Neonatal meningitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neonatal meningitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neonatal meningitis US Medical PG Question 1: A 7-year-old boy is brought to the emergency department because of high-grade fever and lethargy for 4 days. He has had a severe headache for 3 days and 2 episodes of non-bilious vomiting. He has sickle cell disease. His only medication is hydroxyurea. His mother has refused vaccinations and antibiotics in the past because of their possible side effects. He appears ill. His temperature is 40.1°C (104.2°F), pulse is 131/min, and blood pressure is 92/50 mm Hg. Examination shows nuchal rigidity. Kernig and Brudzinski signs are present. A lumbar puncture is performed. Analysis of the cerebrospinal fluid (CSF) shows a decreased glucose concentration, increased protein concentration, and numerous segmented neutrophils. A Gram stain of the CSF shows gram-negative coccobacilli. This patient is at greatest risk for which of the following complications?
- A. Adrenal insufficiency
- B. Cerebral palsy
- C. Hearing loss (Correct Answer)
- D. Communicating hydrocephalus
- E. Brain abscess
Neonatal meningitis Explanation: ***Hearing loss***
- The patient has bacterial meningitis, likely caused by *Haemophilus influenzae* type b given the **gram-negative coccobacilli** and his unvaccinated status.
- **Sensorineural hearing loss is the MOST COMMON long-term neurological sequela of bacterial meningitis**, occurring in 10-30% of survivors, making this the greatest risk for this patient.
- It results from inflammation of the **cochlea and eighth cranial nerve**, which can occur even with appropriate treatment.
- Children with *H. influenzae* meningitis are at particularly high risk for this complication.
*Adrenal insufficiency*
- While adrenal hemorrhage and crisis can occur with overwhelming sepsis (Waterhouse-Friderichsen syndrome), this is **classically associated with meningococcemia**, not *H. influenzae*.
- It is an acute complication of septic shock rather than a common sequela of meningitis itself.
*Cerebral palsy*
- Cerebral palsy requires significant hypoxic-ischemic injury or extensive brain damage during the acute illness.
- While possible with severe meningitis, it is a **much less common** complication compared to hearing loss.
*Communicating hydrocephalus*
- Can occur due to impaired CSF reabsorption at the arachnoid granulations following meningeal inflammation.
- This is a recognized complication but occurs in **fewer than 5-10%** of cases, making it less common than hearing loss.
*Brain abscess*
- Brain abscess represents a focal parenchymal infection and is a **rare complication** of bacterial meningitis.
- It typically occurs when infection spreads from contiguous sites or when meningitis is inadequately treated.
Neonatal meningitis US Medical PG Question 2: A previously healthy 10-day-old infant is brought to the emergency department by his mother because of episodes of weakness and spasms for the past 12 hours. His mother states that he has also had difficulty feeding and a weak suck. He has not had fever, cough, diarrhea, or vomiting. He was born at 39 weeks' gestation via uncomplicated vaginal delivery at home. Pregnancy was uncomplicated. The mother refused antenatal vaccines out of concern they would cause side effects. She is worried his symptoms may be from some raw honey his older sister maybe inadvertently fed him 5 days ago. He appears irritable. His temperature is 37.1°C (98.8°F). Examination shows generalized muscle stiffness and twitches. His fontanelles are soft and flat. The remainder of the examination shows no abnormalities. Which of the following is the most likely causal organism?
- A. Listeria monocytogenes
- B. Neisseria meningitidis
- C. Escherichia coli
- D. Clostridium botulinum (Correct Answer)
- E. Clostridium tetani
Neonatal meningitis Explanation: ***Clostridium botulinum***
- The symptoms of **weakness, spasms, difficulty feeding, weak suck**, and history of possible **raw honey ingestion** are highly suggestive of **infant botulism**.
- **Infant botulism** occurs when *Clostridium botulinum* spores are ingested and colonize the immature gut, producing **neurotoxins** that cause **descending flaccid paralysis**.
- The "muscle stiffness" noted can represent early hypotonia and the **loss of head control** typical of botulism, rather than true spastic rigidity.
- **Honey exposure** in infants under 12 months is a classic risk factor due to spore contamination.
*Listeria monocytogenes*
- This pathogen typically causes **meningitis** or **sepsis** in neonates, with symptoms such as **fever, lethargy**, and **poor feeding**, which differ from the presented neuromuscular symptoms.
- While *Listeria* can be transmitted transplacentally or during birth, it would not be directly associated with the ingestion of **honey**.
