Diabetic ketoacidosis in children US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diabetic ketoacidosis in children. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diabetic ketoacidosis in children US Medical PG Question 1: A 19-year-old man with a history of type 1 diabetes presents to the emergency department for the evaluation of a blood glucose level of 492 mg/dL. Laboratory examination revealed a serum bicarbonate level of 13 mEq/L, serum sodium level of 122 mEq/L, and ketonuria. Arterial blood gas demonstrated a pH of 6.9. He is admitted to the hospital and given bicarbonate and then started on an insulin drip and intravenous fluid. Seven hours later when his nurse is making rounds, he is confused and complaining of a severe headache. Repeat sodium levels are unchanged, although his glucose level has improved. His vital signs include a temperature of 36.6°C (98.0°F), pulse 50/min, respiratory rate 13/min and irregular, and blood pressure 177/95 mm Hg. What other examination findings would be expected in this patient?
- A. Hypoglycemia
- B. Pupillary constriction
- C. Papilledema (Correct Answer)
- D. Pancreatitis
- E. Peripheral edema
Diabetic ketoacidosis in children Explanation: ***Papilledema***
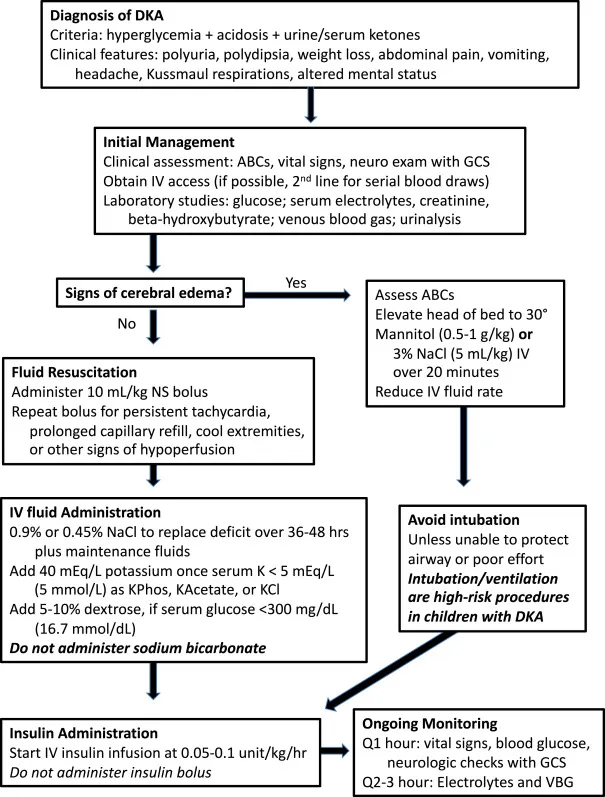
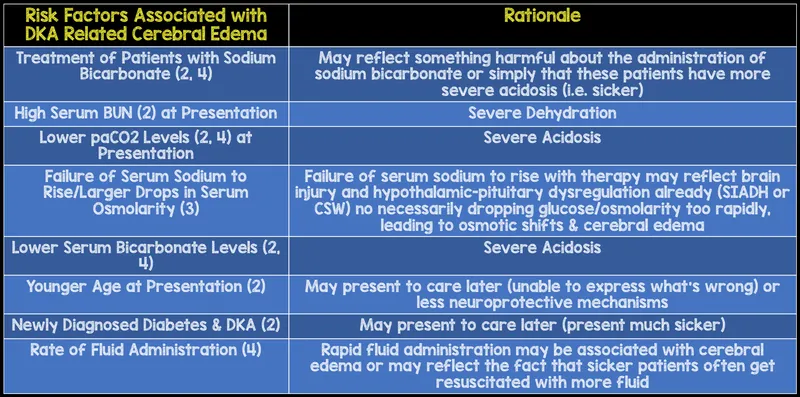
- This patient's symptoms (confusion, severe headache, bradycardia, irregular respiration, hypertension) following treatment for **diabetic ketoacidosis (DKA)** are highly suggestive of **cerebral edema**.
- **Papilledema** is a retinal finding resulting from increased intracranial pressure (ICP), which is a characteristic sign of cerebral edema.
*Hypoglycemia*
- While the patient's glucose level has improved, it is not described as being low enough to cause hypoglycemia, and the symptoms are more consistent with **increased ICP**.
