Long-term outcomes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Long-term outcomes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Long-term outcomes US Medical PG Question 1: A 24-year-old man presents with a complaint of breathlessness while jogging. He says that he recently started marathon training. He does not have any family history of asthma nor has any allergies. He currently takes no medication. The blood pressure is 120/80 mm Hg, and the heart rate is 67/min. With each heartbeat, he experiences pounding in his chest, and his head bobs. On physical examination, he has long fingers, funnel chest, and disproportionate body proportions with a decreased upper-to-lower segment ratio. On auscultation over the 2nd right intercostal space, an early diastolic murmur is heard, and 3rd and 4th heart sounds are heard. Echocardiography shows aortic root dilatation. The patient is scheduled for surgery. Which of the following is associated with this patient's condition?
- A. Klinefelter syndrome
- B. Intravenous drug abuse
- C. Marfan's Syndrome (Correct Answer)
- D. Kawasaki syndrome
- E. Gonorrhea
Long-term outcomes Explanation: ***Marfan's Syndrome***
- The patient presents with **tall stature**, **long fingers (arachnodactyly)**, **funnel chest (pectus excavatum)**, and **aortic root dilation** with **aortic regurgitation** (early diastolic murmur, head bobbing, pounding in the chest), all classic features of Marfan syndrome.
- This is a **connective tissue disorder** caused by a mutation in the **FBN1 gene**, leading to defective **fibrillin-1**, which is crucial for structural integrity in the heart, blood vessels, eyes, and skeleton.
*Klinefelter syndrome*
- Characterized by a **47, XXY karyotype** and typically presents with infertility, small testes, gynecomastia, and tall stature, but not the specific cardiovascular or skeletal features described.
- While it can cause tall stature, it does not explain the **arachnodactyly**, **pectus excavatum**, or the severe **aortic root dilation** and regurgitation.
*Intravenous drug abuse*
- Primarily associated with **infective endocarditis**, particularly affecting the **tricuspid valve**, leading to heart murmurs related to infection, not the skeletal and aortic root abnormalities seen here.
- This history would lead to a different clinical presentation, potentially involving fever, chills, and vegetations on valve leaflets, none of which are mentioned.
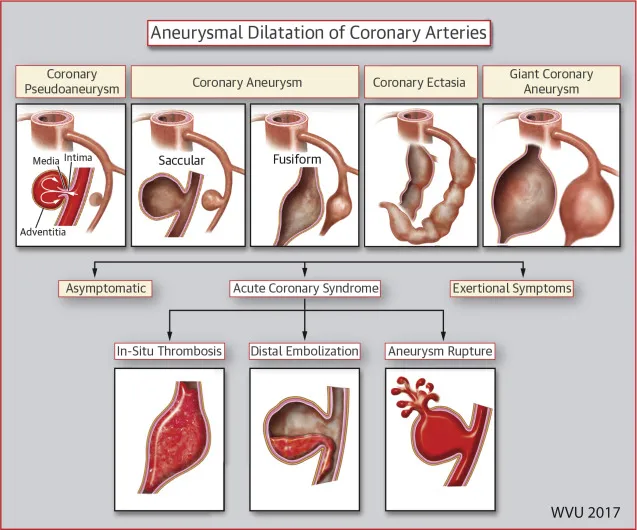
*Kawasaki syndrome*
- An **acute inflammatory vasculitis** primarily affecting young children, characterized by fever, rash, conjunctivitis, lymphadenopathy, and oral mucosal changes.
- While it can cause **coronary artery aneurysms**, it does not explain the skeletal abnormalities or the specific presentation of aortic root dilation with regurgitation in an adult.
*Gonorrhea*
- A **sexually transmitted infection** that can lead to disseminated gonococcal infection, causing arthritis, tenosynovitis, and dermatitis.
- It does not cause the specific skeletal abnormalities or the primary cardiac pathology of aortic root dilation and regurgitation described in this patient.
