Nutritional requirements and disorders

On this page
🍎 Nutritional Foundations: The Pediatric Fuel Matrix
Children's bodies are metabolic marvels, demanding precise fuel ratios that shift dramatically from infancy through adolescence-and when nutrition falters, the consequences ripple across growth, immunity, cognition, and organ function. You'll master how to calculate age-specific requirements, recognize the clinical signatures of deficiency and excess, assess nutritional status through anthropometrics and biochemical markers, and design targeted interventions that restore health across diverse pediatric populations. This lesson transforms you into a nutritional detective, equipped to decode feeding challenges and optimize every child's developmental potential.
Energy Requirements: The Caloric Blueprint
Pediatric energy needs follow predictable patterns based on metabolic demands, growth velocity, and activity levels. The basal metabolic rate accounts for 60-70% of total energy expenditure in infants, compared to 45-50% in adults.
- Infants (0-12 months)
- 0-6 months: 108 kcal/kg/day (exclusively breastfed)
- 6-12 months: 98 kcal/kg/day (with complementary foods)
- Growth accounts for 25-35% of total energy expenditure
- Toddlers (1-3 years)
- 102 kcal/kg/day or 1000-1300 kcal/day total
- Physical activity increases to 15-20% of energy expenditure
- Preschoolers (4-6 years)
- 90 kcal/kg/day or 1400-1800 kcal/day total
- Growth velocity decreases, activity increases
- School-age (7-10 years)
- 70-80 kcal/kg/day or 1800-2200 kcal/day
- Prepubertal steady growth phase
📌 Remember: GROW for energy distribution - Growth (25%), Resting metabolism (60%), Other activities (10%), Waste heat (5%)
Macronutrient Distribution: The Building Blocks
Optimal macronutrient ratios shift dramatically across developmental stages, reflecting changing growth patterns and metabolic priorities.
| Age Group | Protein (%) | Fat (%) | Carbohydrate (%) | Protein (g/kg/day) | Key Considerations |
|---|---|---|---|---|---|
| 0-6 months | 7-10 | 45-50 | 40-45 | 2.2 | Brain development priority |
| 6-12 months | 10-15 | 35-40 | 45-50 | 1.6 | Transition period |
| 1-3 years | 15-20 | 30-35 | 50-55 | 1.1 | Rapid growth continues |
| 4-8 years | 15-20 | 25-30 | 55-60 | 0.95 | Steady growth phase |
| 9-13 years | 15-20 | 25-30 | 55-60 | 0.95 | Pre-pubertal stability |
⭐ Clinical Pearl: Children under 2 years should never receive low-fat diets - fat restriction impairs brain development and growth velocity by 15-25%
Protein Quality: Complete proteins containing all essential amino acids optimize growth. Biological value of breast milk protein reaches 100, compared to 85 for cow's milk and 75 for soy protein.
💡 Master This: The protein efficiency ratio determines growth impact - animal proteins provide 1.2-1.5x the growth benefit of plant proteins due to amino acid completeness and digestibility
Connect these macronutrient foundations through micronutrient cofactors to understand complete nutritional optimization.
🍎 Nutritional Foundations: The Pediatric Fuel Matrix
⚡ Micronutrient Mastery: The Catalytic Command Center
Critical Micronutrients: The Essential Arsenal
Iron: The oxygen transport and cognitive development cornerstone. Requirements peak during periods of rapid growth and blood volume expansion.
- Infants: 0.27 mg/day (0-6 months), 11 mg/day (7-12 months)
- Toddlers: 7 mg/day (1-3 years)
- School-age: 10 mg/day (4-8 years), 8 mg/day (9-13 years)
- Absorption: 15-20% from heme sources, 2-5% from non-heme sources
- Storage: Liver stores provide 3-6 months reserve in healthy children
📌 Remember: TIRED for iron deficiency progression - Tissue depletion, Iron-deficient erythropoiesis, Reduced hemoglobin, Exhaustion, Decreased performance
Zinc: Essential for 300+ enzymatic reactions, immune function, and linear growth. Deficiency affects 17% of global pediatric population.
