Food allergies and intolerances US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Food allergies and intolerances. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
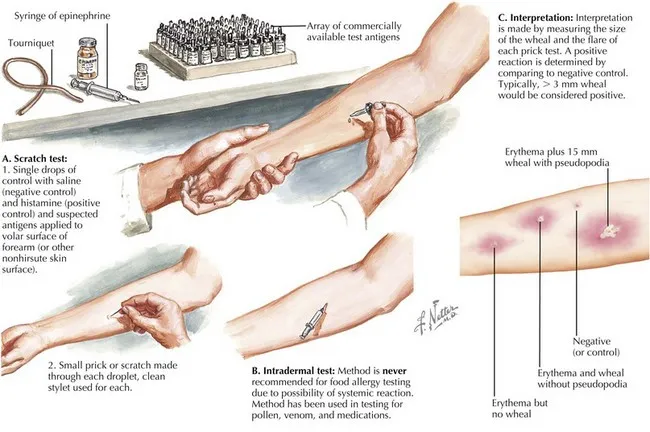
Food allergies and intolerances US Medical PG Question 1: A 7-year-old girl is brought to the physician by her father because of a dry cough, nasal congestion, and intermittent wheezing during the past 2 months. Since birth, she has had four upper respiratory tract infections that resolved without treatment and one episode of acute otitis media treated with antibiotics. She has a history of eczema. Her temperature is 37.1°C (98.7°F), and respirations are 28/min. Physical examination shows a shallow breathing pattern and scattered expiratory wheezing throughout both lung fields. Which of the following is the most appropriate next step in diagnosing this patient’s condition?
- A. Methacholine challenge test
- B. Chest x-ray
- C. Spirometry (Correct Answer)
- D. Serum IgE levels
- E. Arterial blood gas analysis
Food allergies and intolerances Explanation: ***Spirometry***
- Spirometry is the **initial diagnostic test** for asthma in children >5 years, showing **reversible airway obstruction** (decreased FEV1/FVC ratio that improves post-bronchodilator).
- The patient's symptoms (cough, wheezing, history of eczema suggesting atopy) are highly suggestive of **asthma**.
*Methacholine challenge test*
- This test is used to diagnose **asthma** when spirometry is normal but asthma is still clinically suspected.
- Given the patient's clear symptoms and physical findings of wheezing, **spirometry** is a more direct and less invasive initial step.
*Chest x-ray*
- A chest x-ray is generally not indicated in the routine diagnosis of **uncomplicated asthma**.
- It might be considered if there's suspicion of **pneumonia**, foreign body aspiration, or other lung pathology, which is not suggested here.
*Serum IgE levels*
- Elevated **IgE levels** can indicate atopic disease, which is associated with asthma, but they do not directly diagnose asthma or assess lung function.
- While the patient has a history of eczema (an atopic condition), measuring IgE levels is not the primary diagnostic test for **asthma**.
*Arterial blood gas analysis*
- **ABG analysis** is used to assess the severity of respiratory compromise and acid-base status, typically in acute, severe exacerbations of respiratory conditions.
- It is not a diagnostic tool for **chronic asthma** or for initial assessment unless the patient is in significant respiratory distress.
Food allergies and intolerances US Medical PG Question 2: A 23-year-old man presents to the emergency department with shortness of breath. The patient was at a lunch hosted by his employer. He started to feel his symptoms begin when he started playing football outside with a few of the other employees. The patient has a past medical history of atopic dermatitis and asthma. His temperature is 98.3°F (36.8°C), blood pressure is 87/58 mmHg, pulse is 150/min, respirations are 22/min, and oxygen saturation is 85% on room air. Which of the following is the best next step in management?
