Pediatric advanced life support US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pediatric advanced life support. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pediatric advanced life support US Medical PG Question 1: A newborn male is evaluated one minute after birth. He was born at 38 weeks gestation to a 28-year-old gravida 3 via vaginal delivery. The patient’s mother received sporadic prenatal care, and the pregnancy was complicated by gestational diabetes. The amniotic fluid was clear. The patient’s pulse is 70/min, and his breathing is irregular with a slow, weak cry. He whimpers in response to a soft pinch on the thigh, and he has moderate muscle tone with some flexion of his extremities. His body is pink and his extremities are blue. The patient is dried with a warm towel and then placed on his back on a flat warmer bed. His mouth and nose are suctioned with a bulb syringe.
Which of the following is the best next step in management?
- A. Supplemental oxygen via nasal cannula and reassessment of Apgar score at 5 minutes
- B. Chest compressions and bag-mask ventilation
- C. Endotracheal intubation and mechanical ventilation
- D. Intravenous epinephrine and reassessment of Apgar score at 5 minutes
- E. Positive pressure ventilation and reassessment of Apgar score at 5 minutes (Correct Answer)
Pediatric advanced life support Explanation: ***Positive pressure ventilation and reassessment of Apgar score at 5 minutes***
- The newborn's **heart rate is 70/min**, which is below the target of >100/min that warrants **positive pressure ventilation (PPV)**. His irregular breathing and central cyanosis (pink body, blue extremities indicate acrocyanosis, but the overall picture suggests a need for support), along with the low heart rate, indicate inadequate respiratory effort and circulation.
- After initial steps (drying, stimulating, suctioning), if the heart rate remains below 100/min or the infant has gasping/apnea, PPV should be initiated immediately. Reassessing the **Apgar score at 5 minutes** is standard practice.
*Supplemental oxygen via nasal cannula and reassessment of Apgar score at 5 minutes*
- While supplemental oxygen is important, **nasal cannula** provides low-flow oxygen and is insufficient for a newborn with a heart rate of 70/min and irregular breathing. This patient requires more robust respiratory support.
- Oxygen supplementation alone would not address the inadequate respiratory effort and bradycardia to the necessary extent.
*Chest compressions and bag-mask ventilation*
- **Chest compressions** are indicated when the heart rate is below 60/min despite adequate positive pressure ventilation for at least 30 seconds.
- In this case, the heart rate is 70/min, so chest compressions are not yet indicated. The priority is to establish effective ventilation.
*Endotracheal intubation and mechanical ventilation*
- **Endotracheal intubation** is considered if PPV via bag-mask is ineffective, if prolonged resuscitation is anticipated, or if meconium aspiration is present.
- This is a more invasive step and not the immediate next step when PPV can be initiated first to improve heart rate and respiration.
*Intravenous epinephrine and reassessment of Apgar score at 5 minutes*
- **Intravenous epinephrine** is administered only if the heart rate remains below 60/min despite 30 seconds of effective positive pressure ventilation and 60 seconds of effective chest compressions.
- The current heart rate is 70/min, and the prior steps of resuscitation have not yet included effective PPV for the required duration, so epinephrine is not yet indicated.
Pediatric advanced life support US Medical PG Question 2: A 7-year-old boy is brought to the emergency room because of severe, acute diarrhea. He is drowsy with a dull, lethargic appearance. He has sunken eyes, poor skin turgor, and dry oral mucous membranes and tongue. He has a rapid, thready pulse with a systolic blood pressure of 60 mm Hg and his respirations are 33/min. His capillary refill time is 6 sec. He has had no urine output for the past 24 hours. Which of the following is the most appropriate next step in treatment?
- A. Start IV fluid resuscitation by administering colloid solutions
- B. Provide oral rehydration therapy to correct dehydration
- C. Give initial IV bolus of 2 L of Ringer’s lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1
- D. Start IV fluid resuscitation with normal saline or Ringer’s lactate, along with monitoring of vitals and urine output (Correct Answer)
- E. Give antidiarrheal drugs
Pediatric advanced life support Explanation: ***Start IV fluid resuscitation with normal saline or Ringer's lactate, along with monitoring of vitals and urine output***
- This patient presents with **severe dehydration** and **hypovolemic shock** (lethargy, sunken eyes, poor skin turgor, dry mucous membranes, rapid thready pulse, hypotension [systolic BP 60 mmHg], tachypnea, prolonged capillary refill >5 seconds, and anuria).