- Symptoms of hypoglycemia (e.g., tremors, sweating, hunger, anxiety) are different from the patient's current presentation of confusion and severe headache.
*Pupillary constriction*
- **Pupillary constriction** (miosis) is typically not associated with cerebral edema; instead, **pupillary dilation** (mydriasis) can occur with severe increase in ICP due to uncal herniation.
- The combination of bradycardia, irregular respiration, and hypertension (Cushing's triad) is indicative of increased ICP, which would likely cause pupillary changes related to brainstem compression.
*Pancreatitis*
- Pancreatitis is a known complication of DKA, but it typically presents with **severe abdominal pain**, nausea, and vomiting, rather than cerebral symptoms.
- Although the patient had DKA, the current neurological symptoms point directly to an intracranial process rather than an abdominal issue.
*Peripheral edema*
- **Peripheral edema** results from fluid accumulation in peripheral tissues and is not a direct consequence or expected finding in cerebral edema.
- While fluid administration can cause some peripheral fluid retention, it typically does not lead to the acute neurological deterioration seen in this patient.
Diabetic ketoacidosis in children US Medical PG Question 2: A 16-year-old woman presents to the emergency department for evaluation of acute vomiting and abdominal pain. Onset was roughly 3 hours ago while she was sleeping. She has no known past medical history. Her family history is positive for hypothyroidism and diabetes mellitus in her maternal grandmother. On examination, she is found to have fruity breath and poor skin turgor. She appears fatigued and her consciousness is slightly altered. Laboratory results show a blood glucose level of 691 mg/dL, sodium of 125 mg/dL, and elevated serum ketones. Of the following, which is the next best step in patient management?
- A. Administer IV fluids and insulin (Correct Answer)
- B. Initiate basal-bolus insulin regimen
- C. Initiate insulin glargine 10 units at bedtime only
- D. Initiate oral antidiabetic medications
- E. Initiate insulin aspart at mealtimes only
Diabetic ketoacidosis in children Explanation: ***Administer IV fluids and insulin***
- The patient presents with **fruity breath**, **altered consciousness**, **hyperglycemia (691 mg/dL)**, **hyponatremia**, and **elevated serum ketones**, which are classic signs of **diabetic ketoacidosis (DKA)**.
- The immediate management for DKA involves aggressive **intravenous fluid resuscitation** to correct dehydration and hypovolemia, followed by a continuous **intravenous insulin infusion** to lower blood glucose and suppress ketogenesis.
*Initiate basal-bolus insulin regimen*
- A **basal-bolus insulin regimen** is appropriate for long-term management of diabetes but is not the immediate treatment for acute DKA, which requires continuous intravenous insulin.
- This approach does not address the severe dehydration and electrolyte imbalances seen in DKA, which need urgent fluid replacement.
*Initiate insulin glargine 10 units at bedtime only*
- **Insulin glargine** is a long-acting insulin used for basal insulin coverage, typically in the chronic management of diabetes.
- This dose is insufficient to manage acute DKA, and it also fails to address the critical need for fluid resuscitation.
*Initiate oral antidiabetic medications*
- **Oral antidiabetic medications** are suitable for individuals with type 2 diabetes or milder forms of insulin resistance, not for acute DKA.
- They are ineffective in severe hyperglycemia and metabolic acidosis characteristic of DKA, and do not address dehydration.
*Initiate insulin aspart at mealtimes only*
- **Insulin aspart** is a rapid-acting insulin used to cover mealtime glucose excursions.
- Administering it only at mealtimes is inadequate for acute DKA, which requires continuous insulin infusion and aggressive fluid management.
Diabetic ketoacidosis in children US Medical PG Question 3: A 35-year-old patient with a history of diabetes presents to the ED with a myriad of systemic complaints. An arterial blood gas shows serum pH = 7.3, HCO3- = 13 mEq/L, PCO2 = 27 mmHg. Which of the following would you LEAST expect to observe in this patient?
- A. Increased anion gap
- B. Increased urine output
- C. Increased serum potassium
- D. Decreased respiratory rate (Correct Answer)
- E. Increased serum ketones
Diabetic ketoacidosis in children Explanation: ***Decreased respiratory rate***
- This patient has **diabetic ketoacidosis (DKA)**, which causes a metabolic acidosis. The body compensates for acidosis by increasing the respiratory rate (**Kussmaul respirations**) to blow off CO2, thus decreasing serum acidity.