- Requirements: 2-3 mg/day (infants), 3-5 mg/day (toddlers), 5-8 mg/day (school-age)
- Absorption: 20-40% efficiency, decreased by phytates and fiber
- Clinical impact: Zinc deficiency reduces growth velocity by 25-30%
Fat-Soluble Vitamin Dynamics
Vitamin D: The bone health and immune modulator. Deficiency affects 1 billion people worldwide, with children at highest risk.
- Synthesis: 10-15 minutes of midday sun exposure produces 10,000-20,000 IU
- Requirements: 400 IU/day (infants), 600 IU/day (children >1 year)
- Optimal levels: 25(OH)D >30 ng/mL (75 nmol/L)
- Deficiency prevalence: 40-60% in temperate climates
⭐ Clinical Pearl: Vitamin D deficiency increases respiratory infection risk by 36% and reduces vaccine efficacy by 15-25% in pediatric populations
Vitamin A: Critical for vision, immunity, and epithelial integrity. Deficiency remains leading cause of preventable childhood blindness.
- Requirements: 300-400 μg RAE/day (toddlers), 400-500 μg RAE/day (school-age)
- Storage: Liver reserves last 4-6 months with adequate intake
- Deficiency impact: Increases mortality risk by 23% in children under 5
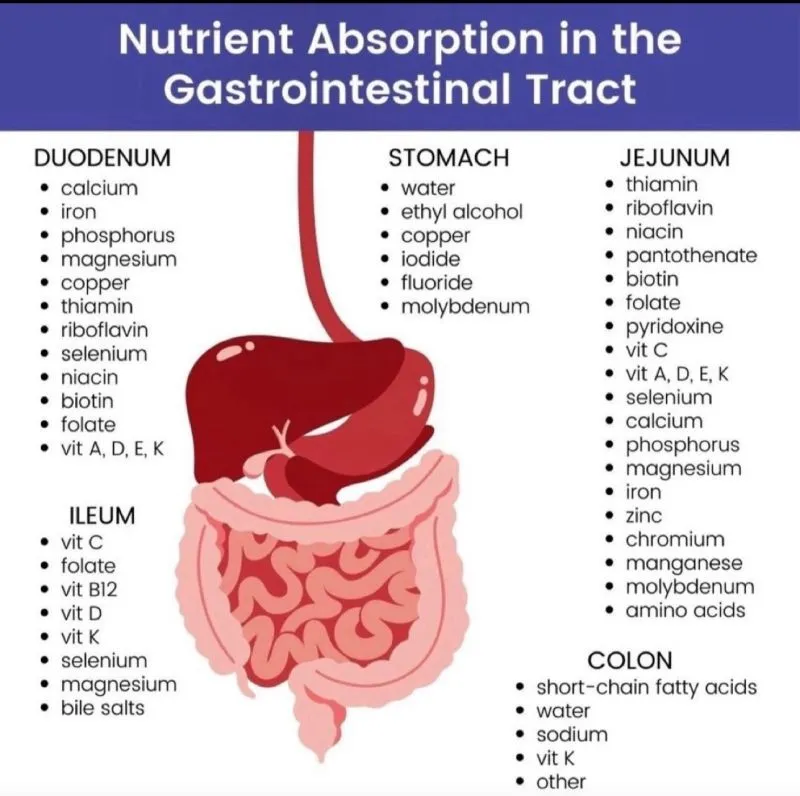
| Micronutrient | Absorption Site | Peak Requirement | Deficiency Prevalence | Clinical Threshold |
|---|---|---|---|---|
| Iron | Duodenum | 7-12 months | 25-30% globally | Ferritin <15 ng/mL |
| Zinc | Jejunum | 1-3 years | 17% globally | Serum zinc <65 μg/dL |
| Vitamin D | Small intestine | Infancy/Adolescence | 40-60% temperate | 25(OH)D <20 ng/mL |
| Vitamin A | Ileum | 6 months-2 years | 15% developing | Retinol <20 μg/dL |
| Folate | Jejunum | Pregnancy/Infancy | 10-15% globally | RBC folate <140 ng/mL |
Connect micronutrient optimization through age-specific feeding strategies to maximize developmental outcomes.
