Malnutrition management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Malnutrition management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Malnutrition management US Medical PG Question 1: A 7-day-old male infant presents to the pediatrician for weight loss. There is no history of excessive crying, irritability, lethargy, or feeding difficulty. The parents deny any history of fast breathing, bluish discoloration of lips/nails, fever, vomiting, diarrhea, or seizures. He was born at full term by vaginal delivery without any perinatal complications and his birth weight was 3.6 kg (8 lb). Since birth he has been exclusively breastfed and passes urine six to eight times a day. His physical examination, including vital signs, is completely normal. His weight is 3.3 kg (7.3 lb); length and head circumference are normal for his age and sex. Which of the following is the next best step in the management of the infant?
- A. Reassurance of parents (Correct Answer)
- B. Evaluation of the mother for malnutrition
- C. Admission of the infant in the NICU to treat with empiric intravenous antibiotics
- D. Emphasize the need to clothe the infant warmly to prevent hypothermia
- E. Supplementation of breastfeeding with an appropriate infant formula
Malnutrition management Explanation: ***Reassurance of parents***
- A **weight loss of 8.3%** (300g from 3.6kg) is within the expected range for a 7-day-old exclusively breastfed infant, which can be up to 7-10% in the first week.
- The infant's normal physical exam, good urine output, and lack of other symptoms suggest **adequate feeding** and overall well-being.
*Evaluation of the mother for malnutrition*
- The mother's nutritional status is not directly indicative of the infant's weight loss within the normal physiological range in this scenario.
- There is no information to suggest the mother is malnourished or that it would directly impact the quality or quantity of breast milk to cause pathological weight loss.
*Admission of the infant in the NICU to treat with empiric intravenous antibiotics*
- This is an overly aggressive intervention as there are **no signs or symptoms of infection** (e.g., fever, lethargy, poor feeding) and the infant appears well.
- Empiric antibiotics are not warranted in an otherwise healthy, full-term infant with normal physiological weight loss.
*Emphasize the need to clothe the infant warmly to prevent hypothermia*
- The infant's **vital signs are normal**, indicating no hypothermia, and there is no clinical evidence to support this as a primary concern.
- While maintaining warmth is important, it is not the next best step for addressing this specific presentation of physiological weight loss.
*Supplementation of breastfeeding with an appropriate infant formula*
- Supplementation is typically not needed for physiological weight loss in an otherwise healthy, exclusively breastfed infant with **adequate urine output** and no signs of dehydration.
- Encouraging continued exclusive breastfeeding and providing support for proper latch and feeding techniques would be more appropriate if there were concerns about inadequate milk intake.
Malnutrition management US Medical PG Question 2: A 7-year-old boy is brought to the emergency room because of severe, acute diarrhea. He is drowsy with a dull, lethargic appearance. He has sunken eyes, poor skin turgor, and dry oral mucous membranes and tongue. He has a rapid, thready pulse with a systolic blood pressure of 60 mm Hg and his respirations are 33/min. His capillary refill time is 6 sec. He has had no urine output for the past 24 hours. Which of the following is the most appropriate next step in treatment?
- A. Start IV fluid resuscitation by administering colloid solutions
- B. Provide oral rehydration therapy to correct dehydration
- C. Give initial IV bolus of 2 L of Ringer’s lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1
- D. Start IV fluid resuscitation with normal saline or Ringer’s lactate, along with monitoring of vitals and urine output (Correct Answer)
- E. Give antidiarrheal drugs
Malnutrition management Explanation: ***Start IV fluid resuscitation with normal saline or Ringer's lactate, along with monitoring of vitals and urine output***
- This patient presents with **severe dehydration** and **hypovolemic shock** (lethargy, sunken eyes, poor skin turgor, dry mucous membranes, rapid thready pulse, hypotension [systolic BP 60 mmHg], tachypnea, prolonged capillary refill >5 seconds, and anuria).
- According to **PALS guidelines**, the immediate priority is rapid intravenous administration of **isotonic crystalloids** (normal saline or Ringer's lactate) given as **20 mL/kg boluses** over 5-20 minutes, repeated as needed based on clinical response.
- Close monitoring of vital signs, mental status, perfusion (capillary refill), and urine output is essential to assess response to resuscitation and guide further fluid management.
