Child abuse evaluation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Child abuse evaluation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Child abuse evaluation US Medical PG Question 1: A 3-year-old child is brought to the emergency department with multiple bruises in various stages of healing. X-rays reveal several metaphyseal fractures and posterior rib fractures. The parents claim the injuries resulted from normal play activities. Which of the following patterns would most strongly suggest non-accidental trauma?
- A. Circular bruises on the knees
- B. Loop-shaped bruises on the back (Correct Answer)
- C. Linear bruises on the shins
- D. Irregular bruises on the forehead
Child abuse evaluation Explanation: ***Loop-shaped bruises on the back***
- **Loop-shaped bruises** are highly suspicious for **non-accidental trauma** as they are pathognomonic for impact with an object like a looped cord or belt
- Bruises on the **back** of a young child are particularly concerning as the back is a non-bony prominence and less likely to be injured during normal play activities
- Combined with the metaphyseal and posterior rib fractures already identified, patterned bruises strongly indicate inflicted trauma
*Circular bruises on the knees*
- Circular bruises on the knees are very common in toddlers and young children due to normal falls and play, which typically involve kneeling and crawling
- This pattern is generally considered consistent with accidental injury and not indicative of abuse
*Linear bruises on the shins*
- Linear bruises on the shins can result from bumping into objects while playing or exploring, which is common in active children
- The shins are bony prominences frequently injured during normal play activities
*Irregular bruises on the forehead*
- Irregular bruises on the forehead can result from accidental falls or bumps, which are common in young children learning to walk or play
- While head injuries should always be carefully evaluated, irregular bruises on the forehead are common accidental injuries in ambulatory toddlers
Child abuse evaluation US Medical PG Question 2: A 6-month-old male presents to the emergency department with his parents after his three-year-old brother hit him on the arm with a toy truck. His parents are concerned that the minor trauma caused an unusual amount of bruising. The patient has otherwise been developing well and meeting all his milestones. His parents report that he sleeps throughout the night and has just started to experiment with solid food. The patient’s older brother is in good health, but the patient’s mother reports that some members of her family have an unknown blood disorder. On physical exam, the patient is agitated and difficult to soothe. He has 2-3 inches of ecchymoses and swelling on the lateral aspect of the left forearm. The patient has a neurological exam within normal limits and pale skin with blue irises. An ophthalmologic evaluation is deferred.
Which of the following is the best initial step?
- A. Genetic testing
- B. Complete blood count and coagulation panel (Correct Answer)
- C. Ensure the child's safety and alert the police
- D. Peripheral blood smear
- E. Hemoglobin electrophoresis
Child abuse evaluation Explanation: ***Complete blood count and coagulation panel***
- The unusual amount of **bruising** after minor trauma, along with a family history of an unknown blood disorder, strongly suggests a potential **bleeding disorder**. A **CBC** and a **coagulation panel** (PT, aPTT, fibrinogen) are essential initial steps to evaluate for abnormalities in platelets, clotting factors, or other hematologic conditions.
- These tests can help narrow down the differential diagnosis between **platelet dysfunction**, **coagulopathies** (like hemophilia or von Willebrand disease), or other less common bleeding disorders, guiding further specific investigations.
- **Important consideration:** The presence of **blue sclera** (described as "blue irises") raises concern for **osteogenesis imperfecta (OI)**, a connective tissue disorder causing bone fragility. However, initial hematologic screening is still appropriate given the family history of blood disorder and presentation of excessive bruising. If coagulation studies are normal, imaging and further workup for OI would be indicated.
*Genetic testing*
- While a genetic component is plausible given the patient's family history and clinical presentation (blue sclera may suggest osteogenesis imperfecta), **genetic testing** is typically performed *after* initial laboratory workup has identified a specific type of bleeding or inherited disorder.
- Starting with genetic testing without basic hematologic parameters is not the most efficient or cost-effective initial diagnostic approach.
*Ensure the child's safety and alert the police*
- While child abuse should always be considered in cases of unexplained or excessive bruising, the presence of a **family history of a blood disorder** and the **blue sclera** (suggesting possible osteogenesis imperfecta) make **medical causes** more immediate concerns for initial investigation.
- Pursuing a medical workup first often clarifies whether abuse is the primary explanation, although child protective services should be notified if suspicion remains high after medical evaluation.
