Special diets in pediatric conditions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Special diets in pediatric conditions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Special diets in pediatric conditions US Medical PG Question 1: A 6-month-old boy is brought to the emergency department by his mother because of recurrent vomiting and yellowing of his eyes. The mother says that he has been eating poorly since she started weaning him off of breast milk 5 days ago. At this time, mashed vegetables and fruits were added to his diet. Examination shows scleral jaundice and dry mucous membranes. The tip of the liver is palpable 4 cm below the right costal margin. His serum glucose concentration is 47 mg/dL, serum alanine aminotransferase is 55 U/L, and serum aspartate aminotransferase is 66 U/L. Which of the following enzymes is most likely deficient?
- A. Fructokinase
- B. Glucose-6-phosphatase
- C. Galactokinase
- D. Galactose-1 phosphate uridyltransferase
- E. Aldolase B (Correct Answer)
Special diets in pediatric conditions Explanation: ***Aldolase B***
- The symptoms, including **jaundice**, vomiting, **hepatomegaly**, and **hypoglycemia** following the introduction of solid foods (specifically fruits and vegetables containing **fructose**), are classic for **hereditary fructose intolerance**.
- **Aldolase B** is crucial for metabolizing fructose in the liver; its deficiency leads to the buildup of **fructose-1-phosphate**, which is toxic to hepatocytes and inhibits glucose production.
*Fructokinase*
- Fructokinase deficiency causes **essential fructosuria**, a benign condition characterized by fructose in the urine, but without the severe metabolic disturbances like hypoglycemia and liver damage seen in this patient.
- This condition does not typically present with the **jaundice**, vomiting, and liver enlargement found in the given case.
*Glucose-6-phosphatase*
- A deficiency in **glucose-6-phosphatase** causes **Type I glycogen storage disease (Von Gierke disease)**, which presents with severe hypoglycemia and hepatomegaly.
- However, it does not typically cause the **jaundice** or acute symptoms triggered by the introduction of solid foods containing fructose as described in this case.
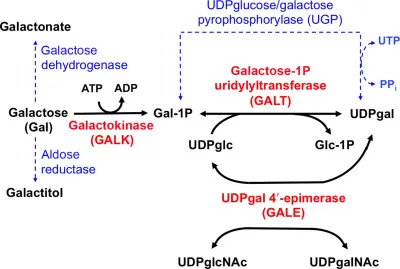
*Galactokinase*
- Deficiency of galactokinase leads to **Type II galactosemia**, characterized primarily by **cataracts** and galactosemia, but typically without the profound liver damage, jaundice, or acute hypoglycemia seen here.
- The symptoms in this case are related to **fructose** intake, not galactose.
*Galactose-1 phosphate uridyltransferase*
- Deficiency in **galactose-1-phosphate uridyltransferase** causes **classic galactosemia**, which presents with **jaundice**, hepatosplenomegaly, vomiting, and cataracts, often triggered by lactose (galactose) intake.
- While it shares some symptoms with the patient's presentation, the trigger of symptoms upon introducing fruits and vegetables (high in fructose) points specifically to an issue with **fructose metabolism**, not galactose.
Special diets in pediatric conditions US Medical PG Question 2: A 6-month-old boy is brought to a pediatrician by his parents for his first visit after they adopt him from a European country. His parents are concerned about the boy’s short episodes of shaking of his arms and legs; they believe it might be epilepsy. They also note that the child is less responsive than other children of his age. The family is unable to provide any vaccination, birth, or family history. His pulse is 130/min, respiratory rate is 28/min, and blood pressure is 90/50 mm Hg. The boy has a light skin tone and emits a noticeable musty body odor. Which of the following should be supplemented in this patient’s diet?
- A. Isoleucine
- B. Leucine
- C. Tyrosine (Correct Answer)
- D. Phenylalanine
- E. Histidine
Special diets in pediatric conditions Explanation: ***Tyrosine***
- The patient's presentation with **seizures**, **developmental delay** (less responsive), **light skin tone**, and a **musty body odor** is highly suggestive of **phenylketonuria (PKU)**.
