Vitamin D deficiency and rickets US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vitamin D deficiency and rickets. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vitamin D deficiency and rickets US Medical PG Question 1: A 67-year-old male presents to his primary care physician complaining of left hip pain for the past six months. He denies any trauma or recent falls. He is accompanied by his wife who reports that he has experienced progressive hearing loss over the same time period. The patient has also noticed that he is no longer able to fit into his favorite hat even though it previously fit well. A radiograph of the patient’s pelvis is shown. Which of the following laboratory abnormalities is most likely to be found in this patient?
- A. Elevated serum calcium
- B. Decreased serum alkaline phosphatase
- C. Decreased serum calcium
- D. Elevated serum parathyroid hormone
- E. Elevated serum alkaline phosphatase (Correct Answer)
Vitamin D deficiency and rickets Explanation: ***Elevated serum alkaline phosphatase***
- The patient's symptoms (hip pain, progressive hearing loss, increased hat size) suggest **Paget's disease of bone**, which is characterized by accelerated bone turnover.
- **Alkaline phosphatase** is an enzyme produced by osteoblasts, and its elevation in serum is a hallmark of increased bone formation and remodeling seen in Paget's disease.
*Elevated serum calcium*
- In uncomplicated Paget's disease, serum calcium levels are typically **normal**, as the increased bone turnover usually maintains a balance between resorption and formation.
- Hypercalcemia in Paget's disease is rare and may occur in cases of **immobility** or concomitant primary hyperparathyroidism.
*Decreased serum alkaline phosphatase*
- This would indicate reduced osteoblastic activity or bone formation, which is the opposite of the accelerated bone remodeling seen in **Paget's disease**.
- Conditions like **hypophosphatasia** or severe malnutrition might lead to decreased alkaline phosphatase.
*Decreased serum calcium*
- Hypocalcemia is not a typical feature of Paget's disease unless there are other contributing factors such as **malabsorption** or **renal failure**.
- Bone turnover in Paget's disease usually maintains normal serum calcium levels through coupled osteoclastic and osteoblastic activity.
*Elevated serum parathyroid hormone*
- While **elevated parathyroid hormone** can cause increased bone turnover, it primarily does so by increasing osteoclastic activity to release calcium from bone, leading to hypercalcemia.
- In Paget's disease, **parathyroid hormone levels are typically normal** unless there is co-existing primary hyperparathyroidism.
Vitamin D deficiency and rickets US Medical PG Question 2: A 70-year-old woman presents to the office for a yearly physical. She states she has recently started experiencing pain in her legs and her back. Last year, she experienced a fracture of her left arm while trying to lift groceries. The patient states that she does not consume any dairy and does not go outside often because of the pain in her legs and back. Of note, she takes carbamazepine for seizures. On exam, her vitals are within normal limits. You suspect the patient might have osteomalacia. Testing for which of the following is the next best step to confirm your suspicion?
- A. Vitamin D2 (ergocalciferol)
- B. 25-hydroxyvitamin D (Correct Answer)
- C. Pre-vitamin D3
- D. 1,25-hydroxyvitamin D
- E. 7-dehydrocholesterol
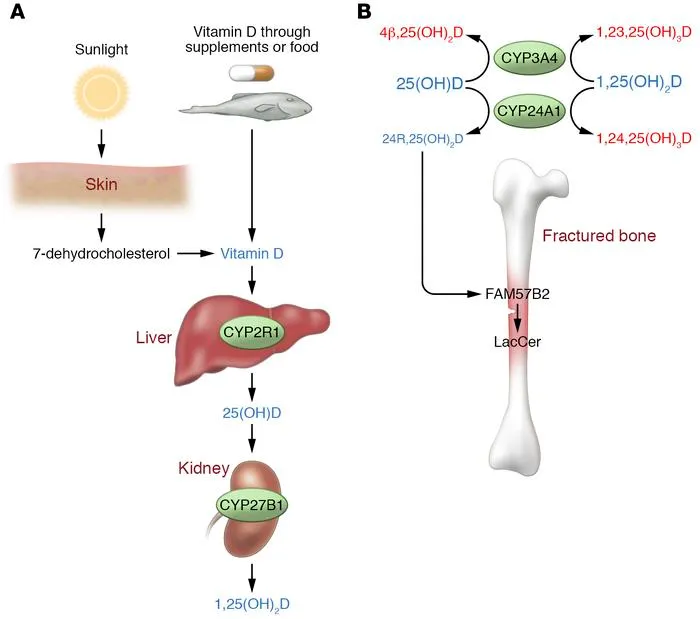
Vitamin D deficiency and rickets Explanation: ***25-hydroxyvitamin D***
- This is the **best initial test** for evaluating vitamin D deficiency, which leads to **osteomalacia**.
