Iron deficiency and anemia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Iron deficiency and anemia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
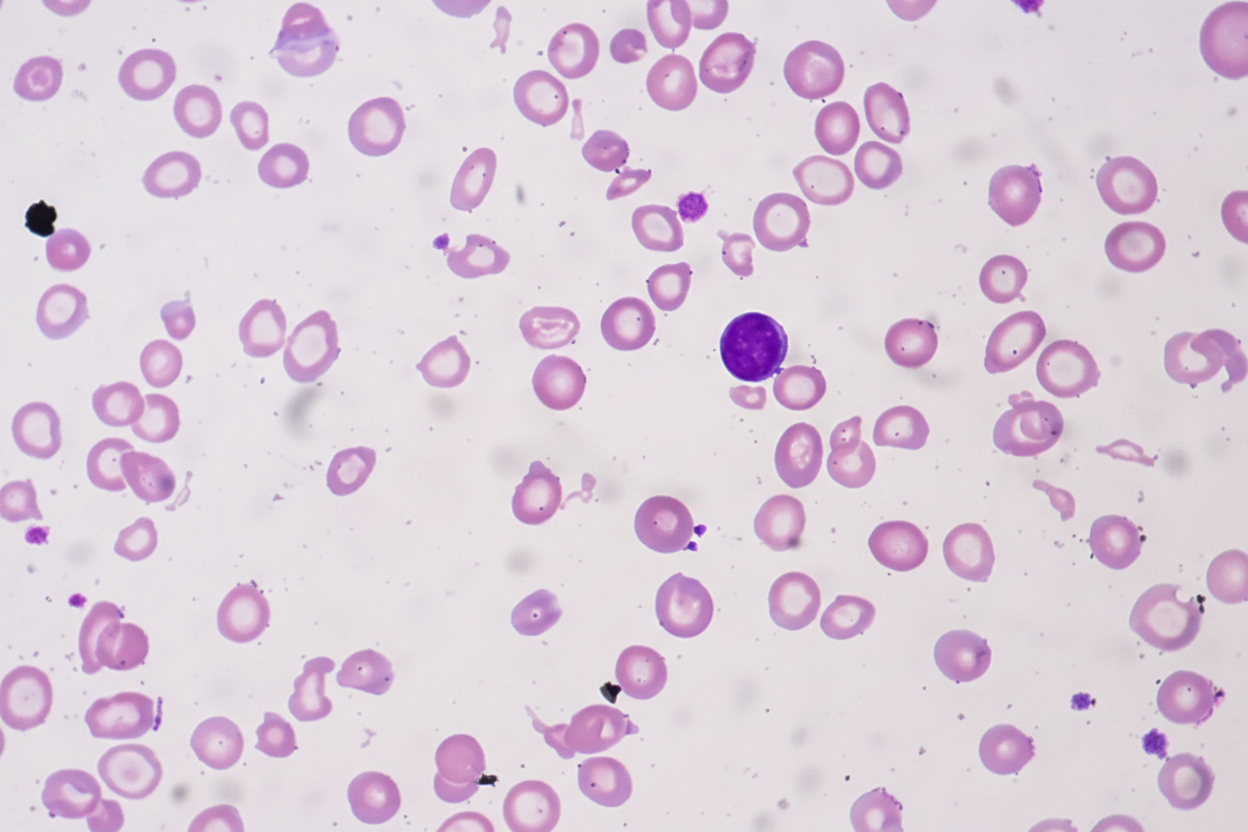
Iron deficiency and anemia US Medical PG Question 1: A 25-year-old African-American woman visits the doctor’s office complaining of fatigue for a couple of months. She says that she feels exhausted by the end of the day. She works as a dental assistant and is on her feet most of the time. However, she eats well and also tries to walk for 30 minutes every morning. She also says that she sometimes feels breathless and has to gasp for air, especially when she is walking or jogging. Her past medical history is insignificant, except for occasional bouts of cold during the winters. Her physical exam findings are within normal limits except for moderate conjunctival pallor. Complete blood count results and iron profile are as follows:
Hemoglobin 9 g/dL
Hematocrit 28.5%
RBC count 5.85 x 106/mm3
WBC count 5,500/mm3
Platelet count 212,000/mm3
MCV 56.1 fl
MCH 20.9 pg/cell
MCHC 25.6 g/dL
RDW 11.7% Hb/cell
Serum iron 170 mcg/dL
Total iron-binding capacity (TIBC) 458 mcg/dL
Transferrin saturation 60%
A peripheral blood smear is given. When questioned about her family history of anemia, she says that all she remembers is her dad was never allowed to donate blood as he was anemic. Which of the following most likely explains her cell counts and blood smear results?
