Pathophysiology theories US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pathophysiology theories. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pathophysiology theories US Medical PG Question 1: A 6-year-old boy presents to his pediatrician accompanied by his mother for evaluation of a rash. The rash appeared a little over a week ago, and since that time the boy has felt tired. He is less interested in playing outside, preferring to remain indoors because his knees and stomach hurt. His past medical history is significant for an upper respiratory infection that resolved uneventfully without treatment 2 weeks ago. Temperature is 99.5°F (37.5°C), blood pressure is 115/70 mmHg, pulse is 90/min, and respirations are 18/min. Physical exam shows scattered maroon macules and papules on the lower extremities. The abdomen is diffusely tender to palpation. There is no cervical lymphadenopathy or conjunctival injection. Which of the following will most likely be found in this patient?
- A. Coronary artery aneurysms
- B. Leukocytoclastic vasculitis (Correct Answer)
- C. Thrombocytopenia
- D. Mitral regurgitation
- E. Occult malignancy
Pathophysiology theories Explanation: ***Leukocytoclastic vasculitis***
- This patient presents with symptoms highly suggestive of **Henoch-Schönlein Purpura (HSP)**, including a preceding URI, fatigue, low-grade fever, **abdominal pain**, and a **palpable purpura** primarily on the lower extremities.
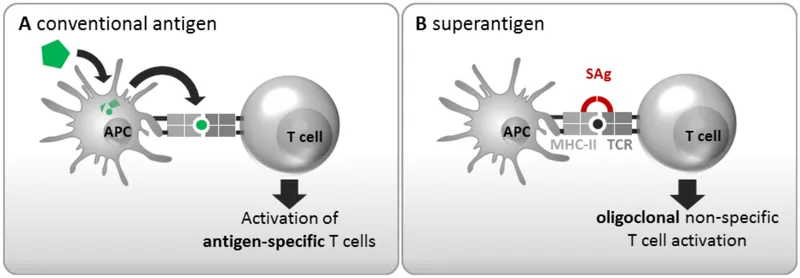
- HSP is characterized by IgA-mediated **small-vessel vasculitis**, which histologically presents as leukocytoclastic vasculitis with IgA deposition on immunofluorescence.
*Coronary artery aneurysms*
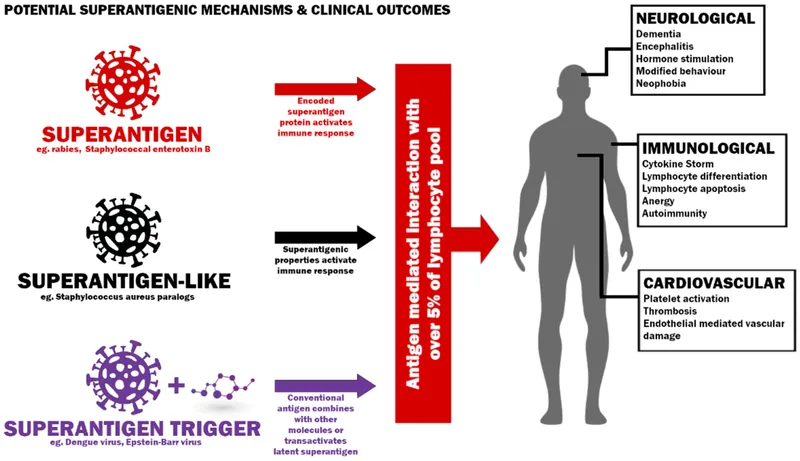
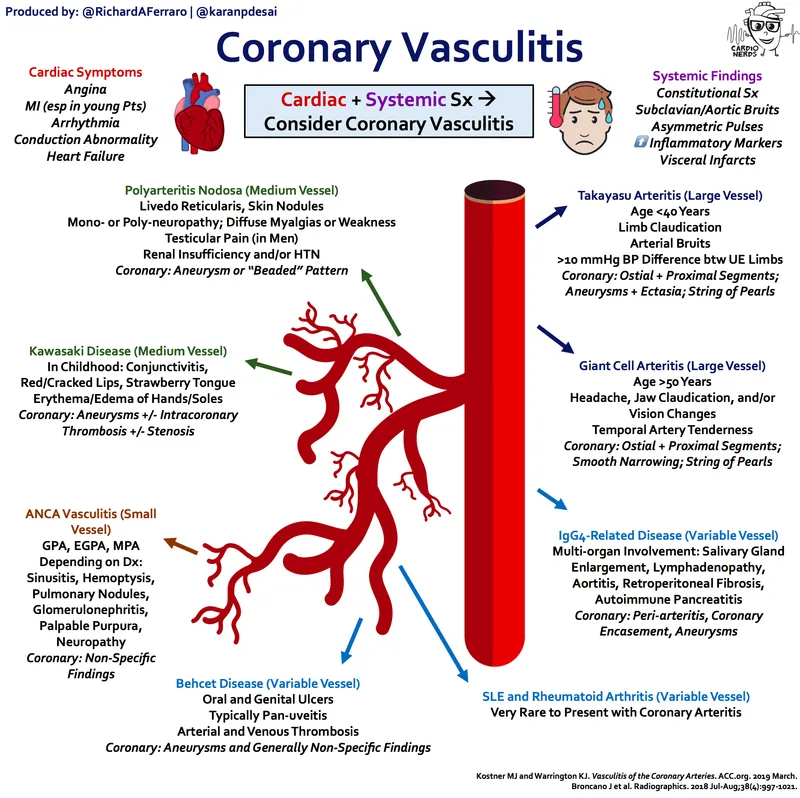
- **Coronary artery aneurysms** are a classic complication of **Kawasaki disease**, not Henoch-Schönlein Purpura.
- Kawasaki disease presents with different clinical features, including prolonged fever, conjunctival injection, oral changes, and cervical lymphadenopathy.
*Thrombocytopenia*
- **Thrombocytopenia** is characterized by a low platelet count and often presents with petechiae, purpura, and bleeding, but the rash in HSP is due to inflammation and extravasation of red blood cells, not low platelets.