*Peripheral blood smear*
- A **peripheral blood smear** provides information on red blood cell morphology, platelet size and number, and white blood cell differential. While useful in assessing for some hematologic conditions, it is often performed *after* a CBC has indicated abnormalities or in conjunction with specialized testing.
- It would not be the *best initial step* as it doesn't directly assess clotting factor function, which is critical in evaluating significant bruising severity.
*Hemoglobin electrophoresis*
- **Hemoglobin electrophoresis** is used to diagnose **hemoglobinopathies** like sickle cell anemia or thalassemia.
- The patient's symptoms (easy bruising) are not characteristic of hemoglobinopathies, and while he has pale skin, this test would not be the initial step to investigate a bleeding disorder.
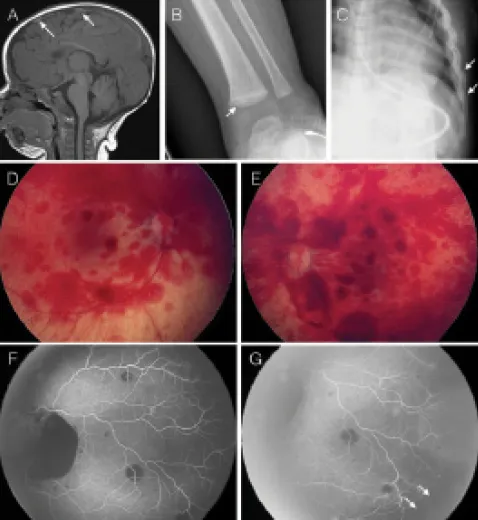
Child abuse evaluation US Medical PG Question 3: A 4-month-old infant is brought to the emergency department with seizures. CT scan reveals bilateral subdural hematomas of different ages and retinal hemorrhages. Which of the following mechanisms best explains these findings?
- A. Infectious meningitis
- B. Acceleration-deceleration forces (Correct Answer)
- C. Birth trauma
- D. Genetic coagulopathy
- E. Direct impact trauma
Child abuse evaluation Explanation: ***Acceleration-deceleration forces***
- **Bilateral subdural hematomas of different ages** and **retinal hemorrhages** are classic findings in **abusive head trauma (shaken baby syndrome)**, caused by severe acceleration-deceleration forces.
- These forces lead to the tearing of **bridging veins** and vitreoretinal traction, resulting in these distinct injuries.
*Infectious meningitis*
- While it can cause seizures, meningitis typically presents with **fever**, **lethargy**, and neck stiffness, and would not cause **subdural hematomas** or **retinal hemorrhages**.
- Its effects on the brain are usually due to inflammation and increased intracranial pressure, not traumatic injury.
*Birth trauma*
- **Birth trauma** might cause subdural hematomas, but they would typically be **acute** and of a **single age**, directly related to the birthing process.
- It is highly unlikely to cause hematomas of "different ages" in a 4-month-old infant, nor would it characteristically cause retinal hemorrhages without other signs of severe, acute trauma.
*Genetic coagulopathy*
- A **genetic coagulopathy** could predispose to bleeding, but it would typically result in more widespread or spontaneous internal bleeding, not specifically **bilateral subdural hematomas** accompanied by **retinal hemorrhages** without other trauma.
- The "different ages" of the hematomas also strongly suggest recurrent episodes of trauma rather than an underlying bleeding disorder.
Child abuse evaluation US Medical PG Question 4: A 7-year-old boy is brought to the emergency department by his mother 1 hour after falling off his bike and landing head-first on the pavement. His mother says that he did not lose consciousness but has been agitated and complaining about a headache since the event. He has no history of serious illness and takes no medications. His temperature is 37.1°C (98.7°F), pulse is 115/min, respirations are 20/min, and blood pressure is 100/65 mm Hg. There is a large bruise on the anterior scalp. Examination, including neurologic examination, shows no other abnormalities. A noncontrast CT scan of the head shows a non-depressed linear skull fracture with a 2-mm separation. Which of the following is the most appropriate next step in management?
- A. Inpatient observation (Correct Answer)
- B. Contact child protective services
- C. CT angiography
- D. Discharge home
- E. MRI of the brain
Child abuse evaluation Explanation: ***Inpatient observation***
- A **nondepressed linear skull fracture** with mild separation and persistent symptoms (headache, agitation) after head trauma warrants **inpatient observation**.
- This allows for close neurological monitoring for potential complications like **intracranial hemorrhage** or worsening of symptoms.