*Neisseria meningitidis*
- *N. meningitidis* is a common cause of **bacterial meningitis** and **meningococcemia**, presenting with **fever, rash, irritability**, and **meningeal signs**, which are not the primary symptoms described.
- While it can affect infants, it does not typically cause the specific **neuromuscular symptoms** seen in this patient nor is it linked to honey ingestion.
*Escherichia coli*
- **E. coli** is a frequent cause of **neonatal sepsis** and **meningitis**, often presenting with **fever, poor feeding, lethargy, and vomiting**.
- The clinical picture of **weakness, difficulty feeding**, and **neuromuscular symptoms** without significant fever or systemic signs points away from typical *E. coli* infections.
*Clostridium tetani*
- **Clostridium tetani** causes **tetanus**, characterized by **muscle spasms, rigidity, and lockjaw** (trismus), which represents **spastic paralysis**.
- However, the history of **raw honey ingestion** is a classic risk factor for **botulism**, not tetanus.
- **Neonatal tetanus** is associated with unhygienic umbilical cord practices, and while **rigidity** is prominent in tetanus, the **flaccid paralysis, weakness**, and **weak suck** are characteristic of **botulism**, not tetanus.
Neonatal meningitis US Medical PG Question 3: An infant boy of unknown age and medical history is dropped off in the emergency department. The infant appears lethargic and has a large protruding tongue. Although the infant exhibits signs of neglect, he is in no apparent distress. The heart rate is 70/min, the respiratory rate is 30/min, and the temperature is 35.7°C (96.2°F). Which of the following is the most likely cause of the patient’s physical exam findings?
- A. Autosomal dominant mutation in the SERPING1 gene
- B. Genetic imprinting disorder affecting chromosome 11p15.5
- C. Type I hypersensitivity reaction
- D. Excess growth hormone secondary to pituitary gland tumor
- E. Congenital agenesis of an endocrine gland in the anterior neck (Correct Answer)
Neonatal meningitis Explanation: ***Congenital agenesis of an endocrine gland in the anterior neck***
- This description is highly suggestive of **congenital hypothyroidism**, caused by **thyroid dysgenesis** (agenesis or hypoplasia of the thyroid gland).
- Symptoms include **lethargy**, **macroglossia** (large protruding tongue), **hypotonia**, **feeding difficulties**, **umbilical hernia**, and **hypothermia**, all consistent with the clinical picture.
*Autosomal dominant mutation in the SERPING1 gene*
- A mutation in the **SERPING1 gene** causes **hereditary angioedema**, characterized by recurrent episodes of unpredictable swelling in various body parts.
- While swelling can affect the tongue, it is typically episodic, painful, and often triggered, which is not suggested by the chronic lethargy and physical signs described.
*Genetic imprinting disorder affecting chromosome 11p15.5*
- This describes **Beckwith-Wiedemann syndrome**, an overgrowth disorder caused by imprinting defects involving genes like **IGF2**, **H19**, and **CDKN1C** on chromosome 11p15.5.
- Features include **macroglossia**, **macrosomia**, **umbilical hernia**, **hemihyperplasia**, and increased risk of embryonal tumors like **Wilms tumor**.
- However, Beckwith-Wiedemann syndrome does not typically present with profound **lethargy** and **hypothermia** as seen in congenital hypothyroidism.
*Type I hypersensitivity reaction*
- A **Type I hypersensitivity reaction** (e.g., anaphylaxis) could cause acute **angioedema** of the tongue, but this would be an acute, rapidly progressing, and life-threatening event.
- The infant's description of being "in no apparent distress" and exhibiting chronic signs like lethargy and hypothermia makes an acute allergic reaction unlikely.
*Excess growth hormone secondary to pituitary gland tumor*
- **Excess growth hormone** (gigantism in children, acromegaly in adults) can cause **macroglossia** and coarse facial features in the long term.
- However, it does not explain the associated **lethargia**, **hypothermia**, and profound developmental delay seen in congenital hypothyroidism in an infant.