- It reflects the circulating levels of vitamin D and is the **most accurate indicator** of the body's vitamin D stores.
*Vitamin D2 (ergocalciferol)*
- While D2 is a form of vitamin D, measuring only D2 levels is **not sufficient** to assess overall vitamin D status.
- The standard test measures total circulating vitamin D, which includes both D2 and D3, but specifically **25-hydroxyvitamin D** reflects the active usable form.
*Pre-vitamin D3*
- **Pre-vitamin D3** is a precursor molecule formed in the skin from 7-dehydrocholesterol upon UV exposure, and it rapidly isomerizes to vitamin D3.
- It is **not a stable measurable form** in the blood for assessing vitamin D status or diagnosing osteomalacia.
*1,25-hydroxyvitamin D*
- This is the **active hormonal form of vitamin D**, primarily regulated by parathyroid hormone (PTH) and kidney function.
- Levels can be normal or even elevated in early vitamin D deficiency due to increased PTH, making it **less reliable** for initial assessment of deficiency.
*7-dehydrocholesterol*
- **7-dehydrocholesterol** is a precursor molecule in the skin that is converted to pre-vitamin D3 by UV radiation.
- Measuring this precursor is **not clinically significant** for diagnosing osteomalacia or assessing vitamin D deficiency.
Vitamin D deficiency and rickets US Medical PG Question 3: A 57-year-old man presents the urgent care clinic with a one-week history of diffuse bone pain and generalized weakness. He was diagnosed with end-stage renal disease 6 months ago and is currently on dialysis. His wife, who is accompanying him today, adds that he is not compliant with his medicines. He has been diabetic for the last 10 years and hypertensive for the last 7 years. He has smoked 4–5 cigarettes per day for 30 years but does not drink alcohol. His family history is insignificant. On examination, the patient has a waddling gait. Hypotonia of all the limbs is evident on neurologic examination. Diffuse bone tenderness is remarkable. X-ray of his legs reveal osteopenia and osseous resorption. The final step of activation of the deficient vitamin in this patient occurs by which of the following enzymes?
- A. α-1-antitrypsin
- B. 24,25 hydroxylase
- C. α-Glucosidase
- D. 7-α-hydroxylase
- E. 1-α-hydroxylase (Correct Answer)
Vitamin D deficiency and rickets Explanation: ***1-α-hydroxylase***
- The patient's symptoms (diffuse bone pain, generalized weakness, waddling gait, hypotonia, osteopenia, and osseous resorption) in the context of **end-stage renal disease (ESRD)** and non-compliance strongly suggest **renal osteodystrophy**, specifically **osteomalacia** due to impaired vitamin D activation.
- In ESRD, the kidneys are unable to produce sufficient amounts of **calcitriol (1,25-dihydroxyvitamin D)**, which is the active form of vitamin D. The enzyme responsible for the final activation step, converting 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D, is **1-α-hydroxylase**, primarily located in the renal proximal tubules.
*α-1-antitrypsin*
- This enzyme is a **serine protease inhibitor** primarily involved in protecting tissues from damage by proteases, especially in the lungs.
- Deficiency is associated with conditions like **emphysema** and **liver disease**, not directly with bone metabolism or vitamin D activation.
*24,25 hydroxylase*
- The enzyme **24-hydroxylase** inactivates calcitriol and its precursor by converting them into inert forms.
- Its activity would lead to reduced active vitamin D, mimicking a deficiency, but it is not the enzyme responsible for the **final activation step** of vitamin D.
*α-Glucosidase*
- This enzyme is crucial for the digestion of **carbohydrates** in the small intestine, breaking down complex sugars into glucose.
- Deficiencies are associated with conditions like **Pompe disease (glycogen storage disease type II)**, which primarily affects muscle and liver, not vitamin D metabolism.
*7-α-hydroxylase*
- **Cholesterol 7-α-hydroxylase (CYP7A1)** is a rate-limiting enzyme in the **bile acid synthesis pathway** in the liver.
- It plays no direct role in the activation of vitamin D; its function is related to cholesterol metabolism and bile production.