*Contact child protective services*
- The history of falling off a bike, a visible bruise, and a fracture consistent with trauma does not suggest **child abuse**.
- There are no other suspicious signs or inconsistencies in the mother's account to raise immediate concerns about neglect or abuse.
*CT angiography*
- **CT angiography** is used to evaluate the cerebral vasculature and is not indicated in this case, as there is no evidence of vascular injury or dissection.
- The primary concern here is the potential for **intracranial bleeding** or evolving neurological compromise, which is best monitored with serial neurological exams and potentially repeat noncontrast CT scans.
*Discharge home*
- The presence of a **skull fracture**, even if linear and nondepressed, combined with persistent symptoms like headache and agitation makes immediate discharge home unsafe.
- There is an increased risk of **epidural hematoma** or other delayed complications that require professional medical monitoring.
*MRI of the brain*
- **MRI** is more sensitive for detecting subtle brain parenchymal injuries but is not the initial or primary imaging modality for acute head trauma, especially in a child who may require sedation.
- An **MRI** would be considered if there were persistent or evolving neurological deficits despite a normal or stable CT scan, or if there is concern for specific soft tissue or white matter injuries that CT cannot adequately assess.
Child abuse evaluation US Medical PG Question 5: A 3-month-old boy is brought to the emergency department by his mom for breathing difficulty after a recent fall. His parents say that he rolled off of the mattress and landed on the hard wood floor earlier today. After an extensive physical exam, he is found to have many purplish bruises and retinal hemorrhages. A non-contrast head CT scan shows a subdural hemorrhage. He was treated in the hospital with full recovery from his symptoms. Which of the following is the most important follow up plan?
- A. Provide parents with anticipatory guidance
- B. Referral to genetics for further testing
- C. Reassurance that accidents are common
- D. Inform child protective services (Correct Answer)
- E. Provide home nursing visits
Child abuse evaluation Explanation: ***Inform child protective services***
- The combination of **multiple purplish bruises**, **retinal hemorrhages**, and **subdural hemorrhage** in a 3-month-old infant after a minor fall (rolling off a mattress) is highly suggestive of **abusive head trauma** (shaken baby syndrome).
- Healthcare professionals have a **legal and ethical obligation** to report suspected child abuse to Child Protective Services (CPS) to ensure the child's safety and initiate an investigation.
*Provide parents with anticipatory guidance*
- While anticipatory guidance on child safety and development is generally important, it is **insufficient and inappropriate** as the primary follow-up in a case of suspected child abuse.
- Focusing solely on guidance would **neglect the immediate safety concerns** and the need for investigation into the injuries.
*Referral to genetics for further testing*
- While some genetic conditions can predispose to easy bruising or bleeding, the specific pattern of injuries (**retinal hemorrhages, subdural hemorrhage, multiple bruises, and a history inconsistent with the severity of injuries**) overwhelmingly points to trauma, not a genetic disorder.
- Genetic testing would be a secondary consideration, if at all, after abuse has been ruled out or addressed.
*Reassurance that accidents are common*
- Reassuring parents that "accidents are common" would be **medically negligent and dangerous** in this scenario, as the injuries sustained are typically not caused by a simple fall from a mattress in an infant of this age.
- This response would dismiss critical signs of potential abuse and leave the child at risk.
*Provide home nursing visits*
- Home nursing visits might be beneficial for monitoring general health and development, but they do **not address the immediate and grave concern** of potential child abuse.
- The primary need is for an investigation into the cause of the injuries and protection for the child, which falls under the purview of CPS.
Child abuse evaluation US Medical PG Question 6: A 6-month-old boy is brought to the emergency department by his mother, who informs the doctor that her alcoholic husband hit the boy hard on his back. The blow was followed by excessive crying for several minutes and the development of redness in the area. On physical examination, the boy is dehydrated, dirty, and irritable and when the vital signs are checked, they reveal tachycardia. He cries immediately upon the physician touching the area around his left scapula. The doctor strongly suspects a fracture of the 6th, 7th, or 8th retroscapular posterior ribs. Evaluation of his skeletal survey is normal. The clinician is concerned about child abuse in this case. Which of the following is the most preferred imaging technique as the next step in the diagnostic evaluation of the infant?