Neonatal meningitis US Medical PG Question 4: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Neonatal meningitis Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Neonatal meningitis US Medical PG Question 5: A 10-year-old boy is brought to the emergency department by his parents because of a dull persistent headache beginning that morning. He has nausea and has vomited twice. During the past four days, the patient has had left-sided ear pain and fever, but his parents did not seek medical attention. He is from Thailand and is visiting his relatives in the United States for the summer. There is no personal or family history of serious illness. He is at the 45th percentile for height and 40th percentile for weight. He appears irritable. His temperature is 38.5°C (101.3°F), pulse is 110/min, and blood pressure is 98/58 mm Hg. The pupils are equal and reactive to light. Lateral gaze of the left eye is limited. The left tympanic membrane is erythematous with purulent discharge. There is no nuchal rigidity. Which of the following is the most appropriate next step in management?
- A. Intravenous ceftriaxone and clindamycin therapy
- B. Lumbar puncture
- C. MRI of the brain (Correct Answer)
- D. Intravenous cefazolin and metronidazole therapy
- E. Cranial burr hole evacuation
Neonatal meningitis Explanation: ***MRI of the brain***
- The patient's presentation with **headache**, **nausea**, **vomiting**, recent **ear infection** (otitis media), **fever**, and **abducens nerve palsy** (limited lateral gaze of the left eye) is highly suggestive of an intracranial complication, such as a **brain abscess** or **epidural abscess**, secondary to the uncontrolled otitis media.
- An MRI of the brain is the **most sensitive and specific imaging modality** for detecting intracranial abscesses, which are critical to diagnose promptly due to their potential for surgical drainage and targeted antibiotic therapy.
*Intravenous ceftriaxone and clindamycin therapy*
- While broad-spectrum antibiotics are necessary, they should be initiated **after establishing a definitive diagnosis and ruling out conditions requiring immediate surgical intervention**.
- Without imaging, there's a risk of delaying crucial surgical management for a contained abscess or empyema.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the presence of focal neurological deficits (like **abducens nerve palsy**) and symptoms of **increased intracranial pressure** (headache, nausea, vomiting), as it carries a significant risk of **herniation** if there's a mass lesion.
- Imaging should always precede LP in such cases.
*Intravenous cefazolin and metronidazole therapy*
- Cefazolin has **poor penetration into the CNS**, making it an inadequate choice for suspected intracranial infection.
- While metronidazole targets anaerobes common in brain abscesses, the overall regimen is not optimal, and imaging is still the priority.
*Cranial burr hole evacuation*
- This is a definitive surgical treatment for a brain abscess but should only be performed **after the abscess has been localized and characterized by imaging**.
- Performing a burr hole without prior imaging would be a blind procedure and is not the appropriate next step in diagnosis and management.
Neonatal meningitis US Medical PG Question 6: A mother delivers in a rural area under the guidance of a skilled care attendant. Which of the following statements is incorrect regarding the care provided by the skilled care attendant at birth?
- A. Start breastfeeding as early as possible
- B. Cover the baby's head and body
- C. Bathe the baby with warm water (Correct Answer)
- D. Clear the eyes with a sterile swab
- E. Dry the baby thoroughly and stimulate breathing
Neonatal meningitis Explanation: ***Bathe the baby with warm water***
- **Delaying the first bath** for at least 6-24 hours after birth is recommended to prevent **hypothermia** and promote **skin-to-skin contact** for bonding and breastfeeding.
- Early bathing can remove **vernix caseosa**, which provides natural antimicrobial protection and moisturization to the newborn's skin.
*Start breastfeeding as early as possible*
- **Early initiation of breastfeeding**, ideally within the first hour of birth, is crucial for both mother and baby.
- It promotes **uterine contractions** to prevent **postpartum hemorrhage** and provides the newborn with **colostrum**, rich in antibodies.
*Cover the baby's head and body*
- Covering the newborn's head and body is essential to prevent **heat loss** and maintain a stable **body temperature**, immediately after birth.
- Newborns are highly susceptible to **hypothermia** due to their large surface area to mass ratio and immature thermoregulation.
*Clear the eyes with a sterile swab*
- Clearing the newborn's eyes with a sterile swab is a standard part of immediate newborn care to remove any **mucus or blood** that might have entered during delivery.
- This helps prevent **ophthalmia neonatorum**, especially if the mother has an infection like gonorrhea or chlamydia.
*Dry the baby thoroughly and stimulate breathing*
- **Drying the baby immediately** after birth is a critical first step in newborn resuscitation and care.
- It helps prevent **hypothermia** and provides **tactile stimulation** to initiate breathing and crying, which is essential for transitioning from fetal to neonatal circulation.
