Milestones

On this page
🎯 The Milestone Mastery Blueprint
Developmental milestones form the diagnostic backbone of pediatrics, revealing whether a child's brain and body are unfolding on schedule or signaling hidden pathology. You'll master how to systematically screen, interpret delays through cultural and biological lenses, distinguish benign variation from true disorder, and deploy evidence-based interventions that change trajectories. This lesson builds your clinical eye for spotting red flags early, your judgment for knowing when to watch versus refer, and your confidence to guide anxious families through one of medicine's most consequential assessments.
Mastering milestone assessment requires understanding both the sequential nature of development and the critical windows for intervention. Each milestone builds upon previous achievements, creating a developmental cascade where early delays can compound into significant functional limitations.
📌 Remember: MILE - Motor skills first, Integration follows, Language emerges, Emotional bonding throughout
The milestone framework encompasses four primary domains: gross motor (25% of assessment), fine motor (20%), language (30%), and social-emotional development (25%). Each domain follows predictable sequences with defined age ranges, though individual variation can span ±2-4 months for most milestones.
-
Gross Motor Development
- Head control: 2-4 months (90% achieve by 4 months)
- Sitting independently: 6-8 months (95% by 9 months)
- Walking independently: 12-15 months (90% by 18 months)
- Early walkers: 9-12 months (10% of children)
- Late normal: 15-18 months (requires evaluation if >18 months)
-
Fine Motor Progression
- Pincer grasp: 9-12 months (precision grip development)
- Tower of 2 blocks: 15-18 months
- Tower of 6 blocks: 24-30 months
- Correlates with cognitive development
- Predicts school readiness at 85% accuracy
-
Language Milestones
- First words: 10-14 months (meaningful vocabulary)
- 50 words: 18-24 months (vocabulary explosion)
- 2-word phrases: 18-24 months (syntactic development)
- Delay if <10 words by 18 months
- Referral indicated if no phrases by 30 months
⭐ Clinical Pearl: Children achieving gross motor milestones early (walking by 10 months) show 15% higher cognitive scores at school age, while those walking after 18 months require developmental screening for underlying conditions.
| Domain | 6 Months | 12 Months | 18 Months | 24 Months | 36 Months |
|---|---|---|---|---|---|
| Gross Motor | Sits with support | Walks with support | Walks independently | Runs steadily | Jumps with both feet |
| Fine Motor | Transfers objects | Pincer grasp | Scribbles | Tower of 4 blocks | Copies circle |
| Language | Babbles | First words | 10-20 words | 50+ words, 2-word phrases | 200+ words, sentences |
| Social | Social smile | Waves bye-bye | Points to show | Parallel play | Cooperative play |
| Red Flags | No head control | No sitting | No walking | No words | No phrases |
Understanding milestone variations enables differentiation between constitutional delay (60% of late achievers) and pathological conditions requiring intervention. This foundation connects directly to screening methodologies that systematically evaluate developmental progress.
🎯 The Milestone Mastery Blueprint
🔍 The Developmental Detective Framework
The Denver Developmental Screening Test (DDST-II) remains the gold standard for milestone assessment, evaluating 125 items across four domains from birth to 6 years. The test demonstrates 83% sensitivity and 43% specificity for detecting developmental delays, making it an excellent screening tool rather than diagnostic instrument.
📌 Remember: DDST - Domains are four, Delay needs more, Screening not diagnosis, Tracking shows progress
- DDST Administration Principles
- Age line calculation: Chronological age minus gestational age correction (if <24 months and born <37 weeks)
- Item selection: Test 3 items to the left of age line, all items crossed by age line, and 3 items to the right
- Scoring criteria: Pass, Fail, Refusal, or No Opportunity
- Normal: No delays, maximum 1 caution
- Suspect: ≥2 cautions and/or ≥1 delay
- Untestable: Refusals on ≥25% of items
The screening process reveals developmental patterns that extend beyond individual milestones. Children demonstrating scatter patterns (advanced in some areas, delayed in others) require different interventions than those with global delays affecting all domains equally.