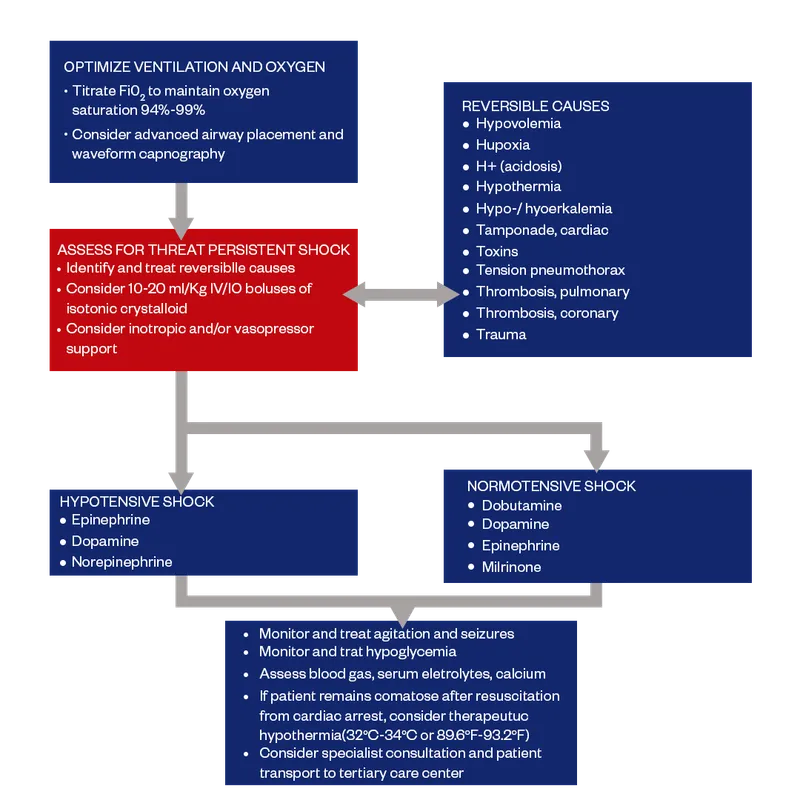
- According to **PALS guidelines**, the immediate priority is rapid intravenous administration of **isotonic crystalloids** (normal saline or Ringer's lactate) given as **20 mL/kg boluses** over 5-20 minutes, repeated as needed based on clinical response.
- Close monitoring of vital signs, mental status, perfusion (capillary refill), and urine output is essential to assess response to resuscitation and guide further fluid management.
*Start IV fluid resuscitation by administering colloid solutions*
- While colloids (albumin, synthetic colloids) can expand intravascular volume, **isotonic crystalloids** are preferred for initial resuscitation in severe dehydration per **WHO and PALS guidelines**.
- Crystalloids are equally effective, more readily available, less expensive, and have fewer potential adverse effects compared to colloids in pediatric dehydration.
- There is no proven survival benefit of colloids over crystalloids in this clinical scenario.
*Provide oral rehydration therapy to correct dehydration*
- **Oral rehydration therapy (ORT)** is the appropriate first-line treatment for **mild to moderate dehydration** in children who can tolerate oral intake.
- However, ORT is **contraindicated** in patients with **severe dehydration** or **hypovolemic shock**, particularly those with altered mental status, inability to drink, or hemodynamic instability.
- This patient's drowsiness, hypotension, and signs of shock require immediate IV resuscitation; ORT would be too slow and potentially dangerous.
*Give initial IV bolus of 2 L of Ringer's lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1*
- A 2-liter bolus is **excessive and dangerous** for a 7-year-old child (average weight ~23 kg); the appropriate initial bolus is **20 mL/kg** (~460 mL), which can be repeated based on response.
- The **1:1:1 massive transfusion protocol** (packed RBCs, FFP, platelets) is indicated for **hemorrhagic shock** with significant blood loss, not for hypovolemic shock from dehydration.
- There is no evidence of bleeding or coagulopathy in this patient; blood products are not indicated.
*Give antidiarrheal drugs*
- **Antidiarrheal agents** (loperamide, diphenoxylate) are **contraindicated** in young children with acute infectious diarrhea, as they can prolong illness, increase risk of complications (toxic megacolon, bacterial overgrowth), and mask serious underlying conditions.
- The priority in severe dehydration is **fluid and electrolyte resuscitation**, not stopping the diarrhea.
- The diarrhea typically resolves once the underlying infection is controlled and hydration is restored.