Neonatal meningitis US Medical PG Question 7: An 8-day-old male infant presents to the pediatrician with a high-grade fever and poor feeding pattern with regurgitation of milk after each feeding. On examination the infant showed abnormal movements, hypertonia, and exaggerated DTRs. The mother explains that during her pregnancy, she has tried to eat only unprocessed foods and unpasteurized dairy so that her baby would not be exposed to any preservatives or unhealthy chemicals. Which of the following characteristics describes the causative agent that caused this illness in the infant?
- A. Gram-positive, facultative intracellular, motile bacilli (Correct Answer)
- B. Gram-negative, maltose fermenting diplococci
- C. Gram-positive, catalase-negative, alpha hemolytic, optochin sensitive cocci
- D. Gram-positive, catalase-negative, beta hemolytic, bacitracin resistant cocci
- E. Gram-negative, lactose-fermenting, facultative anaerobic bacilli
Neonatal meningitis Explanation: ***Gram-positive, facultative intracellular, motile bacilli***
- The infant's symptoms (fever, poor feeding, regurgitation, abnormal movements, hypertonia, exaggerated DTRs) are highly suggestive of **meningitis** or **meningoencephalitis** in a neonate.
- The mother's consumption of **unpasteurized dairy** is a significant risk factor for **Listeria monocytogenes infection**, which is a **gram-positive, facultative intracellular, motile bacillus** that can cause neonatal sepsis and meningitis.
*Gram-negative, maltose fermenting diplococci*
- This description refers to **Neisseria meningitidis**, which is a common cause of meningitis but typically affects older infants, children, and young adults.
- While Neisseria can cause neonatal infection, it is less commonly associated with unpasteurized dairy consumption.
*Gram-positive, catalase-negative, alpha hemolytic, optochin sensitive cocci*
- This describes **Streptococcus pneumoniae**, a common cause of bacterial meningitis, otitis media, and pneumonia.
- S. pneumoniae is generally **catalase-negative** and **alpha-hemolytic**, but it is not typically associated with unpasteurized dairy transmission in neonates.
*Gram-positive, catalase-negative, beta hemolytic, bacitracin resistant cocci*
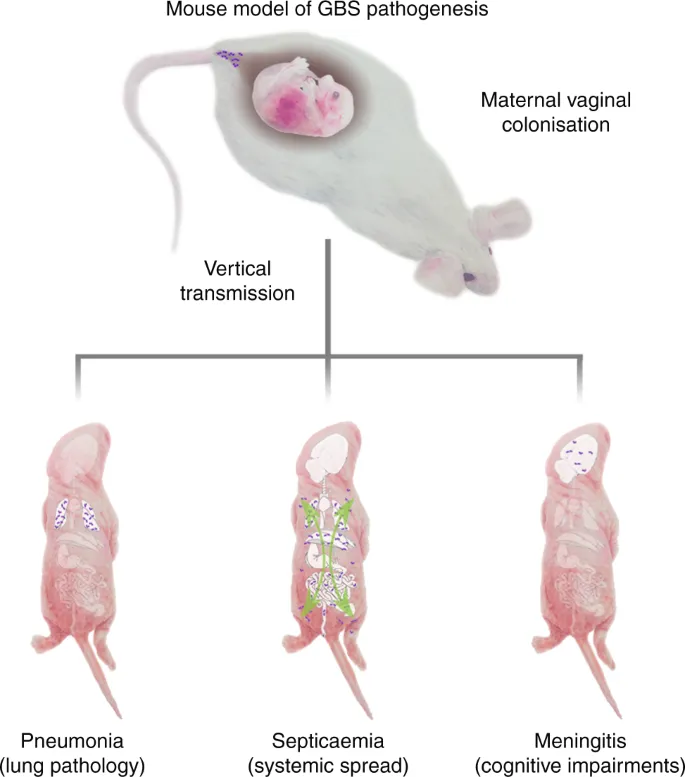
- This description points to **Group B Streptococcus (Streptococcus agalactiae)**, a leading cause of early-onset neonatal sepsis and meningitis.
- While GBS is a common neonatal pathogen, it is transmitted vertically from the mother's birth canal and not primarily through unpasteurized dairy products.
*Gram-negative, lactose-fermenting, facultative anaerobic bacilli*
- This describes organisms like **Escherichia coli**, a common cause of neonatal meningitis, especially in premature or low-birth-weight infants.
- While E. coli can be transmitted via fecal-oral routes, the specific history of unpasteurized dairy strongly points away from E. coli as the *most likely* causative agent in this scenario.