⭐ Clinical Pearl: Parental concerns about development show 74% sensitivity for detecting actual delays - higher than many formal screening tools. Always investigate parental worries, even when formal screening appears normal.
| Screening Tool | Age Range | Domains | Sensitivity | Specificity | Administration Time |
|---|---|---|---|---|---|
| DDST-II | 0-6 years | 4 domains | 83% | 43% | 15-20 minutes |
| ASQ-3 | 1-66 months | 5 domains | 86% | 85% | 10-15 minutes |
| PEDS | 0-8 years | 8 domains | 74% | 64% | 2-10 minutes |
| M-CHAT | 16-30 months | Autism specific | 95% | 95% | 5 minutes |
| BINS | 3-24 months | Neurological | 75-86% | 75-86% | 10 minutes |
- Well-child visits: 9, 18, 24, 30 months (AAP recommendations)
- High-risk populations: Every 3-6 months until 24 months
- Autism screening: 18 and 24 months (M-CHAT-R)
- Additional screening if family history or parental concerns
- Early intervention improves outcomes by 40-60%
💡 Master This: Developmental surveillance differs from screening - surveillance involves continuous monitoring during routine care, while screening uses standardized tools at specific intervals. Both approaches complement each other for optimal detection.
Effective screening identifies children requiring detailed evaluation while avoiding over-referral of normal variants. This systematic approach connects to understanding how cultural factors influence both milestone achievement and screening interpretation.
🔍 The Developmental Detective Framework
🌍 The Cultural Calibration Matrix
Cultural developmental practices affect milestone timing through environmental opportunities, caregiver expectations, and value systems that prioritize different developmental domains. These influences can advance or delay specific milestones by 2-6 months without indicating pathology.
📌 Remember: CULTURE - Context matters most, Understand family values, Language affects timing, Traditions shape practice, Universal needs exist, Respect differences, Evaluate appropriately
-
Motor Development Variations
- Swaddling practices: Delay gross motor milestones by 1-2 months (common in South Asian cultures)
- Floor time: Cultures emphasizing ground-based activities show earlier sitting and crawling
- Carrying practices: Back-carrying (African cultures) may delay independent sitting but enhance trunk strength
- Baby-wearing cultures: 15% later independent sitting
- Tummy time emphasis: 20% earlier rolling and crawling
-
Language Development Patterns
- Multilingual households: Temporary delays in single-language milestones but enhanced overall communication
- Total vocabulary across all languages should meet milestones
- Code-switching emerges by 24-30 months in bilingual children
- Simultaneous bilingualism: May show 6-month delay in single-language measures
- Sequential bilingualism: Silent period of 3-6 months is normal
Indian cultural practices create specific developmental patterns requiring adjusted interpretation. Traditional practices like oil massage, co-sleeping, and extended family involvement influence milestone achievement in predictable ways.
| Cultural Practice | Affected Domain | Timeline Impact | Clinical Consideration |
|---|---|---|---|
| Oil Massage | Gross Motor | +1-2 months earlier | Enhanced muscle tone |
| Co-sleeping | Social-Emotional | Variable | Different attachment patterns |
| Joint Family | Language | +2-3 months earlier | Rich linguistic environment |
| Floor Sitting | Gross Motor | +1 month earlier | Earlier trunk control |
| Hand Feeding | Fine Motor | -1-2 months later | Delayed self-feeding skills |
- Screening Adaptations for Cultural Diversity
- Language assessment: Evaluate total vocabulary across all languages spoken in household
- Motor expectations: Adjust for cultural practices affecting opportunity
- Social milestones: Consider cultural norms for eye contact, stranger interaction
- Some cultures discourage direct eye contact with adults
- Stranger wariness varies significantly across cultures
- Independence expectations differ by 6-12 months between cultures
💡 Master This: Cultural competence in developmental assessment requires distinguishing between cultural variation (normal differences in timing/expression) and cultural disadvantage (limited opportunities affecting development). Both require different clinical responses.
Understanding cultural influences enables accurate screening while respecting family values and traditional practices. This cultural calibration connects directly to systematic evaluation of children identified through screening processes.