Long-term outcomes US Medical PG Question 2: A 71-year-old woman comes to the physician because of sudden loss of vision in her right eye for 15 minutes that morning, which subsided spontaneously. Over the past 4 months, she has had fatigue, a 4-kg (8.8-lb) weight loss, and has woken up on several occasions at night covered in sweat. She has had frequent headaches and pain in her jaw while chewing for the past 2 months. She does not smoke or drink alcohol. Her temperature is 37.5°C (99.5°F), pulse is 88/min, and blood pressure is 118/78 mm Hg. Examination shows a visual acuity of 20/25 in the left eye and 20/30 in the right eye. The pupils are equal and reactive. There is no swelling of the optic discs. Her hemoglobin concentration is 10.5 g/dL, platelet count is 420,000/mm3, and erythrocyte sedimentation rate is 69 mm/h. The patient's condition puts her at the greatest risk of developing which of the following complications?
- A. Pulmonary artery hypertension
- B. Rapidly progressive glomerulonephritis
- C. Thoracic aortic aneurysm (Correct Answer)
- D. Internal carotid artery stenosis
- E. Myocardial infarction
Long-term outcomes Explanation: ***Thoracic aortic aneurysm***
- This patient presents with symptoms highly suggestive of **giant cell arteritis (GCA)**, including sudden, transient vision loss (amaurosis fugax), jaw claudication, headaches, fatigue, weight loss, night sweats, and an elevated ESR. GCA is a **large-vessel vasculitis** that can affect the aorta.
- **Aortic aneurysm and dissection** are serious long-term complications of GCA, affecting up to 15-30% of patients, with the thoracic aorta being particularly vulnerable.
*Pulmonary artery hypertension*
- While systemic inflammatory conditions can sometimes be associated with secondary pulmonary hypertension, it is **not a direct or common complication** of giant cell arteritis.
- Pulmonary artery hypertension is more typically associated with conditions like **scleroderma**, chronic thromboembolic disease, or left heart failure.
*Rapidly progressive glomerulonephritis*
- This condition is characterized by a rapid decline in renal function and is typically seen in **ANCA-associated vasculitides** (e.g., granulomatosis with polyangiitis, microscopic polyangiitis) or anti-GBM disease.
- While GCA is a vasculitis, it primarily affects **large and medium-sized arteries** and does not typically cause rapidly progressive glomerulonephritis.
*Internal carotid artery stenosis*
- While GCA can affect the **carotid arteries**, leading to symptoms like amaurosis fugax due to involvement of the ophthalmic artery (a branch of the internal carotid), it primarily causes **vasculitic inflammation** rather than typical atherosclerotic stenosis which is its own distinct complication.
- The risk of an aneurysm in a large vessel like the aorta is a more distinct and severe systemic complication in this context than focal stenosis of the internal carotid due to the vasculitic process itself.
*Myocardial infarction*
- GCA can increase the risk of cardiovascular events due to sustained inflammation and potential accelerated atherosclerosis, but **myocardial infarction** is not the *greatest risk* or a direct, typical complication of the vasculitic process itself in the way an aortic aneurysm is.
- The primary target of inflammation in GCA is the arterial wall, which directly predisposes to conditions like aneurysm and dissection, especially in the aorta.
Long-term outcomes US Medical PG Question 3: A primary care physician who focuses on treating elderly patients is researching recommendations for secondary prevention. She is particularly interested in recommendations regarding aspirin, as she has several patients who ask her if they should take it. Of the following, which patient should be started on lifelong aspirin as monotherapy for secondary prevention of atherosclerotic cardiovascular disease?
- A. An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits
- B. A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago
- C. A 67-year-old female who has diabetes mellitus and atrial fibrillation
- D. A 45-year-old female with no health problems
- E. A 63-year-old male with a history of a transient ischemic attack (Correct Answer)
Long-term outcomes Explanation: **A 63-year-old male with a history of a transient ischemic attack**
- A patient with a history of **Transient Ischemic Attack (TIA)** has a high risk of subsequent stroke and should be on **lifelong aspirin monotherapy** for secondary prevention of **atherosclerotic cardiovascular disease (ASCVD)**.
- Aspirin helps prevent further thrombotic events by inhibiting platelet aggregation, making it a cornerstone for secondary prevention after TIA or ischemic stroke.