Neonatal meningitis US Medical PG Question 8: Three days after delivery, a 1100-g (2-lb 7-oz) newborn has a tonic seizure that lasts for 25 seconds. She has become increasingly lethargic over the past 18 hours. She was born at 31 weeks' gestation. Antenatal period was complicated by chorioamnionitis. Apgar scores were 3 and 6 at 1 and 5 minutes, respectively. She appears ill. Her pulse is 123/min, respirations are 50/min and irregular, and blood pressure is 60/30 mm Hg. Examination shows a tense anterior fontanelle. The pupils are equal and react sluggishly to light. Examination shows slow, conjugate back and forth movements of the eyes. Muscle tone is decreased in all extremities. The lungs are clear to auscultation. Which of the following is the most likely diagnosis?
- A. Intraventricular hemorrhage (Correct Answer)
- B. Spinal muscular atrophy
- C. Galactosemia
- D. Congenital hydrocephalus
- E. Phenylketonuria
Neonatal meningitis Explanation: ***Intraventricular hemorrhage***
- The combination of **prematurity** (31 weeks' gestation, 1100g), **tonic seizures**, increasing **lethargy**, tense **anterior fontanelle**, **sluggishly reactive pupils**, and **slow conjugate back-and-forth eye movements** (suggesting brainstem involvement from increased intracranial pressure) are classical signs of intraventricular hemorrhage (IVH) in a neonate.
- **IVH** is common in premature infants due to the fragility of germinal matrix vessels and can manifest acutely with neurological deterioration and increased intracranial pressure, typically within the first 72 hours of life.
- While maternal **chorioamnionitis** and low Apgar scores raise concern for neonatal sepsis/meningitis, the specific **ocular movement pattern** and acute neurological signs on day 3 are more characteristic of IVH in this extremely premature infant.
*Spinal muscular atrophy*
- This is a **neuromuscular genetic disorder** characterized by progressive muscle weakness and hypotonia due to anterior horn cell degeneration.
- It would typically present with **decreased muscle tone but without acute neurological signs** like seizures, tense fontanelle, or sluggish pupillary responses.
- Does not cause acute-onset seizures or rapidly progressing lethargy in the neonatal period.
*Galactosemia*
- This is a **metabolic disorder** that presents with symptoms such as **vomiting, jaundice, hepatomegaly**, and **sepsis-like symptoms** upon introduction of lactose-containing feeds (breast milk or regular formula), typically after several days of feeding.
- While it can cause lethargy and seizures, the acute neurological findings including **tense fontanelle** and **abnormal eye movements** in the immediate postnatal period of a premature infant more strongly suggest an anatomical/structural etiology like IVH.
*Congenital hydrocephalus*
- While **hydrocephalus** can cause a **tense fontanelle** and seizures, the **acute onset** of symptoms (day 3 of life with rapid deterioration over 18 hours following a specific tonic seizure) in an extremely premature infant strongly suggests an **acute hemorrhagic event** rather than congenital hydrocephalus.
- Congenital hydrocephalus typically presents with **progressively enlarging head circumference** over time, rather than such acute neurological deterioration in the first 72 hours of life.
- IVH can lead to secondary post-hemorrhagic hydrocephalus, but the acute presentation favors primary IVH.
*Phenylketonuria*
- This is a **metabolic disorder** caused by phenylalanine hydroxylase deficiency that, if untreated, leads to **intellectual disability** and seizures.
- Symptoms typically manifest **several months after birth** (usually 3-6 months) as phenylalanine accumulates, and are not associated with acute neonatal neurological distress like tense fontanelle, abnormal eye movements, or acute lethargy in the first few days of life.
- Would not explain the acute deterioration on day 3 of life in this clinical context.
Neonatal meningitis US Medical PG Question 9: A 2860-g (6-lb 3-oz) male newborn is born at term to a primigravid woman via spontaneous vaginal delivery. The mother has had no routine prenatal care. She reports that there is no family history of serious illness. The initial examination of the newborn shows bowing of the legs and respiratory distress upon palpation of the chest. The skin and joints are hyperextensible. X-rays of the chest and skull show multiple rib fractures and small, irregular bones along the cranial sutures. The patient is at increased risk of which of the following complications?