- A decreased respiratory rate would worsen the acidosis by retaining CO2, which is contrary to the body's compensatory mechanism in DKA.
- This is what you would **LEAST expect** to observe in a patient with DKA.
*Increased anion gap*
- The patient's **pH of 7.3** and **HCO3- of 13 mEq/L** indicate a metabolic acidosis with a PCO2 of 27 mmHg showing respiratory compensation.
- DKA is characterized by the accumulation of **ketoacids** (acetoacetate, beta-hydroxybutyrate), which are unmeasured anions, leading to an **elevated anion gap**.
- This is an **expected finding** in DKA.
*Increased urine output*
- In DKA, **hyperglycemia** leads to an osmotic diuresis as excess glucose is filtered by the kidneys and draws water out, resulting in **polyuria** (increased urine output).
- This excessive urination contributes to **dehydration**, a common finding in DKA.
- This is an **expected finding** in DKA.
*Increased serum potassium*
- Despite total body potassium depletion, patients in DKA often present with **normal or elevated serum potassium** due to intracellular potassium shifting out of cells in exchange for hydrogen ions (to buffer acidosis).
- **Insulin deficiency** also contributes to this shift by impairing potassium uptake into cells.
- This is an **expected finding** in DKA, though potassium will drop with insulin treatment.
*Increased serum ketones*
- **Diabetic ketoacidosis (DKA)** is fundamentally caused by insulin deficiency, leading to increased **lipolysis** and subsequent overproduction of **ketone bodies** (acetoacetate, beta-hydroxybutyrate) by the liver.
- These ketones accumulate in the blood, causing the characteristic metabolic acidosis and are measurable in serum and urine.
- This is an **expected finding** and diagnostic of DKA.
Diabetic ketoacidosis in children US Medical PG Question 4: A previously healthy 14-year-old girl is brought to the emergency department by her mother because of abdominal pain, nausea, and vomiting for 6 hours. Over the past 6 weeks, she has also had increased frequency of urination, and she has been drinking more water than usual. She has lost 6 kg (13 lb) over the same time period despite having a good appetite. Her temperature is 37.1°C (98.8°F), pulse is 125/min, respirations are 32/min, and blood pressure is 94/58 mm Hg. She appears lethargic. Physical examination shows deep and labored breathing and dry mucous membranes. The abdomen is soft, and there is diffuse tenderness to palpation with no guarding or rebound. Urine dipstick is positive for ketones and glucose. Further evaluation is most likely to show which of the following findings?
- A. Excess water retention
- B. Serum glucose concentration > 800 mg/dL
- C. Increased arterial pCO2
- D. Increased arterial blood pH
- E. Decreased total body potassium (Correct Answer)
Diabetic ketoacidosis in children Explanation: ***Decreased total body potassium***
- This is the correct answer. In **diabetic ketoacidosis (DKA)**, patients have **significant total body potassium depletion** due to osmotic diuresis and urinary losses.
- **Serum potassium may initially appear normal or even elevated** due to acidosis-induced extracellular shift of potassium from cells.
- However, **total body potassium stores are markedly depleted**, and during treatment with insulin and fluids, severe hypokalemia can develop as potassium shifts back intracellularly.
*Excess water retention*
- The patient's symptoms, including **polydipsia**, **polyuria**, and **dry mucous membranes**, indicate **dehydration**, not excessive water retention.
- Her blood pressure of 94/58 mm Hg also suggests **volume depletion**.
*Serum glucose concentration > 800 mg/dL*
- While the patient has significant hyperglycemia (indicated by glucose in urine), **DKA** typically presents with glucose levels between **250-600 mg/dL**.
- Glucose levels >800 mg/dL are more characteristic of **hyperosmolar hyperglycemic state (HHS)**, which is less common in children and usually lacks significant ketosis.
*Increased arterial pCO2*
- The patient exhibits **Kussmaul respirations** (deep and labored breathing) and an increased respiratory rate (32/min), which are compensatory mechanisms for **metabolic acidosis**.
- This compensation leads to **decreased arterial pCO2** as the body tries to blow off CO2 to raise pH.
*Increased arterial blood pH*
- The symptoms, particularly **Kussmaul respirations** and the presence of **ketones** in the urine, strongly suggest **diabetic ketoacidosis (DKA)**.