*An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits*
- Aspirin is generally **contraindicated** in patients with a history of **hemorrhagic stroke** due to the increased risk of recurrent bleeding.
- In such cases, the risks of aspirin therapy typically **outweigh the benefits** for cardiovascular prevention.
*A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago*
- A patient with a recently placed **drug-eluting stent (DES)** requires **dual antiplatelet therapy (DAPT)**, typically aspirin plus a P2Y12 inhibitor, for a specific duration (e.g., 6-12 months), not aspirin monotherapy.
- Monotherapy with aspirin alone would be **insufficient** to prevent stent thrombosis in the immediate post-stenting period.
*A 67-year-old female who has diabetes mellitus and atrial fibrillation*
- This patient has two significant risk factors requiring specific management: **diabetes mellitus** for cardiovascular risk and **atrial fibrillation** for stroke risk.
- For atrial fibrillation, **anticoagulation with warfarin or a direct oral anticoagulant (DOAC)** is typically indicated, which makes aspirin monotherapy either unnecessary or potentially harmful if used alone.
*A 45-year-old female with no health problems*
- There is no indication for **aspirin primary prevention** in this patient, especially given the increased risk of bleeding without a clear cardiovascular benefit.
- Guidelines currently recommend against routine aspirin use for primary prevention in healthy individuals due to the **unfavorable risk-benefit ratio**.
Long-term outcomes US Medical PG Question 4: A 73-year-old man presents to the outpatient clinic complaining of chest pain with exertion. He states that resting for a few minutes usually resolves the chest pain. Currently, he takes 81 mg of aspirin daily. He has a blood pressure of 127/85 mm Hg and heart rate of 75/min. Physical examination reveals regular heart sounds and clear lung sounds bilateral. Which medication regimen below should be added?
- A. Metoprolol and a statin daily. Sublingual nitroglycerin as needed. (Correct Answer)
- B. Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.
- C. Amlodipine and a statin daily. Sublingual nitroglycerin as needed.
- D. Amlodipine daily. Sublingual nitroglycerin as needed.
- E. Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.
Long-term outcomes Explanation: ***Metoprolol and a statin daily. Sublingual nitroglycerin as needed.***
- This patient presents with symptoms consistent with **stable angina** (**chest pain with exertion, relieved by rest**). The recommended medical therapy includes **antiplatelet agents** (aspirin, already prescribed), **beta-blockers** (metoprolol) for symptom control and improved survival post-MI, and **high-intensity statins** for lipid management and plaque stabilization. **Sublingual nitroglycerin** is crucial for acute symptom relief.
- Beta-blockers like metoprolol decrease myocardial **oxygen demand** by reducing heart rate and contractility, effectively treating angina. Statins are essential for **atherosclerosis management**.
*Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.*
- While clopidogrel is an **antiplatelet agent**, aspirin is typically the first-line choice for stable angina unless there's an intolerance or compelling reason for dual antiplatelet therapy (e.g., recent stent placement), which is not indicated here.
- Amlodipine, a **calcium channel blocker**, can be used for angina but is usually a second-line agent if beta-blockers are contraindicated or insufficient; it doesn't offer the mortality benefit seen with beta-blockers post-MI.
*Amlodipine and a statin daily. Sublingual nitroglycerin as needed.*
- This regimen includes a **statin** and sublingual nitroglycerin, which are appropriate. However, it uses amlodipine instead of a beta-blocker, which is generally the preferred initial therapy for angina due to its benefits in reducing myocardial oxygen demand and improving outcomes, especially in patients with a history of MI or heart failure.
- Beta-blockers provide superior **mortality reduction benefits** in patients with coronary artery disease compared to calcium channel blockers.
*Amlodipine daily. Sublingual nitroglycerin as needed.*
- This option misses two critical components of comprehensive treatment for stable angina: a **statin** for lipid management and plaque stabilization, and a **beta-blocker** for primary symptom control and long-term cardiac protection.
- Relying solely on amlodipine and sublingual nitroglycerin would leave the patient incompletely treated for their underlying **coronary artery disease**.
*Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.*
- This option lacks a **statin**, which is a cornerstone of therapy for stable angina to manage atherosclerosis.