- Platelet counts in HSP are typically **normal** or can be slightly elevated as an acute phase reactant.
*Mitral regurgitation*
- **Mitral regurgitation** is a common manifestation of **rheumatic fever**, particularly after recurrent episodes, caused by valvular damage.
- Rheumatic fever is also preceded by infection (Group A Strep) but involves different symptoms like migratory polyarthritis, carditis, chorea, erythema marginatum, and subcutaneous nodules, which are not described here.
*Occult malignancy*
- While an **occult malignancy** can cause paraneoplastic syndromes or constitutional symptoms, the specific constellation of symptoms, including the migratory rash, abdominal pain, and preceding URI, points much more strongly to **HSP** in a 6-year-old.
- The presentation is more consistent with an acute, inflammatory process rather than a chronic, insidious malignant one.
Pathophysiology theories US Medical PG Question 2: A 31-year-old Israeli male with a history of heavy smoking presents to your office with painful ulcerations on his hands and feet. Upon examination, he is found to have hypersensitivity to intradermally injected tobacco extract. Which of the following processes is most likely responsible for his condition?
- A. Eosinophil-rich granulomatous inflammation
- B. Segmental vasculitis of small and medium-sized arteries (Correct Answer)
- C. Increased endothelial permeability
- D. Necrotizing inflammation involving renal arteries
- E. Concentric thickening of the arteriolar wall
Pathophysiology theories Explanation: ***Segmental vasculitis of small and medium-sized arteries***
- This presentation is highly characteristic of **Buerger's disease (thromboangiitis obliterans)**, which is a **segmental, inflammatory vasculitis** primarily affecting small and medium-sized arteries and veins of the hands and feet.
- Key features include **painful ulcerations of the hands and feet**, a strong association with **heavy smoking**, and often occurs in young to middle-aged adult males, with a higher prevalence in certain populations (e.g., of Israeli or Asian descent).
*Eosinophil-rich granulomatous inflammation*
- This type of inflammation is characteristic of conditions like **Churg-Strauss syndrome (eosinophilic granulomatosis with polyangiitis)**.