⚡ Micronutrient Mastery: The Catalytic Command Center
🍼 Feeding Evolution: The Developmental Nutrition Pathway

Feeding Readiness: The Neuromotor Foundation
Primitive Reflexes: Essential for early feeding success, with predictable emergence and integration patterns.
- Rooting reflex: Present at birth, integrates by 3-4 months
- Sucking reflex: Strongest at 34-36 weeks gestation
- Swallowing coordination: Mature by 32-34 weeks gestation
- Gag reflex: Present at 18-20 weeks gestation, moves posteriorly with development
Oral-Motor Development: Sequential skill acquisition enabling feeding progression.
- 0-3 months: Reflexive sucking, 120-150 sucks/minute
- 4-6 months: Voluntary sucking, tongue lateralization begins
- 6-9 months: Munching pattern, vertical jaw movement
- 9-12 months: Rotary chewing, diagonal jaw movement
- 12-24 months: Mature chewing pattern established
📌 Remember: SUCK for feeding readiness - Sitting with support, Up-and-down tongue movement lost, Curiosity about food, Keeping food in mouth
Age-Specific Feeding Strategies
Exclusive Breastfeeding (0-6 months): The gold standard providing complete nutrition and immunological protection.
- Frequency: 8-12 feeds/day in newborns, 6-8 feeds/day by 3 months
- Volume: 150-200 mL/kg/day average intake
- Composition: 87% water, 7% lactose, 4% fat, 1% protein
- Immunological factors: >100 bioactive compounds including secretory IgA
Complementary Feeding (6-24 months): Strategic introduction of solid foods while maintaining breast milk.
- Timing: 6 months - not before 4 months, not after 8 months
- Progression: Single foods for 3-5 days, then combinations
- Texture advancement: Purees → mashed → chopped → family foods
- Responsive feeding: Child-led hunger and satiety cues
First Foods Priority:
- Iron-rich foods: Meat, fortified cereals (11 mg/day requirement)
- Zinc sources: Meat, legumes (3 mg/day requirement)
- Allergenic foods: Early introduction reduces allergy risk by 70-80%
⭐ Clinical Pearl: Delaying complementary foods beyond 6 months increases iron deficiency risk by 300% and growth faltering by 40% in breastfed infants
Toddler Feeding (12-36 months): Transition to family foods with continued nutritional vigilance.
- Meal pattern: 3 meals + 2-3 snacks daily
- Portion sizes: 1 tablespoon per year of age as starting guide
- Milk intake: 16-24 oz/day whole milk, <24 oz to prevent iron deficiency
- Self-feeding: 90% independent by 18 months
| Age Range | Primary Nutrition | Feeding Skills | Key Nutrients | Common Challenges |
|---|---|---|---|---|
| 0-6 months | Breast milk/formula | Reflexive sucking | Complete nutrition | Latch difficulties |
| 6-9 months | Breast milk + solids | Munching, sitting | Iron, zinc | Texture acceptance |
| 9-12 months | Increasing solids | Pincer grasp | Iron, vitamin D | Self-feeding mess |
| 12-24 months | Family foods | Independent eating | Iron, calcium | Food neophobia |
| 2-5 years | Balanced diet | Utensil mastery | Fiber, vitamins | Picky eating |
Connect feeding development through nutritional assessment methods to identify and address feeding challenges systematically.
🍼 Feeding Evolution: The Developmental Nutrition Pathway
📏 Assessment Arsenal: The Nutritional Detective Framework
Anthropometric Precision: The Growth Detective
Growth Velocity: The most sensitive indicator of nutritional adequacy, revealing trends before static measurements show abnormalities.
- Weight velocity: 25-30 g/day (0-3 months), 15-20 g/day (3-6 months), 10 g/day (6-12 months)
- Length velocity: 3.5 cm/month (0-3 months), 2 cm/month (3-6 months), 1.3 cm/month (6-12 months)
- Head circumference: 2 cm/month (0-3 months), 1 cm/month (3-6 months), 0.5 cm/month (6-12 months)
Z-Score Interpretation: Standard deviations from population median enabling precise nutritional classification.