- A. Bedside ultrasonography
- B. Magnetic resonance imaging
- C. Babygram
- D. Chest computed tomography scan
- E. Skeletal survey in 2 weeks (Correct Answer)
Child abuse evaluation Explanation: ***Skeletal survey in 2 weeks***
- A repeat **skeletal survey in 2 weeks** is the most appropriate next step in suspected child abuse cases with an initial normal survey, as it allows for the detection of **healing fractures** that may not be apparent immediately after injury.
- New bone formation and callus development around a fracture site become radiographically visible after approximately 7 to 14 days, improving the detection rate of subtle or undisplaced fractures.
*Bedside ultrasonography*
- While **ultrasonography** can detect acute fractures, especially in cartilage and non-ossified bones, its utility in a comprehensive assessment for multiple non-displaced rib fractures as part of a child abuse workup is limited.
- It is highly **operator-dependent** and may not provide the full skeletal overview required in suspected child abuse.
*Magnetic resonance imaging*
- **MRI** is excellent for evaluating soft tissue injuries, bone marrow edema, and non-ossified cartilaginous structures. However, it is not the primary imaging modality for detecting acute or subacute fractures of ossified bone and requires **sedation** in infants, making it less practical for routine skeletal screening.
- The **high cost** and limited availability of MRI also make it less suitable as a first-line diagnostic tool for rib fractures in this context.
*Babygram*
- A **babygram** is a single large radiograph of an infant's entire body, often used to rapidly assess for gross developmental anomalies or immediate concerns.
- It provides **less detailed imaging** of individual bones compared to a standard skeletal survey and is insufficient for reliably detecting subtle or non-displaced rib fractures.
*Chest computed tomography scan*
- A **chest CT scan** is highly sensitive for detecting acute rib fractures, even subtle ones. However, it exposes the infant to **significant radiation** and is usually reserved for specific clinical indications, such as suspected internal organ injury, rather than as a primary screening tool for rib fractures in child abuse in an otherwise stable patient.
- It does not provide a comprehensive view of the entire skeleton, which is crucial for identifying other potential abuse-related injuries elsewhere.
Child abuse evaluation US Medical PG Question 7: A 7-month-old boy is brought to the emergency department by his mother because of a 3-day history of vomiting and poor feeding. The vomit is non-bloody. He transitioned to pureed vegetables 10 days ago. Over the past 2 weeks, he has become increasingly irritable and within the past day has taken more daytime naps and appears much less responsive and interactive. His mother denies any history of fever or trauma at home. He has not received any vaccinations as his parents believe he is already healthy and does not need them. He spends most of the day with a babysitter while both parents are at work. He appears lethargic. His temperature is 37.8°C (100.1°F), pulse is 140/min, respirations are 18/min, and blood pressure is 90/55 mm Hg. The abdomen is soft and nontender. Auscultation of the heart and lungs shows no abnormalities. The anterior fontanelle is tense and bulging. Fundoscopic exam shows bilateral retinal hemorrhage. A complete blood count shows a leukocyte count of 10,000/mm3. An x-ray of the chest shows healing fractures of the 2nd and 3rd right ribs. Further evaluation of this patient is most likely to show which of the following findings?
- A. Vitamin deficiency
- B. Type I collagen synthesis defect
- C. Diffuse axonal damage (Correct Answer)
- D. Bacterial infection
- E. Mass in the posterior fossa
Child abuse evaluation Explanation: ***Diffuse axonal damage***
- The combination of **lethargy**, vomiting, **bulging fontanelle**, and **retinal hemorrhages** in an infant, especially with unexplained healing fractures, is highly suggestive of **abusive head trauma (shaken baby syndrome)**.
- Diffuse axonal injury (DAI) is a common and severe consequence of abusive head trauma due to the shearing forces from acceleration-deceleration movements, leading to widespread brain damage.
*Vitamin deficiency*
- While vitamin deficiencies can cause various neurological symptoms, they typically do not present with the acute constellation of **retinal hemorrhages**, **bulging fontanelle**, and **healing fractures** seen in this case.
- The symptoms are more indicative of acute injury rather than chronic nutritional deficit.
*Type I collagen synthesis defect*
- This description is characteristic of **osteogenesis imperfecta**, a genetic disorder causing **brittle bones** and frequent fractures, but it does not account for the **retinal hemorrhages** or the **acute neurological symptoms** like a bulging fontanelle.
- The history of gradual neurological decline (irritability, lethargy) and acute intracranial signs are not typical for a collagen defect.
