Pediatric basic life support US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pediatric basic life support. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pediatric basic life support US Medical PG Question 1: A newborn male is evaluated one minute after birth. He was born at 38 weeks gestation to a 28-year-old gravida 3 via vaginal delivery. The patient’s mother received sporadic prenatal care, and the pregnancy was complicated by gestational diabetes. The amniotic fluid was clear. The patient’s pulse is 70/min, and his breathing is irregular with a slow, weak cry. He whimpers in response to a soft pinch on the thigh, and he has moderate muscle tone with some flexion of his extremities. His body is pink and his extremities are blue. The patient is dried with a warm towel and then placed on his back on a flat warmer bed. His mouth and nose are suctioned with a bulb syringe.
Which of the following is the best next step in management?
- A. Supplemental oxygen via nasal cannula and reassessment of Apgar score at 5 minutes
- B. Chest compressions and bag-mask ventilation
- C. Endotracheal intubation and mechanical ventilation
- D. Intravenous epinephrine and reassessment of Apgar score at 5 minutes
- E. Positive pressure ventilation and reassessment of Apgar score at 5 minutes (Correct Answer)
Pediatric basic life support Explanation: ***Positive pressure ventilation and reassessment of Apgar score at 5 minutes***
- The newborn's **heart rate is 70/min**, which is below the target of >100/min that warrants **positive pressure ventilation (PPV)**. His irregular breathing and central cyanosis (pink body, blue extremities indicate acrocyanosis, but the overall picture suggests a need for support), along with the low heart rate, indicate inadequate respiratory effort and circulation.
- After initial steps (drying, stimulating, suctioning), if the heart rate remains below 100/min or the infant has gasping/apnea, PPV should be initiated immediately. Reassessing the **Apgar score at 5 minutes** is standard practice.
*Supplemental oxygen via nasal cannula and reassessment of Apgar score at 5 minutes*
- While supplemental oxygen is important, **nasal cannula** provides low-flow oxygen and is insufficient for a newborn with a heart rate of 70/min and irregular breathing. This patient requires more robust respiratory support.
- Oxygen supplementation alone would not address the inadequate respiratory effort and bradycardia to the necessary extent.
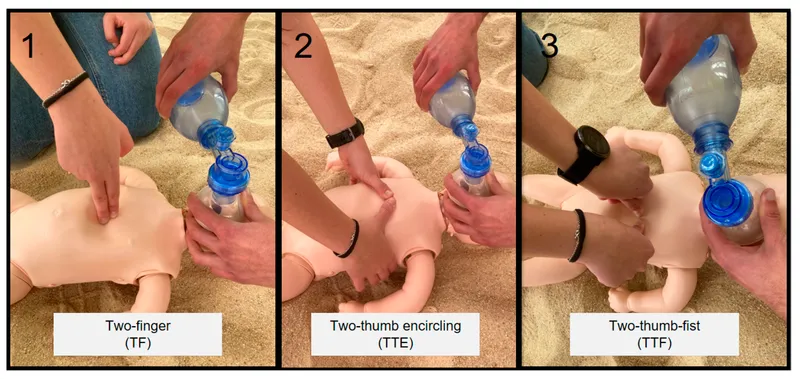
*Chest compressions and bag-mask ventilation*
- **Chest compressions** are indicated when the heart rate is below 60/min despite adequate positive pressure ventilation for at least 30 seconds.
- In this case, the heart rate is 70/min, so chest compressions are not yet indicated. The priority is to establish effective ventilation.
*Endotracheal intubation and mechanical ventilation*
- **Endotracheal intubation** is considered if PPV via bag-mask is ineffective, if prolonged resuscitation is anticipated, or if meconium aspiration is present.
- This is a more invasive step and not the immediate next step when PPV can be initiated first to improve heart rate and respiration.
*Intravenous epinephrine and reassessment of Apgar score at 5 minutes*
- **Intravenous epinephrine** is administered only if the heart rate remains below 60/min despite 30 seconds of effective positive pressure ventilation and 60 seconds of effective chest compressions.
- The current heart rate is 70/min, and the prior steps of resuscitation have not yet included effective PPV for the required duration, so epinephrine is not yet indicated.