Vitamin D deficiency and rickets US Medical PG Question 4: A 6-year-old boy is brought to the physician for a well-child examination. His mother has noticed he frequently falls while running. He was born at term and pregnancy was uncomplicated. He has a seizure disorder treated with phenytoin. He is at the 20th percentile for height and at 30th percentile for weight. Vital signs are within normal limits. Examination shows decreased muscle strength in the lower extremities. There is a deep groove below the costal margins bilaterally. An x-ray of the lower extremities is shown. Which of the following is the most likely cause of these findings?
- A. Proximal tibial growth plate disruption
- B. Metabolic abnormality (Correct Answer)
- C. Normal development
- D. Heavy metal toxicity
- E. Neoplastic growth
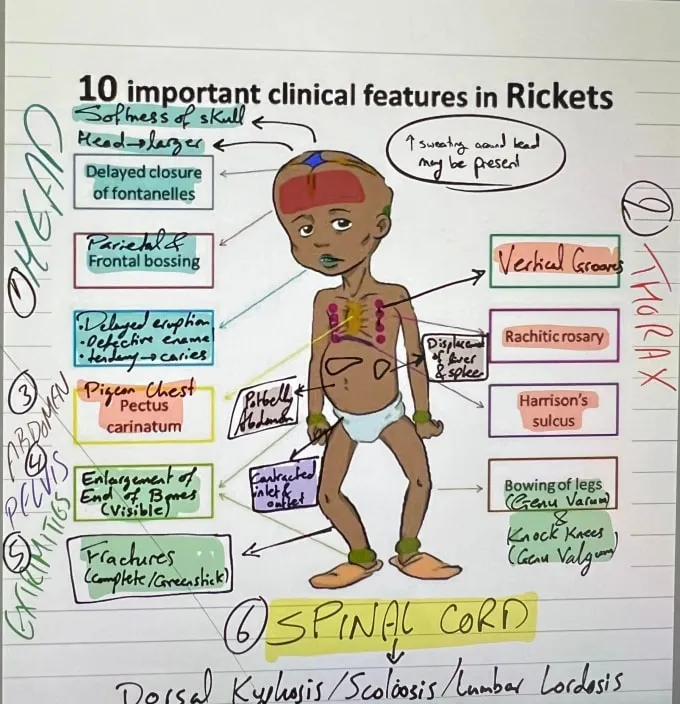
Vitamin D deficiency and rickets Explanation: **Metabolic abnormality**
- The combination of **frequent falls**, **decreased lower extremity strength**, **rachitic rosary** (deep groove below costal margins indicating enlarged costochondral junctions), and **skeletal abnormalities on X-ray** (likely showing widened growth plates and metaphyseal cupping/fraying) strongly suggests a metabolic bone disorder like rickets.
- **Phenytoin use** can interfere with **vitamin D metabolism**, further predisposing to rickets by increasing its catabolism and decreasing calcium absorption.
*Proximal tibial growth plate disruption*
- While falls could potentially cause growth plate injuries, the systemic signs like **rachitic rosary** and general weakness point away from an isolated traumatic injury.
- Growth plate disruption would typically present with acute pain, swelling, and localized tenderness, rather than widespread skeletal and muscle weakness.
*Normal development*
- **Frequent falling** at 6 years old, combined with **decreased muscle strength** and an anatomical finding like a **rachitic rosary**, are not consistent with normal development.
- Normal growth and development in this age group would include improved coordination and muscle strength, not regression or signs of skeletal abnormalities.
*Heavy metal toxicity*
- Heavy metal toxicity (e.g., lead) can cause developmental problems and neurological symptoms, but it typically does not manifest with a **rachitic rosary** or the specific skeletal changes seen in rickets on X-ray.
- Lead poisoning, for example, is associated with **lead lines** in the metaphyses, which are distinct from the changes seen in rickets.
*Neoplastic growth*
- Neoplastic growth, especially bone tumors, could cause localized pain and weakness, but it would not typically present with the diffuse muscle weakness, **rachitic rosary**, and characteristic X-ray findings of rickets.
- Malignancies would generally show lytic or blastic lesions on X-ray and often systemic symptoms like weight loss or night sweats, which are not described here.
Vitamin D deficiency and rickets US Medical PG Question 5: A 67-year-old Caucasian female presents to her primary care physician after a screening DEXA scan reveals a T-score of -3.0. Laboratory work-up reveals normal serum calcium, phosphate, vitamin D, and PTH levels. She smokes 1-2 cigarettes per day. Which of the following measures would have reduced this patient's risk of developing osteoporosis?