- Churg-Strauss syndrome typically involves asthma, allergic rhinitis, and eosinophilia, with vasculitis of small to medium vessels, not primarily affecting the distal extremities in this manner or having such a strong tobacco link.
*Increased endothelial permeability*
- While increased endothelial permeability is a feature of general inflammation and can contribute to edema, it is not the primary underlying pathological process causing the **segmental occlusive vasculitis** seen in Buerger's disease.
- This describes a general vascular response rather than a specific disease pathology.
*Necrotizing inflammation involving renal arteries*
- **Necrotizing inflammation of renal arteries** is characteristic of conditions like **polyarteritis nodosa (PAN)** or other systemic vasculitides that can affect renal vessels.
- These conditions typically present with systemic symptoms, hypertension, and renal dysfunction, which are not described in this patient.
*Concentric thickening of the arteriolar wall*
- **Concentric thickening of arteriolar walls** is a hallmark of **hypertensive arteriolosclerosis** or other forms of systemic hypertension.
- This finding would explain chronic end-organ damage from hypertension but does not account for the acute, painful ulcerations in the extremities associated with heavy smoking.
Pathophysiology theories US Medical PG Question 3: A 72-year-old man comes to the physician because of a 6-month history of intermittent dull abdominal pain that radiates to the back. He has smoked one pack of cigarettes daily for 50 years. His blood pressure is 145/80 mm Hg. Abdominal examination shows generalized tenderness and a pulsatile mass in the periumbilical region on deep palpation. Further evaluation of the affected blood vessel is most likely to show which of the following?
- A. Obliterative inflammation of the vasa vasorum
- B. Formation of giant cells in the tunica media
- C. Necrotizing inflammation of the entire vessel wall
- D. Fragmentation of elastic tissue in the tunica media (Correct Answer)
- E. Accumulation of foam cells in the tunica intima
Pathophysiology theories Explanation: ***Fragmentation of elastic tissue in the tunica media***
- This patient's presentation with **intermittent dull abdominal pain radiating to the back**, a **pulsatile periumbilical mass**, and a history of **heavy smoking** is highly suggestive of an **abdominal aortic aneurysm (AAA)**.
- The pathological hallmark of AAA is **degradation and fragmentation of elastic tissue in the tunica media**, caused by chronic inflammation and increased activity of **matrix metalloproteinases (MMPs)**.
- This medial degeneration leads to **weakening of the vessel wall** and progressive **dilation**, ultimately forming an aneurysm.
- While atherosclerosis initiates the process, the actual aneurysm formation is characterized by this elastic tissue destruction in the media.
*Accumulation of foam cells in the tunica intima*
- This describes the **early lesion of atherosclerosis**, which is a **risk factor** for AAA development.
- However, when examining an **established AAA**, the predominant finding is not intimal foam cells but rather **medial degeneration** with elastic tissue fragmentation.
- Atherosclerosis is the underlying cause, but the question asks about findings in the affected vessel (the aneurysm itself).
*Obliterative inflammation of the vasa vasorum*
- This is characteristic of **syphilitic aortitis** (tertiary syphilis), which typically affects the **ascending thoracic aorta**.
- While syphilis can cause aneurysms, the patient's presentation and demographics are more consistent with atherosclerotic AAA.
*Formation of giant cells in the tunica media*
- This finding is associated with **giant cell arteritis** (temporal arteritis), which affects large and medium-sized arteries, particularly the temporal and ophthalmic arteries.
- It presents with headache, jaw claudication, and visual disturbances—features absent in this case.
*Necrotizing inflammation of the entire vessel wall*
- This describes **necrotizing vasculitis** such as **polyarteritis nodosa**, which affects medium-sized muscular arteries.
- While vasculitis can cause aneurysms, the clinical picture of AAA in an elderly smoker with atherosclerotic risk factors points to atherosclerotic pathogenesis, not primary vasculitis.