- A. Thalassemia (Correct Answer)
- B. Iron-deficiency anemia
- C. B12 deficiency
- D. Hemolysis
- E. Folate deficiency
Iron deficiency and anemia Explanation: ***Thalassemia***
- The patient presents with **microcytic, hypochromic anemia** (low MCV, MCH, MCHC) despite elevated iron stores, which is characteristic of thalassemia.
- The **elevated RBC count** (5.85 x 10^6/mm³) in the presence of anemia (hemoglobin 9 g/dL) is a hallmark of thalassemia, as the body attempts to compensate for ineffective erythropoiesis.
- The **elevated serum iron (170 mcg/dL) and high transferrin saturation (60%)** indicate iron overload, not iron deficiency, which occurs in thalassemia due to ineffective erythropoiesis and increased iron absorption.
- The **low RDW (11.7%)** indicates uniform cell size despite microcytosis, typical of thalassemia (vs. high RDW in iron deficiency).
- **Positive family history** (father was anemic and couldn't donate blood) supports an inherited disorder.
*Iron-deficiency anemia*
- This condition typically presents with **low serum iron**, **high TIBC**, and **low transferrin saturation** (<20%), which contradicts the patient's iron profile showing elevated iron and high transferrin saturation (60%).
- While iron-deficiency anemia also causes **microcytic, hypochromic RBCs**, the RBC count would be low or normal (not elevated), and RDW would be elevated (>14%) due to anisocytosis.
*B12 deficiency*
- **B12 deficiency** causes **macrocytic anemia** (high MCV >100 fl), which is inconsistent with the patient's low MCV (56.1 fl).
- It also often presents with neurological symptoms (peripheral neuropathy, subacute combined degeneration), which are absent in this case.
*Hemolysis*
- While hemolysis can cause anemia and fatigue, it is usually associated with elevated **reticulocyte count**, **indirect bilirubin**, and **LDH**, and decreased **haptoglobin**, none of which are indicated here.
- Hemolysis typically presents with **normocytic anemia** (normal MCV), not the marked **microcytosis** (MCV 56.1 fl) seen in this patient.
*Folate deficiency*
- Similar to B12 deficiency, **folate deficiency** leads to **macrocytic anemia** (high MCV >100 fl), which is not observed in this patient with MCV of 56.1 fl.
- Folate deficiency does not cause neurological symptoms (unlike B12 deficiency), but the **macrocytic** red cell morphology is the key differentiator here.
Iron deficiency and anemia US Medical PG Question 2: A 44-year-old male immigrant presents to his primary care physician for a new patient visit. The patient reports chronic fatigue but states that he otherwise feels well. His past medical history is not known, and he is not currently taking any medications. The patient admits to drinking 7 alcoholic beverages per day and smoking 1 pack of cigarettes per day. His temperature is 99.4°F (37.4°C), blood pressure is 157/98 mmHg, pulse is 99/min, respirations are 18/min, and oxygen saturation is 100% on room air. Physical exam demonstrates mild pallor but is otherwise not remarkable. Laboratory studies are ordered as seen below.
Hemoglobin: 9 g/dL
Hematocrit: 33%
Leukocyte count: 6,500/mm^3 with normal differential
Platelet count: 190,000/mm^3
Mean corpuscular volume (MCV): 60 femtoliters
Free iron: 272 mcg/dL
Total iron binding capacity (TIBC): 175 mcg/dL
Ferritin: 526 ng/mL
Reticulocyte count: 2.8%
Which of the following is the most likely diagnosis?
