Micronutrient deficiencies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Micronutrient deficiencies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Micronutrient deficiencies US Medical PG Question 1: A 61-year-old woman presents for a routine health visit. She complains of generalized fatigue and lethargy on most days of the week for the past 4 months. She has no significant past medical history and is not taking any medications. She denies any history of smoking or recreational drug use but states that she drinks "socially" approx. 6 nights a week. She says she also enjoys a "nightcap," which is 1–2 glasses of wine before bed every night. The patient is afebrile, and her vital signs are within normal limits. On physical examination, there is significant pallor of the mucous membranes. Laboratory findings are significant for a mean corpuscular volume (MCV) of 72 fL, leukocyte count of 4,800/mL, hemoglobin of 11.0 g/dL, and platelet count of 611,000/mL. Stool guaiac test is negative. She is started on oral ferrous sulfate supplements. On follow-up, her laboratory parameters show no interval change in her MCV or platelet level, and she reports good compliance with the medication. Which of the following is the best next step in the management of this patient?
- A. Transfuse the patient with whole blood
- B. Administer folate
- C. Administer iron intravenously (Correct Answer)
- D. Continue oral ferrous sulfate and supplement with omeprazole
- E. Continue oral ferrous sulfate and supplement with ascorbic acid
Micronutrient deficiencies Explanation: **Administer iron intravenously**
- The patient shows **microcytic anemia** (MCV 72 fL) and **thrombocytosis** (platelet count 611,000/mL), which are classic signs of **iron deficiency anemia**.
- Given the failure of oral ferrous sulfate to improve her parameters, despite likely good adherence given the repeat visit, **intravenous iron** is the next appropriate step to ensure adequate iron repletion.
*Transfuse the patient with whole blood*
- **Blood transfusion** is reserved for patients with severe, symptomatic anemia, often with a hemoglobin level much lower than 11.0 g/dL, or in cases of acute hemorrhage.
- This patient's anemia is chronic and her hemoglobin level, while low, is not critically low enough to warrant immediate transfusion.
*Administer folate*
- **Folate deficiency** typically causes **macrocytic anemia** (high MCV), not microcytic anemia, making it an inappropriate treatment for this patient.
- Though chronic alcohol use can affect folate levels, the patient's presentation is more consistent with iron deficiency.
*Continue oral ferrous sulfate and supplement with omeprazole*
- **Omeprazole** is a **proton pump inhibitor** that can actually *reduce* iron absorption by decreasing gastric acidity, making it counterproductive in treating iron deficiency.
- Continuing oral iron alone was already proven ineffective, necessitating a more aggressive approach.
*Continue oral ferrous sulfate and supplement with ascorbic acid*
- **Ascorbic acid (vitamin C)** can enhance the absorption of non-heme iron; however, since the initial trial of oral ferrous sulfate alone was ineffective, merely adding ascorbic acid may not be sufficient.
- The lack of improvement suggests either poor absorption or significant ongoing loss, which intravenous iron addresses more directly.
Micronutrient deficiencies US Medical PG Question 2: A 44-year-old male immigrant presents to his primary care physician for a new patient visit. The patient reports chronic fatigue but states that he otherwise feels well. His past medical history is not known, and he is not currently taking any medications. The patient admits to drinking 7 alcoholic beverages per day and smoking 1 pack of cigarettes per day. His temperature is 99.4°F (37.4°C), blood pressure is 157/98 mmHg, pulse is 99/min, respirations are 18/min, and oxygen saturation is 100% on room air. Physical exam demonstrates mild pallor but is otherwise not remarkable. Laboratory studies are ordered as seen below.
Hemoglobin: 9 g/dL
Hematocrit: 33%
Leukocyte count: 6,500/mm^3 with normal differential
Platelet count: 190,000/mm^3
Mean corpuscular volume (MCV): 60 femtoliters
Free iron: 272 mcg/dL
Total iron binding capacity (TIBC): 175 mcg/dL
Ferritin: 526 ng/mL
Reticulocyte count: 2.8%
Which of the following is the most likely diagnosis?
