Breastfeeding support and counseling US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Breastfeeding support and counseling. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Breastfeeding support and counseling US Medical PG Question 1: A 55-year-old man comes to the physician with a 3-month history of headache, periodic loss of vision, and easy bruising. Physical examination shows splenomegaly. His hemoglobin concentration is 13.8 g/dL, leukocyte count is 8000/mm3, and platelet count is 995,000/mm3. Bone marrow biopsy shows markedly increased megakaryocytes with hyperlobulated nuclei. Genetic analysis shows upregulation of the JAK-STAT genes. The pathway encoded by these genes is also physiologically responsible for signal transmission of which of the following hormones?
- A. Oxytocin
- B. Adrenocorticotropic hormone
- C. Prolactin (Correct Answer)
- D. Cortisol
- E. Insulin
Breastfeeding support and counseling Explanation: ***Prolactin***
- Prolactin utilizes the **JAK-STAT signaling pathway** to exert its effects on target cells, particularly in the mammary glands.
- The **JAK-STAT pathway** is crucial for cell growth, differentiation, and immune response, and its dysregulation is linked to myeloproliferative disorders like those involving megakaryocyte proliferation.
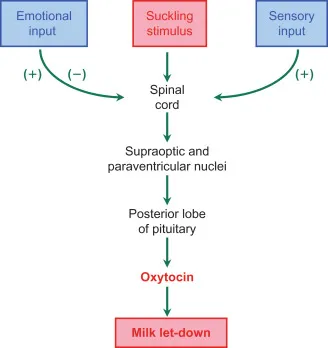
*Oxytocin*
- Oxytocin primarily acts through **G-protein coupled receptors** that activate the phospholipase C/inositol triphosphate pathway, not the JAK-STAT pathway.
- Its main roles involve uterine contraction and milk ejection, which are distinct from the cellular proliferation regulated by JAK-STAT.
*Adrenocorticotropic hormone*
- ACTH binds to **G-protein coupled receptors** in the adrenal cortex, stimulating adenylyl cyclase and increasing cAMP levels.
- This mechanism of action is distinct from the tyrosine kinase activity characteristic of the JAK-STAT pathway.
*Cortisol*
- Cortisol, a steroid hormone, primarily acts via **intracellular glucocorticoid receptors** that translocate to the nucleus to regulate gene transcription.
- Its signaling mechanism involves direct gene regulation rather than a membrane-bound receptor-kinase cascade like JAK-STAT.
*Insulin*
- Insulin signals through a **receptor tyrosine kinase**, which, upon binding, autophosphorylates and initiates a cascade involving IRS proteins and the PI3K/Akt and MAPK pathways.
- While it involves tyrosine phosphorylation, it is distinct from the JAK-STAT pathway, which is primarily activated by cytokine and growth hormone type I receptors.
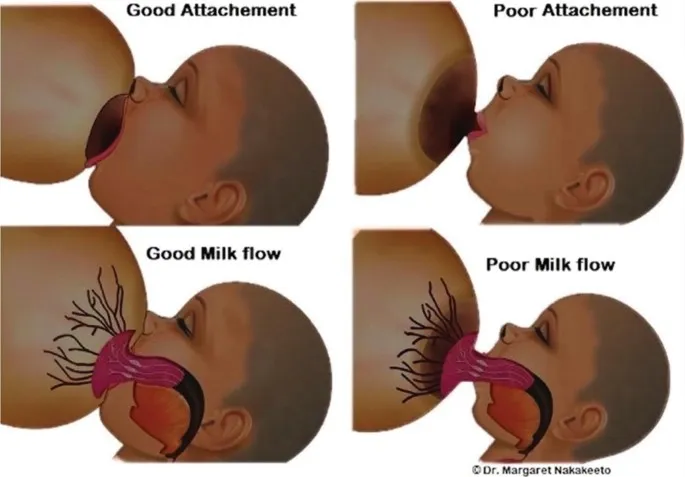
Breastfeeding support and counseling US Medical PG Question 2: A 28-year-old gravida 1 para 1 woman is being seen in the hospital for breast tenderness. She reports that both breasts are swollen and tender. She is also having difficulty getting her newborn to latch. The patient gave birth 4 days ago by uncomplicated vaginal delivery. During her pregnancy, the patient developed gestational diabetes but was otherwise healthy. She took folate and insulin. She attended all her pre-natal appointments. Upon examination, the patient has a low grade fever, but all other vital signs are stable. Bilateral breasts appear engorged and are tender to palpation. There is no erythema, warmth, or induration. A lactation nurse is brought in to assist the patient and her newborn with more effective breastfeeding positions. The patient says a neighbor told her that breastmilk actually lacks in nutrients, and she asks what the best option is for the health of her newborn. Which of the following components is breastmilk a poor source of?