Pediatric advanced life support US Medical PG Question 3: A first time mother of a healthy, full term, newborn girl is anxious about sudden infant death syndrome. Which of the following pieces of advice can reduce the risk of SIDS?
- A. Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in a warm blanket
- B. Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in an infant sleeper
- C. Sleep supine in the parent's bed and use a pacifier after 1 month of age
- D. Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and use a home apnea monitor
- E. Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and avoid smoking (Correct Answer)
Pediatric advanced life support Explanation: ***Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and avoiding smoking***
- **Sleeping supine** (on the back) is the most critical recommendation to reduce SIDS risk, and a **crib without bumpers** and other soft bedding reduces smothering hazards.
- **Pacifier use** after the first month of age has been shown to be protective, and **avoiding smoking** around the infant is crucial as exposure to tobacco smoke significantly increases SIDS risk.
*Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in a warm blanket*
- While **sleeping supine** is correct, **bumpers, pillows, and loose blankets** in the crib are significant risk factors for SIDS, as they can cause accidental suffocation.
- The use of **pillows** is not recommended for infants due to the risk of airway obstruction and suffocation.
*Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in an infant sleeper*
- Similar to the previous option, **bumpers and a pillow** are unsafe as they pose a suffocation risk and should be avoided in an infant's sleep environment.
- While an **infant sleeper** (or sleep sack) is generally safer than a loose blanket, the presence of bumpers and a pillow negates this benefit.
*Sleep supine in the parent's bed and use a pacifier after 1 month of age*
- **Co-sleeping (sharing a bed with parents)** significantly increases the risk of SIDS and accidental suffocation, especially if parents smoke, are impaired, or if heavy bedding is present.
- Although **pacifier use** is recommended, sleeping in the parent's bed is a major risk factor that outweighs any potential benefit here.
*Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and use a home apnea monitor*
- While **sleeping supine** in a **crib without bumpers** and **pacifier use** are correct recommendations, **home apnea monitors** are not recommended for routine SIDS prevention in healthy infants.
- Apnea monitors have not been shown to reduce the incidence of SIDS and can lead to false alarms and unnecessary anxiety without proven benefit.
Pediatric advanced life support US Medical PG Question 4: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Pediatric advanced life support Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Pediatric advanced life support US Medical PG Question 5: A 3-month-old boy is brought to the emergency department by his mom for breathing difficulty after a recent fall. His parents say that he rolled off of the mattress and landed on the hard wood floor earlier today. After an extensive physical exam, he is found to have many purplish bruises and retinal hemorrhages. A non-contrast head CT scan shows a subdural hemorrhage. He was treated in the hospital with full recovery from his symptoms. Which of the following is the most important follow up plan?
- A. Provide parents with anticipatory guidance
- B. Referral to genetics for further testing
- C. Reassurance that accidents are common
- D. Inform child protective services (Correct Answer)
- E. Provide home nursing visits
Pediatric advanced life support Explanation: ***Inform child protective services***
- The combination of **multiple purplish bruises**, **retinal hemorrhages**, and **subdural hemorrhage** in a 3-month-old infant after a minor fall (rolling off a mattress) is highly suggestive of **abusive head trauma** (shaken baby syndrome).
- Healthcare professionals have a **legal and ethical obligation** to report suspected child abuse to Child Protective Services (CPS) to ensure the child's safety and initiate an investigation.
*Provide parents with anticipatory guidance*
- While anticipatory guidance on child safety and development is generally important, it is **insufficient and inappropriate** as the primary follow-up in a case of suspected child abuse.
- Focusing solely on guidance would **neglect the immediate safety concerns** and the need for investigation into the injuries.
*Referral to genetics for further testing*
- While some genetic conditions can predispose to easy bruising or bleeding, the specific pattern of injuries (**retinal hemorrhages, subdural hemorrhage, multiple bruises, and a history inconsistent with the severity of injuries**) overwhelmingly points to trauma, not a genetic disorder.
- Genetic testing would be a secondary consideration, if at all, after abuse has been ruled out or addressed.
*Reassurance that accidents are common*
- Reassuring parents that "accidents are common" would be **medically negligent and dangerous** in this scenario, as the injuries sustained are typically not caused by a simple fall from a mattress in an infant of this age.
- This response would dismiss critical signs of potential abuse and leave the child at risk.
*Provide home nursing visits*
- Home nursing visits might be beneficial for monitoring general health and development, but they do **not address the immediate and grave concern** of potential child abuse.