- A. Folate deficiency
- B. Beta-thalassemia (Correct Answer)
- C. Iron deficiency
- D. B12 deficiency
- E. Hemolytic anemia
Iron deficiency and anemia Explanation: ***Beta-thalassemia***
- The patient presents with **microcytic anemia** (MCV 60 fL) and **elevated ferritin**, **high free iron**, and **low TIBC**, which are characteristic of thalassemia due to ineffective erythropoiesis and iron overload.
- A **reticulocyte count of 2.8%** (elevated for the degree of anemia) indicates the bone marrow is attempting to compensate, consistent with a hemolytic process like thalassemia.
*Folate deficiency*
- Folate deficiency typically causes **macrocytic anemia** (elevated MCV), which is not seen here; the patient has microcytic anemia.
- Alcohol abuse can cause folate deficiency, but the lab values for iron studies and MCV are inconsistent with this diagnosis.
*Iron deficiency*
- Iron deficiency anemia would present with **low ferritin**, **low free iron**, and **high TIBC**, which are opposite to the patient's lab results.
- Although the patient has microcytic anemia, the iron study profile rules out iron deficiency.
*B12 deficiency*
- Vitamin B12 deficiency also causes **macrocytic anemia** (elevated MCV), often with neurological symptoms, neither of which are observed in this patient.
- The patient's microcytic anemia and iron study results contradict a diagnosis of B12 deficiency.
*Hemolytic anemia*
- While beta-thalassemia is a form of hemolytic anemia, the term "hemolytic anemia" alone is too broad and does not specify the underlying cause, especially with the provided iron studies and MCV.
- Other common causes of hemolytic anemia, like autoimmune hemolytic anemia or G6PD deficiency, would require different diagnostic presentations or specific tests not consistent with the given lab values.
Iron deficiency and anemia US Medical PG Question 3: A 2-year-old boy is brought to the physician for generalized fatigue and multiple episodes of abdominal pain and vomiting for the past week. His last bowel movement was 4 days ago. He has been having behavioral problems at home for the past few weeks as well. He can walk up stairs with support and build a tower of 3 blocks. He cannot use a fork. He does not follow simple instructions and speaks in single words. His family emigrated from Bangladesh 6 months ago. He is at the 40th percentile for height and weight. His temperature is 37°C (98.6°F), pulse is 115/min, and blood pressure is 84/45 mm Hg. Examination shows pale conjunctivae and gingival hyperpigmentation. His hemoglobin concentration is 10.1 g/dL, mean corpuscular volume is 68 μm3, and mean corpuscular hemoglobin is 24.5 pg/cell. The patient is most likely going to benefit from administration of which of the following?
- A. Vitamin B12 and folate
- B. Penicillamine
- C. Iron
- D. Thiosulfate and hydroxocobalamin
- E. Succimer and calcium disodium edetate (Correct Answer)
Iron deficiency and anemia Explanation: ***Succimer and calcium disodium edetate***
- This patient presents with symptoms such as **abdominal pain**, **vomiting**, **constipation**, **generalized fatigue**, and **behavioral problems**, along with **gingival hyperpigmentation** and **microcytic anemia** (Hb 10.1 g/dL, MCV 68 μm3, MCH 24.5 pg/cell). These are classic signs of **lead poisoning**.
- **Succimer (DMSA)** and **calcium disodium edetate (CaNa2EDTA)** are chelation therapies used to treat lead poisoning by binding to lead and promoting its excretion. They are indicated for elevated blood lead levels, especially in symptomatic children.
*Vitamin B12 and folate*
- These are given for **megaloblastic anemia**, characterized by **macrocytic red blood cells** (high MCV), which is not seen here as the MCV is low (68 μm3).
- Symptoms of B12 deficiency (e.g., neurological deficits, glossitis) and folate deficiency (e.g., fatigue, megaloblastic changes) are distinct from the patient's presentation.