- A. Whey protein
- B. Vitamin D (Correct Answer)
- C. Lysozymes
- D. Phosphorus
- E. Immunoglobulin A
Breastfeeding support and counseling Explanation: ***Vitamin D***
- **Breast milk** is naturally a **poor source of vitamin D**, making supplementation necessary for breastfed infants to prevent **rickets** and ensure adequate bone development.
- While small amounts of vitamin D are present, they are often insufficient to meet the infant's requirements, especially if maternal vitamin D levels are also low.
*Whey protein*
- **Whey protein** is a major component of breast milk, contributing to its digestibility and providing essential **amino acids** for infant growth.
- It is specifically rich in **alpha-lactalbumin**, which has both nutritional and antimicrobial properties.
*Lysozymes*
- **Lysozymes** are abundant in breast milk and play a crucial role in the infant's innate **immune defense** by breaking down bacterial cell walls.
- These enzymes help protect against gastrointestinal infections and contribute to the establishment of healthy gut flora.
*Phosphorus*
- **Phosphorus** is an essential mineral found in sufficient quantities in **breast milk**, crucial for **bone mineralization**, energy metabolism, and cell function.
- Its concentration is carefully regulated to meet the needs of the growing infant without overloading immature kidneys.
*Immunoglobulin A*
- **Secretory IgA (sIgA)** is the predominant **immunoglobulin** in breast milk, providing passive immunity by coating the infant's intestinal tract and preventing pathogen attachment.
- It is crucial for protecting the infant from various infections, especially those affecting the gastrointestinal and respiratory systems.
Breastfeeding support and counseling US Medical PG Question 3: A 29-year-old G1P1 woman presents to her primary care physician with unilateral breast pain. She is currently breastfeeding her healthy 3-month-old baby boy. She has been breastfeeding since her child's birth without any problems. However, 3 days prior to presentation, she developed left breast pain, purulent nipple discharge, and malaise. Her past medical history is notable for obesity and generalized anxiety disorder. She takes sertraline. She does not smoke or drink alcohol. Her temperature is 100.8°F (38.2°C), blood pressure is 128/78 mmHg, pulse is 91/min, and respirations are 17/min. On exam, she appears lethargic but is able to answer questions appropriately. Her right breast appears normal. Her left breast is tender to palpation, warm to the touch, and swollen relative to the right breast. There is a visible fissure in the left nipple that expresses minimal purulent discharge. Which of the following pathogens is the most likely cause of this patient's condition?
- A. Staphylococcus epidermidis
- B. Candida albicans
- C. Staphylococcus aureus (Correct Answer)
- D. Bacteroides fragilis
- E. Streptococcus pyogenes
Breastfeeding support and counseling Explanation: ***Staphylococcus aureus***
- The patient's unilateral breast pain, purulent nipple discharge, fever, and localized warmth along with a fissure strongly suggest **mastitis**, commonly caused by bacterial infection in breastfeeding women.
- **_Staphylococcus aureus_** is the most common pathogen responsible for infectious mastitis due to its prevalence on the skin and ability to enter through nipple fissures.
*Staphylococcus epidermidis*
- While **_Staphylococcus epidermidis_** is a common skin commensal, it is less frequently implicated alone in significant, symptomatic mastitis with purulent discharge and fever.
- It is more often associated with biofilm-related infections on medical devices or opportunistic infections in immunocompromised individuals.