- Normal: Z-score between -2 and +2
- Mild malnutrition: Z-score -2 to -3
- Moderate malnutrition: Z-score -3 to -4
- Severe malnutrition: Z-score <-4
📌 Remember: WAZ-LAZ-WHZ for anthropometric assessment - Weight-for-Age Z-score (underweight), Length-for-Age Z-score (stunting), Weight-for-Height Z-score (wasting)
Biochemical Markers: The Laboratory Lens
Iron Status Assessment: Multi-parameter approach required due to inflammatory confounding.
- Serum ferritin: <15 ng/mL (iron deficiency), <12 ng/mL (infants)
- Transferrin saturation: <16% indicates iron deficiency
- Soluble transferrin receptor: Elevated in iron deficiency, unaffected by inflammation
- Hemoglobin: <11.0 g/dL (6 months-5 years), <11.5 g/dL (5-11 years)
Vitamin D Status: Critical for bone health and immune function optimization.
- 25(OH)D levels: >30 ng/mL (optimal), 20-30 ng/mL (sufficient), <20 ng/mL (deficient)
- Seasonal variation: 40-60% higher in late summer vs. late winter
- Parathyroid hormone: Elevated when 25(OH)D <30 ng/mL
Protein Status Indicators:
- Albumin: >3.5 g/dL (normal), reflects chronic protein status
- Prealbumin: >20 mg/dL (normal), reflects acute protein changes
- Retinol-binding protein: >3.0 mg/dL (normal), vitamin A transport
| Parameter | Normal Range | Mild Deficiency | Moderate Deficiency | Severe Deficiency | Clinical Significance |
|---|---|---|---|---|---|
| Hemoglobin (6mo-5y) | >11.0 g/dL | 10.0-10.9 g/dL | 8.0-9.9 g/dL | <8.0 g/dL | Oxygen transport |
| Serum ferritin | >15 ng/mL | 12-15 ng/mL | 8-12 ng/mL | <8 ng/mL | Iron stores |
| 25(OH)D | >30 ng/mL | 20-30 ng/mL | 10-20 ng/mL | <10 ng/mL | Bone health |
| Serum zinc | >65 μg/dL | 55-65 μg/dL | 45-55 μg/dL | <45 μg/dL | Growth, immunity |
| RBC folate | >140 ng/mL | 120-140 ng/mL | 100-120 ng/mL | <100 ng/mL | DNA synthesis |
Clinical Assessment: The Physical Evidence
Nutritional Physical Examination: Systematic evaluation revealing micronutrient deficiencies before laboratory confirmation.
- Hair changes: Sparse, easily pluckable (protein), flag sign (kwashiorkor)
- Skin manifestations: Follicular hyperkeratosis (vitamin A), petechiae (vitamin C)
- Oral findings: Angular cheilitis (B vitamins), dental caries (fluoride)
- Ocular signs: Night blindness (vitamin A), pale conjunctiva (iron)
- Neurological: Peripheral neuropathy (B vitamins), tetany (calcium/magnesium)
💡 Master This: Physical signs appear weeks before biochemical abnormalities - angular cheilitis precedes riboflavin deficiency by 2-4 weeks, follicular hyperkeratosis appears 4-6 weeks before vitamin A depletion
Connect assessment findings through evidence-based management protocols to optimize nutritional interventions and monitoring strategies.
📏 Assessment Arsenal: The Nutritional Detective Framework
⚖️ Intervention Strategies: The Therapeutic Nutrition Algorithm
Iron Deficiency Management: The Restoration Protocol
Treatment Intensity: Matched to deficiency severity and underlying etiology.