Pathophysiology theories US Medical PG Question 4: A 50-year-old man comes to the physician for the evaluation of recurrent episodes of chest pain, difficulty breathing, and rapid heart beating over the past two months. During this period, he has had a 4-kg (8.8-lb) weight loss, malaise, pain in both knees, and diffuse muscle pain. Five years ago, he was diagnosed with chronic hepatitis B infection and was started on tenofovir. His temperature is 38°C (100.4°F), pulse is 110/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities except for tachycardia. There are several ulcerations around the ankle and calves bilaterally. Laboratory studies show:
Hemoglobin 11 g/dL
Leukocyte count 14,000/mm3
Erythrocyte sedimentation rate 80 mm/h
Serum
Perinuclear anti-neutrophil cytoplasmic antibodies negative
Hepatitis B surface antigen positive
Urine
Protein +2
RBC 6-7/hpf
Which of the following is the most likely diagnosis?
- A. Granulomatosis with polyangiitis
- B. Giant cell arteritis
- C. Thromboangiitis obliterans
- D. Polyarteritis nodosa (Correct Answer)
- E. Takayasu arteritis
Pathophysiology theories Explanation: ***Polyarteritis nodosa (PAN)***
- This patient presents with **fever**, **weight loss**, **myalgia**, and **arthralgia** along with **skin ulcerations** and **renal involvement** (proteinuria, hematuria), signs of systemic inflammation, and **medium-sized vessel vasculitis**. The history of **chronic Hepatitis B infection** is strongly associated with PAN.
- The elevated **ESR** and **leukocytosis** indicate ongoing inflammation, and the chest pain/rapid heart beating could be signs of cardiac involvement, which is common in PAN. The negative p-ANCA also helps rule out other vasculitides.
*Granulomatosis with polyangiitis*
- This condition is typically associated with **upper and lower respiratory tract involvement**, **glomerulonephritis**, and **c-ANCA positivity** (anti-PR3 antibodies).
- The patient's symptoms do not primarily involve sinusitis, pulmonary nodules, or other upper/lower airway disease, and p-ANCA is negative, rather than c-ANCA positive.
*Giant cell arteritis*
- This is a vasculitis affecting primarily **large-sized arteries**, especially the carotid artery branches, and typically occurs in patients **older than 50 years** (though this patient is 50, other symptoms rule it out).
- Key symptoms include **new-onset headache**, **jaw claudication**, **scalp tenderness**, and potential vision loss, none of which are reported here.
*Thromboangiitis obliterans*
- This condition is strongly linked to **heavy tobacco use** and results in **segmental thrombosis and inflammation of small and medium-sized arteries and veins** in the extremities.
- It primarily causes **ischemia of the digits** (fingers and toes), leading to pain, ulcerations, and gangrene, which is not fully consistent with the patient's widespread systemic symptoms and organ involvement.
*Takayasu arteritis*
- This is a **large-vessel vasculitis** primarily affecting the **aorta and its major branches**, typically seen in **younger women**.
- Symptoms often include **claudication**, **absent or diminished pulses**, and **discrepancies in blood pressure between limbs**, which are not described in this patient.
Pathophysiology theories US Medical PG Question 5: A previously healthy 4-year-old boy is brought to the physician by his parents because he has had a fever, diffuse joint pain, and a rash on his abdomen for the past week. Acetaminophen did not improve his symptoms. He emigrated from China with his family 2 years ago. He attends daycare. His immunization records are not available. His temperature is 38.5°C (101.3°F), pulse is 125/min, and blood pressure is 100/60 mm Hg. Examination shows polymorphous truncal rash. The eyes are pink with no exudate. The tongue is shiny and red, and the lips are cracked. The hands and feet are red and swollen. There is right-sided anterior cervical lymphadenopathy. Which of the following is the most appropriate next step in management?
- A. HHV-6 immunoglobulin M (IgM) detection
- B. ANA measurement
- C. Echocardiography (Correct Answer)
- D. Monospot test
- E. Antistreptolysin O titer measurement
Pathophysiology theories Explanation: ***Echocardiography***
- This patient presents with classic symptoms of **Kawasaki disease**, including protracted fever (>5 days), polymorphous rash, conjunctival injection, cracked lips and red tongue (**strawberry tongue**), swollen hands and feet, and cervical lymphadenopathy.