*Candida albicans*
- **_Candida albicans_** can cause fungal mastitis, often presenting with burning pain in both breasts and nipples, radiating to the back or armpit, typically without purulent discharge or significant fever unless there's a secondary bacterial infection.
- The presence of **purulent discharge** and fever points away from a primary candidal infection in this case.
*Bacteroides fragilis*
- **_Bacteroides fragilis_** is an anaerobic bacterium, usually associated with infections of the abdominal cavity or female genital tract after surgery or trauma, and rarely causes primary breast infections.
- The clinical picture of acute infectious mastitis in a breastfeeding woman is not consistent with **_Bacteroides fragilis_** as a primary pathogen.
*Streptococcus pyogenes*
- **_Streptococcus pyogenes_** can cause skin infections like cellulitis, but it is a relatively rare cause of acute infectious mastitis compared to **_Staphylococcus aureus_**.
- While it can cause severe infections, **_S. aureus_** remains the predominant pathogen in this clinical scenario.
Breastfeeding support and counseling US Medical PG Question 4: A 26-year-old woman presents to her physician with a complaint of milk reduction. 2 months ago, she delivered a healthy girl from an uncomplicated pregnancy. The baby was exclusively breastfed until 1.5 months when the patient had to return to the workforce. She cannot breastfeed her daughter at work so she had to leave her with her grandmother and incorporated baby formula into her diet. She reports breast engorgement shortly after she switched to the described regimen which subsided soon. A week after she switched to such a regimen, she started to notice that she has less milk to feed her baby when she is at home. The patient does not report any other symptoms including weight change or mood disturbances. She has breast implants installed submuscularly using the inframammary approach. At the age of 12 years, she had a blunt chest trauma with breast involvement. After the pregnancy, she had a short course of cetirizine due to hay fever. At presentation, the patient’s vital signs are within normal limits. The patient’s breasts are slightly engorged with no skin color changes. There is no discharge on breast compression. Which of the following statements describes the cause of the patient’s condition?
- A. Obliteration of the ducts due to trauma
- B. Failure of lactogenic ducts to develop
- C. Suppression of lactation by the medications
- D. Insufficient amount of glandular breast tissue
- E. Insufficient breast emptying (Correct Answer)
Breastfeeding support and counseling Explanation: ***Insufficient breast emptying***
- The patient's reduced milk supply is most likely due to **decreased frequency of breast emptying** once she returned to work and started using formula.
- **Regular and complete removal of milk** is essential to maintain supply, as milk production operates on a supply-and-demand basis.
*Obliteration of the ducts due to trauma*
- While significant **blunt chest trauma** could potentially cause ductal damage, it would typically present with immediate and severe lactation issues.
- The patient successfully breastfed for 1.5 months, indicating functional ducts post-trauma and pre-pregnancy.
*Failure of lactogenic ducts to develop*
- This is unlikely given that the patient was able to **successfully breastfeed exclusively for 1.5 months**, indicating the presence and function of lactogenic ducts.
- **Insufficient glandular tissue** (hypoplasia) is a different issue, and while it leads to low milk supply, it's not a "failure of ducts to develop."
*Suppression of lactation by the medications*
- **Cetirizine, an antihistamine**, is generally considered safe during lactation and is not known to significantly suppress milk supply.
- There is no mention of other medications that could strongly inhibit lactation (e.g., certain decongestants or hormonal contraceptives).
*Insufficient amount of glandular breast tissue*
- The patient's ability to **exclusively breastfeed for 1.5 months** suggests that she had sufficient glandular tissue to establish lactation.
- While breast implants can sometimes be associated with lactation difficulties, submuscular placement and inframammary incisions typically **preserve glandular tissue and ducts** better than other approaches.
Breastfeeding support and counseling US Medical PG Question 5: A 24-year-old newly immigrated mother arrives to the clinic to discuss breastfeeding options for her newborn child. Her medical history is unclear as she has recently arrived from Sub-Saharan Africa. You tell her that unfortunately she will not be able to breastfeed until further testing is performed. Which of the following infections is an absolute contraindication to breastfeeding?