*Start IV fluid resuscitation by administering colloid solutions*
- While colloids (albumin, synthetic colloids) can expand intravascular volume, **isotonic crystalloids** are preferred for initial resuscitation in severe dehydration per **WHO and PALS guidelines**.
- Crystalloids are equally effective, more readily available, less expensive, and have fewer potential adverse effects compared to colloids in pediatric dehydration.
- There is no proven survival benefit of colloids over crystalloids in this clinical scenario.
*Provide oral rehydration therapy to correct dehydration*
- **Oral rehydration therapy (ORT)** is the appropriate first-line treatment for **mild to moderate dehydration** in children who can tolerate oral intake.
- However, ORT is **contraindicated** in patients with **severe dehydration** or **hypovolemic shock**, particularly those with altered mental status, inability to drink, or hemodynamic instability.
- This patient's drowsiness, hypotension, and signs of shock require immediate IV resuscitation; ORT would be too slow and potentially dangerous.
*Give initial IV bolus of 2 L of Ringer's lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1*
- A 2-liter bolus is **excessive and dangerous** for a 7-year-old child (average weight ~23 kg); the appropriate initial bolus is **20 mL/kg** (~460 mL), which can be repeated based on response.
- The **1:1:1 massive transfusion protocol** (packed RBCs, FFP, platelets) is indicated for **hemorrhagic shock** with significant blood loss, not for hypovolemic shock from dehydration.
- There is no evidence of bleeding or coagulopathy in this patient; blood products are not indicated.
*Give antidiarrheal drugs*
- **Antidiarrheal agents** (loperamide, diphenoxylate) are **contraindicated** in young children with acute infectious diarrhea, as they can prolong illness, increase risk of complications (toxic megacolon, bacterial overgrowth), and mask serious underlying conditions.
- The priority in severe dehydration is **fluid and electrolyte resuscitation**, not stopping the diarrhea.
- The diarrhea typically resolves once the underlying infection is controlled and hydration is restored.
Malnutrition management US Medical PG Question 3: A 42-year-old man is brought to the emergency department by his wife because of a 1-day history of progressive confusion. He recently lost his job. He has a history of chronic alcoholism and has been drinking 14 beers daily for the past week. Before this time, he drank 6 beers daily. He appears lethargic. His vital signs are within normal limits. Serum studies show a sodium level of 111 mEq/L and a potassium level of 3.7 mEq/L. Urgent treatment for this patient's current condition increases his risk for which of the following adverse events?
- A. Wernicke encephalopathy
- B. Osmotic myelinolysis (Correct Answer)
- C. Cerebral edema
- D. Cardiac arrhythmia
- E. Hyperglycemia
Malnutrition management Explanation: ***Osmotic myelinolysis***
* **Rapid correction of severe hyponatremia** (serum sodium <120 mEq/L), especially when chronic, can cause **osmotic demyelination syndrome** (also known as central pontine myelinolysis).
* This condition results from a sudden shift in osmolality, causing water to leave brain cells, leading to neuronal damage and severe neurological deficits.
*Wernicke encephalopathy*
* **Wernicke encephalopathy** is caused by **thiamine deficiency**, common in chronic alcoholics.
* While he is at risk for Wernicke encephalopathy, the urgent treatment for his hyponatremia (rapid correction) is more likely to cause osmotic myelinolysis, not directly trigger Wernicke encephalopathy.
*Cerebral edema*
* **Cerebral edema** is a direct consequence of **severe, acute hyponatremia** (as fluid shifts into brain cells), not a risk of its *treatment*.
* The question asks about the risk of urgent treatment, which aims to *reduce* cerebral edema.
*Cardiac arrhythmia*
* While severe electrolyte imbalances can cause **cardiac arrhythmias**, the **rapid correction of hyponatremia** does not directly or primarily increase the risk of arrhythmias.
* The immediate risk associated with hyponatremia correction is neurological, related to osmotic shifts.
*Hyperglycemia*
* **Hyperglycemia** is a condition of high blood glucose and is not directly related to or caused by the **rapid correction of hyponatremia**.
* Although chronic alcohol abuse can affect glucose metabolism, hyperglycemia is not an acute adverse event of treating hyponatremia.
Malnutrition management US Medical PG Question 4: A 45-year-old man presents to the physician with limb weakness over the last 24 hours. He is an otherwise healthy man with no significant past medical history. On physical examination, his vital signs are stable. On neurological examination, there is decreased strength in the muscles of all 4 extremities, and the deep tendon reflexes are depressed. A detailed laboratory evaluation shows that he has generalized decreased neuronal excitability due to an electrolyte imbalance. Which of the following electrolyte imbalances is most likely to be present in the man?