- A. Albuterol and prednisone
- B. IV epinephrine
- C. IV fluids and 100% oxygen
- D. Albuterol and norepinephrine
- E. IM epinephrine (Correct Answer)
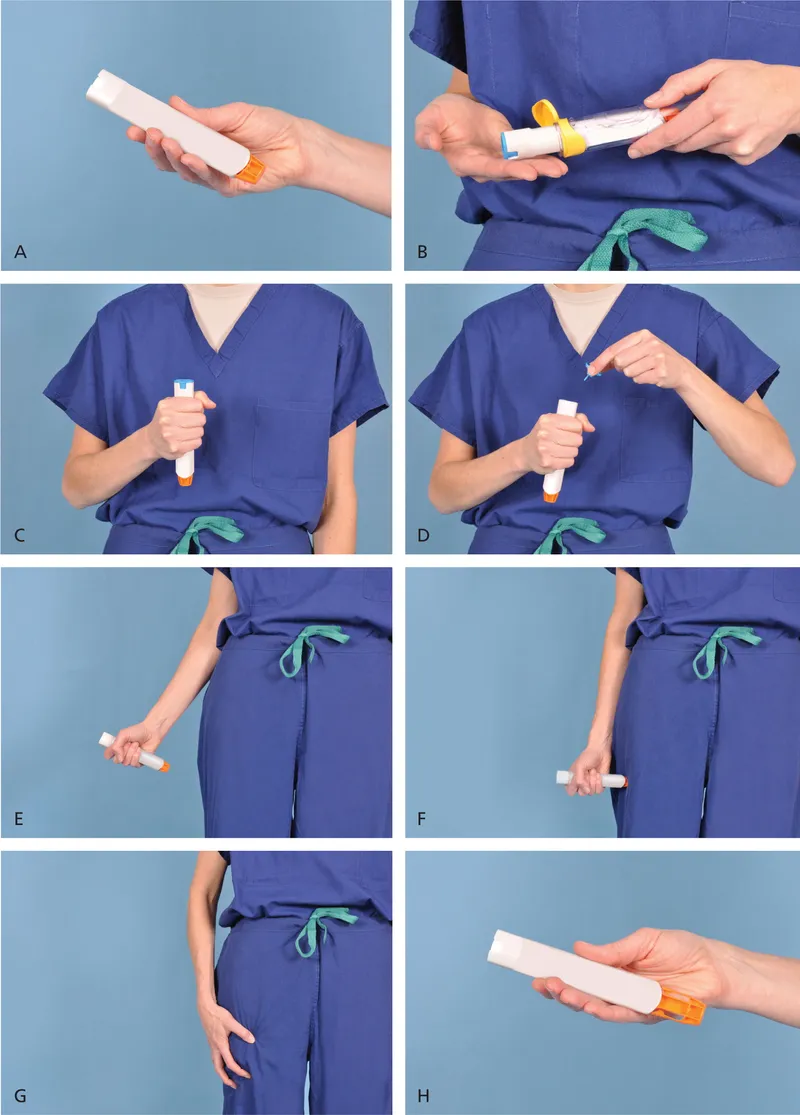
Food allergies and intolerances Explanation: ***IM epinephrine***
- The patient presents with **signs of anaphylaxis**, including acute onset shortness of breath, hypotension (BP 87/58 mmHg), tachycardia (HR 150/min), and hypoxia (SpO2 85%). Given his history of atopic dermatitis and asthma, he is at high risk for severe allergic reactions.
- **Intramuscular epinephrine** is the first-line treatment for anaphylaxis as it acts rapidly to constrict blood vessels, relax airway smooth muscle, and reduce swelling, addressing both cardiovascular collapse and respiratory distress.
*Albuterol and prednisone*
- While **albuterol** (a bronchodilator) might help with bronchoconstriction, and **prednisone** (a corticosteroid) can reduce inflammation, these are not the immediate priority for severe anaphylaxis.
- They act too slowly to counteract the rapid, systemic effects of anaphylaxis, particularly the life-threatening hypotension and airway compromise.
*IV epinephrine*
- **Intravenous epinephrine** is reserved for severe, refractory cases of anaphylaxis, or for patients already receiving IV infusions in a critical care setting.
- Administering IV epinephrine requires careful titration due to the risk of arrhythmias and hypertension, and IM administration is preferred as the initial rapid response.
*IV fluids and 100% oxygen*
- **IV fluids** are crucial to address the distributive shock and hypotension in anaphylaxis, and **100% oxygen** is essential for hypoxia, but these are supportive measures.
- They do not address the underlying immunological mechanism driving the severe allergic reaction as directly and effectively as epinephrine.
*Albuterol and norepinephrine*
- **Albuterol** can help with bronchospasm, but it is insufficient for systemic anaphylaxis. **Norepinephrine** is a potent vasopressor used for severe shock.
- While norepinephrine can raise blood pressure, it does not have the broader beneficial effects of epinephrine on mast cell degranulation, airway dilation, and stabilization of vascular permeability, making it a secondary agent.