- While metoprolol is appropriate and ranolazine can be used as an add-on therapy for refractory angina, it's not typically a first-line agent and doesn't replace the need for a statin.
Long-term outcomes US Medical PG Question 5: A 2-month-old girl is brought to the physician for a well-child examination. She was born at 32 weeks' gestation and weighed 1616 g (3 lb 9 oz); she currently weighs 2466 g (5 lb 7 oz). She is exclusively breastfed and receives vitamin D supplementation. Physical examination shows no abnormalities apart from low height and weight. This patient is at increased risk for which of the following complications?
- A. Iron deficiency anemia (Correct Answer)
- B. Hemorrhage
- C. Scurvy
- D. Subacute combined degeneration
- E. Intussusception
Long-term outcomes Explanation: ***Iron deficiency anemia***
- Preterm infants have **lower iron stores** at birth due to reduced placental transfer in the third trimester.
- Their rapid growth rate and exclusive breastfeeding (breast milk has low iron content) further increase their risk of **iron deficiency anemia**.
*Hemorrhage*
- While preterm infants are at higher risk for certain hemorrhages (e.g., intraventricular hemorrhage), this typically occurs in the **immediate neonatal period** and risk significantly decreases by 2 months of age.
- Hemorrhage is not a common long-term complication unique to a 2-month-old preterm infant without additional risk factors.
*Scurvy*
- Scurvy is caused by **vitamin C deficiency**, which is typically not a concern in breastfed infants as breast milk provides adequate vitamin C.
- The primary deficiency risk addressed by supplementation in breastfed infants is vitamin D, not vitamin C.
*Subacute combined degeneration*
- This condition is caused by **vitamin B12 deficiency**, leading to demyelination of the spinal cord.
- While possible in infants of vegan mothers, it is unlikely in a breastfed infant without specific dietary restrictions in the mother.
*Intussusception*
- Intussusception is a condition where one segment of the intestine telescopes into another, usually occurring between **3 months and 3 years of age**.
- It is not specifically linked to prematurity or low birth weight as an increased long-term risk.
Long-term outcomes US Medical PG Question 6: A 3-year-old male presents with his parents to a pediatrician for a new patient visit. The child was recently adopted and little is known about his prior medical or family history. The parents report that the child seems to be doing well, but they are concerned because the patient is much larger than any of the other 3-year-olds in his preschool class. They report that he eats a varied diet at home, and that they limit juice and snack foods. On physical exam, the patient is in the 73rd percentile for weight, 99th percentile for height, and 86th percentile for head circumference. He appears mildly developmentally delayed. He has a fair complexion and tall stature with a prominent sternum. The patient also has joint hypermobility and hyperelastic skin. He appears to have poor visual acuity and is referred to an ophthalmologist, who diagnoses upward lens subluxation of the right eye.
This child is most likely to develop which of the following complications?
- A. Osteoarthritis
- B. Wilms tumor
- C. Medullary thyroid cancer
- D. Aortic dissection (Correct Answer)
- E. Thromboembolic stroke
Long-term outcomes Explanation: ***Aortic dissection***
- The constellation of **tall stature**, **prominent sternum**, **joint hypermobility**, **hyperelastic skin**, and **upward lens subluxation (ectopia lentis)** in a young child strongly suggests **Marfan syndrome**.
- **Aortic root dilation** and subsequent **aortic dissection** are the most serious cardiovascular complications in Marfan syndrome due to weakened connective tissue in the aortic wall caused by **fibrillin-1 deficiency**.
- This is the **leading cause of mortality** in untreated Marfan syndrome.
*Osteoarthritis*
- While joint hypermobility can contribute to **joint instability** and accelerate degenerative changes, typical **osteoarthritis** is less common as a primary, severe complication in childhood Marfan syndrome.
- Early-onset, severe osteoarthritis is not the major life-threatening complication associated with Marfan syndrome at this age.
*Wilms tumor*
- **Wilms tumor** is a type of kidney cancer typically associated with syndromes like **WAGR (Wilms tumor, Aniridia, Genitourinary anomalies, intellectual disability)** or **Beckwith-Wiedemann syndrome**, none of which fit the patient's presentation.