- A. Acute hypochloremia
- B. Acute hypernatremia
- C. Acute hyperkalemia
- D. Acute hypercalcemia (Correct Answer)
- E. Acute hypomagnesemia
Malnutrition management Explanation: ***Acute hypercalcemia***
- **Hypercalcemia** causes decreased neuronal excitability by stabilizing nerve cell membranes, leading to **muscle weakness** and depressed deep tendon reflexes.
- The generalized weakness and hyporeflexia described are classic neurological manifestations of elevated calcium levels.
*Acute hypochloremia*
- **Hypochloremia** is often associated with gastrointestinal losses and can lead to **metabolic alkalosis** and muscle cramps but not generalized muscle weakness with depressed reflexes.
- Its direct effect on neuronal excitability to cause such profound weakness is not typical.
*Acute hypernatremia*
- **Hypernatremia** primarily causes neurological symptoms due to **cellular dehydration** and cerebral edema, leading to altered mental status, seizures, or coma.
- It does not typically present with generalized muscle weakness and depressed deep tendon reflexes due to decreased neuronal excitability in the manner described.
*Acute hyperkalemia*
- **Hyperkalemia** can cause muscle weakness and paralysis, but it often progresses to **cardiac arrhythmias** and is typically associated with **increased neuronal excitability** initially, before paralyzing effects.
- While it can lead to weakness, the generalized decreased excitability described is more characteristic of calcium imbalance.
*Acute hypomagnesemia*
- **Hypomagnesemia** typically increases neuronal excitability, leading to symptoms like **muscle cramps**, tremors, hyperreflexia, and even seizures.
- It does not cause generalized muscle weakness with depressed deep tendon reflexes as a primary manifestation of decreased neuronal excitability.
Malnutrition management US Medical PG Question 5: A 17-year-old girl with a BMI of 14.5 kg/m2 is admitted to the hospital for the treatment of anorexia nervosa. The patient is administered intravenous fluids and is supplied with 1,600 calories daily with an increase of 200 calories each day. On day 5 of treatment, the patient manifests symptoms of weakness and confusion, and dark brown urine. Which of the following clinical conditions is the most likely cause of the patient's symptoms?
- A. Hypercalcemia
- B. Thiamine deficiency
- C. Hyperkalemia
- D. Hypophosphatemia (Correct Answer)
- E. Hypermagnesemia
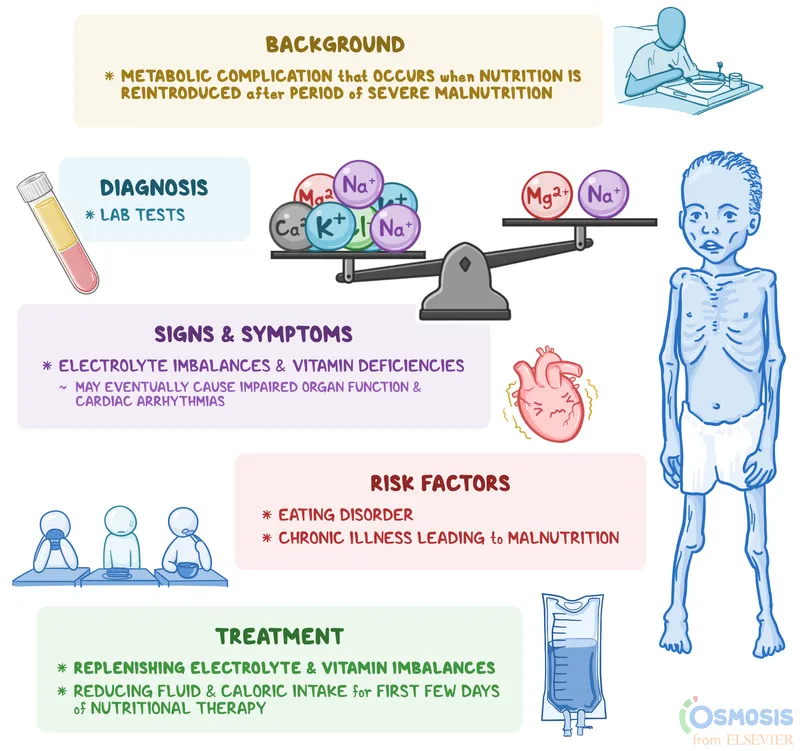
Malnutrition management Explanation: ***Hypophosphatemia***
- The symptoms of **weakness, confusion, and dark brown urine** during refeeding in an anorexic patient strongly suggest **refeeding syndrome**, which is mainly driven by severe **hypophosphatemia**. The dark brown urine indicates **rhabdomyolysis**, a classic sign of severe electrolyte disturbances in this context.