*Penicillamine*
- **Penicillamine** is a chelating agent primarily used for **Wilson's disease** (copper overload) or **cystinuria**.
- While it has some chelating properties for heavy metals, it is not the first-line or most effective treatment for lead poisoning and has a different side-effect profile.
*Iron*
- **Iron supplementation** is used to treat **iron deficiency anemia**, a common cause of microcytic anemia. However, the patient's constellation of symptoms, including neurological and gastrointestinal issues, and gingival hyperpigmentation, strongly points away from simple iron deficiency as the primary diagnosis.
- Giving iron in the presence of lead poisoning without addressing lead can mask the underlying issue and not resolve the more systemic effects.
*Thiosulfate and hydroxocobalamin*
- **Sodium thiosulfate** and **hydroxocobalamin** are antidotes used for **cyanide poisoning**.
- The patient's symptoms are inconsistent with cyanide exposure, which typically involves rapid onset of severe metabolic acidosis, cardiovascular collapse, and respiratory arrest.
Iron deficiency and anemia US Medical PG Question 4: A 2-month-old girl is brought to the physician for a well-child examination. She was born at 32 weeks' gestation and weighed 1616 g (3 lb 9 oz); she currently weighs 2466 g (5 lb 7 oz). She is exclusively breastfed and receives vitamin D supplementation. Physical examination shows no abnormalities apart from low height and weight. This patient is at increased risk for which of the following complications?
- A. Iron deficiency anemia (Correct Answer)
- B. Hemorrhage
- C. Scurvy
- D. Subacute combined degeneration
- E. Intussusception
Iron deficiency and anemia Explanation: ***Iron deficiency anemia***
- Preterm infants have **lower iron stores** at birth due to reduced placental transfer in the third trimester.
- Their rapid growth rate and exclusive breastfeeding (breast milk has low iron content) further increase their risk of **iron deficiency anemia**.
*Hemorrhage*
- While preterm infants are at higher risk for certain hemorrhages (e.g., intraventricular hemorrhage), this typically occurs in the **immediate neonatal period** and risk significantly decreases by 2 months of age.
- Hemorrhage is not a common long-term complication unique to a 2-month-old preterm infant without additional risk factors.
*Scurvy*
- Scurvy is caused by **vitamin C deficiency**, which is typically not a concern in breastfed infants as breast milk provides adequate vitamin C.
- The primary deficiency risk addressed by supplementation in breastfed infants is vitamin D, not vitamin C.
*Subacute combined degeneration*
- This condition is caused by **vitamin B12 deficiency**, leading to demyelination of the spinal cord.
- While possible in infants of vegan mothers, it is unlikely in a breastfed infant without specific dietary restrictions in the mother.
*Intussusception*
- Intussusception is a condition where one segment of the intestine telescopes into another, usually occurring between **3 months and 3 years of age**.
- It is not specifically linked to prematurity or low birth weight as an increased long-term risk.
Iron deficiency and anemia US Medical PG Question 5: A 4-year-old boy is brought to the physician for the evaluation of fatigue since he returned from visiting family in South Africa one week ago. The day after he returned, he had fever, chills, and diffuse joint pain for 3 days. His symptoms improved with acetaminophen. He was born at term and has been healthy. His immunizations are up-to-date. His temperature is 37.6°C (99.68°F), pulse is 100/min, and blood pressure is 100/60 mm Hg. Examination shows conjunctival pallor. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.8 g/dL
Mean corpuscular volume 68 μm3
Red cell distribution width 14% (N = 13%–15%)
Hemoglobin A2 6% (N < 3.5%)
A peripheral smear shows microcytic, hypochromic erythrocytes, some of which have a darkly stained center and peripheral rim, separated by a pale ring. Which of the following is the most appropriate next step in the management of this patient?