- A. Human Immunodeficiency Virus (HIV) (Correct Answer)
- B. Latent tuberculosis
- C. Hepatitis B
- D. Hepatitis C
- E. All of the options
Breastfeeding support and counseling Explanation: ***Human Immunodeficiency Virus (HIV)***
- In developed countries where safe alternatives are available, **HIV-positive mothers** are advised against breastfeeding due to the risk of **vertical transmission** through breast milk.
- This is considered an **absolute contraindication** in settings where formula feeding is accessible and safe.
*Latent tuberculosis*
- **Latent tuberculosis** is not a contraindication to breastfeeding; mothers can breastfeed while receiving treatment.
- Active, untreated tuberculosis, however, generally requires temporary separation of mother and child until the mother is no longer infectious, but pumping and feeding expressed milk is often still an option.
*Hepatitis B*
- **Hepatitis B** infection in the mother is not a contraindication to breastfeeding, especially if the infant receives **hepatitis B vaccine** and **Hepatitis B Immune Globulin (HBIG)** at birth.
- Breastfeeding is considered safe and does not increase the risk of transmission to the infant.
*Hepatitis C*
- **Hepatitis C** is generally **not a contraindication** to breastfeeding, as studies have shown a very low risk of transmission through breast milk.
- Breastfeeding is supported unless the mother has **cracked or bleeding nipples**, which could potentially allow viral transmission.
*All of the options*
- This option is incorrect because **only HIV** is considered an absolute contraindication to breastfeeding in settings where safe alternatives are available.
- Latent TB, Hepatitis B, and Hepatitis C alone do not preclude breastfeeding.
Breastfeeding support and counseling US Medical PG Question 6: Twenty minutes after delivery of a newborn infant, a 22-year-old woman starts breastfeeding. Initially, the expressed milk is thick and yellowish. Three days later, the mother's breasts swell and the expressed milk becomes thinner and whiter. A decrease in maternal serum concentration of which of the following is most likely responsible for the observed changes in milk production?
- A. Human chorionic gonadotropin
- B. Oxytocin
- C. Thyroxine
- D. Progesterone (Correct Answer)
- E. Estrogen
Breastfeeding support and counseling Explanation: ***Progesterone***
- The drop in **progesterone** levels after birth removes its inhibitory effect on **milk production**, allowing for the transition from **colostrum** to **mature milk**.
- High levels of **progesterone** during pregnancy inhibit the full effects of **prolactin** on the mammary glands, preventing lactation (lactogenesis II).
- After placental delivery, the dramatic fall in progesterone allows prolactin to stimulate copious milk secretion, typically occurring around day 3-5 postpartum.
*Human chorionic gonadotropin*
- **hCG** maintains the corpus luteum during early pregnancy but is not directly involved in the regulation of postpartum milk production.
- Its levels decrease significantly after delivery, but this decrease is not the primary driver of milk changes.
*Oxytocin*
- **Oxytocin** is responsible for **milk ejection (let-down)**, not milk production or changes in milk composition.
- Its levels tend to increase during breastfeeding due to suckling, rather than decrease.
*Thyroxine*
- **Thyroxine** (thyroid hormones) is essential for overall metabolism and can affect milk supply, but a decrease in its levels is not primarily responsible for the switch from colostrum to mature milk.
- Decreased thyroxine would more likely lead to *reduced* milk production or broader metabolic disturbances.
*Estrogen*
- **Estrogen** levels decrease significantly after delivery, similar to progesterone, but progesterone's inhibitory effect on lactation is more direct and critical for the transition in milk type.
- While high estrogen during pregnancy also inhibits lactation, the removal of progesterone's block is the key trigger for copious milk secretion.
Breastfeeding support and counseling US Medical PG Question 7: A 6-month-old girl is brought to the physician for a well-child examination. She was born at 37 weeks' gestation. Pregnancy and the neonatal period were uncomplicated. The infant was exclusively breastfed and received vitamin D supplementation. She can sit unsupported and can transfer objects from one hand to the other. She babbles and is uncomfortable around strangers. She is at 40th percentile for length and at 35th percentile for weight. Vital signs are within normal limits. Physical examination shows no abnormalities. In addition to continuing breastfeeding, which of the following is the most appropriate recommendation at this time?