- Rapid reintroduction of carbohydrates leads to an insulin surge, driving **phosphate, potassium, and magnesium** intracellularly. This causes a precipitous drop in serum phosphate levels, impairing ATP production and cellular function, leading to muscular weakness, cardiac dysfunction, and neurological symptoms.
*Hypercalcemia*
- **Hypercalcemia** is not typically a direct complication of refeeding syndrome and would not explain the constellation of symptoms, especially **rhabdomyolysis**.
- Symptoms usually include **constipation, polyuria, polydipsia, and bone pain**, which are different from those presented.
*Thiamine deficiency*
- **Thiamine deficiency** can occur in refeeding syndrome, leading to **Wernicke-Korsakoff syndrome** marked by confusion, ataxia, and ophthalmoplegia. However, it does not typically cause **dark brown urine** due to rhabdomyolysis, which is a hallmark of severe hypophosphatemia.
- While possible, it is less likely to be the *most likely* single cause for all presented symptoms, especially the musculoskeletal and renal manifestations.
*Hyperkalemia*
- **Hyperkalemia** is unlikely in refeeding syndrome; instead, **hypokalemia** is a common electrolyte disturbance as potassium shifts intracellularly with insulin secretion.
- Symptoms of hyperkalemia include **cardiac arrhythmias and muscle weakness**, but it does not cause rhabdomyolysis or dark urine in this context.
*Hypermagnesemia*
- **Hypermagnesemia** is also not a typical complication of refeeding syndrome; instead, **hypomagnesemia** can occur due to intracellular shifting.
- Symptoms of hypermagnesemia include **hypotension, bradycardia, muscle weakness, and respiratory depression**, which do not align with the patient's presentation.
Malnutrition management US Medical PG Question 6: A 24-year-old man is running a marathon (42.2 km) on a hot summer day and collapses about halfway through the run. Emergency personnel are called and find him having a seizure. As the seizure subsides, the runner exhibits confusion, dry lips and decreased skin turgor. On the way to the emergency department, he denies taking medication or having a history of seizures. He reports that he drank water, but he admits that it was probably not enough. Which of the following would be the next best step in the management of this patient?
- A. 0.9% NaCl (Correct Answer)
- B. Relcovaptan
- C. Furosemide
- D. Indapamide
- E. 3% NaCl
Malnutrition management Explanation: ***0.9% NaCl***
- The patient presents with signs of **volume depletion** (dry lips, decreased skin turgor) and **exercise-associated collapse with seizure**.
- While the seizure raises concern for **exercise-associated hyponatremia (EAH)**, **initial management** requires stabilization with **isotonic saline (0.9% NaCl)** for volume resuscitation.
- Without laboratory confirmation of sodium levels, **isotonic saline is the safest initial choice** as it provides volume support without risking rapid sodium shifts.
- If severe hyponatremia is later confirmed with labs, treatment can be escalated to hypertonic saline with careful monitoring.
*3% NaCl*
- **Hypertonic saline (3% NaCl)** is indicated for **severe, symptomatic hyponatremia** with neurological manifestations (seizures, altered mental status).
- While this patient has a seizure suggesting possible severe hyponatremia, **hypertonic saline should only be administered after laboratory confirmation** of serum sodium levels.
- Administering 3% NaCl without labs risks **overcorrection** and **osmotic demyelination syndrome** if the diagnosis is incorrect or correction is too rapid.
- Initial stabilization with isotonic saline is safer until sodium levels are known.
*Relcovaptan*
- Relcovaptan is a **vasopressin V2 receptor antagonist** used for treating **chronic hyponatremia** (e.g., SIADH, heart failure).
- It is **not appropriate for acute emergency management** of suspected exercise-associated hyponatremia with active seizures.
- The patient requires immediate fluid resuscitation and stabilization, not oral chronic therapy.