Pediatric basic life support US Medical PG Question 2: A 1-month-old infant is brought to the physician for a well-child examination. His mother reports that she had previously breastfed her son every 2 hours for 15 minutes but is now feeding him every 4 hours for 40 minutes. She says that the infant sweats a lot and is uncomfortable during feeds. He has 6 wet diapers and 2 stools daily. He was born at 36 weeks' gestation. He currently weighs 3500 g (7.7 lb) and is 52 cm (20.4 in) in length. He is awake and alert. His temperature is 37.1°C (98.8°F), pulse is 170/min, respirations are 55/min, and blood pressure is 80/60 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. Cardiopulmonary examination shows a 4/6 continuous murmur along the upper left sternal border. After confirming the diagnosis via echocardiography, which of the following is the most appropriate next step in the management of this patient?
- A. Digoxin and furosemide (Correct Answer)
- B. Percutaneous surgery
- C. X-ray of the chest
- D. Prostaglandin E1 infusion
- E. Indomethacin infusion
Pediatric basic life support Explanation: ***Digoxin and furosemide***
- This 1-month-old infant presents with classic signs of **heart failure** from a symptomatic **patent ductus arteriosus (PDA)**: tachycardia (170/min), tachypnea (55/min), poor feeding with prolonged feeding times, diaphoresis during feeds, and a continuous murmur at the left upper sternal border.
- At **1 month of age**, the initial management focuses on **medical treatment of heart failure** with **furosemide** (loop diuretic to reduce volume overload) and **digoxin** (inotropic support to improve cardiac contractility).
- This stabilizes the infant before definitive closure is considered if medical management fails.
*Indomethacin infusion*
- **Indomethacin** (NSAID/prostaglandin inhibitor) is effective for **PDA closure only in premature infants within the first 7-14 days of life**.
- At **1 month of age** (approximately 40 weeks corrected gestational age), the ductus arteriosus is no longer responsive to prostaglandin inhibition, making indomethacin ineffective.
- This would have been appropriate if the infant was still in the early neonatal period.
*Percutaneous surgery*
- **Percutaneous transcatheter closure** or surgical ligation may be required if medical management of heart failure fails or the PDA remains hemodynamically significant.
- However, this is **not the initial step**—medical stabilization with heart failure management should be attempted first.
- Procedural closure is typically considered after 6 months of age if spontaneous closure has not occurred.
*X-ray of the chest*
- A chest X-ray would show **cardiomegaly** and **increased pulmonary vascular markings** consistent with the left-to-right shunt from PDA.
- However, the diagnosis has already been **confirmed by echocardiography**, and imaging does not constitute therapeutic management for this symptomatic infant.
*Prostaglandin E1 infusion*
- **Prostaglandin E1** is used to **maintain** ductal patency in **ductal-dependent congenital heart lesions** (e.g., critical coarctation, hypoplastic left heart syndrome, pulmonary atresia).
- In this case with symptomatic PDA, the goal is to manage heart failure and potentially achieve ductal closure, making PGE1 **contraindicated**.
Pediatric basic life support US Medical PG Question 3: A first time mother of a healthy, full term, newborn girl is anxious about sudden infant death syndrome. Which of the following pieces of advice can reduce the risk of SIDS?
- A. Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in a warm blanket
- B. Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in an infant sleeper
- C. Sleep supine in the parent's bed and use a pacifier after 1 month of age
- D. Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and use a home apnea monitor
- E. Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and avoid smoking (Correct Answer)
Pediatric basic life support Explanation: ***Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and avoiding smoking***
- **Sleeping supine** (on the back) is the most critical recommendation to reduce SIDS risk, and a **crib without bumpers** and other soft bedding reduces smothering hazards.
- **Pacifier use** after the first month of age has been shown to be protective, and **avoiding smoking** around the infant is crucial as exposure to tobacco smoke significantly increases SIDS risk.
*Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in a warm blanket*
- While **sleeping supine** is correct, **bumpers, pillows, and loose blankets** in the crib are significant risk factors for SIDS, as they can cause accidental suffocation.
- The use of **pillows** is not recommended for infants due to the risk of airway obstruction and suffocation.
*Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in an infant sleeper*
- Similar to the previous option, **bumpers and a pillow** are unsafe as they pose a suffocation risk and should be avoided in an infant's sleep environment.