🌍 The Cultural Calibration Matrix
🔬 The Diagnostic Deep Dive Architecture
The evaluation process follows structured protocols that systematically explore biological, environmental, and genetic factors contributing to developmental delays. Early identification and intervention can improve outcomes by 40-70% depending on the underlying condition.
📌 Remember: EVALUATE - Etiology first, Validated tools, All domains, Longitudinal view, Underlying causes, Action plan, Team approach, Early intervention
-
Comprehensive History Components
- Prenatal factors: Maternal infections (15% of delays), substance exposure (25% risk), complications (10% risk)
- Perinatal events: Birth weight <1500g (40% delay risk), Apgar <7 at 5 minutes (20% risk)
- Postnatal factors: Head trauma (5% of delays), infections (8%), environmental toxins (12%)
- Lead exposure >5 μg/dL: Cognitive delays in 30%
- Chronic otitis media: Language delays in 25%
-
Physical Examination Priorities
- Growth parameters: Microcephaly (<2nd percentile) suggests genetic/structural causes
- Dysmorphic features: Present in 40% of children with genetic syndromes
- Neurological signs: Asymmetry, tone abnormalities, primitive reflexes
- Persistent primitive reflexes after 6 months: 75% have underlying pathology
- Hypotonia: Present in 60% of children with global delays
Standardized assessment tools provide objective measures of developmental functioning across domains. These tools demonstrate high reliability (r=0.85-0.95) and validity for detecting delays requiring intervention.
| Assessment Tool | Age Range | Domains | Purpose | Reliability |
|---|---|---|---|---|
| Bayley-III | 1-42 months | 5 domains | Comprehensive assessment | r=0.91 |
| Mullen | 0-68 months | 5 domains | Early learning composite | r=0.83 |
| ADOS-2 | 12 months+ | Autism spectrum | Diagnostic gold standard | r=0.92 |
| Vineland-3 | 0-90 years | Adaptive behavior | Functional skills | r=0.93 |
| WISC-V | 6-16 years | Cognitive abilities | IQ assessment | r=0.96 |
- Laboratory Investigation Guidelines
- First-tier testing: Chromosomal microarray, Fragile X, thyroid function
- Second-tier testing: Metabolic screen, lead level, vision/hearing assessment
- Neuroimaging: MRI brain if microcephaly, seizures, or focal signs
- Abnormal MRI: Found in 30-40% of children with global delays
- Diagnostic yield: Higher with dysmorphic features (60%) vs isolated delay (15%)
💡 Master This: Developmental evaluation requires longitudinal assessment over 3-6 months to distinguish transient delays from persistent conditions. Single assessments can miss 25-30% of children who normalize with environmental interventions.

This systematic evaluation framework enables accurate diagnosis and appropriate intervention planning. Understanding evaluation principles connects directly to evidence-based treatment approaches that optimize developmental outcomes.
🔬 The Diagnostic Deep Dive Architecture
⚡ The Intervention Optimization Engine

Intervention effectiveness depends on timing, intensity, and family involvement. Programs initiated before 24 months show 2-3 times greater improvement compared to later interventions, reflecting neuroplasticity advantages during critical periods.
📌 Remember: INTERVENE - Intensity matters, Neuroplasticity peaks early, Team approach, Evidence-based, Routine integration, Very early start, Engage families, Naturalistic methods, Evaluate progress
-
Early Intervention Service Components
- Developmental therapy: 2-3 sessions weekly, 45-60 minutes each
- Speech-language therapy: 1-2 sessions weekly for language delays
- Physical therapy: 1-2 sessions weekly for motor delays
- Intensive programs: >20 hours weekly show 40% greater gains
- Family-centered approach: Doubles intervention effectiveness
-
Evidence-Based Treatment Protocols
- Autism interventions: Applied Behavior Analysis shows 47% improvement in cognitive scores
- Motor delays: Neurodevelopmental treatment improves gross motor function by 65%
- Language delays: Naturalistic interventions increase vocabulary by 150-200%
- Parent-mediated therapy: Cost-effective with sustained gains
- Peer-mediated interventions: Social communication improvements of 80%
Treatment algorithms guide service intensity and intervention selection based on delay severity and child characteristics. Individualized Family Service Plans (IFSP) coordinate multi-disciplinary approaches with measurable outcomes.