- The diagnosis can be made clinically when fever ≥5 days plus ≥4 of 5 principal criteria are present, which this patient meets.
- **Echocardiography** is essential to establish a **baseline cardiac assessment** and screen for **coronary artery aneurysms**, which occur in 15-25% of untreated patients.
- Among the diagnostic options listed, echocardiography is the most appropriate next step, though in clinical practice, **treatment with IVIG and high-dose aspirin should be initiated promptly** (ideally within 10 days of fever onset) and should not be delayed pending echocardiography results.
*HHV-6 immunoglobulin M (IgM) detection*
- **Human Herpesvirus 6 (HHV-6)** causes **roseola infantum** (exanthem subitum), which presents with high fever for 3-5 days followed by a rash that appears **as the fever resolves**.
- The mucocutaneous findings in this case (strawberry tongue, cracked lips, conjunctival injection, extremity swelling) are not consistent with roseola.
*ANA measurement*
- **Antinuclear antibody (ANA)** testing screens for **autoimmune diseases** such as systemic lupus erythematosus or juvenile idiopathic arthritis.
- While this patient has fever and joint pain, the specific mucocutaneous changes (strawberry tongue, cracked lips, conjunctival injection, polymorphous rash, extremity edema) and cervical lymphadenopathy are pathognomonic for Kawasaki disease, not typical autoimmune conditions.
*Monospot test*
- The **Monospot test** diagnoses **infectious mononucleosis** caused by **Epstein-Barr virus (EBV)**.
- While EBV can cause fever, rash, and lymphadenopathy (typically posterior cervical), the characteristic mucocutaneous findings of Kawasaki disease (strawberry tongue, cracked lips, conjunctival injection without exudate, extremity changes) are not seen in mononucleosis.
- Additionally, mononucleosis is uncommon in preschool-aged children.
*Antistreptolysin O titer measurement*
- **Antistreptolysin O (ASO) titer** detects recent **Group A Streptococcus** infection and can support a diagnosis of **acute rheumatic fever (ARF)**.
- ARF presents with migratory polyarthritis, carditis, and **erythema marginatum** (not a polymorphous rash), occurring 2-4 weeks after streptococcal pharyngitis.
- The mucocutaneous features in this case are specific to Kawasaki disease and not consistent with ARF.
Pathophysiology theories US Medical PG Question 6: A 48-year-old male presents to his primary physician with the chief complaints of fever, abdominal pain, weight loss, muscle weakness, and numbness in his lower extremities. UA is normal. A biopsy of the sural nerve reveals transmural inflammation and fibrinoid necrosis of small and medium arteries. Chart review reveals a remote history of cigarette smoking as a teenager and Hepatitis B seropositivity. What is the most likely diagnosis?
- A. Raynaud disease
- B. Systemic lupus erythematosus
- C. Microscopic polyangiitis
- D. Thromboangiitis obliterans
- E. Polyarteritis nodosa (Correct Answer)
Pathophysiology theories Explanation: ***Polyarteritis nodosa***
- The constellation of **fever, abdominal pain, weight loss, muscle weakness, and numbness in the lower extremities** (suggesting **neuropathy**) along with **Hepatitis B seropositivity**, is highly indicative of **Polyarteritis nodosa (PAN)**.
- The **sural nerve biopsy findings of transmural inflammation and fibrinoid necrosis of small and medium arteries** are pathognomonic for PAN, confirming a **necrotizing vasculitis** primarily affecting these vessel types.
*Raynaud disease*
- This condition involves **vasospasm of small arteries and arterioles**, typically in the fingers and toes, leading to characteristic color changes.
- It does not present with systemic symptoms like **fever, weight loss, or abdominal pain**, nor does it cause **transmural inflammation or fibrinoid necrosis** of arteries.
*Systemic lupus erythematosus*
- SLE is a multisystem autoimmune disease that can cause a wide range of symptoms, but it is not typically characterized by **necrotizing vasculitis of small and medium arteries** with **fibrinoid necrosis** as seen in the biopsy.
- While it can cause neuropathy, the specific biopsy findings and the strong association with **Hepatitis B** make PAN a more fitting diagnosis.