- While an **infant sleeper** (or sleep sack) is generally safer than a loose blanket, the presence of bumpers and a pillow negates this benefit.
*Sleep supine in the parent's bed and use a pacifier after 1 month of age*
- **Co-sleeping (sharing a bed with parents)** significantly increases the risk of SIDS and accidental suffocation, especially if parents smoke, are impaired, or if heavy bedding is present.
- Although **pacifier use** is recommended, sleeping in the parent's bed is a major risk factor that outweighs any potential benefit here.
*Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and use a home apnea monitor*
- While **sleeping supine** in a **crib without bumpers** and **pacifier use** are correct recommendations, **home apnea monitors** are not recommended for routine SIDS prevention in healthy infants.
- Apnea monitors have not been shown to reduce the incidence of SIDS and can lead to false alarms and unnecessary anxiety without proven benefit.
Pediatric basic life support US Medical PG Question 4: A 57-year-old man is admitted to the burn unit after he was brought to the emergency room following an accidental fire in his house. His past medical history is unknown due to his current clinical condition. Currently, his blood pressure is 75/40 mmHg, pulse rate is 140/min, and respiratory rate is 17/min. The patient is subsequently intubated and started on aggressive fluid resuscitation. A Swan-Ganz catheter is inserted to clarify his volume status. Which of the following hemodynamic parameters would you expect to see in this patient?
- A. Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
- B. Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔
- C. Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔
- D. Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓ (Correct Answer)
- E. Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
Pediatric basic life support Explanation: ***Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓***
- The patient's **hypotension (75/40 mmHg)** and **tachycardia (140/min)**, combined with severe burns, indicate **hypovolemic shock** due to massive fluid loss from damaged capillaries.
- In response to decreased cardiac output and hypovolemia, the body compensates by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, and **pulmonary artery wedge pressure (PAWP)** will be low due to reduced intravascular volume.
*Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This option incorrectly suggests that systemic vascular resistance and pulmonary artery wedge pressure would be normal, which is inconsistent with **hypovolemic shock**.
- In shock, the body's compensatory mechanisms would lead to significant changes in SVR and PAWP, not maintain them at baseline.
*Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔*
- Increased cardiac output is usually seen in **distributive shock** (e.g., septic shock) where vasodilation leads to reduced SVR, not increased SVR as suggested here.
- An elevated SVR coupled with an increased cardiac output would typically result in a higher blood pressure unless there is a compensatory drop in other parameters.
*Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔*
- This pattern (high cardiac output, low SVR) is characteristic of **distributive shock**, such as **septic shock** or anaphylactic shock, rather than the hypovolemic shock expected in a burn patient.
- Severe burns primarily cause massive fluid shifts, leading to hypovolemia and a reduced cardiac output, not an elevated one.
*Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This scenario represents **normal hemodynamic parameters**, which would not be expected in a patient experiencing severe shock from extensive burns.
- The patient's clinical presentation (hypotension, tachycardia) clearly indicates a state of hemodynamic instability.
Pediatric basic life support US Medical PG Question 5: A 6-month-old male presents to the emergency department with his parents after his three-year-old brother hit him on the arm with a toy truck. His parents are concerned that the minor trauma caused an unusual amount of bruising. The patient has otherwise been developing well and meeting all his milestones. His parents report that he sleeps throughout the night and has just started to experiment with solid food. The patient’s older brother is in good health, but the patient’s mother reports that some members of her family have an unknown blood disorder. On physical exam, the patient is agitated and difficult to soothe. He has 2-3 inches of ecchymoses and swelling on the lateral aspect of the left forearm. The patient has a neurological exam within normal limits and pale skin with blue irises. An ophthalmologic evaluation is deferred.
Which of the following is the best initial step?
- A. Genetic testing
- B. Complete blood count and coagulation panel (Correct Answer)
- C. Ensure the child's safety and alert the police
- D. Peripheral blood smear
- E. Hemoglobin electrophoresis
Pediatric basic life support Explanation: ***Complete blood count and coagulation panel***
- The unusual amount of **bruising** after minor trauma, along with a family history of an unknown blood disorder, strongly suggests a potential **bleeding disorder**. A **CBC** and a **coagulation panel** (PT, aPTT, fibrinogen) are essential initial steps to evaluate for abnormalities in platelets, clotting factors, or other hematologic conditions.