- A. Oral pyridoxine
- B. Iron supplementation
- C. Reassurance (Correct Answer)
- D. Folic acid therapy
- E. Oral succimer
Iron deficiency and anemia Explanation: ***Reassurance***
- The patient's presentation with **microcytic anemia**, elevated **Hemoglobin A2 (6%)**, and **target cells** on peripheral smear is highly suggestive of **beta-thalassemia trait** (minor). This genetic condition is more common in individuals with Mediterranean, African, Middle Eastern, or South Asian ancestry.
- Beta-thalassemia trait is a **benign condition** that does not typically require specific medical intervention. The mild anemia does not usually cause significant symptoms or complications, and patients can live normal lives without treatment.
- The elevated HbA2 is the key diagnostic finding that distinguishes thalassemia trait from iron deficiency anemia.
*Oral pyridoxine*
- **Pyridoxine (Vitamin B6)** supplementation is indicated for **sideroblastic anemia**, which can also cause microcytic anemia.
- However, sideroblastic anemia typically presents with **ring sideroblasts** in the bone marrow and does not have the characteristic elevated HbA2 seen in beta-thalassemia trait.
*Iron supplementation*
- **Iron deficiency anemia** is a common cause of microcytic hypochromic anemia, but it would present with **low ferritin** and **low or normal HbA2** (not elevated).
- In this case, iron supplementation would not be appropriate and could potentially be harmful due to the risk of **iron overload** in thalassemia syndromes, even in the trait form.
- The elevated HbA2 and normal RDW help distinguish thalassemia trait from iron deficiency.
*Folic acid therapy*
- **Folic acid** is primarily used in the management of **macrocytic anemias** or in conditions with high red blood cell turnover, such as **hemolytic anemias** or major thalassemia syndromes requiring chronic transfusions.
- It is not indicated for beta-thalassemia trait, which is a microcytic anemia with normal red blood cell turnover and no significant hemolysis.
*Oral succimer*
- **Succimer** is a chelating agent used to treat **lead poisoning**, which can cause microcytic anemia with basophilic stippling.
- There are no clinical or laboratory findings in this patient (e.g., **basophilic stippling**, developmental delays, neurological symptoms, abdominal pain) to suggest lead poisoning.
Iron deficiency and anemia US Medical PG Question 6: A 55-year-old woman presents with fatigue. She says her symptoms are present throughout the day and gradually started 4 months ago. Her past medical history is significant for rheumatoid arthritis–treated with methotrexate, and diabetes mellitus type 2–treated with metformin. The patient is afebrile, and her vital signs are within normal limits. A physical examination reveals pallor of the mucous membranes. Initial laboratory tests show hemoglobin of 7.9 g/dL, hematocrit of 22%, and mean corpuscular volume of 79 fL. Which of the following is the best next diagnostic step in this patient?
- A. Serum ferritin level and total iron-binding capacity (TIBC)
- B. Serum ferritin and serum iron levels
- C. Serum ferritin and soluble transferrin receptor levels (Correct Answer)
- D. Serum iron level
- E. Serum ferritin level
Iron deficiency and anemia Explanation: ***Serum ferritin and soluble transferrin receptor levels***
- This patient has **anemia** (hemoglobin 7.9 g/dL) with **microcytic** (MCV 79 fL) and **hypochromic** features, suggesting either **iron deficiency anemia (IDA)** or **anemia of chronic disease (ACD)**. Given her history of **rheumatoid arthritis**, ACD is highly likely, but co-existing IDA needs to be excluded.
- **Serum ferritin** is an acute-phase reactant, so it can be elevated in ACD masking a co-existing iron deficiency. **Soluble transferrin receptor (sTfR)** levels are increased in IDA and remain normal or only mildly elevated in ACD, making it a reliable marker to differentiate between these two conditions when ferritin is uninterpretable due to inflammation.
*Serum ferritin level and total iron-binding capacity (TIBC)*
- While these tests are useful for diagnosing iron deficiency, **ferritin** can be falsely elevated in the context of inflammation (e.g., from **rheumatoid arthritis**), making it unreliable for diagnosing IDA in this patient.
- **TIBC** can be decreased in ACD, complicating its interpretation for IDA when inflammation is present.