- A. Folate deficiency
- B. Beta-thalassemia (Correct Answer)
- C. Iron deficiency
- D. B12 deficiency
- E. Hemolytic anemia
Micronutrient deficiencies Explanation: ***Beta-thalassemia***
- The patient presents with **microcytic anemia** (MCV 60 fL) and **elevated ferritin**, **high free iron**, and **low TIBC**, which are characteristic of thalassemia due to ineffective erythropoiesis and iron overload.
- A **reticulocyte count of 2.8%** (elevated for the degree of anemia) indicates the bone marrow is attempting to compensate, consistent with a hemolytic process like thalassemia.
*Folate deficiency*
- Folate deficiency typically causes **macrocytic anemia** (elevated MCV), which is not seen here; the patient has microcytic anemia.
- Alcohol abuse can cause folate deficiency, but the lab values for iron studies and MCV are inconsistent with this diagnosis.
*Iron deficiency*
- Iron deficiency anemia would present with **low ferritin**, **low free iron**, and **high TIBC**, which are opposite to the patient's lab results.
- Although the patient has microcytic anemia, the iron study profile rules out iron deficiency.
*B12 deficiency*
- Vitamin B12 deficiency also causes **macrocytic anemia** (elevated MCV), often with neurological symptoms, neither of which are observed in this patient.
- The patient's microcytic anemia and iron study results contradict a diagnosis of B12 deficiency.
*Hemolytic anemia*
- While beta-thalassemia is a form of hemolytic anemia, the term "hemolytic anemia" alone is too broad and does not specify the underlying cause, especially with the provided iron studies and MCV.
- Other common causes of hemolytic anemia, like autoimmune hemolytic anemia or G6PD deficiency, would require different diagnostic presentations or specific tests not consistent with the given lab values.
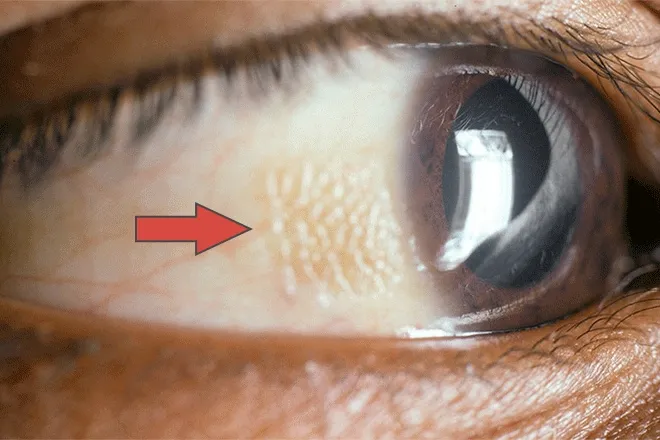
Micronutrient deficiencies US Medical PG Question 3: A 46-year-old man presents to the office complaining of dry, irritated eyes that have gotten worse over the last week. The patient states that he has also developed a red bumpy rash on his arms. On exam, his bilateral cornea and conjunctiva are dry and thickened. There are small ulcerations on the cornea. The skin of the bilateral arms has an erythematous rash characterized by small, white raised lesions. The patient has a history of alcoholism but has no other significant past medical history. What is most likely deficient in this patient?
- A. Thiamine
- B. Folic acid
- C. Vitamin B12
- D. Vitamin A (Correct Answer)
- E. Vitamin K
Micronutrient deficiencies Explanation: ***Vitamin A***
- **Dry, irritated eyes** with **corneal and conjunctival thickening and ulcerations** are classic signs of **xerophthalmia**, a severe manifestation of **vitamin A deficiency**.
- The **red bumpy rash with small, white raised lesions** on the arms (follicular hyperkeratosis or **phrynoderma**) is also characteristic of **vitamin A deficiency**, commonly seen in individuals with **alcoholism** due to poor nutrition and malabsorption.
*Thiamine*
- **Thiamine (B1) deficiency** (beriberi or Wernicke-Korsakoff syndrome) primarily affects the **nervous and cardiovascular systems**, leading to symptoms like peripheral neuropathy, Wernicke's encephalopathy, or heart failure.