- The primary need is for an investigation into the cause of the injuries and protection for the child, which falls under the purview of CPS.
Pediatric advanced life support US Medical PG Question 6: A 3-week-old boy is brought to the emergency department by his parents because of a 3-day history of progressive lethargy and difficulty feeding. He was born at term and did not have difficulty feeding previously. His temperature is 39.4°C (103°F), pulse is 220/min, respirations are 45/min, and blood pressure is 50/30 mm Hg. Pulse oximetry on 100% oxygen shows an oxygen saturation of 97%. Examination shows dry mucous membranes, delayed capillary refill time, and cool skin with poor turgor. Despite multiple attempts by the nursing staff, they are unable to establish peripheral intravenous access. Which of the following is the most appropriate next step in management?
- A. Intraosseous cannulation (Correct Answer)
- B. Ultrasound-guided antecubital vein cannulation
- C. Internal jugular vein cannulation
- D. Intramuscular epinephrine
- E. Rapid sequence intubation
Pediatric advanced life support Explanation: ***Intraosseous cannulation***
- This infant is in **pediatric septic shock** with signs of **poor perfusion** (delayed capillary refill, cool skin, poor turgor, hypotension) and **difficulty obtaining peripheral intravenous access**.
- **Intraosseous (IO) access** is recommended in pediatric emergencies when IV access cannot be established rapidly, providing a route for fluids, medications, and blood products.
*Ultrasound-guided antecubital vein cannulation*
- While ultrasound can improve success rates for peripheral IVs, the **critical condition** of this infant necessitates immediate vascular access, making IO a faster and more reliable option when peripheral attempts fail.
- Delaying definitive fluid resuscitation and medication administration to attempt a more technically challenging peripheral IV could worsen the patient's outcome.
*Internal jugular vein cannulation*
- **Central venous access (e.g., internal jugular)** is a more invasive and time-consuming procedure with higher risks (e.g., pneumothorax) and is not the first-line access in an emergent, unstable pediatric patient due to the time constraint.
- **IO access** is a quicker and safer route for immediate life-saving interventions in pediatric emergencies.
*Intramuscular epinephrine*
- **Intramuscular epinephrine** is primarily used for the treatment of **anaphylaxis** or in certain cardiac arrest algorithms, neither of which is the primary concern here.
- This patient is in septic shock requiring fluid resuscitation and likely antibiotics, which cannot be adequately delivered via intramuscular injection.
*Rapid sequence intubation*
- While intubation might be considered if the patient's respiratory status deteriorates further or for airway protection, the **immediate priority** is to address the **shock** and **poor perfusion** through vascular access and fluid resuscitation.
- **Intubation** alone will not correct the underlying circulatory collapse and shock state.
Pediatric advanced life support US Medical PG Question 7: A 5-year-old is brought into the emergency department for trouble breathing. He was at a family picnic playing when his symptoms began. The patient is currently struggling to breathe and has red, warm extremities. The patient has an unknown medical history and his only medications include herbs that his parents give him. His temperature is 99.5°F (37.5°C), pulse is 112/min, blood pressure is 70/40 mmHg, respirations are 18/min, and oxygen saturation is 82% on 100% O2. Which of the following is the best initial step in management?
- A. Intubation
- B. Albuterol
- C. Cricothyroidotomy
- D. Albuterol, ipratropium, and magnesium
- E. Epinephrine (Correct Answer)
Pediatric advanced life support Explanation: ***Epinephrine***
- This patient is exhibiting signs of **anaphylactic shock** (difficulty breathing, red/warm extremities, hypotension) likely triggered by an allergen at the picnic. **Epinephrine** is the first-line treatment for anaphylaxis due to its alpha and beta-adrenergic effects that counteract vasodilation, bronchoconstriction, and histamine release.
- The rapid onset of symptoms and cardiovascular collapse (hypotension) necessitate immediate administration of epinephrine to stabilize the patient.
*Intubation*
- While the patient is in respiratory distress, intubation is a more invasive procedure and not the *initial* best step for anaphylactic shock. **Epinephrine** should be administered first to address the underlying physiological derangements.
- Airway management, including intubation, may be necessary if epinephrine fails to improve respiratory status, but it is secondary to addressing the systemic allergic reaction.
*Albuterol*
- **Albuterol** is a bronchodilator that helps with bronchospasm, but it does not address the widespread vasodilation, hypotension, or other systemic effects of anaphylaxis.