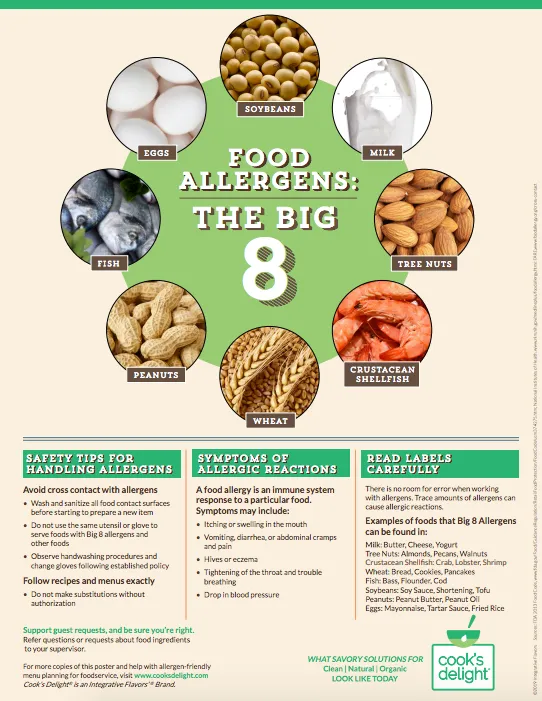
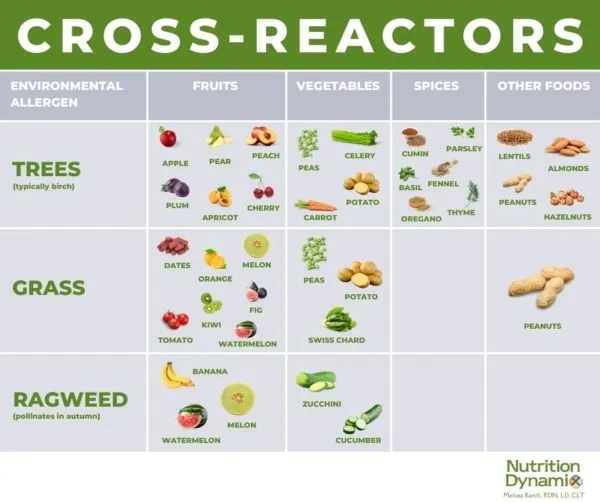
Food allergies and intolerances US Medical PG Question 3: A 12-month-old boy presents for a routine checkup. The patient immigrated from the Philippines with his parents a few months ago. No prior immunization records are available. The patient’s mother claims that he had a series of shots at 6 months of age which gave him a severe allergic reaction with swelling of the tongue and the face. She also remembers that he had the same reaction when she introduced solid foods to his diet, including carrots, eggs, and bananas. Which of the following vaccinations are not recommended for this patient?
- A. Measles, mumps, and rubella (MMR) vaccine
- B. Hepatitis B vaccine
- C. Varicella vaccine
- D. Intranasal influenza vaccine
- E. Intramuscular influenza vaccine (Correct Answer)
Food allergies and intolerances Explanation: ***Important Note on Current Guidelines***
Based on **current CDC/ACIP guidelines (2023-2024)**, egg allergy alone is **no longer a contraindication** to influenza vaccines. However, this question tests knowledge of vaccine safety in the context of **severe anaphylaxis to a prior vaccination**.