- It does not typically cause the specific ocular or dermatological findings described in this patient.
*Folic acid*
- **Folic acid deficiency** usually presents with **macrocytic anemia**, fatigue, and glossitis.
- It is not associated with the ocular and skin manifestations seen in this patient.
*Vitamin B12*
- **Vitamin B12 deficiency** can cause **macrocytic anemia** and neurological symptoms such as peripheral neuropathy, cognitive impairment, and subacute combined degeneration of the spinal cord.
- It does not explain the specific eye and skin symptoms observed.
*Vitamin K*
- **Vitamin K deficiency** primarily leads to **coagulopathy** (bleeding disorders) due to impaired synthesis of clotting factors.
- It does not cause the ocular dryness, corneal damage, or the specific rash described in the patient.
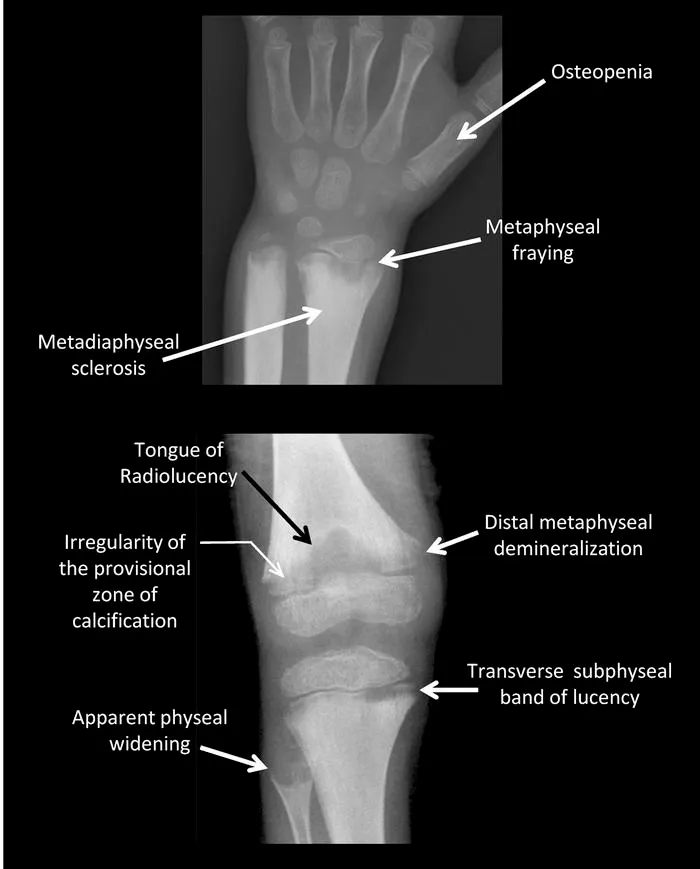
Micronutrient deficiencies US Medical PG Question 4: A 67-year-old male presents to his primary care physician complaining of left hip pain for the past six months. He denies any trauma or recent falls. He is accompanied by his wife who reports that he has experienced progressive hearing loss over the same time period. The patient has also noticed that he is no longer able to fit into his favorite hat even though it previously fit well. A radiograph of the patient’s pelvis is shown. Which of the following laboratory abnormalities is most likely to be found in this patient?
- A. Elevated serum calcium
- B. Decreased serum alkaline phosphatase
- C. Decreased serum calcium
- D. Elevated serum parathyroid hormone
- E. Elevated serum alkaline phosphatase (Correct Answer)
Micronutrient deficiencies Explanation: ***Elevated serum alkaline phosphatase***
- The patient's symptoms (hip pain, progressive hearing loss, increased hat size) suggest **Paget's disease of bone**, which is characterized by accelerated bone turnover.
- **Alkaline phosphatase** is an enzyme produced by osteoblasts, and its elevation in serum is a hallmark of increased bone formation and remodeling seen in Paget's disease.