- DKA is characterized by **severe metabolic acidosis**, meaning the arterial blood pH would be **decreased**, not increased.
Diabetic ketoacidosis in children US Medical PG Question 5: A 20-year-old male is brought by ambulance to the emergency room in extremis. He is minimally conscious, hypotensive, and tachypneic, and his breath gives off a "fruity" odor. An arterial blood gas and metabolic panel show anion gap metabolic acidosis. This patient is most likely deficient in which of the following metabolic actions?
- A. Glucagon production
- B. Cortisol secretion
- C. Formation of ketone bodies
- D. Glucose production
- E. Cellular uptake of glucose (Correct Answer)
Diabetic ketoacidosis in children Explanation: ***Cellular uptake of glucose***
- The patient's symptoms, including **fruity odor breath**, **anion gap metabolic acidosis**, and being found in extremis, are classic signs of **diabetic ketoacidosis (DKA)**.
- DKA results from a profound lack of **insulin**, which is essential for cells (especially muscle and adipose tissue) to take up glucose from the bloodstream, leading to hyperglycemia and a shift to fat metabolism.
*Glucagon production*
- **Glucagon** is a counter-regulatory hormone that *raises* blood glucose levels, and its production is often *increased* in DKA as the body attempts to provide fuel to cells in the absence of insulin's effect.
- A deficiency in glucagon production would more likely lead to **hypoglycemia**, not the profound hyperglycemia seen in DKA.
*Cortisol secretion*
- **Cortisol** is another counter-regulatory hormone that *increases* blood glucose, and its secretion is typically *elevated* in stress states like DKA.
- A deficiency in cortisol (e.g., in adrenal insufficiency) would present with different symptoms such as **hypoglycemia**, **hyponatremia**, and **hyperkalemia**, without the classic DKA picture.
*Formation of ketone bodies*
- The patient's **fruity odor breath** and **anion gap metabolic acidosis** are direct consequences of the *overproduction* of **ketone bodies**.
- This overproduction occurs when the body, lacking glucose for fuel due to insulin deficiency, switches to **fat metabolism**, leading to excessive formation of acetoacetate, beta-hydroxybutyrate, and acetone.
*Glucose production*
- **Glucose production** (gluconeogenesis and glycogenolysis) is typically *increased* in DKA as the liver tries to supply glucose to the body due to perceived cellular starvation (despite high blood glucose).
- A deficiency in glucose production, such as in certain glycogen storage diseases or severe liver failure, would lead to **hypoglycemia**, not the hyperglycemia characteristic of DKA.
Diabetic ketoacidosis in children US Medical PG Question 6: A 14-year-old boy is admitted to the emergency department with acute onset of confusion, malaise, diffuse abdominal pain, nausea, and a single episode of vomiting. He denies ingestion of any suspicious foods, fevers, respiratory symptoms, or any other symptoms preceding his current condition. However, he notes an increase in his liquid consumption and urinary frequency over the last 6 months. On physical examination, he is responsive but somnolent. His blood pressure is 90/50 mm Hg, heart rate is 101/min, respiratory rate is 21/min, temperature is 36.0°C (96.8°F), and SpO2 is 96% on room air. He has facial pallor and dry skin and mucous membranes. His lungs are clear to auscultation, and heart sounds are normal. His abdomen is soft with no rebound tenderness on palpation. Neurological examination is significant for 1+ deep tendon reflexes in all extremities. A dipstick test shows 3+ for ketones and glucose. The patient’s blood tests show the following findings:
RBCs 4.1 million/mm3
Hb 13.7 mg/dL
Hematocrit 56%
Leukocyte count 7,800/mm3
Platelet count 321,000/mm3
Glucose 565 mg/dL
Potassium 5.8 mEq/L
Sodium 136 mEq/L
ALT 15 U/L
AST 17 U/L
Amylase 88 U/L
Bicarbonate 19 mEq/L
BE −3 mEq/L
pH 7.3
pCO2 37 mm Hg
pO2 66 mm Hg
Which of the medications listed below should be administered to the patient intravenously?
- A. Insulin detemir
- B. Regular insulin (Correct Answer)
- C. Cefazolin
- D. Potassium chloride
- E. Isophane insulin
Diabetic ketoacidosis in children Explanation: **Regular insulin**
- The patient presents with **diabetic ketoacidosis (DKA)**, characterized by **hyperglycemia** (glucose 565 mg/dL), **ketonuria** (ketones 3+), and **metabolic acidosis** (pH 7.3, bicarbonate 19 mEq/L, BE -3 mEq/L). **Intravenous regular insulin** is the cornerstone of DKA treatment to lower blood glucose and resolve ketosis.