- In PKU, there is a deficiency in the enzyme **phenylalanine hydroxylase**, which converts **phenylalanine** to **tyrosine**. Therefore, **tyrosine** becomes an **essential amino acid** and must be supplemented in the diet.
*Isoleucine*
- **Isoleucine** is a **branched-chain amino acid** that is typically restricted, along with leucine and valine, in conditions like **maple syrup urine disease (MSUD)**, not PKU.
- Supplementation of isoleucine would be detrimental in MSUD and is not indicated for PKU.
*Leucine*
- Similar to isoleucine, **leucine** is a **branched-chain amino acid** whose metabolism is impaired in **MSUD**, not PKU.
- Supplementing leucine is not beneficial for PKU and would be harmful in MSUD.
*Phenylalanine*
- **Phenylalanine** is the amino acid that accumulates to toxic levels in **PKU** due to the enzyme deficiency.
- Therefore, phenylalanine must be **strictly restricted** in the patient's diet, not supplemented.
*Histidine*
- **Histidine** is an essential amino acid but is not directly involved in the metabolic pathway affected by PKU.
- There is no indication for histidine supplementation in the management of PKU.
Special diets in pediatric conditions US Medical PG Question 3: A 22-year-old man comes to the physician for a routine physical examination. He feels well. He has no history of major medical illness and takes no medications. His vital signs are within normal limits. Examination shows no abnormalities. Laboratory studies, including a complete blood count and a standard electrolyte panel, are within normal limits. Urine dipstick is negative for glucose; a reducing substance test result of the urine is positive. Which of the following is the most appropriate dietary recommendation for this patient?
- A. Eliminate galactose and lactose
- B. Eliminate fructose and sucrose
- C. Increase intake of ketogenic amino acids
- D. Decrease purine intake
- E. No changes needed (Correct Answer)
Special diets in pediatric conditions Explanation: ***No changes needed***
- The positive urine reducing substance test with negative urine glucose in an otherwise healthy individual often indicates **essential fructosuria**, a benign condition.
- Essential fructosuria is caused by a deficiency in **fructokinase** and does not require any dietary modifications.
*Eliminate galactose and lactose*
- This recommendation would be appropriate for **galactosemia**, a condition where the body cannot properly metabolize galactose.
- Galactosemia typically presents with more severe symptoms in infancy, such as **failure to thrive**, **jaundice**, and **cataracts**, which are not present here.
*Eliminate fructose and sucrose*
- This is the recommended diet for **hereditary fructose intolerance**, a more severe disorder involving a deficiency of **aldolase B**.
- Hereditary fructose intolerance would lead to symptoms like **hypoglycemia**, **vomiting**, and **liver damage** upon ingestion of fructose, which are absent in this case.
*Increase intake of ketogenic amino acids*
- This dietary approach is typically used for conditions like **pyruvate dehydrogenase complex deficiency** or **glucose transporter type 1 deficiency syndrome (Glut1 deficiency)**.
- These conditions involve metabolic crises or neurological symptoms that are not relevant to the patient's presentation.
*Decrease purine intake*
- A low-purine diet is recommended for conditions associated with **hyperuricemia**, such as **gout** or **Lesch-Nyhan syndrome**.
- There is no indication of elevated uric acid levels or symptoms related to purine metabolism in this patient.
Special diets in pediatric conditions US Medical PG Question 4: A 2-year-old boy is brought to the emergency department by his mother 30 minutes after having a generalized tonic-clonic seizure. He was born at home and has not attended any well-child visits. He is not yet able to walk and does not use recognizable words. His paternal uncle has a severe intellectual disability and has been living in an assisted-living facility all of his life. The boy's urine phenylacetate level is markedly elevated. Which of the following amino acids is most likely nutritionally essential for this patient because of his underlying condition?