***Intramuscular influenza vaccine***
- **Historically**, this was considered the most concerning option for patients with severe egg allergy, as many influenza vaccines were produced using egg-based culture methods
- **Current practice**: Per CDC guidelines, persons with egg allergy of any severity can receive any age-appropriate influenza vaccine, as egg protein content is minimal or absent in modern formulations
- However, if this patient had a **documented anaphylactic reaction to the influenza vaccine itself** (not just eggs), then it would be contraindicated
- Given the timing (6 months) and symptoms described, this represents the **historically correct answer**, though modern practice has evolved
*Measles, mumps, and rubella (MMR) vaccine*
- MMR vaccine is grown in **chick embryo fibroblast cells**, NOT in eggs, and contains **no egg protein**
- **Safe for patients with egg allergy** - no contraindication based on egg allergy
- Should be administered on schedule for catch-up immunization
*Hepatitis B vaccine*
- Produced using **recombinant DNA technology in yeast cells**
- Contains **no egg protein** and no animal-derived proteins
- **No contraindication** for this patient - safe to administer
*Varicella vaccine*
- Grown in **human diploid cell cultures**, NOT in eggs
- Contains **no egg protein**
- **Safe for patients with egg allergy** - no contraindication
- Should be administered as part of catch-up immunization
*Intranasal influenza vaccine (LAIV)*
- Like the intramuscular formulation, **current guidelines allow administration** to patients with egg allergy of any severity
- Contains similar or less egg protein than inactivated vaccines in modern formulations
- **Not contraindicated** based solely on egg allergy per current CDC guidelines
Food allergies and intolerances US Medical PG Question 4: A 6-year-old boy is brought to the emergency room by ambulance, accompanied by his kindergarten teacher. Emergency department staff attempt to call his parents, but they cannot be reached. The boy’s medical history is unknown. According to his teacher, the boy was eating in the cafeteria with friends when he suddenly complained of itching and developed a widespread rash. Physical exam is notable for diffuse hives and tongue edema. His pulse is 100/min and blood pressure is 90/60 mmHg. The boy appears frightened and tells you that he does not want any treatment until his parents arrive. Which of the following is the next best step in the management of this patient?
- A. Immediately administer epinephrine and provide supportive care (Correct Answer)
- B. Continue calling the patient’s parents and do not intubate until verbal consent is obtained over the phone
- C. Obtain written consent to intubate from the patient’s teacher
- D. Wait for the patient's parents to arrive, calm the patient, and provide written consent before intubating
- E. Obtain written consent to intubate from the patient
Food allergies and intolerances Explanation: ***Immediately administer epinephrine and provide supportive care***
- This patient is experiencing **anaphylaxis**, characterized by diffuse hives, tongue edema, and hypotension (BP 90/60 mmHg in a 6-year-old). **Epinephrine** is the first-line treatment for anaphylaxis and should be administered immediately.
- In an emergency where a child's life is at risk and parents are unreachable, **implied consent** allows for life-saving treatment without explicit parental permission. Delaying treatment for consent would put the child's life at severe risk.
*Continue calling the patient’s parents and do not intubate until verbal consent is obtained over the phone*
- Delaying life-saving treatment like **epinephrine** or potential intubation for anaphylaxis while waiting for parental consent over the phone is unethical and could lead to irreversible harm or death.
- Anaphylaxis with tongue edema and hypotension is a **medical emergency** requiring immediate intervention, irrespective of consent if the patient is a minor and parents are unavailable.
*Obtain written consent to intubate from the patient’s teacher*
- A kindergarten teacher typically **does not have legal authority** to provide consent for invasive medical procedures like intubation for a student.
- The immediate priority is to treat the anaphylaxis with **epinephrine**, not to focus on intubation consent from an unauthorized party.
*Wait for the patient's parents to arrive, calm the patient, and provide written consent before intubating*
- Waiting for parents to arrive for written consent in a rapidly progressing anaphylactic reaction with **airway compromise** (tongue edema) and **hypotension** is extremely dangerous and potentially fatal.
- The patient's expressed wishes or fear do not supersede the immediate need for **life-saving intervention** when a minor's life is at risk and they lack the capacity to make such decisions.
*Obtain written consent to intubate from the patient*
- A 6-year-old child is considered a **minor** and does not have the legal capacity to give informed consent for complex medical procedures like intubation.
- While a child's assent is important, in a life-threatening emergency, the medical team is obligated to provide necessary treatment under the principle of **implied consent**.
Food allergies and intolerances US Medical PG Question 5: An 82-year-old woman presents with 2 months of foul-smelling, greasy diarrhea. She says that she also has felt very tired recently and has had some associated bloating and flatus. She denies any recent abdominal pain, nausea, melena, hematochezia, or vomiting. She also denies any history of recent travel and states that her home has city water. Which of the following tests would be most appropriate to initially work up the most likely diagnosis in this patient?
- A. Fecal fat test (Correct Answer)
- B. Tissue transglutaminase antibody test
- C. Stool O&P
- D. Stool guaiac test
- E. CT of the abdomen with oral contrast
Food allergies and intolerances Explanation: ***Fecal fat test***
- The patient's symptoms of **foul-smelling, greasy diarrhea**, along with **fatigue, bloating, and flatus**, strongly suggest **malabsorption**, specifically **steatorrhea** (excess fat in stool).