*Microscopic polyangiitis*
- **Microscopic polyangiitis (MPA)** is a **pauci-immune necrotizing vasculitis** that primarily affects **small vessels** (capillaries, venules, arterioles) and is often associated with **ANCA** (anti-neutrophil cytoplasmic antibodies).
- While it can cause systemic symptoms and neuropathy, the biopsy finding of **transmural inflammation affecting medium arteries** and the strong link to **Hepatitis B** point away from MPA and towards PAN.
*Thromboangiitis obliterans*
- This is a **segmental, thrombosing vasculitis** primarily affecting **small and medium arteries and veins of the extremities**, almost exclusively seen in **smokers**.
- While the patient has a remote history of smoking, the biopsy finding of **transmural inflammation and fibrinoid necrosis** is typical of PAN, not the thrombosing inflammation of Thromboangiitis obliterans.
Pathophysiology theories US Medical PG Question 7: A 32-year-old woman presents with new left-arm pain. She was previously well but for 2 months has had episodes of low-grade fever, night sweats, and dizziness. She works as a stock assistant and has noticed left arm pain when she stocks shelves. She is taking a multivitamin but no other medications. On physical examination, her blood pressure is 126/72 in her right arm, but it cannot be measured in her left arm. The left radial pulse is not detectable. There is a bruit over the left subclavian area. Femoral and pedal pulses are normal and no abdominal bruits are heard. The left hand is cool but has no other evidence of ischemia. Which of the following is the most likely etiology of this patient’s condition?
- A. Raynaud’s phenomenon
- B. Fibromuscular dysplasia
- C. Subclavian steal syndrome
- D. Aortic coarctation
- E. Takayasu arteritis (Correct Answer)
Pathophysiology theories Explanation: ***Takayasu arteritis***
- This **large-vessel vasculitis** predominantly affects **young women** (typically <40 years old) and involves the aorta and its major branches, including the subclavian arteries.
- The patient's **constitutional symptoms** (low-grade fever, night sweats) reflect the systemic inflammatory nature of the disease.
- The **absent left radial pulse**, **unmeasurable left arm blood pressure**, and **subclavian bruit** indicate significant stenosis or occlusion of the left subclavian artery, a hallmark of Takayasu arteritis.
- This arterial stenosis can lead to **subclavian steal syndrome** (a manifestation, not the etiology) and **arm claudication** with exertion (pain when stocking shelves).
- The **normal femoral and pedal pulses** help localize the pathology to the upper extremity vessels.
*Subclavian steal syndrome*
- This is a **hemodynamic phenomenon** (manifestation), not an underlying etiology.
- It occurs when subclavian artery stenosis causes retrograde flow from the vertebral artery to supply the affected arm, which can cause dizziness due to vertebrobasilar insufficiency.
- The underlying **cause** in this young woman with systemic symptoms is most likely Takayasu arteritis.
*Raynaud's phenomenon*
- Characterized by **episodic vasospasm** of digital arteries in response to cold or stress, causing color changes (white-blue-red).
- Does not cause **absent pulses**, **unequal blood pressures between arms**, **bruits**, or **constitutional symptoms**.
*Aortic coarctation*
- A **congenital narrowing of the aorta**, typically just distal to the left subclavian artery origin.
- Would cause **hypertension in both upper extremities** with **diminished lower extremity pulses and blood pressures** (upper-lower discrepancy, not left-right arm discrepancy).
- Does not explain the constitutional symptoms or isolated left arm findings.
*Fibromuscular dysplasia*
- A **noninflammatory arteriopathy** causing abnormal cellular proliferation in arterial walls, most commonly affecting **renal and carotid arteries**.
- Typically occurs in **middle-aged women** without systemic symptoms.
- While it can rarely affect subclavian arteries, the **constitutional symptoms** and pattern of large-vessel involvement strongly favor an inflammatory vasculitis like Takayasu arteritis.