| Delay Severity | Service Intensity | Expected Outcomes | Timeline |
|---|---|---|---|
| Mild (1-1.5 SD) | 5-10 hours/week | 70-80% normalize | 6-12 months |
| Moderate (1.5-2 SD) | 15-25 hours/week | 50-60% significant improvement | 12-18 months |
| Severe (>2 SD) | 25-40 hours/week | 30-40% major gains | 18-24 months |
| Profound (>3 SD) | 40+ hours/week | Functional improvements | Ongoing |
- Family-Centered Intervention Principles
- Parent coaching: Increases intervention dosage by 300-400%
- Sibling involvement: Enhances social skill development by 45%
- Cultural adaptation: Improves engagement and reduces dropout by 60%
- Culturally responsive practices increase family satisfaction to >90%
- Bilingual services: Essential for non-English speaking families
💡 Master This: Intervention success requires systematic progress monitoring using data-driven decision making. Weekly measurements of target behaviors enable rapid adjustments to maximize therapeutic gains within critical windows.
This evidence-based intervention framework optimizes developmental outcomes through systematic, intensive, and family-centered approaches. Understanding intervention principles connects to advanced integration of multi-system developmental processes.
⚡ The Intervention Optimization Engine
🧠 The Neurodevelopmental Integration Network
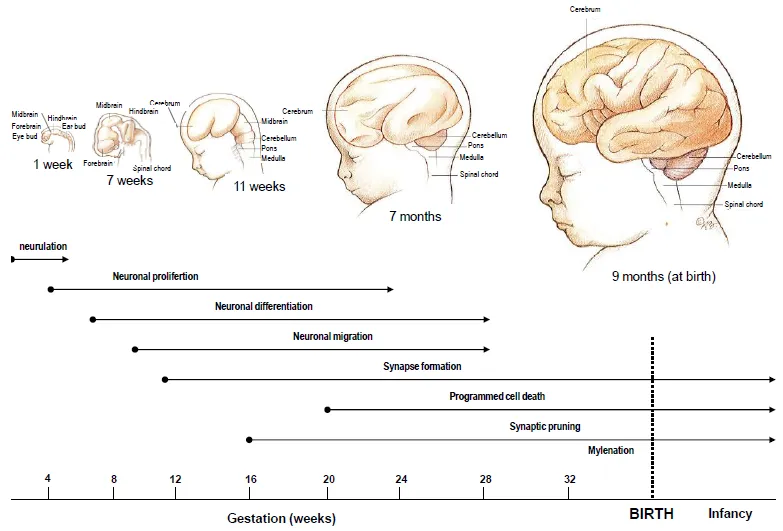
Neurodevelopmental integration occurs through activity-dependent processes where experience literally sculpts brain architecture. Critical periods represent windows when specific experiences are required for normal development, while sensitive periods offer enhanced but not exclusive opportunities for skill acquisition.
📌 Remember: NETWORKS - Neural plasticity peaks, Experience shapes structure, Timing is critical, Windows close gradually, Opportunity costs exist, Rewiring possible, Key periods matter, Systems interact
-
Critical Period Neurobiology
- Visual system: Critical period ends by 8 years (monocular deprivation after 6 months causes permanent deficits)
- Language acquisition: Sensitive period 0-7 years (phoneme discrimination lost by 12 months without exposure)
- Social attachment: Critical period 6-24 months (disruption affects lifelong relationship patterns)
- Synaptic pruning: 40% of synapses eliminated by adolescence
- Myelination: Continues until 25 years in prefrontal cortex
-
Multi-System Developmental Interactions
- Motor-cognitive coupling: Gross motor delays predict executive function deficits (r=0.65)
- Language-social integration: Communication skills correlate with peer relationships (r=0.72)
- Sensory-motor integration: Vestibular function affects spatial cognition (r=0.58)
- Cross-domain interventions show 30% greater efficacy than single-domain approaches
- Embodied cognition: Physical movement enhances abstract thinking by 25%
Developmental systems theory explains how multiple levels of organization (genes, cells, circuits, behaviors, environment) co-evolve through bidirectional influences. This dynamic systems approach reveals why linear cause-effect models fail to predict developmental outcomes.