- A. Continue vitamin D
- B. Introduce solid foods
- C. Introduce solid foods and add vitamin C
- D. Introduce solid foods and cow milk
- E. Introduce solid foods and continue vitamin D (Correct Answer)
Breastfeeding support and counseling Explanation: ***Introduce solid foods and continue vitamin D***
- At **6 months of age**, infants typically show developmental readiness for **solid foods**, such as the ability to sit unsupported and transfer objects, while **breastfeeding** continues to be important.
- **Vitamin D supplementation** should continue as it is crucial for bone health and is not adequately supplied by breast milk or early solid foods alone.
*Continue vitamin D*
- While vitamin D supplementation is important, this option **misses the crucial developmental milestone** of introducing solid foods at 6 months.
- At this age, infants' **iron stores** begin to dwindle, and solid foods are needed to provide essential nutrients not sufficiently met by breast milk alone.
*Introduce solid foods*
- This option correctly identifies the need to introduce solid foods but **fails to mention the continued importance of vitamin D supplementation**.
- Breastfed infants require continued **vitamin D supplementation** to prevent **rickets**, as breast milk does not contain sufficient amounts.
*Introduce solid foods and add vitamin C*
- While **vitamin C** is important, the primary focus at 6 months should be on **iron-rich solid foods** and continued **vitamin D supplementation**.
- Breast milk contains adequate vitamin C, and introducing diverse solid foods typically provides enough, making dedicated vitamin C supplementation usually unnecessary unless a deficiency is identified.
*Introduce solid food and cow milk*
- **Cow's milk** should **not be introduced** as a primary drink before **12 months of age** because it can cause **gastrointestinal bleeding**, **iron-deficiency anemia**, and is difficult for infants to digest.
- Introducing cow's milk too early can also interfere with the absorption of essential nutrients from breast milk or formula.
Breastfeeding support and counseling US Medical PG Question 8: A 19-year-old African female refugee has been granted asylum in Stockholm, Sweden and has been living there for the past month. She arrived in Sweden with her 2-month-old infant, whom she exclusively breast feeds. Which of the following deficiencies is the infant most likely to develop?
- A. Vitamin E
- B. Vitamin A
- C. Vitamin C
- D. Vitamin B1
- E. Vitamin D (Correct Answer)
Breastfeeding support and counseling Explanation: ***Vitamin D***
- The combination of exclusive breastfeeding, a 2-month-old infant, being of African heritage (darker skin), and living in a high-latitude region like Stockholm, Sweden, significantly increases the risk of **vitamin D deficiency**. Darker skin pigmentation reduces the efficiency of **cutaneous vitamin D synthesis** from sunlight, and insufficient sun exposure in northern latitudes further exacerbates this.
- Breast milk is a relatively poor source of **vitamin D**, and infants specifically require supplementation, especially when they have risk factors for deficiency such as being of African descent and living in an area with limited sunshine.
*Vitamin E*
- **Vitamin E deficiency** in infants is rare and typically seen in premature infants or those with severe malabsorption, neither of which is indicated in this scenario.
- While breast milk contains vitamin E, deficiency is not directly linked to geographic location, skin color, or a 2-month-old infant.
*Vitamin A*
- **Vitamin A deficiency** can be a concern in developing countries, but it is less likely to be the primary concern under these specific circumstances in a 2-month-old exclusively breastfed infant unless the mother herself is severely deficient.
- Breast milk usually provides adequate **vitamin A** if the mother's nutritional status is sufficient.
*Vitamin C*
- **Vitamin C deficiency** (scurvy) is rare in breastfed infants because breast milk typically contains adequate vitamin C if the mother has adequate dietary intake.
- Scurvy would be more likely in infants fed with improperly prepared formula or after 6 months if complementary foods lack vitamin C.
*Vitamin B1*
- **Vitamin B1 (thiamine) deficiency** is uncommon in exclusively breastfed infants in developed countries.
- It is often associated with maternal malnutrition in endemic areas or specific genetic disorders, which are not suggested here.