- A **fecal fat test** (e.g., Sudan stain or 72-hour quantitative stool fat collection) directly assesses fat malabsorption and would be the most appropriate initial diagnostic test.
*Tissue transglutaminase antibody test*
- This test is used to screen for **celiac disease**, which can cause malabsorption symptoms.
- While celiac disease is a possibility, a fecal fat test is a more general and appropriate initial step to confirm fat malabsorption before looking for specific causes.
*Stool O&P*
- Stands for **Stool Ova and Parasites**, used to detect parasitic infections like **Giardia** or **Cryptosporidium**, which can cause diarrhea.
- However, the absence of recent travel, city water, and the prominent greasy nature of the stool make this less likely as the primary initial investigation compared to confirming malabsorption.
*Stool guaiac test*
- This test detects **occult blood in stool**.
- The patient denies **melena or hematochezia**, and there are no signs pointing to gastrointestinal bleeding, making this test irrelevant for her presenting symptoms.
*CT of the abdomen with oral contrast*
- A CT scan with contrast might be used to investigate structural abnormalities or inflammation if other tests confirm malabsorption or point to a specific organ pathology (e.g., pancreatitis, Crohn's disease).
- It's an imaging study and generally not the most appropriate *initial* test for evaluating the described symptoms of malabsorption.
Food allergies and intolerances US Medical PG Question 6: An 11-month-old boy is brought to a pediatrician by his parents for evaluation of vomiting and watery diarrhea over the last day. The mother informs the pediatrician that the boy had consumed an apple bought from a fruit vendor on the previous day, but that otherwise there has been no recent change in his diet. There is no history of blood in the stool, flatulence, irritability, or poor appetite. There is no history of recurrent or chronic diarrhea or any other gastrointestinal symptoms. On physical examination, his temperature is 37.6°C (99.6°F), pulse is 120/min, respirations are 24/min, and blood pressure is 92/60 mm Hg. General examination reveals a playful infant with normal skin turgor and no sunken eyes. The pediatrician explains to the parents that he most likely has acute gastroenteritis and that no specific medication is indicated at present. He also instructs the parents about his diet during the illness and reviews the danger signs of dehydration. He suggests a follow-up evaluation after 48 hours or earlier if any complications arise. Which of the following dietary recommendations did the pediatrician make?
- A. Plenty of juices and carbonated sodas
- B. Age-appropriate diet (Correct Answer)
- C. Diluted formula milk
- D. Lactose-free diet
- E. BRAT diet
Food allergies and intolerances Explanation: ***Age-appropriate diet***
- For **mild acute gastroenteritis** without significant dehydration, the latest recommendations advise continuing **age-appropriate feeding** to support nutritional requirements and promote gut recovery.
- This approach helps to prevent malnutrition and does not prolong the course of diarrhea.
*Plenty of juices and carbonated sodas*
- **High sugar content** in juices and sodas can worsen diarrhea due to their **osmotic effect**, drawing more water into the intestine.
- These beverages also lack essential **electrolytes** needed for rehydration.
*Diluted formula milk*
- Diluting formula can lead to **insufficient caloric intake** and nutritional deficiencies, which is generally not recommended for mild gastroenteritis.
- Undiluted formula is usually well-tolerated, as most infants with acute gastroenteritis do not develop significant **lactose intolerance**.
*Lactose-free diet*
- Routine use of **lactose-free diets** is generally not recommended unless there is strong evidence of **secondary lactase deficiency**, which typically presents with increased flatulence, bloating, and worsening diarrhea.
- The majority of children with acute gastroenteritis can tolerate their usual milk intake.
*BRAT diet*
- The **B**ananas, **R**ice, **A**pplesauce, **T**oast (BRAT) diet is **nutritionally restrictive**, providing inadequate protein and fat, which can hinder recovery and growth in infants.
- Current guidelines no longer recommend the BRAT diet for acute gastroenteritis.
Food allergies and intolerances US Medical PG Question 7: A 7-year-old boy presents to an urgent care clinic from his friend’s birthday party after experiencing trouble breathing. His father explains that the patient had eaten peanut butter at the party, and soon after, he developed facial flushing and began scratching his face and neck. This has never happened before but his father says that they have avoided peanuts and peanut butter in the past because they were worried about their son having an allergic reaction. The patient has no significant medical history and takes no medications. His blood pressure is 94/62 mm Hg, heart rate is 125/min, and respiratory rate is 22/min. On physical examination, his lips are edematous and he has severe audible stridor. Of the following, which type of hypersensitivity reaction is this patient experiencing?