*Serum ferritin and serum iron levels*
- As mentioned, **serum ferritin** is an acute-phase reactant and may be elevated due to **rheumatoid arthritis**, potentially masking **iron deficiency**.
- **Serum iron levels** fluctuate significantly and are not a reliable standalone indicator for iron status, especially in the context of chronic disease.
*Serum iron level*
- **Serum iron levels** are highly variable and not sufficient for diagnosing **iron deficiency** or differentiating it from **anemia of chronic disease**.
- A low serum iron can be seen in both IDA and ACD but does not provide definitive diagnostic information on its own.
*Serum ferritin level*
- Measuring **serum ferritin** alone is insufficient because it is an **acute-phase reactant** that can be elevated due to the patient's **rheumatoid arthritis**, even if she has co-existing **iron deficiency anemia**.
- A normal or high ferritin level in this context does not rule out **iron deficiency**.
Iron deficiency and anemia US Medical PG Question 7: An 11-year-old boy presents to his pediatrician for a wellness checkup. The child is an immigrant, and this is his first visit. The patient is in the 99th percentile for height and 50th percentile for weight. The child is struggling in school, and basic cognitive testing suggests he is moderately mentally disabled. His temperature is 99.5°F (37.5°C), blood pressure is 107/68 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Laboratory values are obtained and shown below.
Hemoglobin: 9 g/dL
Hematocrit: 30%
MCV: 110 fL
Leukocyte count: 5,500/mm^3 with normal differential
Platelet count: 192,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 90 mg/dL
Creatinine: 1.0 mg/dL
Ca2+: 10.0 mg/dL
AST: 12 U/L
ALT: 10 U/L
The patient is started on vitamin B9 and B12. Which of the following interventions could decrease the risk for cardiac complications the most in this patient?
- A. Folic acid supplementation
- B. Homocysteine level monitoring
- C. Iron supplementation
- D. Pyridoxine (Vitamin B6) (Correct Answer)
- E. No additional interventions needed
Iron deficiency and anemia Explanation: ***Pyridoxine (Vitamin B6)***
- This patient has **homocystinuria** (tall stature, mental disability, macrocytic anemia) and is already on **folate (B9) and B12** supplementation
- **Pyridoxine (B6)** is the most important additional intervention because it is a cofactor for **cystathionine β-synthase**, the enzyme deficient in classical homocystinuria
- Approximately **50% of homocystinuria patients are B6-responsive**, meaning pyridoxine can dramatically reduce homocysteine levels
- The complete treatment regimen for homocystinuria includes **B6, B9 (folate), and B12** - since B9 and B12 are already started, **B6 is the critical missing intervention**
- Reducing homocysteine levels decreases risk of **thromboembolism, stroke, and cardiovascular disease**, which are the major causes of morbidity and mortality in homocystinuria
*Folic acid supplementation*
- The patient is **already receiving vitamin B9 (folic acid)** as stated in the question stem
- While folic acid is essential for lowering homocysteine through the remethylation pathway, it is already being administered
- This option would be redundant
*Homocysteine level monitoring*
- Monitoring homocysteine is important for **assessing treatment response** but is a diagnostic tool, not an intervention
- It does not directly decrease cardiac risk, though it helps guide therapy
- The question asks for an intervention that decreases risk, not a monitoring strategy
*Iron supplementation*
- The patient has **macrocytic anemia (MCV 110 fL)**, not microcytic anemia
- Macrocytic anemia suggests **folate/B12 deficiency**, not iron deficiency
- Iron supplementation would not address the underlying cause (elevated homocysteine) or reduce cardiac complications
- In fact, unnecessary iron supplementation can cause harm
*No additional interventions needed*
- This is incorrect because the standard treatment for homocystinuria requires **all three B vitamins: B6, B9, and B12**
- Since only B9 and B12 have been started, **pyridoxine (B6) is still needed** to optimally reduce homocysteine and cardiac risk
- B6 is particularly important as it addresses the underlying enzyme deficiency in many patients
Iron deficiency and anemia US Medical PG Question 8: A 12-month-old boy is brought to the pediatrician for a routine examination. Past medical history is significant for a pyloric myomectomy at 2 months of age after a few episodes of projectile vomiting. He has reached all appropriate developmental milestones. He currently lives with his parents and pet cat in a house built in the 1990s. He was weaned off of breast milk at 6 months of age. He is a very picky eater, but drinks 5–6 glasses of whole milk a day. The patient's height and weight are in the 50th percentile for his age and sex. The vital signs are within normal limits except for the presence of slight tachycardia. Physical examination reveals an alert infant with a slight pallor. Abdomen is soft and nondistended. A grade 2/6 systolic ejection murmur is noted in the left upper sternal border. Which of the following will most likely be expected in this patient's laboratory results?