*Bacterial infection*
- While **bacterial meningitis** can cause fever, lethargy, vomiting, and a **bulging fontanelle**, it typically presents with a higher fever, possible neck stiffness, and often a higher **leukocyte count** with left shift.
- The presence of **retinal hemorrhages** and **healing bone fractures** makes infection a less likely primary explanation for all findings.
*Mass in the posterior fossa*
- A posterior fossa mass could explain the vomiting and bulging fontanelle due to increased intracranial pressure, but it would not typically cause **bilateral retinal hemorrhages** or **healing fractures** in the absence of trauma.
- The rapid onset of severe neurological symptoms along with the other signs points away from a slowly growing mass.
Child abuse evaluation US Medical PG Question 8: A 9-month-old male infant is brought to his pediatrician by his mother with lethargy and decreased oral intake for one day. His mother also mentions that he did not sleep well the previous night. A review of the medical record reveals several missed appointments and that the boy was born at 36 weeks gestation via spontaneous vaginal delivery. At the clinic, his temperature is 37.2ºC (99.0ºF), pulse rate is 140/minute, respirations are 44/minute, and blood pressure is 92/60 mm Hg. On physical exam the infant is awake but irritable and the rest of the physical is within normal limits for his age. On ophthalmologic examination, there are multiple retinal hemorrhages that extend to the periphery in both eyes. Which of the following investigations is most likely to be helpful in the management of the infant?
- A. Bone marrow aspiration
- B. Peripheral blood smear
- C. Lumbar puncture
- D. Hemoglobin electrophoresis
- E. Noncontrast computed tomography of head (Correct Answer)
Child abuse evaluation Explanation: ***Noncontrast computed tomography of head***
- The combination of **lethargy**, decreased oral intake, irritability, and **bilateral retinal hemorrhages** in an infant strongly suggests **abusive head trauma (shaken baby syndrome)**, requiring urgent neuroimaging to assess for intracranial hemorrhage.
- A **noncontrast CT of the head** is the immediate and most appropriate investigation to identify acute intracranial bleeds, such as subdural or subarachnoid hemorrhages, which are common in abusive head trauma.
*Bone marrow aspiration*
- This procedure is primarily used to diagnose **hematologic malignancies** (e.g., leukemia) or certain storage disorders.
- It is not indicated as a first-line investigation for lethargy and retinal hemorrhages, as these symptoms do not specifically point to a bone marrow pathology.
*Peripheral blood smear*
- A peripheral blood smear is useful for evaluating **anemia**, **thrombocytopenia**, or abnormal cells in the circulation.
- While it can help assess for underlying blood disorders, it will not directly diagnose or localize the cause of the suspected intracranial injury.
*Lumbar puncture*
- A lumbar puncture is used to analyze **cerebrospinal fluid (CSF)**, primarily to diagnose infections like meningitis or encephalitis, or certain inflammatory conditions.
- Performing a lumbar puncture in suspected abusive head trauma can be dangerous if there is significant intracranial pressure or a mass lesion, making neuroimaging a necessary prerequisite.
*Hemoglobin electrophoresis*
- This test is used to detect **hemoglobinopathies** like sickle cell disease or thalassemia.
- While useful in specific contexts, there are no symptoms or signs in this case to suggest a hemoglobin disorder.
Child abuse evaluation US Medical PG Question 9: A 3-year-old girl is brought to the physician by her mother two days after the sudden onset of a rash. The mother says that the rash developed an hour after she bathed the child in hot water. Two weeks ago, the patient was diagnosed with a skin infection and was treated with penicillin V. She has been otherwise healthy but has missed several well-child examinations. She lives with her single mother, who recently lost her job and is now dependent on social assistance. The patient's mother has major depressive disorder and her maternal aunt has systemic lupus erythematosus. The girl's temperature is 36.8°C (98.2°F), pulse is 112/min, and blood pressure is 108/62 mm Hg. She has poor eye contact. Physical examination shows sharply delineated erythema on the lower extremities up to the umbilicus with sparing of the knees and flexor surfaces. Further evaluation is most likely to reveal which of the following?