- A. Weight loss
- B. Reduced physical activity to decrease the chance of a fall
- C. Initiating a swimming exercise program three days per week
- D. Calcium and vitamin D supplementation
- E. Smoking cessation (Correct Answer)
Vitamin D deficiency and rickets Explanation: ***Smoking cessation***
- **Smoking** is a well-established, modifiable risk factor for osteoporosis that directly impairs bone metabolism
- Cigarette smoking **decreases osteoblast activity**, increases **bone resorption**, and reduces intestinal calcium absorption
- This patient is **actively smoking 1-2 cigarettes per day**, making cessation the most relevant preventive measure for her specific situation
- **Smoking cessation** would have directly addressed a harmful exposure that contributed to her bone loss
*Calcium and vitamin D supplementation*
- While important for bone health, this patient's laboratory work-up shows **normal serum calcium and vitamin D levels**
- Supplementation beyond adequate levels has **limited additional benefit** for osteoporosis prevention in patients with normal baseline values
- Supplementation is most beneficial in patients with documented **deficiency** or inadequate dietary intake
*Weight loss*
- **Weight loss** and being underweight are actually **risk factors for osteoporosis**
- Lower body weight reduces mechanical loading on bones, which is necessary for maintaining bone density
- Weight-bearing stress stimulates bone formation through mechanotransduction
*Initiating a swimming exercise program three days per week*
- While **swimming** is excellent for cardiovascular fitness and overall health, it is **not a weight-bearing exercise**
- Osteoporosis prevention requires **weight-bearing or resistance exercises** such as walking, jogging, dancing, or strength training
- These activities provide the mechanical stress needed to stimulate bone formation
*Reduced physical activity to decrease the chance of a fall*
- **Reducing physical activity** accelerates bone loss due to decreased mechanical loading
- While fall prevention is important in osteoporosis management, it should focus on **environmental modifications** and **balance training**, not activity reduction
- Maintaining appropriate physical activity is essential for preserving bone density
Vitamin D deficiency and rickets US Medical PG Question 6: A 6-month-old girl is brought to the physician for a well-child examination. She was born at 37 weeks' gestation. Pregnancy and the neonatal period were uncomplicated. The infant was exclusively breastfed and received vitamin D supplementation. She can sit unsupported and can transfer objects from one hand to the other. She babbles and is uncomfortable around strangers. She is at 40th percentile for length and at 35th percentile for weight. Vital signs are within normal limits. Physical examination shows no abnormalities. In addition to continuing breastfeeding, which of the following is the most appropriate recommendation at this time?
- A. Continue vitamin D
- B. Introduce solid foods
- C. Introduce solid foods and add vitamin C
- D. Introduce solid foods and cow milk
- E. Introduce solid foods and continue vitamin D (Correct Answer)
Vitamin D deficiency and rickets Explanation: ***Introduce solid foods and continue vitamin D***
- At **6 months of age**, infants typically show developmental readiness for **solid foods**, such as the ability to sit unsupported and transfer objects, while **breastfeeding** continues to be important.
- **Vitamin D supplementation** should continue as it is crucial for bone health and is not adequately supplied by breast milk or early solid foods alone.
*Continue vitamin D*
- While vitamin D supplementation is important, this option **misses the crucial developmental milestone** of introducing solid foods at 6 months.
- At this age, infants' **iron stores** begin to dwindle, and solid foods are needed to provide essential nutrients not sufficiently met by breast milk alone.
*Introduce solid foods*
- This option correctly identifies the need to introduce solid foods but **fails to mention the continued importance of vitamin D supplementation**.
- Breastfed infants require continued **vitamin D supplementation** to prevent **rickets**, as breast milk does not contain sufficient amounts.
*Introduce solid foods and add vitamin C*
- While **vitamin C** is important, the primary focus at 6 months should be on **iron-rich solid foods** and continued **vitamin D supplementation**.
- Breast milk contains adequate vitamin C, and introducing diverse solid foods typically provides enough, making dedicated vitamin C supplementation usually unnecessary unless a deficiency is identified.
*Introduce solid food and cow milk*
- **Cow's milk** should **not be introduced** as a primary drink before **12 months of age** because it can cause **gastrointestinal bleeding**, **iron-deficiency anemia**, and is difficult for infants to digest.
- Introducing cow's milk too early can also interfere with the absorption of essential nutrients from breast milk or formula.