- A. Increased Hb S levels
- B. Decreased vitamin B12 levels
- C. Metabolic alkalosis
- D. Decreased hemoglobin (Correct Answer)
- E. Increased lead levels
Iron deficiency and anemia Explanation: ***Decreased hemoglobin***
- The patient's **picky eating habits**, combined with consuming **large amounts of whole milk** (low in iron), suggest a high risk for **iron deficiency anemia**.
- **Pallor** and **tachycardia** are classic signs of anemia, and a **systolic ejection murmur** can be a functional murmur due to increased cardiac output in anemic states.
*Increased Hb S levels*
- **Hb S** is characteristic of **sickle cell disease**, typically resulting in symptomatic episodes like **vaso-occlusive crises** and chronic anemia.
- The patient's presentation with dietary factors and pallor points more strongly to **nutritional anemia**, not a hemoglobinopathy.
*Decreased vitamin B12 levels*
- **Vitamin B12 deficiency** can cause megaloblastic anemia, but is usually associated with **neurological symptoms** and is less common at this age due to dietary intake habits.
- While prolonged exclusive breastfeeding could lead to B12 deficiency if the mother is deficient, the child was weaned at 6 months, and the symptoms are more consistent with iron deficiency.
*Metabolic alkalosis*
- **Metabolic alkalosis** was likely present during his previous illness involving **projectile vomiting** due to pyloric stenosis, but this has since been surgically corrected.
- His current symptoms of pallor and tachycardia are not indicative of an acid-base imbalance, but rather a circulatory issue like anemia.
*Increased lead levels*
- **Lead poisoning** can cause anemia and abdominal pain, but the patient's house was built in the 1990s (reducing the risk of lead paint exposure) and he has no history of pica.
- While it's a possibility, the specific dietary history of high milk intake and poor solid food consumption makes **iron deficiency anemia** a more direct and probable cause of his symptoms.
Iron deficiency and anemia US Medical PG Question 9: A 19-year-old African female refugee has been granted asylum in Stockholm, Sweden and has been living there for the past month. She arrived in Sweden with her 2-month-old infant, whom she exclusively breast feeds. Which of the following deficiencies is the infant most likely to develop?
- A. Vitamin E
- B. Vitamin A
- C. Vitamin C
- D. Vitamin B1
- E. Vitamin D (Correct Answer)
Iron deficiency and anemia Explanation: ***Vitamin D***
- The combination of exclusive breastfeeding, a 2-month-old infant, being of African heritage (darker skin), and living in a high-latitude region like Stockholm, Sweden, significantly increases the risk of **vitamin D deficiency**. Darker skin pigmentation reduces the efficiency of **cutaneous vitamin D synthesis** from sunlight, and insufficient sun exposure in northern latitudes further exacerbates this.
- Breast milk is a relatively poor source of **vitamin D**, and infants specifically require supplementation, especially when they have risk factors for deficiency such as being of African descent and living in an area with limited sunshine.
*Vitamin E*
- **Vitamin E deficiency** in infants is rare and typically seen in premature infants or those with severe malabsorption, neither of which is indicated in this scenario.
- While breast milk contains vitamin E, deficiency is not directly linked to geographic location, skin color, or a 2-month-old infant.