- There is no known direct association between Wilms tumor and Marfan syndrome.
*Medullary thyroid cancer*
- **Medullary thyroid cancer** is a feature of **Multiple Endocrine Neoplasia type 2 (MEN 2) syndromes**, which also present with pheochromocytomas and parathyroid hyperplasia.
- The clinical features described in the patient are not consistent with MEN 2.
*Thromboembolic stroke*
- While Marfan syndrome can lead to cardiovascular issues, a **thromboembolic stroke** is not a primary or characteristic complication, especially in comparison to the high risk of aortic dissection.
- The main vascular pathology in Marfan is related to connective tissue weakness, not primarily hypercoagulability or mural thrombi leading to stroke.
- Thromboembolic complications are more characteristic of **homocystinuria**, which presents with **downward** lens subluxation.
Long-term outcomes US Medical PG Question 7: A 4-year-old boy is brought to the physician by his parents because of fever and mild abdominal pain for 7 days. His parents report that he developed a rash 2 days ago. He has had no diarrhea or vomiting. Four weeks ago, he returned from a camping trip to Colorado with his family. His immunization records are unavailable. His temperature is 39.4°C (102.9°F), pulse is 111/min, respirations are 27/min, and blood pressure is 96/65 mm Hg. Examination shows bilateral conjunctival injections and fissures on his lower lips. The pharynx is erythematous. There is tender cervical lymphadenopathy. The hands and feet appear edematous. A macular morbilliform rash is present over the trunk. Bilateral knee joints are swollen and tender; range of motion is limited by pain. Which of the following is the most appropriate treatment for this patient's condition?
- A. Supportive treatment only
- B. Intravenous immunoglobulin (Correct Answer)
- C. Oral ibuprofen
- D. Oral penicillin
- E. Oral doxycycline
Long-term outcomes Explanation: ***Intravenous immunoglobulin***
- This patient presents with symptoms highly suggestive of **Kawasaki disease**, including a persistent fever for over 5 days, **bilateral conjunctival injection**, **lip fissures**, **erythematous pharynx**, **cervical lymphadenopathy**, and **edema of hands and feet** followed by a rash.
- **IV immunoglobulin (IVIG)** is the cornerstone of treatment for Kawasaki disease, significantly reducing the risk of **coronary artery aneurysms** if given early in the disease course.
*Supportive treatment only*
- While supportive care (fever reduction, hydration) is important, relying solely on it for **Kawasaki disease** would increase the risk of severe complications, particularly **coronary artery involvement**.
- **Kawasaki disease** is a systemic vasculitis requiring specific immunomodulatory therapy to prevent long-term cardiac sequelae.
*Oral ibuprofen*
- **Ibuprofen**, a non-steroidal anti-inflammatory drug (**NSAID**), can help manage fever and joint pain, but it does not address the underlying **vasculitis** or prevent the cardiac complications of **Kawasaki disease**.
- **Aspirin** (high-dose initially, then low-dose) is part of Kawasaki disease treatment, but ibuprofen alone is insufficient as primary therapy.
*Oral penicillin*
- **Penicillin** is an antibiotic used to treat bacterial infections, such as **streptococcal pharyngitis**.
- This patient's symptoms are inconsistent with a typical bacterial infection requiring penicillin and are more indicative of a **systemic inflammatory condition** like Kawasaki disease, which is not bacterial.
*Oral doxycycline*
- **Doxycycline** is an antibiotic often used for **rickettsial infections** (e.g., Rocky Mountain spotted fever) or Lyme disease, which might be considered given the camping trip.
- However, the classic constellation of symptoms (conjunctival injection, lip changes, edema of extremities, diffuse rash) points strongly away from these and towards **Kawasaki disease**, for which doxycycline is ineffective.