- These tests can help narrow down the differential diagnosis between **platelet dysfunction**, **coagulopathies** (like hemophilia or von Willebrand disease), or other less common bleeding disorders, guiding further specific investigations.
- **Important consideration:** The presence of **blue sclera** (described as "blue irises") raises concern for **osteogenesis imperfecta (OI)**, a connective tissue disorder causing bone fragility. However, initial hematologic screening is still appropriate given the family history of blood disorder and presentation of excessive bruising. If coagulation studies are normal, imaging and further workup for OI would be indicated.
*Genetic testing*
- While a genetic component is plausible given the patient's family history and clinical presentation (blue sclera may suggest osteogenesis imperfecta), **genetic testing** is typically performed *after* initial laboratory workup has identified a specific type of bleeding or inherited disorder.
- Starting with genetic testing without basic hematologic parameters is not the most efficient or cost-effective initial diagnostic approach.
*Ensure the child's safety and alert the police*
- While child abuse should always be considered in cases of unexplained or excessive bruising, the presence of a **family history of a blood disorder** and the **blue sclera** (suggesting possible osteogenesis imperfecta) make **medical causes** more immediate concerns for initial investigation.
- Pursuing a medical workup first often clarifies whether abuse is the primary explanation, although child protective services should be notified if suspicion remains high after medical evaluation.
*Peripheral blood smear*
- A **peripheral blood smear** provides information on red blood cell morphology, platelet size and number, and white blood cell differential. While useful in assessing for some hematologic conditions, it is often performed *after* a CBC has indicated abnormalities or in conjunction with specialized testing.
- It would not be the *best initial step* as it doesn't directly assess clotting factor function, which is critical in evaluating significant bruising severity.
*Hemoglobin electrophoresis*
- **Hemoglobin electrophoresis** is used to diagnose **hemoglobinopathies** like sickle cell anemia or thalassemia.
- The patient's symptoms (easy bruising) are not characteristic of hemoglobinopathies, and while he has pale skin, this test would not be the initial step to investigate a bleeding disorder.
Pediatric basic life support US Medical PG Question 6: A 3-year-old girl with no significant past medical history presents to the clinic with a 4-day history of acute onset cough. Her parents have recently started to introduce several new foods into her diet. Her vital signs are all within normal limits. Physical exam is significant for decreased breath sounds on the right. What is the most appropriate definitive management in this patient?