*Vitamin A*
- **Vitamin A deficiency** can be a concern in developing countries, but it is less likely to be the primary concern under these specific circumstances in a 2-month-old exclusively breastfed infant unless the mother herself is severely deficient.
- Breast milk usually provides adequate **vitamin A** if the mother's nutritional status is sufficient.
*Vitamin C*
- **Vitamin C deficiency** (scurvy) is rare in breastfed infants because breast milk typically contains adequate vitamin C if the mother has adequate dietary intake.
- Scurvy would be more likely in infants fed with improperly prepared formula or after 6 months if complementary foods lack vitamin C.
*Vitamin B1*
- **Vitamin B1 (thiamine) deficiency** is uncommon in exclusively breastfed infants in developed countries.
- It is often associated with maternal malnutrition in endemic areas or specific genetic disorders, which are not suggested here.
Iron deficiency and anemia US Medical PG Question 10: A 5-month-old male presents to the pediatrician with his mother for a well visit. The patient was born at 35 weeks gestation to a 30-year-old gravida 2 via vaginal delivery. The pregnancy and labor were uncomplicated. The patient required no resuscitation after delivery and was discharged from the hospital on day two of life. His mother now reports that the patient has been exclusively breastfed since birth, and she says that feedings have been going well, and that the patient appears satisfied afterwards. The patient feeds for 30 minutes every two hours and urinates 8-10 times per day. The patient’s mother reports that she eats a varied diet that includes animal products, but she worries that the patient is not meeting his nutritional needs with breastmilk alone. The patient’s height and weight at birth were in the 15th and 20th percentile, respectively. His height and weight are now in the 20th and 25th percentile, respectively. His temperature is 98.1°F (36.7°C), blood pressure is 58/46 mmHg, pulse is 128/min, and respirations are 34/min. On physical exam, the patient appears well-developed and well-nourished. He has mild conjunctival pallor.
Which of the following is the most appropriate guidance regarding this patient’s nutritional needs?
- A. Add cow's milk to his diet
- B. Supplement his diet with formula
- C. No changes are necessary to his diet
- D. Supplement his diet with iron and vitamin D (Correct Answer)
- E. Add pureed foods to his diet
Iron deficiency and anemia Explanation: ***Supplement his diet with iron and vitamin D***
- This 5-month-old infant, exclusively breastfed, requires **iron supplementation** because maternal iron stores are depleted by 4-6 months, and breast milk is a poor source of iron. Additionally, **Vitamin D supplementation** is crucial for all exclusively breastfed infants to prevent rickets.
- The presence of mild **conjunctival pallor** further suggests possible iron deficiency.
*Add cow's milk to his diet*
- **Cow's milk** should not be introduced before 12 months of age as it contains high protein and mineral content that can stress an infant's immature kidneys and can lead to **gastrointestinal bleeding**, insufficient iron absorption, and **iron-deficiency anemia**.
- It also has a low iron content and lacks the essential fatty acids necessary for proper infant development.
*Supplement his diet with formula*
- While formula contains iron and vitamin D, the mother reports that the baby is feeding well and appears satisfied, with appropriate weight gain (20th to 25th percentile) and frequent wet diapers, indicating **adequate nutrition from breast milk alone**.
- **Exclusive breastfeeding** is recommended for the first 6 months of life when feasible, and there is no clear indication that breast milk alone is insufficient for overall caloric and macronutrient needs here yet.
*No changes are necessary to his diet*
- This is incorrect because, despite adequate breastfeeding, **exclusive breastfed infants** like this one require supplementation with **iron and vitamin D** to meet their micronutrient needs.
- The mild conjunctival pallor also suggests a potential, or impending, deficiency that warrants intervention.
*Add pureed foods to his diet*
- The current recommendations suggest introducing solid foods, including pureed foods, around **6 months of age**, when the infant shows signs of developmental readiness.
- While the infant is close to 6 months, introducing solids at 5 months is typically not necessary if growth is appropriate and specific micronutrient deficiencies (like iron and vitamin D) can be addressed through supplementation.
More Iron deficiency and anemia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.