Pathophysiology theories US Medical PG Question 8: A 7-year-old girl is brought to the physician by her mother because of a 2-week history of generalized fatigue, intermittent fever, and progressively worsening shortness of breath. Physical examination shows pallor, jugular venous distention, and nontender cervical and axillary lymphadenopathy. Inspiratory stridor is heard on auscultation of the chest. The liver is palpated 3 cm below the right costal margin. Her hemoglobin concentration is 9.5 g/dL, leukocyte count is 66,000/mm³, and platelet count is 102,000/mm³. An x-ray of the chest shows a mediastinal mass. A bone marrow aspirate predominantly shows leukocytes and presence of 35% lymphoblasts. Which of the following additional findings is most likely in this patient?
- A. t(8;14) translocation
- B. Positive myeloperoxidase staining
- C. Positive CD3/CD7 staining (Correct Answer)
- D. t(9;22) translocation
- E. Reed-Sternberg cells
Pathophysiology theories Explanation: ***Positive CD3/CD7 staining***
- The presence of a **mediastinal mass** with **T-cell lymphoblastic leukemia/lymphoma (T-ALL)** is highly associated with a **T-cell immunophenotype**. **CD3** and **CD7** are **T-cell surface markers**.
- The constellation of findings, including **lymphadenopathy**, **hepatomegaly**, **bone marrow involvement** with 35% lymphoblasts, and a **mediastinal mass** causing **stridor**, is classic for T-ALL, which is typically of T-cell origin.
*t(8;14) translocation*
- This translocation is characteristic of **Burkitt lymphoma**, which typically presents as an **extranodal mass** (e.g., jaw, abdomen) rather than a primary mediastinal mass causing stridor.
- While Burkitt lymphoma is also a B-cell non-Hodgkin lymphoma and can have bone marrow involvement, the clinical picture here is not typical for Burkitt lymphoma.
*Positive myeloperoxidase staining*
- **Myeloperoxidase** is an enzyme found in the granules of **myeloid cells**, and its staining is characteristic of **acute myeloid leukemia (AML)**.
- While the patient has leukocytosis and anemia, the predominance of **lymphoblasts** in the bone marrow aspirate points away from AML.
*t(9;22) translocation*
- The **Philadelphia chromosome**, associated with **t(9;22) translocation**, is highly characteristic of **chronic myeloid leukemia (CML)** and can be seen in a subset of **B-cell acute lymphoblastic leukemia (B-ALL)**.
- However, the clinical presentation with a large mediastinal mass causing stridor is more typical of T-ALL, which is not strongly associated with t(9;22).
*Reed-Sternberg cells*
- **Reed-Sternberg cells** are the hallmark of **Hodgkin lymphoma**.
- While Hodgkin lymphoma can present with **mediastinal mass** and **lymphadenopathy**, it typically affects older children/adolescents or young adults, and the presence of **35% lymphoblasts** in the bone marrow indicates leukemia, not Hodgkin lymphoma.
Pathophysiology theories US Medical PG Question 9: A 3-year-old boy is brought to the physician because of a 3-day history of a pruritic skin rash on his chest. His mother says that he has no history of dermatological problems. He was born at term and has been healthy except for recurrent episodes of otitis media. His immunizations are up-to-date. He appears pale. His temperature is 37°C (98.6°F), pulse is 110/min, respirations are 26/min, and blood pressure is 102/62 mm Hg. Examination shows vesicles and flaccid bullae with thin brown crusts on the chest. Lateral traction of the surrounding skin leads to sloughing. Examination of the oral mucosa shows no abnormalities. Complete blood count is within the reference range. Which of the following is the most likely diagnosis?
- A. Bullous pemphigoid
- B. Dermatitis herpetiformis
- C. Bullous impetigo (Correct Answer)
- D. Pemphigus vulgaris
- E. Stevens-Johnson syndrome
Pathophysiology theories Explanation: ***Bullous impetigo***
- The presence of **flaccid bullae with thin brown crusts** and the positive **Nikolsky's sign** (sloughing with lateral traction), in the absence of mucosal involvement, are classic signs of bullous impetigo, a **Staphylococcus aureus** infection.
- This condition is common in children and can present with localized lesions, as seen on the chest.
*Bullous pemphigoid*
- Typically presents with **tense bullae** in older adults, often with **urticarial plaques**, unlike the flaccid bullae and crusts seen here.