- A. Inhaled bronchodilators and oral corticosteroids
- B. Rigid bronchoscopy (Correct Answer)
- C. Chest x-ray (CXR)
- D. Empiric antibiotic therapy
- E. Flexible bronchoscopy
Pediatric basic life support Explanation: ***Rigid bronchoscopy***
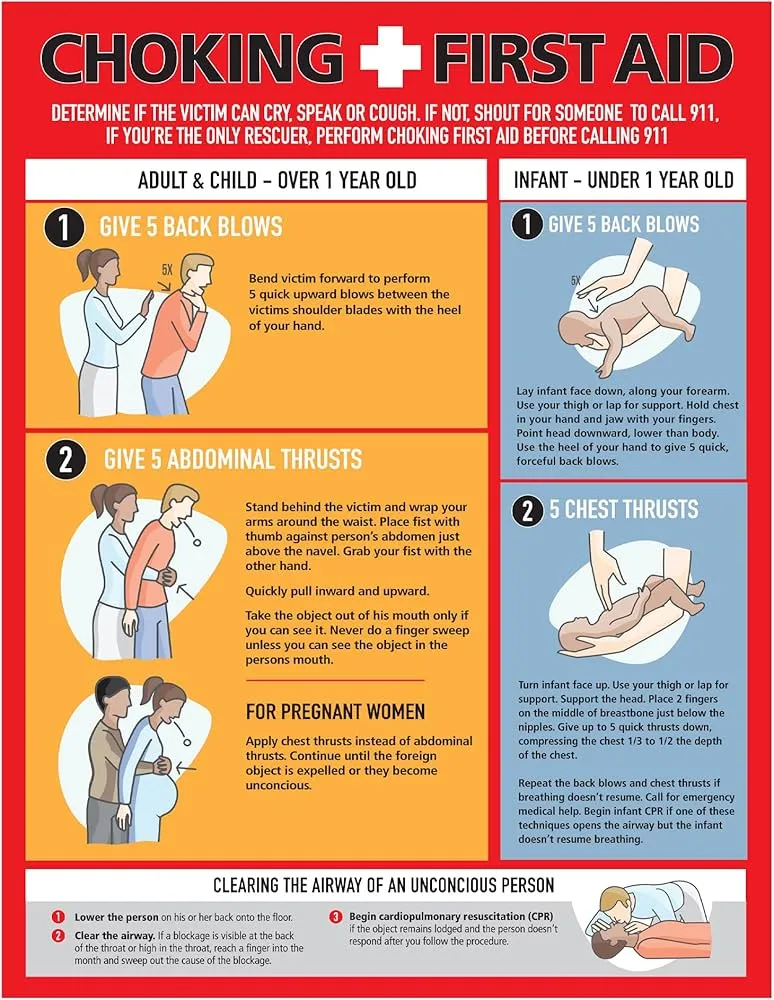
- The sudden onset of cough in a 3-year-old following new food introductions, coupled with decreased breath sounds on the right, strongly suggests a **foreign body aspiration**.
- **Rigid bronchoscopy** is the definitive and preferred method for both diagnosing and removing airway foreign bodies, especially in children, due to its ability to provide better airway control and allow the use of larger instruments.
*Inhaled bronchodilators and oral corticosteroids*
- These therapies are indicated for conditions like **asthma** or **bronchiolitis**, which typically present with wheezing and diffuse airway obstruction, not localized decreased breath sounds.
- They would not resolve a mechanical obstruction caused by a **foreign body**.
*Chest x-ray (CXR)*
- A CXR is often the **initial imaging study** in suspected foreign body aspiration, but it is not definitive management.
- Many foreign bodies are **radiolucent** and may not be visible, and even if visible, the CXR does not remove the object.
*Empiric antibiotic therapy*
- This therapy would be considered for a presumed **bacterial infection** (e.g., pneumonia), which usually presents with fever, productive cough, and specific CXR findings, none of which are primarily indicated here.
- It would not address a **mechanical airway obstruction**.
*Flexible bronchoscopy*
- While flexible bronchoscopy can be used for foreign body removal in some cases, **rigid bronchoscopy** is generally preferred in children for its superior airway control, better visualization, and ability to remove larger or more firmly lodged objects with specialized tools.
- Flexible scopes are more often used for **diagnostic purposes** or in adults for less emergent situations.
Pediatric basic life support US Medical PG Question 7: A mother brings her 6-month-old boy to the emergency department. She reports that her son has been breathing faster than usual for the past 2 days, and she has noted occasional wheezing. She states that prior to the difficulty breathing, she noticed some clear nasal discharge for several days. The infant was born full-term, with no complications, and no significant medical history. His temperature is 100°F (37.8°C), blood pressure is 60/30 mmHg, pulse is 120/min, respirations are 40/min, and oxygen saturation is 95% on room air. Physical exam reveals expiratory wheezing, crackles diffusely, and intercostal retractions. The child is currently playing with toys. Which of the following is the most appropriate next step in management?