- A. Hearing loss (Correct Answer)
- B. Spinal canal stenosis
- C. Costochondral junction enlargement
- D. Intestinal rupture
- E. Intellectual disability
Neonatal meningitis Explanation: ***Hearing loss***
- The described clinical picture of **bone fragility (multiple rib fractures, bowing of legs)**, **hyperextensible skin and joints**, and **wormian bones** (small, irregular bones along cranial sutures) is classic for **osteogenesis imperfecta (OI)**.
- Individuals with OI are at increased risk for **conductive or sensorineural hearing loss**, which can manifest in childhood or adolescence.
*Spinal canal stenosis*
- While patients with OI can develop **scoliosis** and **vertebral compression fractures**, resulting in spinal cord compression, **spinal canal stenosis** itself is not a primary or direct complication of the underlying collagen defect in the same way hearing loss is.
- The primary spinal complications are related to **vertebral fractures** and **deformities**.
*Costochondral junction enlargement*
- **Costochondral junction enlargement** (rachitic rosary) is a hallmark of **rickets**, a disorder of **vitamin D or phosphate metabolism**, not osteogenesis imperfecta.
- The described features point to a **collagen synthesis defect**, not mineralization issues.
*Intestinal rupture*
- While there can be some smooth muscle abnormalities, **intestinal rupture** is not a commonly described or significant complication of osteogenesis imperfecta.
- The primary systemic manifestations relate to **collagen defects** in bone, skin, tendons, and blood vessels, but not typically leading to spontaneous gastrointestinal rupture.
*Intellectual disability*
- **Intellectual function** is typically **unaffected** in osteogenesis imperfecta.
- The disease primarily affects **connective tissue**, particularly bone development, and does not directly cause cognitive impairment.
Neonatal meningitis US Medical PG Question 10: A 7-year-old boy is brought to the emergency department because of a 3-day history of generalized fatigue, myalgia, and fever. He has sickle cell disease. His current medications include hydroxyurea and folic acid. He appears ill. His temperature is 39.2°C (102.6°F), pulse is 103/min, and respirations are 28/min. Examination shows pale conjunctivae. The lungs are clear to auscultation. The abdomen is soft and nontender. Neurologic examination shows no focal findings, His hemoglobin concentration is 10.3 g/dL and leukocyte count is 14,100/mm3. Intravenous fluid is administered and blood cultures are obtained. Which of the following is the most appropriate next step in treatment?
- A. Clindamycin
- B. Prednisone
- C. Vancomycin
- D. Ceftriaxone (Correct Answer)
- E. Levofloxacin
Neonatal meningitis Explanation: ***Ceftriaxone***
- This patient presents with **fever** and **sickle cell disease**, placing him at high risk for bacterial infections, especially from **encapsulated organisms** like *Streptococcus pneumoniae* and *Haemophilus influenzae*. **Ceftriaxone** is a broad-spectrum third-generation cephalosporin that provides excellent coverage against these common pathogens.
- Due to the high risk of **sepsis** and rapid progression of infection in sickle cell patients, empiric, prompt administration of **intravenous antibiotics** is crucial, even before culture results are available.
*Clindamycin*
- **Clindamycin** is primarily effective against **anaerobic bacteria** and some gram-positive organisms, including methicillin-sensitive *Staphylococcus aureus* (MSSA).
- It does not provide adequate coverage against the most common and life-threatening pathogens in febrile sickle cell patients, such as encapsulated bacteria.
*Prednisone*
- **Prednisone** is a corticosteroid used for its **anti-inflammatory** and immunosuppressive effects. It is not indicated for the initial management of fever and suspected bacterial infection.
- Administering corticosteroids in a patient with suspected infection without appropriate antibiotic coverage could worsen the infection.
*Vancomycin*
- **Vancomycin** is a powerful antibiotic primarily used to cover **multi-drug resistant gram-positive bacteria**, especially **MRSA** and drug-resistant *S. pneumoniae*.
- While it covers gram-positive organisms well, it does **not cover gram-negative bacteria** such as *H. influenzae* or *Salmonella* species, which are important pathogens in sickle cell patients. **Ceftriaxone** provides broader coverage including both gram-positive and gram-negative encapsulated organisms, making it the preferred empiric choice.
*Levofloxacin*
- **Levofloxacin** is a fluoroquinolone that provides broad-spectrum coverage, including against atypical organisms and some gram-negatives and gram-positives.
- However, **fluoroquinolones** are generally avoided in children due to potential adverse effects on cartilage development, and it is not the first-line empiric choice for severe bacterial infections in this age group, especially when **cephalosporins** are highly effective and safer.
More Neonatal meningitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.