or RSV), lung transplantation, or toxic inhalational injury.
- While it can occur in neonates post-ventilation, it is less common in this specific context and would typically present with more severe obstructive findings, hyperinflation, and air trapping on imaging rather than chronic diffuse granular densities and atelectasis.
*Interstitial emphysema*
- **Pulmonary interstitial emphysema** usually occurs acutely in the first days to weeks of mechanical ventilation, characterized by air dissecting into the lung interstitium and perivascular spaces.
- While it can be a complication that contributes to the development of BPD, the persistent nature of respiratory distress five weeks post-delivery, along with diffuse granular densities and chronic radiographic changes, points toward the established chronic lung disease of BPD rather than acute interstitial emphysema.
*Pneumonia*
- Neonatal **pneumonia** would typically present with acute onset or worsening of respiratory distress, temperature instability, and signs of systemic infection.
- While a chest X-ray might show infiltrates or consolidations, the chronic progressive course over 5 weeks, history of extreme prematurity, and prolonged ventilation make BPD a more fitting diagnosis than acute pneumonia in this clinical scenario.
Respiratory distress assessment and management US Medical PG Question 10: A 4-year-old girl is brought to the emergency department by her parents with a sudden onset of breathlessness. She has been having similar episodes over the past few months with a progressive increase in frequency over the past week. They have noticed that the difficulty in breathing is more prominent during the day when she plays in the garden with her siblings. She gets better once she comes indoors. During the episodes, she complains of an inability to breathe and her parents say that she is gasping for breath. Sometimes they hear a noisy wheeze while she breathes. The breathlessness does not disrupt her sleep. On examination, she seems to be in distress with noticeable intercostal retractions. Auscultation reveals a slight expiratory wheeze. According to her history and physical findings, which of the following mechanisms is most likely responsible for this child’s difficulty in breathing?
- A. Defective chloride channel function leading to mucus plugging
- B. Chronic mucus plugging and inflammation leading to impaired mucociliary clearance
- C. Airway hyperreactivity to external allergens causing intermittent airway obstruction (Correct Answer)
- D. Inflammation leading to permanent dilation and destruction of alveoli
- E. Destruction of the elastic layers of bronchial walls leading to abnormal dilation
Respiratory distress assessment and management Explanation: **Airway hyperreactivity to external allergens causing intermittent airway obstruction**
- The child's symptoms of **recurrent breathlessness** and **wheezing**, especially while playing in the garden (suggesting **allergen exposure**), and subsequent improvement indoors, are highly indicative of **allergen-induced bronchoconstriction**.
- The history points to **intermittent airway obstruction** triggered by environmental factors, characteristic of conditions like **asthma** where airways are hyperresponsive to triggers.
*Defective chloride channel function leading to mucus plugging*
- This mechanism is characteristic of **cystic fibrosis**, which typically presents with chronic respiratory issues, recurrent infections, and growth failure, not the acute, intermittent, and allergen-triggered episodes described.
- While mucus plugging can occur, it's a chronic process in cystic fibrosis and doesn't align with the acute, reversible nature and specific triggers mentioned in the case.
*Chronic mucus plugging and inflammation leading to impaired mucociliary clearance*
- This describes conditions like **bronchiectasis** or chronic bronchitis, which involve persistent cough, sputum production, and recurrent infections, rather than acute episodic wheezing based on allergen exposure.
- Impaired mucociliary clearance would lead to more continuous respiratory issues, not the relief experienced upon coming indoors.
*Inflammation leading to permanent dilation and destruction of alveoli*
- This mechanism is characteristic of **emphysema**, a condition primarily seen in adults, typically due to smoking, and presenting with chronic shortness of breath and airflow limitation, rather than episodic, allergen-triggered wheezing in a child.
- Emphysema involves alveolar damage, not primarily bronchial obstruction or hyperreactivity.
*Destruction of the elastic layers of bronchial walls leading to abnormal dilation*
- This describes **bronchiectasis**, which is characterized by permanent dilation of the bronchi, leading to chronic cough with sputum production and recurrent respiratory infections.
- The symptoms presented by the child are acute, reversible episodes of breathlessness and wheezing, not indicative of permanent structural damage to the bronchial walls.
More Respiratory distress assessment and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.