- A. Monitoring (Correct Answer)
- B. Intubation
- C. Albuterol
- D. Chest radiograph
- E. Azithromycin and ceftriaxone
Pediatric basic life support Explanation: ***Monitoring (Supportive Care)***
- This infant presents with classic **viral bronchiolitis** (tachypnea, wheezing, crackles, retractions following upper respiratory symptoms)
- The child is **clinically stable**: O2 saturation 95% on room air, alert and playing with toys
- **Current AAP guidelines** recommend **supportive care only** for bronchiolitis, which includes monitoring vital signs, assessing work of breathing, ensuring adequate hydration, and oxygen supplementation if saturation drops below 90%
- This patient requires close observation but no immediate intervention given stable vital signs and reassuring clinical appearance
*Albuterol*
- **Bronchodilators are NOT recommended** for routine use in bronchiolitis per current AAP clinical practice guidelines
- Multiple randomized controlled trials have shown **no significant benefit** from albuterol in bronchiolitis
- While a trial may be considered in select cases with strong family history of asthma, routine use is discouraged
- Bronchiolitis is caused by **small airway inflammation and mucus plugging**, not bronchospasm
*Intubation*
- **Intubation** is reserved for severe respiratory failure with impending respiratory arrest, persistent hypoxemia despite high-flow oxygen, apnea, or altered mental status
- This child has adequate oxygenation (95%), is alert, and playing—**no indication for intubation**
- Signs that would warrant intubation include lethargy, severe retractions with fatigue, O2 sat <90% despite supplementation
*Chest radiograph*
- **Not routinely indicated** in typical bronchiolitis
- Consider only if there's diagnostic uncertainty, concern for complications (pneumothorax, lobar consolidation suggesting bacterial pneumonia), or failure to improve with supportive care
- The clinical presentation is clearly consistent with bronchiolitis, and imaging would not change initial management
*Azithromycin and ceftriaxone*
- Bronchiolitis is a **viral infection** (most commonly RSV), and **antibiotics provide no benefit**
- Antibiotics should only be used if there is clear evidence of **bacterial superinfection** (high fever, focal consolidation, elevated inflammatory markers)
- Routine antibiotic use contributes to antimicrobial resistance and adverse effects
Pediatric basic life support US Medical PG Question 8: A 2-year-old girl is brought to the emergency department after swallowing a button battery that was lying on the table 1 hour ago. She has no shortness of breath or chest discomfort. Her pulse is 112/min and respirations are 30/min. Pulse oximetry on room air shows an oxygen saturation of 98%. Physical examination shows no abnormalities. An x-ray of the chest shows the battery lodged in the esophagus at the level of T2. Which of the following is the most appropriate next step in management?
- A. Removal of the battery with magnet and nasogastric tube
- B. Administer syrup of ipecac
- C. Administer chelation therapy
- D. Endoscopic removal of the battery (Correct Answer)
- E. Reassurance and observation
Pediatric basic life support Explanation: ***Endoscopic removal of the battery***
- A button battery lodged in the esophagus is a **medical emergency** requiring prompt removal due to the risk of **corrosive injury, perforation, and fistula formation**.
- **Endoscopic removal** allows direct visualization and controlled extraction, minimizing further damage.
*Removal of the battery with magnet and nasogastric tube*
- While magnets can be used for foreign body removal in some cases, a **nasogastric tube is not an appropriate tool for safely extracting a button battery from the esophagus**.
- This method poses a risk of further trauma to the esophageal wall or dislodging the battery into the airway.
*Administer syrup of ipecac*
- **Syrup of ipecac induces emesis**, which is contraindicated here as it could lead to further esophageal damage, aspiration, or lodging the battery elsewhere in the GI tract.
- Its use for ingested foreign bodies is generally **discouraged**.
*Administer chelation therapy*
- **Chelation therapy is used for heavy metal poisoning**, such as lead or mercury, not for the direct removal of an ingested foreign body like a battery.
- The primary concern with button batteries is **local corrosive injury**, not systemic toxicity from metal absorption (unless it perforates).
*Reassurance and observation*
- This approach is dangerously inappropriate for an esophageal button battery, as **damage can occur within hours**, leading to strictures, perforation, and even death.
- Immediate intervention is crucial, even if the patient appears asymptomatic initially.
Pediatric basic life support US Medical PG Question 9: A previously healthy 5-year-old boy is brought to the emergency department because of a 1-day history of high fever. His temperature prior to arrival was 40.0°C (104°F). There is no family history of serious illness. Development has been appropriate for his age. He is administered rectal acetaminophen. While in the waiting room, he becomes unresponsive and starts jerking his arms and legs back and forth. A fingerstick blood glucose concentration is 86 mg/dL. After 5 minutes, he continues having jerky movements and is unresponsive to verbal and painful stimuli. Which of the following is the most appropriate next step in management?
- A. Intravenous administration of lorazepam (Correct Answer)
- B. Intravenous administration of phenobarbital
- C. Obtain blood cultures
- D. Intravenous administration of valproate
- E. Intravenous administration of fosphenytoin
Pediatric basic life support Explanation: ***Intravenous administration of lorazepam***
- The child is experiencing a **prolonged seizure** (greater than 5 minutes) following a high fever, which is concerning for **status epilepticus** secondary to a febrile seizure.