- **Nikolsky's sign is negative** in bullous pemphigoid, which helps distinguish it from bullous impetigo and pemphigus conditions.
*Dermatitis herpetiformis*
- Characterized by intensely **pruritic papules and vesicles** found symmetrically on extensor surfaces, often associated with **celiac disease**.
- The lesions are usually small and grouped, not flaccid bullae with positive Nikolsky's sign.
*Pemphigus vulgaris*
- Presents with **flaccid bullae** and a positive Nikolsky's sign, but characteristically also involves the **oral mucosa**, which is normal in this patient.
- It usually affects older individuals and can be more widespread than the localized rash described.
*Stevens-Johnson syndrome*
- A severe mucocutaneous reaction typically characterized by **widespread epidermal necrosis**, **target lesions**, and often involves **mucous membranes** (oral, ocular, genital) extensively.
- This patient's localized rash without mucosal involvement, target lesions, or systemic toxicity does not fit the criteria for SJS.
Pathophysiology theories US Medical PG Question 10: A 10-year-old girl with a rash is brought to the clinic by her mother. The patient’s mother says that the onset of the rash occurred 2 days ago. The rash was itchy, red, and initially localized to the cheeks with circumoral pallor, and it gradually spread to the arms and trunk. The patient’s mother also says her daughter had been reporting a high fever of 39.4°C (102.9°F), headaches, myalgia, and flu-like symptoms about a week ago, which resolved in 2 days with acetaminophen. The patient has no significant past medical history. Her vital signs include: temperature 37.0°C (98.6°F), pulse 90/min, blood pressure 125/85 mm Hg, respiratory rate 20/min. Physical examination shows a symmetric erythematous maculopapular rash on both cheeks with circumoral pallor, which extends to the patient’s trunk, arms, and buttocks. The remainder of the exam is unremarkable. Laboratory findings are significant for a leukocyte count of 7,100/mm3 and platelet count of 325,000/mm3. Which of the following is the next best step in the management of this patient?
- A. Administer intravenous immunoglobulin (IVIG)
- B. Discharge home, saying that the patient may return to school after the disappearance of the rash
- C. Transfuse with whole blood
- D. Discharge home with instructions for strict isolation from pregnant women until disappearance of the rash
- E. Discharge home, saying that the patient may immediately return to school (Correct Answer)
Pathophysiology theories Explanation: ***Discharge home, saying that the patient may immediately return to school***
- This patient likely has **Fifth Disease (Erythema Infectiosum)**, caused by **Parvovirus B19**, characterized by a **"slapped cheek" rash** and a **lacy, reticular rash** on the trunk and extremities.
- Patients with Fifth Disease are **contagious before the rash appears** and are generally **no longer contagious once the rash develops**, making immediate return to school safe.
*Administer intravenous immunoglobulin (IVIG)*
- **IVIG** is typically reserved for **severe cases of Parvovirus B19 infection** in immunocompromised individuals or those with chronic hemolytic anemias who develop **aplastic crisis**.
- The patient's symptoms are mild and self-limiting, without evidence of severe complications like aplastic anemia (normal leukocyte and platelet counts).
*Discharge home, saying that the patient may return to school after the disappearance of the rash*
- This advice is incorrect because the patient is **no longer contagious once the rash erupts**.
- Requiring isolation until the rash disappears would be unnecessarily disruptive and is not medically indicated for Fifth Disease.
*Transfuse with whole blood*
- **Whole blood transfusion** is not indicated for uncomplicated Fifth Disease, as it can cause significant complications.
- Transfusions are considered only in cases of **severe aplastic crisis** with significant anemia, which is not present in this patient (normal complete blood count).
*Discharge home with instructions for strict isolation from pregnant women until disappearance of the rash*
- While exposure to **Parvovirus B19 in pregnant women** can lead to significant fetal complications (e.g., hydrops fetalis), the patient is **no longer infectious once the rash appears**.
- Therefore, strict isolation from pregnant women **after rash onset** is not necessary, as the risk of transmission has passed.
More Pathophysiology theories US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.