- A. Type II hypersensitivity reaction
- B. Type III hypersensitivity reaction
- C. Type I hypersensitivity reaction (Correct Answer)
- D. Type IV hypersensitivity reaction
- E. Combined type I and type III hypersensitivity reactions
Food allergies and intolerances Explanation: ***Type I hypersensitivity reaction***
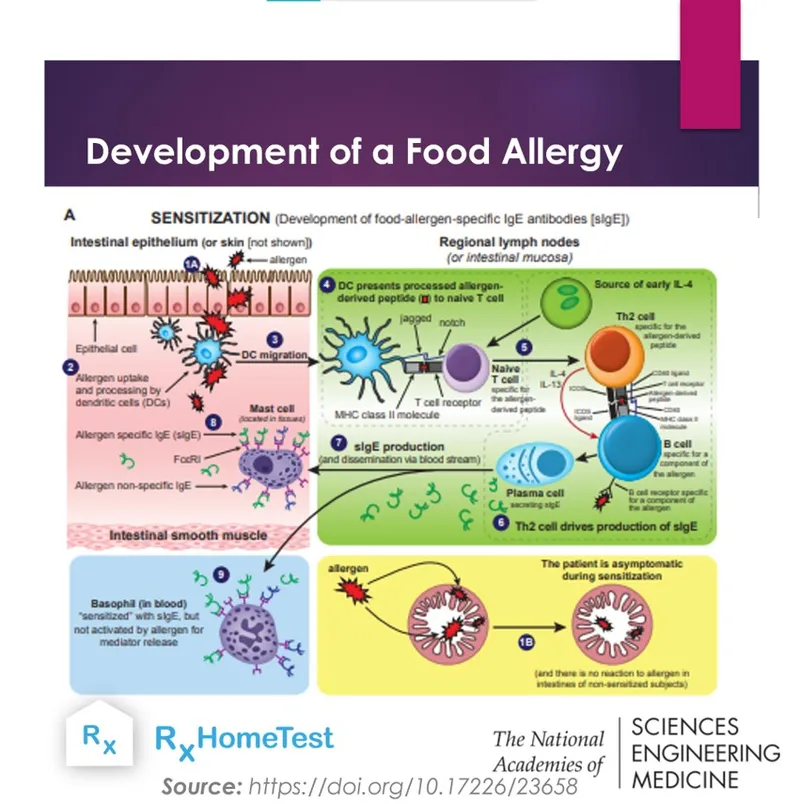
- This patient is experiencing **anaphylaxis** due to **peanut exposure**, a classic example of a **Type I hypersensitivity reaction**. This involves **IgE-mediated mast cell and basophil degranulation**, releasing histamines and other inflammatory mediators.
- The symptoms like **facial flushing, itching, angioedema (edematous lips), stridor (upper airway obstruction), tachycardia**, and potentially **hypotension** (blood pressure 94/62 mmHg in a child suggests relative hypotension) are all consistent with a severe systemic allergic reaction.
*Type II hypersensitivity reaction*
- Type II hypersensitivity involves **antibody-mediated cytotoxicity**, where **IgG or IgM antibodies** bind to antigens on cell surfaces, leading to cell destruction.
- This type of reaction typically manifests as **hemolytic anemia, thrombocytopenia**, or **Goodpasture syndrome**, which are distinct from the patient's acute allergic presentation.
*Type III hypersensitivity reaction*
- Type III hypersensitivity is characterized by the formation of **immune complexes** (antigen-antibody complexes) that deposit in tissues, leading to inflammation and tissue damage.
- Conditions like **serum sickness, lupus nephritis**, or **Arthus reaction** are examples of Type III reactions and do not fit the acute, IgE-mediated symptoms seen in this patient.
*Type IV hypersensitivity reaction*
- Type IV hypersensitivity is a **delayed-type hypersensitivity** reaction mediated by **T-cells**, not antibodies. It takes 24-72 hours to develop.
- Examples include **contact dermatitis (e.g., poison ivy)**, **tuberculin skin test reactions**, or **graft rejection**, which are much slower and have different mechanisms than the immediate anaphylactic response described.