- Regular insulin is the only type of insulin that can be administered intravenously and has a **rapid onset** and **short duration of action**, allowing for precise titration and quick correction of severe hyperglycemia and acidosis.
*Insulin detemir*
- **Insulin detemir** is a **long-acting insulin analog** primarily used for basal insulin replacement, not for acute management of severe hyperglycemia or DKA.
- It has a **slow onset of action** (1-2 hours) and a prolonged duration (up to 24 hours), making it unsuitable for the urgent and rapid correction required in DKA.
*Cefazolin*
- **Cefazolin** is a **first-generation cephalosporin antibiotic** used to treat bacterial infections.
- This patient's symptoms are consistent with DKA, not a bacterial infection, and there is no indication for antibiotic therapy.
*Potassium chloride*
- Despite the patient's **hyperkalemia** (potassium 5.8 mEq/L) at presentation, DKA treatment with insulin will shift potassium intracellularly, leading to **hypokalemia**.
- **Potassium chloride** is typically added to IV fluids **after insulin therapy has begun and potassium levels start to drop**, to prevent severe hypokalemia, not as an initial treatment when levels are already high.
*Isophane insulin*
- **Isophane insulin (NPH)** is an **intermediate-acting insulin** that is administered subcutaneously.
- It has a **delayed onset of action** (2-4 hours) and cannot be given intravenously, making it inappropriate for the acute management of DKA.
Diabetic ketoacidosis in children US Medical PG Question 7: A boy with diabetic ketoacidosis is admitted to the pediatric intensive care unit for closer monitoring. Peripheral venous access is established. He is treated with IV isotonic saline and started on an insulin infusion. This patient is at the highest risk for which of the following conditions in the next 24 hours?
- A. Cerebral edema (Correct Answer)
- B. Intrinsic kidney injury
- C. Cognitive impairment
- D. Hyperkalemia
- E. Deep venous thrombosis
Diabetic ketoacidosis in children Explanation: ***Cerebral edema***
- **Cerebral edema** is a severe and potentially fatal complication of **diabetic ketoacidosis (DKA)** treatment, particularly in children.
- It results from a rapid decrease in serum osmolality during treatment, causing water to shift into brain cells.
*Intrinsic kidney injury*
- While dehydration in DKA can lead to **prerenal acute kidney injury**, **intrinsic kidney injury** is less common as an acute risk directly from DKA treatment in the first 24 hours.
- Initial fluid resuscitation often improves renal perfusion, reducing the risk of intrinsic damage unless other predisposing factors are present.
*Cognitive impairment*
- Cognitive impairment after DKA is more commonly observed in the long term, potentially due to recurrent episodes or severe DKA with cerebral edema.
- It is not the most immediate and highest risk acute complication in the short-term (next 24 hours).
*Hyperkalemia*
- Patients with DKA typically present with **hyperkalemia** due to acidosis and insulin deficiency, which resolves with insulin therapy as potassium shifts back into cells.
- The more immediate risk during treatment, especially after initial fluid resuscitation and insulin, is **hypokalemia**, not hyperkalemia, due to the intracellular shift of potassium.
*Deep venous thrombosis*
- **Dehydration** and **hyperviscosity** associated with DKA can increase the risk of **thrombosis**, but **deep venous thrombosis** is not the highest or most immediate acute risk in the next 24 hours.
- **Cerebral edema** is a more specific and life-threatening complication directly related to the treatment of DKA in children.
Diabetic ketoacidosis in children US Medical PG Question 8: An 8-year old boy is brought to the emergency department because he has been lethargic and has had several episodes of nausea and vomiting for the past day. He has also had increased thirst over the past two months. He has lost 5.4 kg (11.9 lbs) during this time. He is otherwise healthy and has no history of serious illness. His temperature is 37.5 °C (99.5 °F), blood pressure is 95/68 mm Hg, pulse is 110/min, and respirations are 30/min. He is somnolent and slightly confused. His mucous membranes are dry. Laboratory studies show:
Hemoglobin 16.2 g/dL
Leukocyte count 9,500/mm3
Platelet count 380,000/mm3
Serum
Na+ 130 mEq/L
K+ 5.5 mEq/L
Cl- 99 mEq/L
HCO3- 16 mEq/L
Creatinine 1.2 mg/dL
Glucose 570 mg/dL
Ketones positive
Blood gases, arterial
pH 7.25
pCO2 21 mm Hg
Which of the following is the most appropriate next step in management?