Long-term outcomes US Medical PG Question 8: A 4-year-old boy is brought to a pediatrician by his parents with a history of fever for the last 5 days and irritability, decreased appetite, vomiting, and swelling of the hands and feet for the last 3 days. The patient’s mother mentions that he has been taking antibiotics and antipyretics prescribed by another physician for the last 3 days, but there has been no improvement His temperature is 39.4°C (103.0°F), pulse is 128/min, respiratory rate is 24/min, and blood pressure is 96/64 mm Hg. On physical examination, there is significant edema of the hands and feet bilaterally. There is a 2.5 cm diameter freely moveable, nontender cervical lymph node is palpable on the right side. A strawberry tongue and perianal erythema are noted. Conjunctival injection is present bilaterally. Laboratory findings reveal mild anemia and a leukocytosis with a left-shift. Erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) are increased. If not treated appropriately, this patient is at increased risk of developing which of the following complications?
- A. Lower gastrointestinal hemorrhage
- B. Coronary artery ectasia (Correct Answer)
- C. Acute renal failure
- D. Pulmonary embolism
- E. Acute disseminated encephalomyelitis (ADEM)
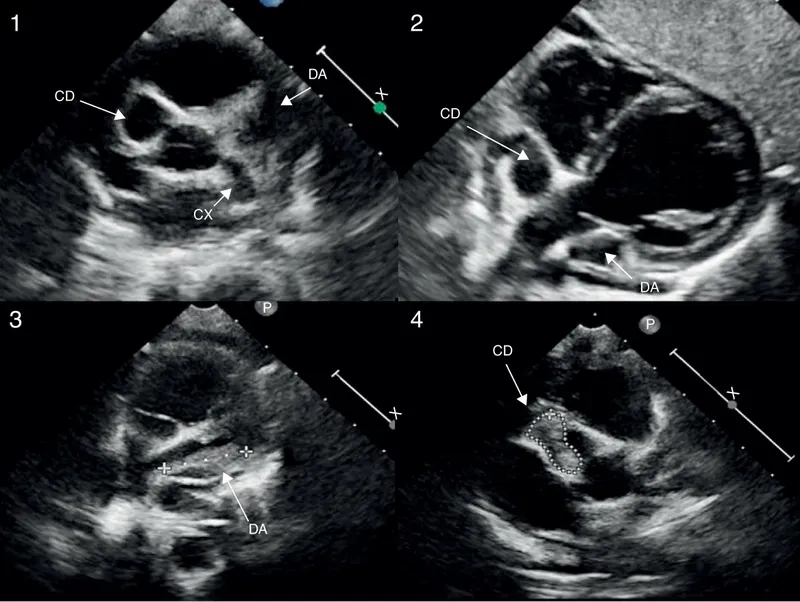
Long-term outcomes Explanation: ***Coronary artery ectasia***
- The patient's symptoms, including **prolonged fever**, **conjunctival injection**, **strawberry tongue**, **cervical lymphadenopathy**, **edema of hands and feet**, and **perianal erythema**, are characteristic of **Kawasaki disease**.
- If left untreated, **Kawasaki disease** can lead to significant cardiovascular complications, most notably **coronary artery aneurysms** or ectasia, due to vasculitis of medium-sized arteries.
*Lower gastrointestinal hemorrhage*
- While **gastrointestinal symptoms** such as vomiting and diarrhea can occur in **Kawasaki disease**, severe complications like **lower gastrointestinal hemorrhage** are rare and not the most common or critical untreated complication.
- Other conditions, like **Meckel's diverticulum** or **inflammatory bowel disease**, are more typically associated with lower GI hemorrhage in children.
*Acute renal failure*
- **Renal involvement** in **Kawasaki disease** is uncommon and usually presents as **mild proteinuria** or **sterile pyuria**; **acute renal failure** is an extremely rare complication.
- Significant renal dysfunction is more commonly seen in conditions like **hemolytic-uremic syndrome** or severe dehydration.
*Pulmonary embolism*
- **Pulmonary embolism** is rare in young children and not a typical complication of untreated **Kawasaki disease**.
- It is more commonly associated with conditions causing **hypercoagulability** or prolonged immobility.
*Acute disseminated encephalomyelitis (ADEM)*
- **ADEM** is an **immune-mediated demyelinating disorder** of the central nervous system that typically follows an infection or vaccination.
- It is not a recognized complication of untreated **Kawasaki disease**, whose primary pathology involves systemic vasculitis.