*Furosemide*
- **Furosemide** is a loop diuretic that promotes excretion of water and electrolytes, which would **worsen hypovolemia**.
- It is **contraindicated** in a patient presenting with signs of volume depletion and potential heatstroke.
*Indapamide*
- **Indapamide** is a thiazide-like diuretic that would promote further diuresis and **exacerbate dehydration**.
- Thiazide diuretics can also cause hyponatremia, making this particularly inappropriate in this clinical context.
Malnutrition management US Medical PG Question 7: An 8-year-old boy is brought to the emergency department with severe dyspnea, fatigue, and vomiting. His mother reports that he has been lethargic for the last several days with an increase in urine output. She thinks he may even be losing weight, despite eating and drinking more than normal for the last couple weeks. Laboratory results are notable for glucose of 440, potassium of 5.8, pH of 7.14 and HCO3 of 17. After administrating IV fluids and insulin, which of the following would you expect?
- A. Increase in anion gap
- B. Increase in serum glucose
- C. Decrease in serum potassium (Correct Answer)
- D. Decrease in pH
- E. Decrease in serum bicarbonate
Malnutrition management Explanation: ***Decrease in serum potassium***
- **Insulin therapy** drives **potassium** into cells, as it stimulates the **Na+/K+ ATPase pump**, leading to a decrease in serum potassium levels.
- The initial **hyperkalemia** (potassium 5.8) is due to extracellular fluid shifts and acidosis, which will correct as **DKA** resolves with treatment.
*Increase in anion gap*
- The presented patient has **diabetic ketoacidosis (DKA)**, which is characterized by a **high anion gap metabolic acidosis** (evidenced by low pH and bicarbonate).
- Treatment with **IV fluids and insulin** aims to resolve the ketoacidosis, which would consequently lead to a **decrease** in the **anion gap**, not an increase.
*Increase in serum glucose*
- The primary goal of **IV fluids and insulin** in **DKA** is to lower the critically high **serum glucose** levels by promoting glucose uptake into cells and inhibiting hepatic glucose production.
- Therefore, one would expect a **decrease** in serum glucose, not an increase, as treatment progresses.
*Decrease in pH*
- The patient's initial pH of 7.14 indicates **acidosis**, a hallmark of **DKA**.
- **Insulin therapy** and **fluid resuscitation** will resolve the ketoacidosis, leading to an **increase** in **pH** towards normal, not a further decrease.
*Decrease in serum bicarbonate*
- The patient already presents with **decreased serum bicarbonate** (17 mEq/L), which is consistent with **metabolic acidosis** due to DKA.
- Treatment with **fluids and insulin** will correct the acidosis by reducing ketone production, leading to an **increase** in **serum bicarbonate**, not a further decrease.
Malnutrition management US Medical PG Question 8: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Malnutrition management Explanation: ***Constitutional growth delay***
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Malnutrition management US Medical PG Question 9: A 14-year-old girl is brought to the physician for evaluation of her short stature. She was born at term, and her birth length was normal. She has not yet attained menarche. Her mother is 162 cm (5 ft 4 in) tall and her father is 177 cm (5 ft 10 in) tall. She is at the 3rd percentile for height and 40th percentile for weight. Vital signs are within normal limits. Breast and pubic hair development are Tanner stage 2. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in diagnosis?
- A. Measurement of serum thyroid-stimulating hormone concentration
- B. Measurement of serum insulin-like growth factor concentration
- C. Genetic karyotyping
- D. X-ray of the hand and wrist (Correct Answer)
- E. MRI of the brain
Malnutrition management Explanation: ***X-ray of the hand and wrist***
- An **X-ray of the hand and wrist** is used to determine **bone age**, which is crucial for evaluating short stature by comparing skeletal maturity to chronological age.
- In a 14-year-old girl with short stature and delayed puberty (Tanner stage 2, no menarche), a **delayed bone age** would suggest a constitutional growth delay, which is a common cause of short stature.
*Measurement of serum thyroid-stimulating hormone concentration*
- While **hypothyroidism** can cause short stature and delayed puberty, there are no other clinical signs (e.g., fatigue, weight gain, cold intolerance) to strongly suggest this diagnosis in this patient.
- A TSH measurement would typically be considered after initial screening tests, or if other symptoms are present.
*Measurement of serum insulin-like growth factor concentration*
- **Insulin-like growth factor 1 (IGF-1)** is used to screen for **growth hormone deficiency**, but this is usually evaluated after bone age assessment.