*Combined type I and type III hypersensitivity reactions*
- While some complex immune conditions might involve multiple types of hypersensitivity over time, the patient's acute, rapid-onset symptoms after peanut ingestion are overwhelmingly characteristic of a **primary Type I hypersensitivity reaction**.
- There is no clinical evidence in this presentation to suggest the involvement of **immune complex deposition** (Type III) in addition to the immediate IgE-mediated response.
Food allergies and intolerances US Medical PG Question 8: A 5-year-old is brought into the emergency department for trouble breathing. He was at a family picnic playing when his symptoms began. The patient is currently struggling to breathe and has red, warm extremities. The patient has an unknown medical history and his only medications include herbs that his parents give him. His temperature is 99.5°F (37.5°C), pulse is 112/min, blood pressure is 70/40 mmHg, respirations are 18/min, and oxygen saturation is 82% on 100% O2. Which of the following is the best initial step in management?
- A. Intubation
- B. Albuterol
- C. Cricothyroidotomy
- D. Albuterol, ipratropium, and magnesium
- E. Epinephrine (Correct Answer)
Food allergies and intolerances Explanation: ***Epinephrine***
- This patient is exhibiting signs of **anaphylactic shock** (difficulty breathing, red/warm extremities, hypotension) likely triggered by an allergen at the picnic. **Epinephrine** is the first-line treatment for anaphylaxis due to its alpha and beta-adrenergic effects that counteract vasodilation, bronchoconstriction, and histamine release.
- The rapid onset of symptoms and cardiovascular collapse (hypotension) necessitate immediate administration of epinephrine to stabilize the patient.
*Intubation*
- While the patient is in respiratory distress, intubation is a more invasive procedure and not the *initial* best step for anaphylactic shock. **Epinephrine** should be administered first to address the underlying physiological derangements.
- Airway management, including intubation, may be necessary if epinephrine fails to improve respiratory status, but it is secondary to addressing the systemic allergic reaction.
*Albuterol*
- **Albuterol** is a bronchodilator that helps with bronchospasm, but it does not address the widespread vasodilation, hypotension, or other systemic effects of anaphylaxis.
- While it might provide some symptomatic relief for breathing, it is insufficient as a standalone treatment for anaphylactic shock and would not prevent cardiovascular collapse.
*Cricothyroidotomy*
- **Cricothyroidotomy** is an emergency airway procedure used when conventional intubation is impossible due to upper airway obstruction.
- In this scenario, the primary issue is systemic anaphylaxis causing bronchospasm and shock, not an isolated upper airway obstruction, making epinephrine the more appropriate initial intervention.
*Albuterol, ipratropium, and magnesium*
- This combination is typically used for severe asthma exacerbations, focusing on bronchodilation and smooth muscle relaxation.
- Like albuterol alone, this combination does not address the underlying systemic vasodilation and hypotension characteristic of anaphylactic shock, which requires **epinephrine**.
Food allergies and intolerances US Medical PG Question 9: You are working in the emergency room of a children's hospital when a 4-year-old girl is brought in by ambulance due to "difficulty breathing." The patient had been eating lunch on a school field trip when she suddenly complained of abdominal pain. Shortly thereafter, she was noted to have swelling of the lips, a rapidly developing red rash and difficulty breathing. In the ambulance her blood pressure was persistently 80/50 mmHg despite intramuscular epinephrine. In the course of stabilization and work up of the patient, you note an elevated tryptase level. What is the mechanism behind this elevated tryptase level?
- A. IgM mediated complement activation
- B. Cross-linking of IgE on mast cells (Correct Answer)
- C. IgG production by plasma cells
- D. Antibody-antigen immune complexes
- E. Cross-linking of IgG on mast cells
Food allergies and intolerances Explanation: **Cross-linking of IgE on mast cells**
- The rapid onset of symptoms like **lip swelling**, **rash**, and **difficulty breathing** after eating, along with **hypotension** despite epinephrine, points to **anaphylaxis**, which is primarily mediated by **IgE**.
- **Tryptase** is a serine protease selectively stored in the secretory granules of **mast cells** and is released upon mast cell activation, making it a reliable marker for **anaphylaxis**.
*IgM mediated complement activation*
- **IgM-mediated complement activation** is primarily involved in host defense against infections and in autoimmune conditions, but not typically in acute allergic reactions like anaphylaxis.