- A. Alanine
- B. Glutamate
- C. Phenylalanine
- D. Cysteine
- E. Tyrosine (Correct Answer)
Special diets in pediatric conditions Explanation: ***Tyrosine***
- The patient's presentation with seizures, developmental delay, and elevated **phenylacetate (a phenylalanine metabolite)** strongly suggest **phenylketonuria (PKU)**.
- In PKU, the enzyme **phenylalanine hydroxylase (PAH)** is deficient, preventing the conversion of **phenylalanine** to **tyrosine**, making **tyrosine** a **nutritionally essential** amino acid.
*Alanine*
- **Alanine** is a **non-essential** amino acid synthesized from pyruvate and other amino acids, and its synthesis is not impaired in PKU.
- It plays a role in **gluconeogenesis** but is not directly related to the metabolic defect in PKU.
*Glutamate*
- **Glutamate** is a **non-essential** amino acid, crucial for neurotransmission and protein synthesis, and is not affected by PKU.
- It can be synthesized from various metabolic intermediates, and its status is not altered in patients with PKU.
*Phenylalanine*
- **Phenylalanine** is an **essential amino acid** that becomes **toxic** when accumulated due to PKU, making it necessary to restrict it in the diet.
- It is the precursor to **tyrosine**, but its inability to be metabolized is the core problem in PKU, not a nutritional essentiality related to the disease.
*Cysteine*
- **Cysteine** is a **conditionally essential** amino acid, often synthesized from methionine, and its synthesis is not directly impacted by PKU.
- While potentially essential in certain conditions, it is not the primary amino acid that becomes essential due to the specific enzymatic defect in PKU.
Special diets in pediatric conditions US Medical PG Question 5: A previously healthy 20-year-old woman comes to the physician because of recurrent abdominal cramps, bloating, and diarrhea for 4 months. She describes her stools as greasy, foul-smelling, and difficult to flush. During this time she has had a 6-kg (13.2-lb) weight loss. She has no personal or family history of serious illness. Physical examination shows pallor and cheilitis. Laboratory studies show a hemoglobin concentration of 11 g/dL. Serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. Test of the stool for occult blood is negative and stool microscopy reveals no pathogens and no leukocytes. Analysis of a 24-hour stool sample shows 12 g of fat. The patient is asked to consume 25 g of d-xylose. Five hours later, its concentration is measured in urine at 2 g (N = > 4 g/5 h). The test is repeated after a two-week course of rifaximin, but the urinary concentration of d-xylose remains the same. Which of the following is the most likely diagnosis?
- A. Exocrine pancreatic insufficiency
- B. Bacterial overgrowth in the small intestine
- C. Tropheryma whipplei infection
- D. Hypersensitivity to gliadin (Correct Answer)
- E. Lactose intolerance
Special diets in pediatric conditions Explanation: ***Hypersensitivity to gliadin***
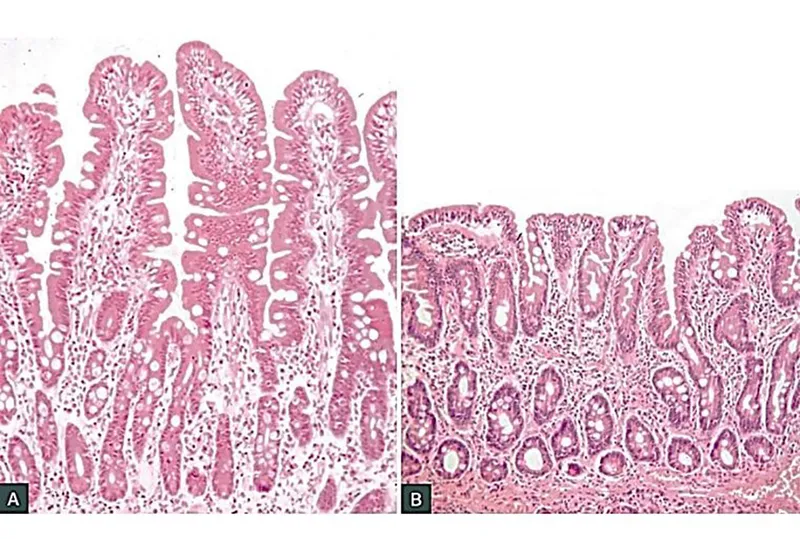
* The patient's symptoms (greasy, foul-smelling stools, weight loss, abdominal cramps, bloating, diarrhea, pallor, cheilitis, iron-deficiency anemia) are highly suggestive of **malabsorption**.