*Elevated serum calcium*
- In uncomplicated Paget's disease, serum calcium levels are typically **normal**, as the increased bone turnover usually maintains a balance between resorption and formation.
- Hypercalcemia in Paget's disease is rare and may occur in cases of **immobility** or concomitant primary hyperparathyroidism.
*Decreased serum alkaline phosphatase*
- This would indicate reduced osteoblastic activity or bone formation, which is the opposite of the accelerated bone remodeling seen in **Paget's disease**.
- Conditions like **hypophosphatasia** or severe malnutrition might lead to decreased alkaline phosphatase.
*Decreased serum calcium*
- Hypocalcemia is not a typical feature of Paget's disease unless there are other contributing factors such as **malabsorption** or **renal failure**.
- Bone turnover in Paget's disease usually maintains normal serum calcium levels through coupled osteoclastic and osteoblastic activity.
*Elevated serum parathyroid hormone*
- While **elevated parathyroid hormone** can cause increased bone turnover, it primarily does so by increasing osteoclastic activity to release calcium from bone, leading to hypercalcemia.
- In Paget's disease, **parathyroid hormone levels are typically normal** unless there is co-existing primary hyperparathyroidism.
Micronutrient deficiencies US Medical PG Question 5: A 10-year-old boy is brought into your clinic by his mother for sunburns that have not been healing. The mother states that he easily gets sunburned. The mother admits she gave birth to him at home and has never taken him to see a doctor. The patient walks with a wide stance gait and appears unstable on his feet. He has an extensive erythematous, scaling, hyperkeratotic rash on his face, neck, arms and legs. After extensive workup, the patient is found to have a genetic disorder that results in defective absorption of an important vitamin. Which of the following is likely to be low if measured?
- A. Vitamin K
- B. Niacin (Correct Answer)
- C. Folate
- D. Vitamin A
- E. Vitamin B12
Micronutrient deficiencies Explanation: ***Niacin***
- The constellation of **sunburns that don't heal**, a **wide-stanced unstable gait**, and an **erythematous, scaling, hyperkeratotic rash** (consistent with dermatitis) strongly suggests **pellagra**.
- Pellagra is caused by a deficiency of **niacin (Vitamin B3)**, which is characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia (or neurological symptoms like ataxia)**.
*Vitamin K*
- Deficiency typically leads to **bleeding disorders** due to impaired coagulation, which is not indicated by the patient's symptoms.
- While newborns often receive a **vitamin K shot**, his current symptoms are unrelated to its deficiency.
*Folate*
- Folate deficiency primarily causes **megaloblastic anemia** and can lead to **neural tube defects** in developing fetuses.
- It does not explain the characteristic dermatological and neurological symptoms described.
*Vitamin A*
- Vitamin A deficiency is known to cause **night blindness** and **xerophthalmia** (dry eyes), and impaired immune function.
- While it plays a role in skin health, the specific rash and gait abnormalities point away from primary vitamin A deficiency.
*Vitamin B12*
- Deficiency leads to **megaloblastic anemia** with **neurological symptoms** such as peripheral neuropathy, but the dermatological manifestations (scaling, hyperkeratotic rash) and unhealing sunburn are not typical.
- The gait could be linked to neurological symptoms, but the overall presentation is better explained by niacin deficiency.
Micronutrient deficiencies US Medical PG Question 6: A 24-year-old man presents to the emergency department complaining of a prolonged course of diarrhea. He reports that he has had 3–4 large volume watery stools daily for the last several weeks. He has no pain with bowel movements, no abdominal pain, and no blood in his stools. He is homeless and uses recreational drugs. He also reports that he usually drinks a half-liter of whiskey, or whatever else he can find, every day and he has done this for several years. The physical exam is notable for a hyperpigmented rash across his face, neck, chest, and the backs of his hands and forearms. On mental status exam, he is oriented to person and place but not time; he scores a 23/30 on the Montreal Cognitive Assessment (MOCA). This patient's presentation is most likely related to which of the following micronutrients?