- While complement activation can occur in severe allergic reactions, the direct trigger and primary mechanism for tryptase release in anaphylaxis is **IgE cross-linking**.
*IgG production by plasma cells*
- **IgG production by plasma cells** is part of the adaptive immune response, responsible for long-term immunity and neutralizing toxins and pathogens.
- It is not the immediate mechanism for **mast cell degranulation** and **tryptase release** in an acute allergic reaction such as anaphylaxis.
*Antibody-antigen immune complexes*
- **Antibody-antigen immune complexes** are typically associated with Type III hypersensitivity reactions, which involve deposition of complexes in tissues, leading to inflammation (e.g., lupus, serum sickness).
- These reactions generally have a delayed onset and a different clinical presentation, not the acute, systemic symptoms of **anaphylaxis** seen here.
*Cross-linking of IgG on mast cells*
- While **IgG** can play a role in some immune responses, the primary immunoglobulin involved in immediate hypersensitivity reactions like anaphylaxis, leading to mast cell degranulation, is **IgE**, not IgG.
- Mast cells have **Fc receptors** for IgE, not IgG, that, when cross-linked by allergen, trigger the release of mediators including **tryptase**.
Food allergies and intolerances US Medical PG Question 10: A 4-week-old infant is brought to the physician by his mother because of blood-tinged stools for 3 days. He has also been passing whitish mucoid strings with the stools during this period. He was delivered at 38 weeks' gestation by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. He was monitored in the intensive care unit for a day prior to being discharged. His 6-year-old brother was treated for viral gastroenteritis one week ago. The patient is exclusively breastfed. He is at the 50th percentile for height and 60th percentile for weight. He appears healthy and active. His vital signs are within normal limits. Examination shows a soft and nontender abdomen. The liver is palpated just below the right costal margin. The remainder of the examination shows no abnormalities. Test of the stool for occult blood is positive. A complete blood count and serum concentrations of electrolytes and creatinine are within the reference range. Which of the following is the most appropriate next step in management?
- A. Perform stool antigen immunoassay
- B. Perform an air enema on the infant
- C. Assess for IgA (anti‑)tissue transglutaminase antibodies (tTG)
- D. Stop breastfeeding and switch to soy-based formula
- E. Continue breastfeeding and advise mother to avoid dairy and soy products (Correct Answer)
Food allergies and intolerances Explanation: ***Continue breastfeeding and advise mother to avoid dairy and soy products***
- The infant's symptoms of **blood-tinged stools** and **mucoid strings**, along with a positive occult blood test, in an otherwise healthy, exclusively breastfed infant point towards **food protein-induced proctocolitis (FPIAP)**.
- The most common triggers for FPIAP are **cow's milk protein** and **soy protein** from the maternal diet transmitted through breast milk. The initial management involves the mother eliminating these proteins from her diet.
*Perform stool antigen immunoassay*
- This test is used to detect specific viral, bacterial, or parasitic antigens in stool, often for conditions like **rotavirus, giardiasis, or C. difficile**.
- The infant's clinical presentation with **no fever, vomiting, or diarrhea**, and an otherwise healthy appearance, makes an infectious cause less likely compared to FPIAP.
*Perform an air enema on the infant*
- An air enema is primarily a diagnostic and therapeutic intervention for **intussusception**, a condition where one segment of the intestine telescopes into another.
- Intussusception typically presents with sudden onset of severe, colicky abdominal pain, **"currant jelly" stools**, and often a palpable abdominal mass, none of which are described in this infant.
*Assess for IgA (anti‑)tissue transglutaminase antibodies (tTG)*
- This test is used to screen for **celiac disease**, an autoimmune disorder triggered by gluten consumption.
- Celiac disease typically presents after the introduction of **gluten-containing foods** into the diet, usually around 6-12 months of age, and is characterized by malabsorption symptoms like diarrhea, weight loss, and failure to thrive, which are absent here.
*Stop breastfeeding and switch to soy-based formula*
- Stopping breastfeeding is generally **not recommended** as breast milk provides numerous benefits.
- Switching to a **soy-based formula** may not resolve the issue, as many infants with cow's milk protein allergy also have a **soy protein allergy**. The preferred approach is to eliminate allergens from the maternal diet while continuing breastfeeding.
More Food allergies and intolerances US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.