- While it might provide some symptomatic relief for breathing, it is insufficient as a standalone treatment for anaphylactic shock and would not prevent cardiovascular collapse.
*Cricothyroidotomy*
- **Cricothyroidotomy** is an emergency airway procedure used when conventional intubation is impossible due to upper airway obstruction.
- In this scenario, the primary issue is systemic anaphylaxis causing bronchospasm and shock, not an isolated upper airway obstruction, making epinephrine the more appropriate initial intervention.
*Albuterol, ipratropium, and magnesium*
- This combination is typically used for severe asthma exacerbations, focusing on bronchodilation and smooth muscle relaxation.
- Like albuterol alone, this combination does not address the underlying systemic vasodilation and hypotension characteristic of anaphylactic shock, which requires **epinephrine**.
Pediatric advanced life support US Medical PG Question 8: An inconsolable mother brings her 2-year-old son to the emergency room after finding a large amount of bright red blood in his diaper, an hour ago. She states that for the past week her son has been having crying fits while curling his legs towards his chest in a fetal position. His crying resolves either after vomiting or passing fecal material. Currently, the child is in no apparent distress. Physical examination with palpation in the gastric region demonstrates no acute findings. X-ray of the abdominal area demonstrates no acute findings. His current temperature is 36.5°C (97.8°F), heart rate is 93/min, blood pressure is 100/64 mm Hg, and respiratory rate is 26/min. His weight is 10.8 kg (24.0 lb), and height is 88.9 cm (35.0 in). Laboratory tests show the following:
RBC count 5 million/mm3
Hematocrit 36%
Hemoglobin 12 g/dL
WBC count 6,000/mm3
Mean corpuscular volume 78 fL
What is the most likely underlying embryological cause predisposing to this condition?
- A. Failure of the vitelline duct to close (Correct Answer)
- B. Failure of the vitelline duct to open
- C. Elevated anti-mitochondrial antibodies
- D. Problem with bilirubin conjugation
- E. Problem with bilirubin uptake
Pediatric advanced life support Explanation: ***Failure of the vitelline duct to close***
- The clinical presentation of a 2-year-old with recurrent episodes of abdominal pain, crying spells (curling legs to chest), and the passage of bright red blood in the diaper is highly suggestive of **intussusception**. This can be transiently relieved when the "curled" bowel straightens itself out, or gas/fecal matter is passed. The presence of **bright red blood** (often referred to as **currant jelly stools** when mixed with mucus) further supports this diagnosis, indicating ischemic bowel.
- In children, intussusception is often idiopathic, but in a small percentage of cases, especially in older infants and children, an **anatomical lead point** can cause it. The most common anatomical lead point is a **Meckel's diverticulum**, which results from the **incomplete obliteration of the vitelline duct** (also known as the omphalomesenteric duct) during embryological development. The diverticulum can act as a foreign body that then telescopes into the adjacent bowel, causing intussusception.
*Failure of the vitelline duct to open*
- The vitelline duct should normally regress and disappear. Therefore, a "failure to open" is not a recognized embryological anomaly or pathology.
- Problems related to the vitelline duct involve either its **incomplete closure** (leading to Meckel's diverticulum, vitelline cysts, or fistulas) or other abnormal remnants, not a failure to open.
*Elevated anti-mitochondrial uptake*
- This option refers to **anti-mitochondrial antibodies (AMAs)**, which are characteristic markers for **primary biliary cholangitis (PBC)**, an autoimmune disease primarily affecting the liver.
- PBC is an adult-onset condition and is not associated with intussusception or the gastrointestinal symptoms described in the child.
*Problem with bilirubin conjugation*
- Issues with **bilirubin conjugation** primarily manifest as different types of **jaundice** (e.g., Crigler-Najjar syndrome, Gilbert's syndrome) due to the accumulation of unconjugated bilirubin.
- These conditions do not cause abdominal pain, intussusception, or bloody stools.
*Problem with bilirubin uptake*
- Problems with **bilirubin uptake** by hepatocytes also lead to **unconjugated hyperbilirubinemia** and jaundice.
- This condition is unrelated to acute abdominal emergencies like intussusception or gastrointestinal bleeding.
Pediatric advanced life support US Medical PG Question 9: An 11-year-old boy presents to the emergency department with heavy drooling. The patient was being watched by his babysitter when she found him in this manner. His temperature is 99.1°F (37.3°C), blood pressure is 107/58 mmHg, pulse is 119/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for a young boy in acute distress who is drooling. The boy states he is in pain and can’t swallow. The patient’s tongue seems abnormally enlarged and erythematous. Which of the following is the most likely diagnosis?