- A. Vitamin B2
- B. Vitamin B12
- C. Vitamin D
- D. Vitamin C
- E. Vitamin B3 (Correct Answer)
Micronutrient deficiencies Explanation: ***Vitamin B3***
- The patient's symptoms—diarrhea, dermatitis (hyperpigmented rash), and dementia (disorientation to time, MOCA 23/30)—are the classic **3 Ds of pellagra**, which is caused by a **vitamin B3 (niacin) deficiency**.
- His chronic alcohol use and poor nutritional status (homelessness, recreational drug use) put him at high risk for such a deficiency, as alcohol impairs nutrient absorption and niacin is often lacking in the diets of those with limited food access.
*Vitamin B2*
- Deficiency in **vitamin B2 (riboflavin)** typically presents with cheilosis, angular stomatitis, glossitis, seborrheic dermatitis, and ocular symptoms like corneal vascularization, none of which are specifically mentioned here.
- While chronic alcohol use can also cause riboflavin deficiency, the patient's full symptom complex points more strongly to pellagra.
*Vitamin B12*
- **Vitamin B12 deficiency** often leads to **macrocytic anemia**, neurological symptoms including peripheral neuropathy, ataxia, and cognitive impairment, and glossitis, but it does not typically cause the characteristic dermatologic rash or diarrhea seen in this patient.
- While chronic alcohol use is a risk factor, the specific triad of diarrhea, dermatitis, and dementia is not consistent with B12 deficiency.
*Vitamin D*
- **Vitamin D deficiency** is associated with bone health issues (rickets in children, osteomalacia in adults), muscle weakness, and in severe cases, hypocalcemia.
- It does not present with the specific combination of diarrhea, hyperpigmented rash, and cognitive changes described in the patient.
*Vitamin C*
- **Vitamin C deficiency (scurvy)** typically manifests as perifollicular hyperkeratosis, bleeding gums, petechiae, impaired wound healing, and musculoskeletal pain.
- While malnourishment and alcohol abuse increase the risk of scurvy, the patient's symptoms do not align with the classic presentation of vitamin C deficiency.
Micronutrient deficiencies US Medical PG Question 7: A 17-year-old girl is brought in by her mother due to rapid weight loss over the past month. The patient says she has been having episodes of diarrhea, which she attributes to laxatives she takes regularly to keep her weight down. She also says she has not had her period yet. The patient’s mother adds that the patient has been underperforming at school and acting very strangely at home. Her current BMI is 16.8 kg/m2. On physical examination, the skin on her limbs and around her neck is inflamed and erythematous. Her tongue is bright red and smooth. She states that over the last 2 weeks, she has been eating nothing but small portions of fruit. She is diagnosed with a vitamin deficiency. Which of the following statements is true about the vitamin most likely deficient in this patient?
- A. It increases the GI absorption of iron
- B. It is derived from tyrosine
- C. Synthesis requires vitamin B2 and B6 (Correct Answer)
- D. Synthesis requires vitamin B1 and B6
- E. It is used to treat hypertension
Micronutrient deficiencies Explanation: ***Synthesis requires vitamin B2 and B6***
- The patient's symptoms (diarrhea, dermatitis, dementia-like behavior, glossitis, and weight loss) are classic for **pellagra**, which is caused by a deficiency in **niacin (vitamin B3)**.
- The synthesis of **niacin** from **tryptophan** requires **pyridoxine (vitamin B6)** and **riboflavin (vitamin B2)** as cofactors.
*It increases the GI absorption of iron*
- **Vitamin C** (ascorbic acid) enhances the **gastrointestinal absorption of non-heme iron** by reducing ferric iron to its ferrous form.
- Niacin does not play a direct role in the absorption of iron.
*It is derived from tyrosine*
- **Tyrosine** is a precursor to several important compounds, including **catecholamines** (dopamine, norepinephrine, epinephrine) and **thyroid hormones**.
- **Niacin** is predominantly synthesized from the essential amino acid **tryptophan**.
*Synthesis requires vitamin B1 and B6*
- While **vitamin B6** is essential for niacin synthesis from tryptophan, **vitamin B1 (thiamine)** is not directly involved in this pathway.