- A. Dermatographism
- B. Multiple injuries in different stages of healing (Correct Answer)
- C. Ulcers of the oral mucosa
- D. Malar rash with sparing of the nasolabial folds
- E. Positive Nikolsky's sign
Child abuse evaluation Explanation: ***Multiple injuries in different stages of healing***
- This scenario strongly suggests **child abuse**. The "rash" described is suspicious; it is a **sharply delineated erythema** on the lower extremities up to the umbilicus with sparing of the knees and flexor surfaces, appearing after a hot bath. This pattern is classic for a **scald injury**, which would be considered abuse if inflicted by hot water.
- The mother's claim of a sudden rash occurring an hour after a hot bath makes a thermal injury more likely, especially given her recent job loss, dependence on social assistance, and major depressive disorder, all of which are **risk factors for child abuse**. The child's poor eye contact also raises concerns.
*Dermatographism*
- **Dermatographism** is a form of urticaria where strokes or pressure on the skin cause raised, red lines.
- This condition presents as transient wheals and would not align with the described **sharply delineated erythema** in a specific distribution, nor would it be triggered only by a hot bath in this manner.
*Ulcers of the oral mucosa*
- **Oral ulcers** are common in various systemic conditions (e.g., aphthous stomatitis, viral infections, lupus) but are not directly suggested by a sudden onset of skin erythema after a hot bath.
- While some forms of abuse might involve oral injury, the described skin rash is not a typical presentation or associated finding that would lead one to specifically look for oral ulcers.
*Malar rash with sparing of the nasolabial folds*
- A **malar rash** (butterfly rash) is characteristic of **systemic lupus erythematosus (SLE)**, which the patient's maternal aunt has. However, this rash typically affects the cheeks and bridge of the nose.
- The patient's rash is described as **sharply delineated erythema** on the lower extremities up to the umbilicus, with sparing of specific areas, which is inconsistent with the distribution and appearance of a malar rash.
*Positive Nikolsky's sign*
- **Nikolsky's sign** involves the epidermal detachment upon light friction, indicative of blistering disorders like **pemphigus vulgaris** or **staphylococcal scalded skin syndrome (SSSS)**.
- While SSSS can cause widespread erythema and skin peeling, the description of **sharply delineated erythema** on specific body parts after a hot bath is more consistent with a thermal injury than the diffuse blistering and epidermal sloughing seen in SSSS.
Child abuse evaluation US Medical PG Question 10: A 5-year-old non-verbal child with a history of autism is brought into the emergency department by his grandmother. The patient’s grandmother is concerned her grandchild is being abused at home. The patient lives in an apartment with his mother, step-father, and two older brothers in low-income housing. The department of social services has an open case regarding this patient and his family. The patient is afebrile. His vital signs include: blood pressure 97/62 mm Hg, pulse 175/min, respiratory rate 62/min. Physical examination reveals a malnourished and dehydrated child in dirty and foul-smelling clothes. Which one of the following people is most likely abusing this patient?
- A. Mother (Correct Answer)
- B. Neighbor
- C. Brother
- D. Stranger
- E. Step-father
Child abuse evaluation Explanation: ***Mother***
- **Child abuse** is complex, but the **mother (or primary caregiver)** is often the abuser, especially in cases where the child is non-verbal and has a disability.
- The child's **malnutrition and poor hygiene** point to neglect, which is a form of abuse, and the primary caregiver is responsible for the child's basic needs.
*Neighbor*
- While abuse can occur outside the home, a **neighbor is highly unlikely** to be responsible for the child's chronic neglect, malnutrition, and dehydration, given the living circumstances described.
- **Neighbors typically do not have consistent, unsupervised access** to a child in a manner that would lead to such severe and ongoing neglect.
*Brother*
- Although **siblings can be perpetrators of abuse**, particularly physical or sexual abuse, it is **uncommon for siblings to be responsible for severe neglect** leading to malnutrition and chronic poor hygiene in a younger child.
- This kind of chronic neglect usually points to a **primary caregiver's failure** to provide basic needs.
*Stranger*
- Abuse by a **stranger is relatively rare** compared to abuse by a family member or acquaintance.
- The consistent pattern of **neglect, malnutrition, and poor hygiene** suggests ongoing failure of care within the home environment, not a single or intermittent encounter with a stranger.
*Step-father*
- A **step-father is a recognized risk factor for child abuse**, and he could certainly be involved, especially given the child's vulnerability.
- However, in cases of **chronic neglect and failure to provide basic care**, the primary responsibility often lies with the **biological parent** who is also a co-resident caregiver.
More Child abuse evaluation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.