Vitamin D deficiency and rickets US Medical PG Question 7: A 28-year-old gravida 1 para 1 woman is being seen in the hospital for breast tenderness. She reports that both breasts are swollen and tender. She is also having difficulty getting her newborn to latch. The patient gave birth 4 days ago by uncomplicated vaginal delivery. During her pregnancy, the patient developed gestational diabetes but was otherwise healthy. She took folate and insulin. She attended all her pre-natal appointments. Upon examination, the patient has a low grade fever, but all other vital signs are stable. Bilateral breasts appear engorged and are tender to palpation. There is no erythema, warmth, or induration. A lactation nurse is brought in to assist the patient and her newborn with more effective breastfeeding positions. The patient says a neighbor told her that breastmilk actually lacks in nutrients, and she asks what the best option is for the health of her newborn. Which of the following components is breastmilk a poor source of?
- A. Whey protein
- B. Vitamin D (Correct Answer)
- C. Lysozymes
- D. Phosphorus
- E. Immunoglobulin A
Vitamin D deficiency and rickets Explanation: ***Vitamin D***
- **Breast milk** is naturally a **poor source of vitamin D**, making supplementation necessary for breastfed infants to prevent **rickets** and ensure adequate bone development.
- While small amounts of vitamin D are present, they are often insufficient to meet the infant's requirements, especially if maternal vitamin D levels are also low.
*Whey protein*
- **Whey protein** is a major component of breast milk, contributing to its digestibility and providing essential **amino acids** for infant growth.
- It is specifically rich in **alpha-lactalbumin**, which has both nutritional and antimicrobial properties.
*Lysozymes*
- **Lysozymes** are abundant in breast milk and play a crucial role in the infant's innate **immune defense** by breaking down bacterial cell walls.
- These enzymes help protect against gastrointestinal infections and contribute to the establishment of healthy gut flora.
*Phosphorus*
- **Phosphorus** is an essential mineral found in sufficient quantities in **breast milk**, crucial for **bone mineralization**, energy metabolism, and cell function.
- Its concentration is carefully regulated to meet the needs of the growing infant without overloading immature kidneys.
*Immunoglobulin A*
- **Secretory IgA (sIgA)** is the predominant **immunoglobulin** in breast milk, providing passive immunity by coating the infant's intestinal tract and preventing pathogen attachment.
- It is crucial for protecting the infant from various infections, especially those affecting the gastrointestinal and respiratory systems.
Vitamin D deficiency and rickets US Medical PG Question 8: A 3-month-old African American boy presents to his pediatrician’s office for his routine well visit. He was born full-term from an uncomplicated vaginal delivery. He is exclusively breastfeeding and not receiving any medications or supplements. Today, his parents report no issues or concerns with their child. He is lifting his head for brief periods and smiling. He has received only 2 hepatitis B vaccines. Which of the following is the correct advice for this patient’s parents?
- A. He should be sleeping more.
- B. He should have his serum lead level checked to screen for lead intoxication.
- C. He should start vitamin D supplementation. (Correct Answer)
- D. He should start rice cereal.
- E. He needs a 3rd hepatitis B vaccine.
Vitamin D deficiency and rickets Explanation: ***He should start vitamin D supplementation.***
- **Exclusively breastfed** infants, regardless of maternal vitamin D intake, require **vitamin D supplementation** due to insufficient amounts in breast milk.
- The recommended daily dose is **400 IU** starting from the first few days of life, to prevent **rickets** and promote bone health.
- **African American infants** have an additional risk factor due to increased skin melanin content, which reduces cutaneous vitamin D synthesis from sunlight exposure.
*He should be sleeping more.*
- A 3-month-old infant typically sleeps between **14-17 hours per day**, with **waking periods to feed** and interact.
- The case description does not indicate any concerns with the child's sleep patterns, and **developmental milestones** like lifting his head and smiling are being met.
*He should have his serum lead level checked to screen for lead intoxication.*
- **Lead screening** is not routinely recommended for all infants unless specific **risk factors** are present, such as living in an older home with lead paint, or having siblings with elevated lead levels.
- There are no reported risk factors for lead exposure in this patient's history.
*He should start rice cereal.*
- Introduction of solid foods, such as rice cereal, is typically recommended around **6 months of age**, when the infant shows signs of **developmental readiness**.
- These signs include **head control**, sitting with support, and showing interest in food.
*He needs a 3rd hepatitis B vaccine.*
- The **third dose of the hepatitis B vaccine** is typically administered between **6 and 18 months of age**.
- At 3 months old, the infant is not yet due for his third dose.