Mild Iron Deficiency (ferritin 12-15 ng/mL):
- Dietary optimization: Iron-rich foods 3x daily
- Enhancers: Vitamin C 25-75 mg with iron-containing meals
- Inhibitor avoidance: Separate calcium, tea, coffee by 2 hours
- Monitoring: Hemoglobin and ferritin at 4-6 weeks
Moderate-Severe Iron Deficiency (ferritin <12 ng/mL):
- Elemental iron: 3-6 mg/kg/day divided into 2-3 doses
- Formulation: Ferrous sulfate most bioavailable (20% elemental iron)
- Duration: 3 months beyond hemoglobin normalization
- Response: Hemoglobin increase 1-2 g/dL within 4 weeks
📌 Remember: IRON supplementation principles - Incremental dosing, Reticulocyte response in 5-10 days, Optimal absorption on empty stomach, Normalization takes 2-4 months
Side Effect Management:
- Gastrointestinal intolerance: 10-20% incidence, dose-dependent
- Mitigation strategies: Start low dose, take with food, liquid preparations
- Alternative forms: Iron bisglycinate better tolerated, equivalent efficacy
Vitamin D Deficiency: The Bone Health Restoration
Deficiency Classification and Treatment:
Insufficiency (25(OH)D 20-30 ng/mL):
- Daily dosing: 1000-2000 IU/day for 6-8 weeks
- Maintenance: 600-1000 IU/day ongoing
- Monitoring: 25(OH)D level at 8-12 weeks
Deficiency (25(OH)D <20 ng/mL):
- High-dose therapy: 50,000 IU weekly for 6-8 weeks
- Alternative: 6000 IU daily for 8 weeks
- Maintenance: 1000-2000 IU daily after repletion
- Cofactors: Adequate calcium 500-1300 mg/day and magnesium
| Deficiency Type | 25(OH)D Level | Treatment Dose | Duration | Expected Response | Maintenance |
|---|---|---|---|---|---|
| Insufficiency | 20-30 ng/mL | 1000-2000 IU/day | 6-8 weeks | 10-15 ng/mL ↑ | 600-1000 IU/day |
| Mild deficiency | 10-20 ng/mL | 50,000 IU/week | 6-8 weeks | 20-30 ng/mL ↑ | 1000-2000 IU/day |
| Severe deficiency | <10 ng/mL | 50,000 IU 2x/week | 8-12 weeks | 30-40 ng/mL ↑ | 2000-4000 IU/day |
| Rickets | <10 ng/mL + symptoms | 50,000 IU 2x/week | 12-16 weeks | Clinical improvement | 2000-4000 IU/day |
Zinc Deficiency: The Growth Catalyst
Therapeutic Zinc Supplementation:
- Dosing: 10-20 mg elemental zinc/day for 2-4 months
- Formulation: Zinc sulfate most studied, zinc gluconate better tolerated
- Timing: 1 hour before or 2 hours after meals for optimal absorption
- Response: Growth velocity improvement within 4-6 weeks
Monitoring Parameters:
- Serum zinc: Target >70 μg/dL after 8-12 weeks
- Growth velocity: Expect 25-50% improvement in linear growth
- Immune function: Reduced infection frequency by 30-40%
💡 Master This: Zinc-copper interaction - prolonged zinc supplementation >40 mg/day can induce copper deficiency, monitor copper status with long-term therapy
Connect intervention strategies through comprehensive monitoring protocols to ensure optimal outcomes and prevent complications.
⚖️ Intervention Strategies: The Therapeutic Nutrition Algorithm
🔗 Integration Matrix: The Multi-System Nutritional Network
Nutrient Synergies: The Biochemical Orchestra
Iron-Vitamin C Partnership: Classic example of nutritional synergy optimizing bioavailability.
- Mechanism: Vitamin C reduces Fe³⁺ to Fe²⁺, increasing absorption 3-4 fold
- Optimal ratio: 25-75 mg vitamin C per 10-15 mg iron
- Clinical application: Orange juice with iron-fortified cereal increases absorption from 3% to 12%
- Timing: Simultaneous consumption required - vitamin C effect lasts <2 hours
Calcium-Vitamin D-Magnesium Triad: Essential for optimal bone mineralization and growth.
- Calcium absorption: 25-30% with adequate vitamin D, <10% when deficient
- Magnesium requirement: 50-60% of calcium intake for optimal bone health
- PTH regulation: Maintains calcium homeostasis when vitamin D >30 ng/mL
- Growth impact: Optimal triad increases linear growth velocity by 15-20%
📌 Remember: ZINC-IRON competition - Zinc and Iron compete for Name Carrier proteins, separate supplementation by 2 hours for optimal absorption
Metabolic Integration Pathways
Protein-Energy Malnutrition Cascade: Understanding the progression reveals intervention targets.