* The **impaired d-xylose absorption** that does not improve after antibiotics points to an intrinsic small bowel mucosal defect rather than bacterial overgrowth, making celiac disease (hypersensitivity to gliadin) the most likely diagnosis.
*Exocrine pancreatic insufficiency*
* While it causes **steatorrhea** and malabsorption, it typically presents with normal d-xylose absorption because **d-xylose is a monosaccharide that is absorbed directly by the intestinal mucosa without requiring pancreatic enzymes**.
* The normal function of the small intestinal mucosa would allow for adequate d-xylose absorption.
*Bacterial overgrowth in the small intestine*
* Symptoms can mimic malabsorption, and d-xylose absorption may be impaired due to bacterial consumption.
* However, the patient's d-xylose test did not improve after a course of **rifaximin**, which is an antibiotic effective against bacterial overgrowth.
*Tropheryma whipplei infection*
* Whipple's disease can cause malabsorption, **steatorrhea**, and abdominal symptoms similar to those described.
* However, it also commonly presents with **arthralgia, lymphadenopathy, and neurological symptoms**, which are absent in this patient.
*Lactose intolerance*
* This condition primarily causes bloating, cramps, and diarrhea, but typically does not lead to **significant weight loss** or **steatorrhea (greasy stools)**.
* D-xylose absorption would also be expected to be normal because it is a **monosaccharide** that is absorbed directly, unlike lactose which requires lactase.
Special diets in pediatric conditions US Medical PG Question 6: You are counseling a mother whose newborn has just screened positive for a deficit of phenylalanine hydroxylase enzyme. You inform her that her child will require dietary supplementation of which of the following?
- A. Aspartame
- B. Niacin
- C. Homogentisic Acid
- D. Tyrosine (Correct Answer)
- E. Leucine
Special diets in pediatric conditions Explanation: ***Tyrosine***
- A deficit of **phenylalanine hydroxylase** prevents the conversion of phenylalanine to tyrosine, making **tyrosine** an essential amino acid that must be supplemented.
- Dietary restriction of **phenylalanine** is also crucial to prevent the accumulation of toxic byproducts that can cause severe neurological damage.
*Aspartame*
- **Aspartame** is an artificial sweetener that contains **phenylalanine**, which would be harmful for a child with phenylalanine hydroxylase deficiency.
- Consumption of aspartame would increase the body's phenylalanine load, exacerbating the metabolic disorder.
*Niacin*
- **Niacin** (vitamin B3) is a vitamin and its supplementation is not related to the phenylalanine hydroxylase pathway or its deficiency.
- Deficiency of niacin is associated with **pellagra**, characterized by dermatitis, diarrhea, and dementia.
*Homogentisic Acid*
- **Homogentisic acid** is an intermediate in the metabolism of tyrosine, and its accumulation is characteristic of **alkaptonuria**, a different metabolic disorder.
- It is not a therapeutic supplement for phenylalanine hydroxylase deficiency.
*Leucine*
- **Leucine** is a branched-chain amino acid, and its metabolism is unrelated to phenylalanine hydroxylase deficiency.
- Supplemental leucine is not required in this condition and would not address the metabolic defect.