Vitamin D deficiency and rickets US Medical PG Question 9: A 35-year-old female presents to her primary care physician complaining of right upper quadrant pain over the last 6 months. Pain is worst after eating and feels like intermittent squeezing. She also admits to lighter colored stools and a feeling of itchiness on her skin. Physical exam demonstrates a positive Murphy's sign. The vitamin level least likely to be affected by this condition is associated with which of the following deficiency syndromes?
- A. Rickets and osteomalacia
- B. Hemolytic anemia
- C. Night blindness
- D. Increased prothrombin time and easy bleeding
- E. Scurvy (Correct Answer)
Vitamin D deficiency and rickets Explanation: ***Scurvy***
- This condition is likely **cholestasis** due to common bile duct obstruction, given the RUQ pain after eating, light-colored stools, itchiness, and **positive Murphy's sign**.
- Cholestasis impairs the absorption of **fat-soluble vitamins** (A, D, E, K), but not **water-soluble vitamins** like vitamin C, which prevents scurvy.
*Rickets and osteomalacia*
- These conditions are caused by **vitamin D deficiency**, which is a **fat-soluble vitamin**.
- Impaired fat absorption in cholestasis would significantly impact vitamin D levels, leading to increased risk of rickets in children and osteomalacia in adults.
*Hemolytic anemia*
- This can be caused by **vitamin E deficiency**, a **fat-soluble vitamin**.
- Cholestasis impairs vitamin E absorption, which can lead to increased red blood cell fragility and hemolytic anemia.
*Night blindness*
- This is a classic symptom of **vitamin A deficiency**, which is a **fat-soluble vitamin**.
- Impaired fat absorption in cholestasis would reduce vitamin A uptake, contributing to night blindness.
*Increased prothrombin time and easy bleeding*
- These symptoms are indicative of **vitamin K deficiency**, a **fat-soluble vitamin**.
- Vitamin K is essential for the synthesis of clotting factors, and its absorption is severely hindered in cholestasis, leading to coagulopathies.
Vitamin D deficiency and rickets US Medical PG Question 10: A child presents with rachitic changes in the limbs that are not responding to Vitamin D supplementation. Investigations reveal the following results:
- Calcium: $9.5 \mathrm{mg} / \mathrm{dl}$
- Phosphorus: $1.6 \mathrm{mg} / \mathrm{dl}$
- Alkaline phosphatase (ALP): 814 IU
- Serum PTH: $24.2 \mathrm{pg} / \mathrm{ml}$
- Serum electrolytes, creatinine, and blood gases: Normal.
What is the most likely diagnosis?
- A. Hypophosphatemic rickets (Correct Answer)
- B. Vitamin D-dependent rickets type 2
- C. Vitamin D-dependent rickets type 1
- D. Chronic renal failure
- E. Vitamin D deficiency rickets
Vitamin D deficiency and rickets Explanation: ***Hypophosphatemic rickets***
- The combination of **rachitic changes** not responding to Vitamin D, **low serum phosphorus (1.6 mg/dl)**, and **normal calcium and PTH levels** strongly points to hypophosphatemic rickets, a condition characterized by impaired renal phosphate reabsorption.
- The **elevated alkaline phosphatase** indicates increased bone turnover as the body tries to mineralize bone despite phosphate deficiency.
*Vitamin D-dependent rickets type 2*
- This condition involves resistance to **1,25-dihydroxyvitamin D**, leading to **hypocalcemia** and elevated PTH, none of which are present here.
- It would also typically show an inadequate response to Vitamin D, but the primary biochemical derangement is different.
*Vitamin D-dependent rickets type 1*
- This type is caused by a defect in **1-alpha-hydroxylase**, leading to an inability to convert 25-hydroxyvitamin D to its active form, resulting in **hypocalcemia** and elevated PTH, which are not observed.
- It would also show a poor response to standard Vitamin D supplementation.
*Vitamin D deficiency rickets*
- This is the most common form of rickets caused by inadequate Vitamin D intake or synthesis, presenting with **hypocalcemia**, **elevated PTH**, and **low phosphorus**.
- However, it typically responds well to Vitamin D supplementation, unlike the presentation here, and would show elevated PTH levels.
*Chronic renal failure*
- Chronic renal failure would present with **elevated creatinine**, and typically leads to **secondary hyperparathyroidism** (elevated PTH), **hyperphosphatemia**, and metabolic acidosis, none of which are suggested by the provided lab results.
- The serum electrolytes, creatinine, and blood gases are explicitly stated as normal.
More Vitamin D deficiency and rickets US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.