Breastfeeding support and counseling US Medical PG Question 9: A 2-month-old girl is brought to the physician for a well-child examination. She was born at 32 weeks' gestation and weighed 1616 g (3 lb 9 oz); she currently weighs 2466 g (5 lb 7 oz). She is exclusively breastfed and receives vitamin D supplementation. Physical examination shows no abnormalities apart from low height and weight. This patient is at increased risk for which of the following complications?
- A. Iron deficiency anemia (Correct Answer)
- B. Hemorrhage
- C. Scurvy
- D. Subacute combined degeneration
- E. Intussusception
Breastfeeding support and counseling Explanation: ***Iron deficiency anemia***
- Preterm infants have **lower iron stores** at birth due to reduced placental transfer in the third trimester.
- Their rapid growth rate and exclusive breastfeeding (breast milk has low iron content) further increase their risk of **iron deficiency anemia**.
*Hemorrhage*
- While preterm infants are at higher risk for certain hemorrhages (e.g., intraventricular hemorrhage), this typically occurs in the **immediate neonatal period** and risk significantly decreases by 2 months of age.
- Hemorrhage is not a common long-term complication unique to a 2-month-old preterm infant without additional risk factors.
*Scurvy*
- Scurvy is caused by **vitamin C deficiency**, which is typically not a concern in breastfed infants as breast milk provides adequate vitamin C.
- The primary deficiency risk addressed by supplementation in breastfed infants is vitamin D, not vitamin C.
*Subacute combined degeneration*
- This condition is caused by **vitamin B12 deficiency**, leading to demyelination of the spinal cord.
- While possible in infants of vegan mothers, it is unlikely in a breastfed infant without specific dietary restrictions in the mother.
*Intussusception*
- Intussusception is a condition where one segment of the intestine telescopes into another, usually occurring between **3 months and 3 years of age**.
- It is not specifically linked to prematurity or low birth weight as an increased long-term risk.
Breastfeeding support and counseling US Medical PG Question 10: A 13-month-old boy with sickle cell anemia is brought to the emergency department because of continuous crying and severe left-hand swelling. His condition started 2 hours earlier without any preceding trauma. The child was given diclofenac syrup at home with no relief. The temperature is 37°C (98.6°F), blood pressure is 100/60 mm Hg, and pulse is 100/min. The physical examination reveals swelling and tenderness to palpation of the left hand. The hemoglobin level is 10.4 g/dL. Which of the following is the best initial step in management of this patient condition?
- A. Magnetic resonance imaging (MRI) of the affected joint
- B. Incentive spirometry
- C. Joint aspiration
- D. Intravenous meperidine
- E. Intravenous morphine (Correct Answer)
Breastfeeding support and counseling Explanation: ***Intravenous morphine***
- The patient presents with classic signs of **dactylitis**, a painful vaso-occlusive crisis in sickle cell anemia, characterized by acute onset of **painful swelling of hands and feet**.
- **Opioids** like intravenous morphine are the cornerstone for managing severe pain in sickle cell pain crises, and a **multimodal approach** to pain control is recommended.
*Magnetic resonance imaging (MRI) of the affected joint*
- While MRI can visualize soft tissue and bone, it is **not the initial step** in managing a sickle cell pain crisis due to its cost, time, and potential need for sedation in a child.
- The diagnosis of **dactylitis is primarily clinical**, based on the patient's history and physical examination.
*Incentive spirometry*
- **Incentive spirometry** is primarily used to prevent or treat **pulmonary complications** like atelectasis, often in postoperative patients or those with acute chest syndrome.
- It is not indicated for the management of **acute pain due to dactylitis** and would not address the patient's immediate problem.
*Joint aspiration*
- **Joint aspiration** is performed to diagnose infectious arthritis or to relieve pressure from effusions, which presents with signs of inflammation.
- The patient's symptoms are consistent with **vaso-occlusive crisis** in sickle cell disease, not an infection, making aspiration unnecessary and potentially harmful.
*Intravenous meperidine*
- **Meperidine (Demerol)** is generally **avoided in sickle cell patients** due to the accumulation of its metabolite, **normeperidine**, which can cause **neurotoxicity**, including seizures.
- Other opioids like morphine or hydromorphone are preferred for severe pain in this population.
More Breastfeeding support and counseling US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.