- Phase 1: Glycogen depletion (12-24 hours)
- Phase 2: Fat mobilization (2-7 days)
- Phase 3: Protein catabolism (>7 days)
- Phase 4: Organ dysfunction (>14 days)
- Recovery: Reverse order with anabolic rebound requiring 150-200% normal intake
Micronutrient Cofactor Networks: Essential for macronutrient metabolism.
- Carbohydrate metabolism: Requires thiamine, niacin, riboflavin, magnesium
- Fat metabolism: Depends on carnitine, riboflavin, niacin, pantothenic acid
- Protein synthesis: Needs folate, B₁₂, zinc, magnesium, vitamin B₆
- Energy production: Integrates iron, copper, magnesium, phosphorus
Growth Factor Interactions
IGF-1 Nutritional Regulation: The master growth coordinator responding to nutritional status.
- Protein requirement: >1.0 g/kg/day maintains IGF-1 production
- Zinc dependency: IGF-1 synthesis requires adequate zinc status
- Energy threshold: IGF-1 drops 50-70% with energy restriction <80% needs
- Recovery time: IGF-1 normalization takes 2-4 weeks after nutritional restoration
Leptin-Ghrelin Balance: Appetite regulation integrating energy status and growth needs.
- Leptin production: Proportional to fat mass, signals satiety
- Ghrelin secretion: Increases 2-3 fold before meals, stimulates appetite
- Nutritional modulation: Protein increases satiety 25-30% more than carbohydrates
- Developmental changes: Leptin sensitivity decreases during adolescent growth spurts
| System Integration | Key Nutrients | Interaction Mechanism | Clinical Outcome | Optimization Strategy |
|---|---|---|---|---|
| Bone-Immune | Vitamin D, calcium | VDR activation | 36% ↓ infections | 25(OH)D >30 ng/mL |
| Brain-Growth | Iron, zinc, DHA | Neurotransmitter synthesis | 15-20% ↑ cognition | Early intervention |
| GI-Absorption | Folate, B₁₂, zinc | Enterocyte turnover | 40-60% ↑ bioavailability | Gut health priority |
| Muscle-Metabolism | Protein, leucine | mTOR activation | 25-30% ↑ lean mass | Post-exercise timing |
| Immune-Inflammation | Zinc, vitamin A | Cytokine modulation | 30-40% ↓ infections | Adequate status |
Cutting-Edge Nutritional Genomics
Nutrigenomics Applications: Personalized nutrition based on genetic variations affecting nutrient metabolism.
- MTHFR polymorphisms: 40-50% population frequency, affects folate requirements
- Lactase persistence: 65% global lactose intolerance, varies by ethnicity
- Iron metabolism genes: HFE mutations affect iron absorption and storage
- Vitamin D receptor: VDR polymorphisms influence vitamin D sensitivity
Epigenetic Nutrition Effects: Early nutritional experiences modify gene expression patterns.
- DNA methylation: Folate, B₁₂, choline influence methylation patterns
- Histone modifications: Protein restriction alters growth gene expression
- Critical windows: First 1000 days most susceptible to epigenetic programming
- Transgenerational effects: Maternal nutrition affects 2-3 generations
💡 Master This: Nutritional resilience develops through diverse food exposure during complementary feeding - children exposed to >20 different foods by 12 months show 40-50% lower allergy rates and better micronutrient status
Connect multi-system integration through practical clinical mastery tools for immediate application in pediatric practice.