| System Level | Time Scale | Key Processes | Clinical Implications |
|---|---|---|---|
| Molecular | Milliseconds-hours | Gene expression, protein synthesis | Pharmacological targets |
| Cellular | Hours-days | Neurogenesis, differentiation | Stem cell therapies |
| Circuit | Days-weeks | Synaptogenesis, pruning | Stimulation protocols |
| Behavioral | Weeks-months | Skill acquisition, habits | Intervention timing |
| Environmental | Months-years | Cultural transmission | Family/school programs |
- Cutting-Edge Research Applications
- Neuroplasticity-based interventions: Computerized training programs improve working memory by 40%
- Epigenetic modifications: Environmental enrichment reverses genetic risk for cognitive delays
- Biomarker development: EEG patterns at 6 months predict autism with 81% accuracy
- Precision medicine: Genetic profiles guide individualized intervention selection
- Digital therapeutics: App-based interventions show equivalent efficacy to traditional therapy
💡 Master This: Developmental resilience emerges from multiple protective factors operating across biological, psychological, and social levels. Building resilience requires strengthening these protective networks rather than simply addressing deficits.
This systems-level understanding enables precision approaches to developmental intervention that optimize outcomes through targeted, timing-sensitive strategies. These advanced concepts connect to practical mastery tools for clinical application.
🧠 The Neurodevelopmental Integration Network
🎯 The Clinical Mastery Command Center
Clinical mastery in developmental assessment requires rapid integration of multiple data streams into actionable insights. This expertise develops through deliberate practice with systematic frameworks that transform complex information into clear clinical decisions.
Essential Clinical Arsenal - Critical Numbers for Immediate Reference:
- Red Flag Thresholds
- No social smile by 3 months
- No sitting by 9 months
- No walking by 18 months
- No words by 16 months
- No phrases by 24 months
📌 Remember: MASTER - Milestones have windows, Always screen systematically, Suspect if parental concern, Time-sensitive interventions, Early is everything, Refer when uncertain
| Quick Reference | Normal Range | Concern Threshold | Action Required |
|---|---|---|---|
| Head Control | 2-4 months | >6 months | Neurology referral |
| Pincer Grasp | 9-12 months | >15 months | OT evaluation |
| First Words | 10-14 months | >18 months | Audiology + SLP |
| Independent Walking | 12-15 months | >18 months | PT assessment |
| Toilet Training | 24-36 months | >42 months | Developmental eval |
💡 Master This: The 5-Minute Assessment - Social engagement (30 seconds), gross motor observation (2 minutes), fine motor tasks (1 minute), language sample (1.5 minutes) provides 80% diagnostic accuracy for significant delays.
Clinical Decision Framework for immediate application transforms milestone knowledge into systematic practice excellence, enabling early detection and optimal outcomes through evidence-based developmental surveillance.
🎯 The Clinical Mastery Command Center
Practice Questions: Milestones
Test your understanding with these related questions
A 6-month-old boy is brought to the physician for a well-child examination. The boy was born at term, and the pregnancy was complicated by prolonged labor. There is no family history of any serious illnesses. He can sit upright but needs help to do so and cannot roll over from the prone to the supine position. He can grasp his rattle and can transfer it from one hand to the other. He babbles. He cries if anyone apart from his parents holds him or plays with him. He touches his own reflection in the mirror. Vital signs are within normal limits. He is at the 40th percentile for head circumference, 30th percentile for length, and 40th percentile for weight. Physical examination reveals no abnormalities. Which of the following developmental milestones is delayed in this infant?