- A. Intravenous hydration with 0.45% normal saline and insulin
- B. Intravenous hydration with 5% dextrose solution and 0.45% normal saline
- C. Intravenous sodium bicarbonate
- D. Intravenous hydration with 0.9% normal saline and insulin (Correct Answer)
- E. Intravenous hydration with 0.9% normal saline and potassium chloride
Diabetic ketoacidosis in children Explanation: ***Intravenous hydration with 0.9% normal saline and insulin***
- This patient presents with **diabetic ketoacidosis (DKA)**, characterized by hyperglycemia (glucose 570 mg/dL), metabolic acidosis (pH 7.25, HCO3- 16 mEq/L, ketones positive), and dehydration (dry mucous membranes, increased thirst, weight loss).
- Initial management of DKA involves aggressive **volume expansion** with **0.9% normal saline** to restore perfusion and reduce hyperglycemia; subsequently, **insulin infusion** is started to correct hyperglycemia and halt ketogenesis.
*Intravenous hydration with 0.45% normal saline and insulin*
- While insulin is crucial, **0.45% normal saline (hypotonic saline)** is generally not the initial fluid of choice for DKA due to the risk of exacerbating cerebral edema, especially in children.
- **Isotonic saline (0.9% normal saline)** is preferred for initial resuscitation to rapidly restore extracellular fluid volume.
*Intravenous hydration with 5% dextrose solution and 0.45% normal saline*
- **5% dextrose solution** should only be added to intravenous fluids when the blood glucose level falls to around 200-250 mg/dL, to prevent hypoglycemia while continuing insulin to resolve ketosis.
- Administering dextrose initially would worsen the existing severe hyperglycemia.
*Intravenous sodium bicarbonate*
- **Sodium bicarbonate** is generally not recommended for mild to moderate DKA due to potential risks like cerebral edema and metabolic alkalosis, and potential paradoxical worsening of CNS acidosis.
- Bicarbonate therapy is reserved for **severe acidosis (pH < 6.9 or 7.0)** with hemodynamic instability or impaired cardiac contractility, which is not the case here.
*Intravenous hydration with 0.9% normal saline and potassium chloride*
- While **0.9% normal saline** is appropriate, this option lacks **insulin therapy**, which is essential for treating DKA by halting ketogenesis and correcting hyperglycemia.
- Although potassium supplementation will be necessary during DKA treatment (as insulin drives K+ into cells and can cause hypokalemia), the most appropriate **next step** is to initiate both fluid resuscitation and insulin therapy together.
- The patient's current potassium level of 5.5 mEq/L is at the upper limit of normal, but reflects total body potassium depletion; potassium should be added to maintenance fluids once adequate urine output is established.
Diabetic ketoacidosis in children US Medical PG Question 9: A previously healthy 10-year-old boy is brought to the emergency room by his mother 5 hours after the onset of abdominal pain and nausea. Over the past 2 weeks, he has also had progressive abdominal pain and a 4-kg (8.8-lb) weight loss. The mother reports that her son has been drinking more water than usual during this period. Last week he wet his bed three times despite being completely toilet-trained since 3 years of age. His temperature is 37.8°C (100°F), pulse is 128/min, respirations are 35/min, and blood pressure is 95/55 mm Hg. He appears lethargic. Physical examination shows deep and labored breathing and dry mucous membranes. The abdomen is soft, and there is diffuse tenderness to palpation with no guarding or rebound. Serum laboratory studies show:
Na+ 133 mEq/L
K+ 5.9 mEq/L
Cl- 95 mEq/L
HCO3- 13 mEq/L
Urea nitrogen 25 mg/dL
Creatinine 1.0 mg/dL
Urine dipstick is positive for ketones and glucose. Further evaluation is most likely to reveal which of the following?