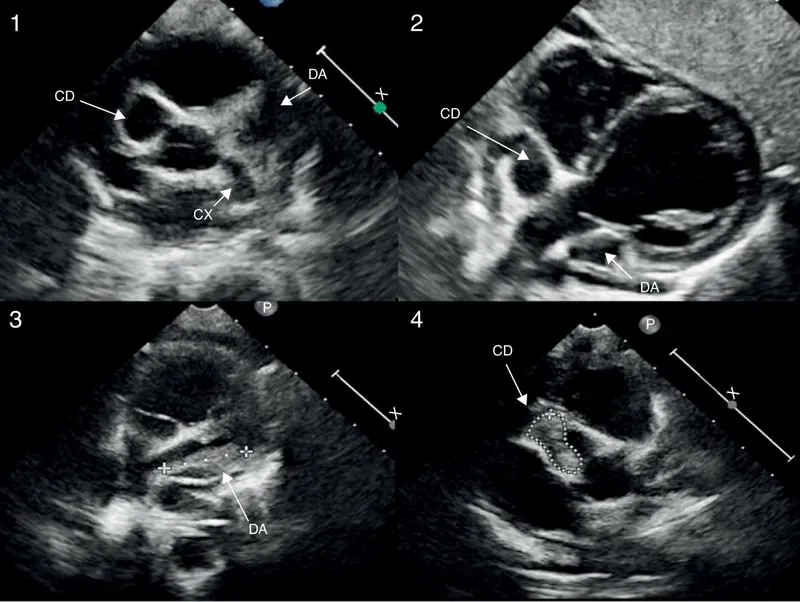
Long-term outcomes US Medical PG Question 9: A 5-year-old girl presents with a rash and a persistent fever of 41.0°C (105.8°F), not relieved by Tylenol. The patient's mother says that her symptoms started 5 days ago and have not improved. The rash started on her trunk and now is present everywhere including the palms and soles. Her birth history is normal. Her pulse is 120/min and respiratory rate is 22/min. On physical examination, the patient is agitated and ill-appearing. There is significant swelling of the distal upper and lower extremities bilaterally. The pharynx is hyperemic (see image). Generalized edema with palpable cervical lymphadenopathy is noted. Muscle tone is normal. Remainder of exam is unremarkable. Laboratory findings are significant for the following:
Laboratory test
Hb 9 g/dL
RBC 3.3/mm3
Neutrophilic leukocytosis 28,000/mm3
Normal platelet count 200,000/mm3
Serum ɣ-GT increased
Hyperbilirubinemia 2.98 mg/dL
AST and ALT are normal, but there is markedly increased serum CRP. Which of the following is the most likely diagnosis in this patient?
- A. Juvenile rheumatoid arthritis
- B. Scarlet fever
- C. Adenovirus infection
- D. Staphylococcal scalded skin syndrome
- E. Kawasaki disease (Correct Answer)
Long-term outcomes Explanation: ***Kawasaki disease***
- The constellation of **prolonged fever, rash (including palms and soles), swollen extremities, hyperemic pharynx, and cervical lymphadenopathy** in a young child is highly suggestive of **Kawasaki disease**.
- Laboratory findings such as **neutrophilic leukocytosis, elevated CRP, and increased γ-GT** further support this diagnosis, which is a **vasculitis** of medium-sized arteries.
*Juvenile rheumatoid arthritis*
- While juvenile rheumatoid arthritis (JRA) can cause **fever and joint swelling**, it typically does not present with the specific rash distribution, **hyperemic pharynx**, or **cervical lymphadenopathy** seen in this patient.
- The **acute onset and severity** of systemic symptoms are more characteristic of Kawasaki disease than typical JRA.
*Scarlet fever*
- Scarlet fever is caused by *Streptococcus pyogenes* and presents with a characteristic **sandpaper-like rash**, **strawberry tongue**, and **fever**.
- It does not typically cause **swelling of the extremities** or the specific laboratory abnormalities like **increased γ-GT** as seen here, and the rash of Kawasaki disease is often polymorphous rather than sandpaper-like.