- **Lorazepam** is a first-line benzodiazepine for status epilepticus due to its rapid onset of action and prolonged anticonvulsant effect.
*Intravenous administration of phenobarbital*
- **Phenobarbital** is a long-acting anticonvulsant often used for **refractory status epilepticus** or as a long-term maintenance therapy.
- It is not the preferred initial treatment for an acute, prolonged seizure due to its slower onset compared to benzodiazepines.
*Obtain blood cultures*
- While obtaining blood cultures is important for identifying potential sources of infection causing the fever, it is **not the immediate priority** when a child is actively seizing and unresponsive.
- **Seizure termination** takes precedence to prevent potential neurological injury.
*Intravenous administration of valproate*
- **Valproate** is an anticonvulsant that can be used for various seizure types, but it is typically reserved for **refractory status epilepticus** or as a long-term maintenance drug.
- It does not have the rapid onset of action required for initial management of an acute, prolonged seizure.
*Intravenous administration of fosphenytoin*
- **Fosphenytoin** is an antiepileptic drug often used for **refractory status epilepticus** after benzodiazepines have failed.
- It is not the first-line medication for the initial management of an acute seizure of this duration.
Pediatric basic life support US Medical PG Question 10: A 5-year-old boy is brought to the emergency department by his grandmother because of difficulty breathing. Over the past two hours, the grandmother has noticed his voice getting progressively hoarser and occasionally muffled, with persistent drooling. He has not had a cough. The child recently immigrated from Africa, and the grandmother is unsure if his immunizations are up-to-date. He appears uncomfortable and is sitting up and leaning forward with his chin hyperextended. His temperature is 39.5°C (103.1°F), pulse is 110/min, and blood pressure is 90/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 95%. Pulmonary examination shows inspiratory stridor and scattered rhonchi throughout both lung fields, along with poor air movement. Which of the following is the most appropriate next step in management?
- A. Nebulized albuterol
- B. Direct laryngoscopy and pharyngoscopy
- C. Immediate nasotracheal intubation in the emergency department
- D. Prepare for emergency airway management in the operating room with anesthesia and ENT backup (Correct Answer)
- E. Intravenous administration of antibiotics
Pediatric basic life support Explanation: ***Prepare for emergency airway management in the operating room with anesthesia and ENT backup***
- The constellation of **hoarseness**, **muffled voice**, **drooling**, **inspiratory stridor**, **fever**, and the classic **tripod position** (sitting up, leaning forward, hyperextended chin) in an unimmunized child strongly indicates **epiglottitis**.
- Given the risk of **complete airway obstruction**, securing the airway in a controlled environment like the **operating room** with specialized personnel (**anesthesia**, **ENT**) is the safest and most appropriate immediate step.
*Nebulized albuterol*
- This medication is a **bronchodilator** primarily used for conditions like **asthma** or **bronchiolitis** that involve bronchospasm.
- It would not alleviate airway obstruction caused by supraglottic swelling in epiglottitis and could potentially worsen the child's distress.
*Direct laryngoscopy and pharyngoscopy*
- Performing a direct laryngoscopy or pharyngoscopy in the emergency department, especially without immediate intubation capabilities, could precipitate **laryngospasm** and **complete airway obstruction** in a child with suspected epiglottitis.
- Visualization of the airway should only be attempted in a controlled setting where immediate intubation or tracheostomy can be performed.
*Immediate nasotracheal intubation in the emergency department*
- While intubation is necessary, attempting it immediately in the emergency department without the controlled environment of an operating room and without the full support of anesthesia and ENT specialists carries significant risks.
- The swelling can make intubation extremely difficult and increase the likelihood of failed attempts or trauma, further compromising the airway.
*Intravenous administration of antibiotics*
- Although antibiotics are a crucial part of epiglottitis treatment (typically **ceftriaxone** or **cefotaxime** to cover *Haemophilus influenzae* type b), they are not the immediate priority.
- The most urgent threat is airway compromise; therefore, securing the airway takes precedence over initiating antibiotic therapy.
More Pediatric basic life support US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.