- Thiamine's primary role is in carbohydrate metabolism.
*It is used to treat hypertension*
- While **niacin** can affect lipid profiles, it is **not commonly used as a primary treatment for hypertension**.
- **Niacin** is used, primarily in pharmacologic doses, to **lower LDL cholesterol** and **triglycerides** and **raise HDL cholesterol**, often in conjunction with other lipid-lowering agents.
Micronutrient deficiencies US Medical PG Question 8: A 67-year-old male presents with left hip pain. Examination reveals mild effusions in both knees, with crepitus in both patellofemoral joints. He states his hearing has worsened recently and that he feels like his hats don't fit anymore. Bone scan reveals diffuse uptake in the calvarium, right proximal femur, and left ilium. Which of the following laboratory abnormalities would be expected in this patient?
- A. Increased serum calcium
- B. Increased serum alkaline phosphatase (Correct Answer)
- C. Decreased serum alkaline phosphatase
- D. Increased serum parathyroid hormone
- E. Decreased serum parathyroid hormone
Micronutrient deficiencies Explanation: ***Increased serum alkaline phosphatase***
- The clinical picture (hip pain, worsened hearing, hats not fitting, diffuse bone uptake on scan) is highly suggestive of **Paget's disease of bone**.
- In Paget's disease, there is increased bone turnover with excessive osteoclastic activity followed by compensatory, disorganized osteoblastic activity, leading to a marked elevation in **serum alkaline phosphatase (ALP)**, a marker of osteoblastic activity.
*Increased serum calcium*
- While bone breakdown occurs in Paget's disease, hypercalcemia is uncommon; it usually only occurs in immobilized patients.
- The bone remodeling is typically balanced, with increased formation countering increased resorption.
*Decreased serum alkaline phosphatase*
- Paget's disease is characterized by significantly *increased* bone turnover and osteoblastic activity, leading to **elevated** rather than decreased serum alkaline phosphatase.
- A decreased ALP level would suggest conditions like hypophosphatasia, not Paget's disease.
*Increased serum parathyroid hormone*
- **Primary hyperparathyroidism** would lead to increased PTH, causing hypercalcemia and bone resorption, but the widespread, disorganized bone changes and localized uptake on a bone scan are more consistent with Paget's disease.
- Increased PTH is not a direct consequence or feature of uncomplicated Paget's disease.
*Decreased serum parathyroid hormone*
- This would typically be seen in states of hypercalcemia not driven by PTH, or in conditions like primary hypoparathyroidism.
- There is no direct mechanism in Paget's disease that would cause decreased PTH levels.
Micronutrient deficiencies US Medical PG Question 9: A 19-year-old African female refugee has been granted asylum in Stockholm, Sweden and has been living there for the past month. She arrived in Sweden with her 2-month-old infant, whom she exclusively breast feeds. Which of the following deficiencies is the infant most likely to develop?
- A. Vitamin E
- B. Vitamin A
- C. Vitamin C
- D. Vitamin B1
- E. Vitamin D (Correct Answer)
Micronutrient deficiencies Explanation: ***Vitamin D***
- The combination of exclusive breastfeeding, a 2-month-old infant, being of African heritage (darker skin), and living in a high-latitude region like Stockholm, Sweden, significantly increases the risk of **vitamin D deficiency**. Darker skin pigmentation reduces the efficiency of **cutaneous vitamin D synthesis** from sunlight, and insufficient sun exposure in northern latitudes further exacerbates this.
- Breast milk is a relatively poor source of **vitamin D**, and infants specifically require supplementation, especially when they have risk factors for deficiency such as being of African descent and living in an area with limited sunshine.
*Vitamin E*
- **Vitamin E deficiency** in infants is rare and typically seen in premature infants or those with severe malabsorption, neither of which is indicated in this scenario.
- While breast milk contains vitamin E, deficiency is not directly linked to geographic location, skin color, or a 2-month-old infant.