- A. Insecticide exposure
- B. Iron overdose
- C. Diphenhydramine ingestion
- D. Caustic ingestion (Correct Answer)
- E. Aspirin overdose
Pediatric advanced life support Explanation: ***Caustic ingestion***
- The combination of **heavy drooling**, inability to swallow (**dysphagia**), and **painful oropharynx** with an enlarged, erythematous tongue points strongly to **caustic ingestion**, which causes corrosive injury to the oral mucosa and esophagus.
- The acute onset in a child with no other clear cause for distress, particularly when an unknown exposure (babysitter found him) is suggested, raises suspicion for accidental poisoning.
*Insecticide exposure*
- **Insecticide (organophosphate)** exposure would typically involve symptoms of **cholinergic crisis**, such as **salivation**, lacrimation, urination, defecation, GI upset, and emesis (SLUDGE syndrome), along with **miosis** and **bradycardia**.
- While drooling is present, the absence of other cholinergic signs and the specific description of tongue enlargement and redness makes this less likely.
*Iron overdose*
- **Iron overdose** can cause significant gastrointestinal irritation, leading to **vomiting**, diarrhea, and **abdominal pain**, potentially with hematemesis or melena.
- It does not typically present with severe drooling and a visibly enlarged, erythematous tongue in the acute phase as the primary complaint.
*Diphenhydramine ingestion*
- **Diphenhydramine** is an **antihistamine** with significant **anticholinergic effects**, which would cause **dry mouth**, not heavy drooling.
- Other symptoms would include **tachycardia**, altered mental status, and dilated pupils, none of which are consistent with the presentation.
*Aspirin overdose*
- **Aspirin (salicylate) overdose** typically causes a mixed **acid-base disturbance** (respiratory alkalosis and metabolic acidosis), **tinnitus**, and gastrointestinal upset (vomiting, abdominal pain).
- It does not explain the pronounced drooling, difficulty swallowing, or the physical findings of an enlarged, erythematous tongue in this acute presentation.
Pediatric advanced life support US Medical PG Question 10: A previously healthy 5-year-old boy is brought to the emergency department because of a 1-day history of high fever. His temperature prior to arrival was 40.0°C (104°F). There is no family history of serious illness. Development has been appropriate for his age. He is administered rectal acetaminophen. While in the waiting room, he becomes unresponsive and starts jerking his arms and legs back and forth. A fingerstick blood glucose concentration is 86 mg/dL. After 5 minutes, he continues having jerky movements and is unresponsive to verbal and painful stimuli. Which of the following is the most appropriate next step in management?
- A. Intravenous administration of lorazepam (Correct Answer)
- B. Intravenous administration of phenobarbital
- C. Obtain blood cultures
- D. Intravenous administration of valproate
- E. Intravenous administration of fosphenytoin
Pediatric advanced life support Explanation: ***Intravenous administration of lorazepam***
- The child is experiencing a **prolonged seizure** (greater than 5 minutes) following a high fever, which is concerning for **status epilepticus** secondary to a febrile seizure.
- **Lorazepam** is a first-line benzodiazepine for status epilepticus due to its rapid onset of action and prolonged anticonvulsant effect.
*Intravenous administration of phenobarbital*
- **Phenobarbital** is a long-acting anticonvulsant often used for **refractory status epilepticus** or as a long-term maintenance therapy.
- It is not the preferred initial treatment for an acute, prolonged seizure due to its slower onset compared to benzodiazepines.
*Obtain blood cultures*
- While obtaining blood cultures is important for identifying potential sources of infection causing the fever, it is **not the immediate priority** when a child is actively seizing and unresponsive.
- **Seizure termination** takes precedence to prevent potential neurological injury.
*Intravenous administration of valproate*
- **Valproate** is an anticonvulsant that can be used for various seizure types, but it is typically reserved for **refractory status epilepticus** or as a long-term maintenance drug.
- It does not have the rapid onset of action required for initial management of an acute, prolonged seizure.
*Intravenous administration of fosphenytoin*
- **Fosphenytoin** is an antiepileptic drug often used for **refractory status epilepticus** after benzodiazepines have failed.
- It is not the first-line medication for the initial management of an acute seizure of this duration.
More Pediatric advanced life support US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.