*Adenovirus infection*
- Adenovirus infections can cause **fever, pharyngitis, and conjunctivitis**, but they do not typically lead to the characteristic widespread rash (including palms and soles), marked **extremity swelling**, or significantly elevated inflammatory markers observed in this case.
- The clinical picture presented is much more severe and specific for a systemic inflammatory condition.
*Staphylococcal scalded skin syndrome*
- **Staphylococcal scalded skin syndrome (SSSS)** is characterized by **erythema and superficial blistering/peeling of the skin**, giving a "scalded" appearance, often starting around the mouth.
- It does not typically cause the **hyperemic pharynx, swollen extremities, or cervical lymphadenopathy** described, and the rash in this patient is not described as blistering or peeling.
Long-term outcomes US Medical PG Question 10: A previously healthy 4-year-old boy is brought to the physician by his parents because he has had a fever, diffuse joint pain, and a rash on his abdomen for the past week. Acetaminophen did not improve his symptoms. He emigrated from China with his family 2 years ago. He attends daycare. His immunization records are not available. His temperature is 38.5°C (101.3°F), pulse is 125/min, and blood pressure is 100/60 mm Hg. Examination shows polymorphous truncal rash. The eyes are pink with no exudate. The tongue is shiny and red, and the lips are cracked. The hands and feet are red and swollen. There is right-sided anterior cervical lymphadenopathy. Which of the following is the most appropriate next step in management?
- A. HHV-6 immunoglobulin M (IgM) detection
- B. ANA measurement
- C. Echocardiography (Correct Answer)
- D. Monospot test
- E. Antistreptolysin O titer measurement
Long-term outcomes Explanation: ***Echocardiography***
- This patient presents with classic symptoms of **Kawasaki disease**, including protracted fever (>5 days), polymorphous rash, conjunctival injection, cracked lips and red tongue (**strawberry tongue**), swollen hands and feet, and cervical lymphadenopathy.
- The diagnosis can be made clinically when fever ≥5 days plus ≥4 of 5 principal criteria are present, which this patient meets.
- **Echocardiography** is essential to establish a **baseline cardiac assessment** and screen for **coronary artery aneurysms**, which occur in 15-25% of untreated patients.
- Among the diagnostic options listed, echocardiography is the most appropriate next step, though in clinical practice, **treatment with IVIG and high-dose aspirin should be initiated promptly** (ideally within 10 days of fever onset) and should not be delayed pending echocardiography results.
*HHV-6 immunoglobulin M (IgM) detection*
- **Human Herpesvirus 6 (HHV-6)** causes **roseola infantum** (exanthem subitum), which presents with high fever for 3-5 days followed by a rash that appears **as the fever resolves**.
- The mucocutaneous findings in this case (strawberry tongue, cracked lips, conjunctival injection, extremity swelling) are not consistent with roseola.
*ANA measurement*
- **Antinuclear antibody (ANA)** testing screens for **autoimmune diseases** such as systemic lupus erythematosus or juvenile idiopathic arthritis.
- While this patient has fever and joint pain, the specific mucocutaneous changes (strawberry tongue, cracked lips, conjunctival injection, polymorphous rash, extremity edema) and cervical lymphadenopathy are pathognomonic for Kawasaki disease, not typical autoimmune conditions.
*Monospot test*
- The **Monospot test** diagnoses **infectious mononucleosis** caused by **Epstein-Barr virus (EBV)**.
- While EBV can cause fever, rash, and lymphadenopathy (typically posterior cervical), the characteristic mucocutaneous findings of Kawasaki disease (strawberry tongue, cracked lips, conjunctival injection without exudate, extremity changes) are not seen in mononucleosis.
- Additionally, mononucleosis is uncommon in preschool-aged children.
*Antistreptolysin O titer measurement*
- **Antistreptolysin O (ASO) titer** detects recent **Group A Streptococcus** infection and can support a diagnosis of **acute rheumatic fever (ARF)**.
- ARF presents with migratory polyarthritis, carditis, and **erythema marginatum** (not a polymorphous rash), occurring 2-4 weeks after streptococcal pharyngitis.
- The mucocutaneous features in this case are specific to Kawasaki disease and not consistent with ARF.
More Long-term outcomes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.