Special diets in pediatric conditions US Medical PG Question 7: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
Special diets in pediatric conditions Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
Special diets in pediatric conditions US Medical PG Question 8: A 4-week-old infant is brought to the physician by his mother because of blood-tinged stools for 3 days. He has also been passing whitish mucoid strings with the stools during this period. He was delivered at 38 weeks' gestation by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. He was monitored in the intensive care unit for a day prior to being discharged. His 6-year-old brother was treated for viral gastroenteritis one week ago. The patient is exclusively breastfed. He is at the 50th percentile for height and 60th percentile for weight. He appears healthy and active. His vital signs are within normal limits. Examination shows a soft and nontender abdomen. The liver is palpated just below the right costal margin. The remainder of the examination shows no abnormalities. Test of the stool for occult blood is positive. A complete blood count and serum concentrations of electrolytes and creatinine are within the reference range. Which of the following is the most appropriate next step in management?
- A. Perform stool antigen immunoassay
- B. Perform an air enema on the infant
- C. Assess for IgA (anti‑)tissue transglutaminase antibodies (tTG)
- D. Stop breastfeeding and switch to soy-based formula
- E. Continue breastfeeding and advise mother to avoid dairy and soy products (Correct Answer)
Special diets in pediatric conditions Explanation: ***Continue breastfeeding and advise mother to avoid dairy and soy products***
- The infant's symptoms of **blood-tinged stools** and **mucoid strings**, along with a positive occult blood test, in an otherwise healthy, exclusively breastfed infant point towards **food protein-induced proctocolitis (FPIAP)**.
- The most common triggers for FPIAP are **cow's milk protein** and **soy protein** from the maternal diet transmitted through breast milk. The initial management involves the mother eliminating these proteins from her diet.
*Perform stool antigen immunoassay*
- This test is used to detect specific viral, bacterial, or parasitic antigens in stool, often for conditions like **rotavirus, giardiasis, or C. difficile**.
- The infant's clinical presentation with **no fever, vomiting, or diarrhea**, and an otherwise healthy appearance, makes an infectious cause less likely compared to FPIAP.
*Perform an air enema on the infant*
- An air enema is primarily a diagnostic and therapeutic intervention for **intussusception**, a condition where one segment of the intestine telescopes into another.
- Intussusception typically presents with sudden onset of severe, colicky abdominal pain, **"currant jelly" stools**, and often a palpable abdominal mass, none of which are described in this infant.
*Assess for IgA (anti‑)tissue transglutaminase antibodies (tTG)*
- This test is used to screen for **celiac disease**, an autoimmune disorder triggered by gluten consumption.
- Celiac disease typically presents after the introduction of **gluten-containing foods** into the diet, usually around 6-12 months of age, and is characterized by malabsorption symptoms like diarrhea, weight loss, and failure to thrive, which are absent here.
*Stop breastfeeding and switch to soy-based formula*
- Stopping breastfeeding is generally **not recommended** as breast milk provides numerous benefits.
- Switching to a **soy-based formula** may not resolve the issue, as many infants with cow's milk protein allergy also have a **soy protein allergy**. The preferred approach is to eliminate allergens from the maternal diet while continuing breastfeeding.
Special diets in pediatric conditions US Medical PG Question 9: A 15-month-old girl is brought to the pediatrician by her mother with a history of 3 episodes of breath-holding spells. The patient’s mother says that this is a new behavior and she is concerned. The patient was born at full term by spontaneous vaginal delivery with an uneventful perinatal period. She is also up to date on her vaccines. However, after the age of 6 months, the patient’s mother noticed that she was not as playful as other children of similar age. She is also not interested in interacting with others and her eye contact is poor. Her growth charts suggest that her weight, length, and head circumference were normal at birth, but there have been noticeable decelerations in weight and head circumference. On physical examination, her vital signs are normal. A neurologic examination reveals the presence of generalized mild hypotonia. She also makes repetitive hand wringing motions. Which of the following clinical features is most likely to develop in this patient during the next few years?