🔗 Integration Matrix: The Multi-System Nutritional Network
🎯 Clinical Mastery Toolkit: The Pediatric Nutrition Command Center
The Essential Numbers Arsenal
Growth Velocity Red Flags - Memorize these thresholds for instant recognition:
- Weight gain <15 g/day (0-3 months) = immediate evaluation
- Length velocity <2 cm/month (0-6 months) = growth failure
- Head circumference <0.5 cm/month (6-12 months) = concerning
- BMI crossing >2 percentile lines = nutritional intervention needed
Laboratory Action Thresholds:
- Hemoglobin <11.0 g/dL (6 months-5 years) = iron deficiency workup
- Ferritin <15 ng/mL = iron supplementation indicated
- 25(OH)D <20 ng/mL = vitamin D deficiency treatment
- Albumin <3.5 g/dL = protein malnutrition assessment
📌 Remember: FAST nutrition screening - Ferritin <15, Albumin <3.5, Stunting (LAZ <-2), Thinness (WHZ <-2)
Rapid Assessment Protocol
The 60-Second Nutrition Screen:
- Plot growth parameters (15 seconds) - identify crossing percentiles
- Calculate growth velocity (15 seconds) - compare to age norms
- Visual inspection (15 seconds) - pallor, muscle wasting, edema
- Dietary recall (15 seconds) - milk intake, iron sources, variety
High-Yield Physical Findings:
- Pallor: Check conjunctiva, nail beds - sensitivity 85% for anemia
- Koilonychia: Spoon-shaped nails - specific for iron deficiency
- Angular cheilitis: Cracks at mouth corners - B-vitamin deficiency
- Dental caries: >3 cavities suggests poor dietary quality
| Clinical Pearl | Recognition Pattern | Immediate Action | Follow-up Timeline |
|---|---|---|---|
| Iron deficiency | Pallor + pica + fatigue | CBC, ferritin, iron supplement | 4-6 weeks |
| Vitamin D deficiency | Bone pain + dental delay | 25(OH)D, high-dose vitamin D | 8-12 weeks |
| Protein malnutrition | Edema + hair changes | Albumin, prealbumin, nutrition consult | 2-4 weeks |
| Zinc deficiency | Poor growth + infections | Serum zinc, zinc supplement | 8-12 weeks |
| Failure to thrive | Growth deceleration | Comprehensive assessment | 2-4 weeks |
Evidence-Based Intervention Protocols
Iron Deficiency Treatment Algorithm:
- Mild (Hgb 10-11 g/dL): 2-3 mg/kg/day elemental iron × 3 months
- Moderate (Hgb 8-10 g/dL): 3-6 mg/kg/day elemental iron × 3-6 months
- Severe (Hgb <8 g/dL): 6 mg/kg/day + investigate underlying cause
Vitamin D Deficiency Protocol:
- Insufficiency: 1000-2000 IU/day × 6-8 weeks
- Deficiency: 50,000 IU/week × 6-8 weeks, then maintenance
- Rickets: 50,000 IU twice weekly × 12 weeks + calcium
💡 Master This: The Rule of 3s for supplement monitoring - check response at 3 days (tolerance), 3 weeks (early response), 3 months (full effect), then every 3 months for maintenance
Feeding Problem Triage:
- Organic causes (15%): Growth failure + medical symptoms
- Non-organic causes (85%): Normal growth velocity + behavioral issues
- Mixed causes (30%): Combination requiring multidisciplinary approach
This clinical mastery toolkit provides the foundation for expert pediatric nutrition practice, enabling rapid assessment, evidence-based interventions, and optimal developmental outcomes across all pediatric populations.
🎯 Clinical Mastery Toolkit: The Pediatric Nutrition Command Center
Practice Questions: Nutritional requirements and disorders
Test your understanding with these related questions
A 61-year-old woman presents for a routine health visit. She complains of generalized fatigue and lethargy on most days of the week for the past 4 months. She has no significant past medical history and is not taking any medications. She denies any history of smoking or recreational drug use but states that she drinks "socially" approx. 6 nights a week. She says she also enjoys a "nightcap," which is 1–2 glasses of wine before bed every night. The patient is afebrile, and her vital signs are within normal limits. On physical examination, there is significant pallor of the mucous membranes. Laboratory findings are significant for a mean corpuscular volume (MCV) of 72 fL, leukocyte count of 4,800/mL, hemoglobin of 11.0 g/dL, and platelet count of 611,000/mL. Stool guaiac test is negative. She is started on oral ferrous sulfate supplements. On follow-up, her laboratory parameters show no interval change in her MCV or platelet level, and she reports good compliance with the medication. Which of the following is the best next step in the management of this patient?