*Vitamin A*
- **Vitamin A deficiency** can be a concern in developing countries, but it is less likely to be the primary concern under these specific circumstances in a 2-month-old exclusively breastfed infant unless the mother herself is severely deficient.
- Breast milk usually provides adequate **vitamin A** if the mother's nutritional status is sufficient.
*Vitamin C*
- **Vitamin C deficiency** (scurvy) is rare in breastfed infants because breast milk typically contains adequate vitamin C if the mother has adequate dietary intake.
- Scurvy would be more likely in infants fed with improperly prepared formula or after 6 months if complementary foods lack vitamin C.
*Vitamin B1*
- **Vitamin B1 (thiamine) deficiency** is uncommon in exclusively breastfed infants in developed countries.
- It is often associated with maternal malnutrition in endemic areas or specific genetic disorders, which are not suggested here.
Micronutrient deficiencies US Medical PG Question 10: A 5-month-old male presents to the pediatrician with his mother for a well visit. The patient was born at 35 weeks gestation to a 30-year-old gravida 2 via vaginal delivery. The pregnancy and labor were uncomplicated. The patient required no resuscitation after delivery and was discharged from the hospital on day two of life. His mother now reports that the patient has been exclusively breastfed since birth, and she says that feedings have been going well, and that the patient appears satisfied afterwards. The patient feeds for 30 minutes every two hours and urinates 8-10 times per day. The patient’s mother reports that she eats a varied diet that includes animal products, but she worries that the patient is not meeting his nutritional needs with breastmilk alone. The patient’s height and weight at birth were in the 15th and 20th percentile, respectively. His height and weight are now in the 20th and 25th percentile, respectively. His temperature is 98.1°F (36.7°C), blood pressure is 58/46 mmHg, pulse is 128/min, and respirations are 34/min. On physical exam, the patient appears well-developed and well-nourished. He has mild conjunctival pallor.
Which of the following is the most appropriate guidance regarding this patient’s nutritional needs?
- A. Add cow's milk to his diet
- B. Supplement his diet with formula
- C. No changes are necessary to his diet
- D. Supplement his diet with iron and vitamin D (Correct Answer)
- E. Add pureed foods to his diet
Micronutrient deficiencies Explanation: ***Supplement his diet with iron and vitamin D***
- This 5-month-old infant, exclusively breastfed, requires **iron supplementation** because maternal iron stores are depleted by 4-6 months, and breast milk is a poor source of iron. Additionally, **Vitamin D supplementation** is crucial for all exclusively breastfed infants to prevent rickets.
- The presence of mild **conjunctival pallor** further suggests possible iron deficiency.
*Add cow's milk to his diet*
- **Cow's milk** should not be introduced before 12 months of age as it contains high protein and mineral content that can stress an infant's immature kidneys and can lead to **gastrointestinal bleeding**, insufficient iron absorption, and **iron-deficiency anemia**.
- It also has a low iron content and lacks the essential fatty acids necessary for proper infant development.
*Supplement his diet with formula*
- While formula contains iron and vitamin D, the mother reports that the baby is feeding well and appears satisfied, with appropriate weight gain (20th to 25th percentile) and frequent wet diapers, indicating **adequate nutrition from breast milk alone**.
- **Exclusive breastfeeding** is recommended for the first 6 months of life when feasible, and there is no clear indication that breast milk alone is insufficient for overall caloric and macronutrient needs here yet.
*No changes are necessary to his diet*
- This is incorrect because, despite adequate breastfeeding, **exclusive breastfed infants** like this one require supplementation with **iron and vitamin D** to meet their micronutrient needs.
- The mild conjunctival pallor also suggests a potential, or impending, deficiency that warrants intervention.
*Add pureed foods to his diet*
- The current recommendations suggest introducing solid foods, including pureed foods, around **6 months of age**, when the infant shows signs of developmental readiness.
- While the infant is close to 6 months, introducing solids at 5 months is typically not necessary if growth is appropriate and specific micronutrient deficiencies (like iron and vitamin D) can be addressed through supplementation.
More Micronutrient deficiencies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.