- Growth hormone deficiency is less likely without other symptoms or a clear growth curve deceleration.
*Genetic karyotyping*
- **Genetic karyotyping** is indicated if **Turner syndrome** (XO karyotype) is suspected, which could cause short stature and primary amenorrhea.
- However, the patient's normal birth length and lack of characteristic dysmorphic features make it a less immediate first step compared to bone age assessment.
*MRI of the brain*
- An **MRI of the brain** would be considered if there was suspicion of a **pituitary or hypothalamic tumor** causing growth hormone deficiency or delayed puberty.
- There are no specific neurological symptoms or signs of increased intracranial pressure to warrant a brain MRI as the initial diagnostic step in this case.
Malnutrition management US Medical PG Question 10: A 69-year-old man is brought to the emergency room by his daughter due to confusion. She reports that her father did not remember who she was yesterday, and his refrigerator was completely empty when she tried to make him lunch. She states that he was acting like himself when she visited him last week. She also notes that he has struggled with alcoholism for many years and has not seen a doctor in over two decades. She is unsure if he has any other chronic medical conditions. In the emergency room, the patient’s temperature is 101.2°F (38.4°C), pulse is 103/min, respirations are 22/min, and O2 saturation is 92% on room air. His BMI is 17.1 kg/m^2. Physical exam reveals an extremely thin and frail man who is not oriented to person, place, or time. As he is being examined, he becomes unresponsive and desaturates to 84%. He is intubated and admitted to the intensive care unit for what is found to be pneumonia, and the patient is started on total parental nutrition as he is sedated and has a history of aspiration from a prior hospitalization. Two days later, physical exam is notable for new peripheral edema. Laboratory tests at that time reveal the following:
Serum:
Na+: 133 mEq/L
Cl-: 101 mEq/L
K+: 2.4 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 124 mg/dL
Creatinine: 1.1 mg/dL
Phosphate: 1.1 mg/dL
Mg2+: 1.0 mg/dL
Which of the following could have prevented the complication seen in this patient?
- A. Initiation of furosemide
- B. Use of low-sugar TPN
- C. Use of enteral nutrition
- D. Initiation of intermittent dialysis
- E. Slow initiation of total parenteral nutrition (TPN) (Correct Answer)
Malnutrition management Explanation: ***Slow initiation of total parenteral nutrition (TPN)***
- This patient likely developed **refeeding syndrome**, which is characterized by severe electrolyte shifts (especially **hypophosphatemia**, **hypokalemia**, and **hypomagnesemia**) and fluid retention (peripheral edema) upon rapid reintroduction of nutrition to severely malnourished individuals.
- A **slow and gradual introduction of TPN** would have allowed the body to adapt to the increased metabolic demands, preventing the sudden intracellular shift of electrolytes and subsequent depletion in the serum.
*Initiation of furosemide*
- Furosemide is a **loop diuretic** primarily used to treat fluid overload and edema by increasing renal excretion of water and electrolytes.
- While it could address the peripheral edema, it would not correct the underlying electrolyte imbalances of refeeding syndrome and could potentially worsen them (e.g., contributing to **hypokalemia**).
*Use of low-sugar TPN*
- Refeeding syndrome is triggered by the shift from fat metabolism to carbohydrate metabolism, leading to increased insulin secretion and subsequent intracellular movement of electrolytes.
- While a lower glucose load might slightly mitigate the insulin response, it does not address the core issue of rapid nutrient repletion in a severely malnourished state, and the absolute amount of carbohydrates would still be significant in TPN.
*Use of enteral nutrition*
- **Enteral nutrition** (feeding via the gastrointestinal tract) is generally preferred over TPN when feasible, as it helps maintain gut integrity and has a lower risk of certain complications.
- However, if initiated too rapidly in a severely malnourished patient, enteral nutrition can also precipitate refeeding syndrome, as the metabolic shifts are triggered by carbohydrate repletion regardless of the delivery route.
*Initiation of intermittent dialysis*
- **Intermittent dialysis** is a renal replacement therapy used for acute or chronic kidney failure to remove waste products and excess fluid.
- This patient's creatinine and BUN are only mildly elevated for someone with pneumonia and dehydration, indicating **no clear indication for dialysis**; phosphorus and magnesium could be corrected with supplementation.
More Malnutrition management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 in a child with color-coded tape)
in a child with color-coded tape)