- A. Hemiparesis
- B. Intention tremor
- C. Absence seizures
- D. Sensorineural deafness
- E. Loss of purposeful use of her hands (Correct Answer)
Special diets in pediatric conditions Explanation: ***Loss of purposeful use of her hands***
- The constellation of symptoms—**normal development up to 6 months**, followed by **developmental regression** (loss of playfulness, poor social interaction, poor eye contact), **deceleration in head circumference**, **hypotonia**, and **repetitive hand-wringing motions**—is highly suggestive of **Rett syndrome**.
- A hallmark feature of Rett syndrome is the **loss of purposeful hand skills**, which typically occurs between 1 to 4 years of age, replaced by characteristic hand stereotypies like wringing or clapping.
*Hemiparesis*
- **Hemiparesis** is characterized by weakness on one side of the body and is not a typical feature of Rett syndrome.
- While some neurological issues occur, unilateral weakness is more indicative of focal neurological injury rather than this diffuse neurodevelopmental disorder.
*Intention tremor*
- **Intention tremor** is a type of dyskinesia that worsens during voluntary movement and is often associated with cerebellar dysfunction.
- While motor difficulties are prominent in Rett syndrome, **ataxia** and **apraxia** are more characteristic than a predominant intention tremor.
*Absence seizures*
- **Absence seizures** involve brief, sudden lapses of consciousness and are a type of generalized epilepsy.
- Although seizures are common in Rett syndrome, **generalized tonic-clonic seizures** or **focal seizures** are more frequently observed than isolated absence seizures.
*Sensorineural deafness*
- **Sensorineural deafness** implies damage to the inner ear or auditory nerve, resulting in permanent hearing loss.
- While communication difficulties are significant in Rett syndrome, they are due to speech apraxia and cognitive impairment, not primary hearing loss.
Special diets in pediatric conditions US Medical PG Question 10: A 16-year-old boy is brought to the physician for a follow-up examination. He has a 6-year history of type 1 diabetes mellitus and his only medication is insulin. Seven months ago, he was treated for an episode of diabetic ketoacidosis. He has previously been compliant with his diet and insulin regimen. He wants to join the high school soccer team. Vital signs are within normal limits. His hemoglobin A1C is 6.3%. Which of the following is the most appropriate recommendation at this time?
- A. Limit activity to 20 minutes per day
- B. Lower insulin dosage on days of exercise (Correct Answer)
- C. Advise against physical activity
- D. Switch from insulin to metformin
- E. Increase insulin dosage on days of exercise
Special diets in pediatric conditions Explanation: ***Lower insulin dosage on days of exercise***
- Exercise increases **insulin sensitivity** and glucose uptake by muscle cells, which can lead to **hypoglycemia** if insulin dosing is not adjusted.
- Reducing insulin dosage on exercise days, along with appropriate monitoring, is a common strategy to prevent exercise-induced hypoglycemia in individuals with **type 1 diabetes**.
*Limit activity to 20 minutes per day*
- There is no medical justification to arbitrarily limit activity to 20 minutes for a well-controlled diabetic patient, especially one who wants to join a soccer team.
- **Regular physical activity** is beneficial for overall health and diabetes management, and arbitrary restrictions can be detrimental to a teenager's well-being.
*Advise against physical activity*
- **Physical activity** is generally encouraged for individuals with type 1 diabetes as it improves **cardiovascular health**, **insulin sensitivity**, and overall well-being.
- Advising against it would be counterproductive, especially with an **HbA1c of 6.3%**, indicating good glycemic control and proper management.
*Switch from insulin to metformin*
- **Metformin** is an oral hypoglycemic agent used primarily for type 2 diabetes by reducing hepatic glucose production and improving insulin sensitivity.
- It is **not effective** in type 1 diabetes, where the pancreas fails to produce insulin, making **exogenous insulin** essential for survival.
*Increase insulin dosage on days of exercise*
- Increasing insulin dosage on exercise days would significantly raise the risk of **hypoglycemia** due to enhanced glucose utilization by muscles.
- The standard approach is to **decrease** insulin or increase carbohydrate intake to prevent low blood sugar during and after exercise.
More Special diets in pediatric conditions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.