- A. Serum glucose concentration > 600 mg/dL
- B. Increased total body sodium
- C. Increased arterial pCO2
- D. Hypervolemia
- E. Decreased total body potassium (Correct Answer)
Diabetic ketoacidosis in children Explanation: **Decreased total body potassium**
- Despite **hyperkalemia** on serum labs, patients with **diabetic ketoacidosis (DKA)** often have a **total body potassium deficit** due to increased renal losses and intracellular-to-extracellular shifts.
- The combination of polyuria, vomiting, and acidemia all contribute to significant potassium disturbances.
*Serum glucose concentration > 600 mg/dL*
- A glucose level of **over 600 mg/dL** is more characteristic of **hyperglycemic hyperosmolar state (HHS)**, not typically seen in pediatric DKA.
- While DKA involves hyperglycemia, severe dehydration and altered mentation typically occur at lower glucose thresholds in DKA.
*Increased total body sodium*
- Patients with DKA are typically **hypovolemic and hyponatremic** (even if serum sodium appears normal due to pseudohyponatremia) due to osmotic diuresis caused by hyperglycemia.
- There is no mechanism in DKA that would lead to an increase in total body sodium.
*Increased arterial pCO2*
- The patient's **deep and labored breathing (Kussmaul respirations)** is a compensatory mechanism to **blow off CO2** and correct the metabolic acidosis.
- Therefore, arterial pCO2 would be **decreased**, not increased.
*Hypervolemia*
- **Polyuria** (increased urination) due to osmotic diuresis and poor oral intake typically leads to **hypovolemia and dehydration** in DKA patients.
- The patient exhibits signs of dehydration such as dry mucous membranes, increased pulse, and low blood pressure.
Diabetic ketoacidosis in children US Medical PG Question 10: A 27-year-old man presents to the emergency department with his family because of abdominal pain, excessive urination, and drowsiness since the day before. He has had type 1 diabetes mellitus for 2 years. He ran out of insulin 2 days ago. The vital signs at admission include: temperature 36.8°C (98.2°F), blood pressure 102/69 mm Hg, and pulse 121/min. On physical examination, he is lethargic and his breathing is rapid and deep. There is a mild generalized abdominal tenderness without rebound tenderness or guarding. His serum glucose is 480 mg/dL. Arterial blood gas of this patient will most likely show which of the following?
- A. ↑ pH, ↑ bicarbonate, and normal pCO2
- B. ↓ pH, ↓ bicarbonate and ↑ anion gap (Correct Answer)
- C. ↑ pH, normal bicarbonate and ↓ pCO2
- D. ↓ pH, ↓ bicarbonate and normal anion gap
- E. ↓ pH, normal bicarbonate and ↑ pCO2
Diabetic ketoacidosis in children Explanation: ***↓ pH, ↓ bicarbonate and ↑ anion gap***
- The patient's symptoms (abdominal pain, excessive urination, drowsiness, rapid and deep breathing, hyperglycemia) and history of Type 1 diabetes with missed insulin are highly suggestive of **diabetic ketoacidosis (DKA)**.
- DKA is characterized by **metabolic acidosis** due to the accumulation of ketone bodies, leading to a **decreased pH**, consumption of bicarbonate and thus a **decreased bicarbonate level**, and an **increased anion gap**.
*↑ pH, ↑ bicarbonate, and normal pCO2*
- This pattern suggests a **metabolic alkalosis**, which is inconsistent with the patient's presentation of DKA.
- Metabolic alkalosis is typically seen in conditions like severe vomiting or diuretic use, not uncontrolled diabetes.
*↑ pH, normal bicarbonate and ↓ pCO2*
- This profile describes **respiratory alkalosis**, often caused by primary hyperventilation.
- While the patient has rapid and deep breathing (Kussmaul respiration), this is a compensatory mechanism for metabolic acidosis, not a primary respiratory alkalosis.
*↓ pH, ↓ bicarbonate and normal anion gap*
- This indicates a **normal anion gap metabolic acidosis**, also known as hyperchloremic acidosis.
- This is typically seen in conditions like renal tubular acidosis or severe diarrhea, where bicarbonate is lost or chloride is retained, which is not the case for DKA.
*↓ pH, normal bicarbonate and ↑ pCO2*
- This presentation indicates **respiratory acidosis**, which is caused by hypoventilation and retention of CO2.
- The patient's rapid and deep breathing (Kussmaul breathing) is a compensatory mechanism to blow off CO2 and would decrease pCO2, not increase it.
More Diabetic ketoacidosis in children US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.